From Wikipedia, the free encyclopedia
Alternative medicine is any practice that is put forward as having the healing effects of medicine, but is not founded on evidence gathered using the scientific method.[1] It consists of a wide range of health care practices, products and therapies.[2] Examples include new and traditional medicine practices such as homeopathy, naturopathy, chiropractic, energy medicine, various forms of acupuncture, traditional Chinese medicine, Ayurvedic medicine, and Christian faith healing. The treatments are those that are not part of the conventional, science-based healthcare system,[3][4][5][6] and are not backed by scientific evidence.
Complementary medicine is alternative medicine used together with conventional medical treatment in a belief, not proven by using scientific methods, that it "complements" the treatment.[n 1][1][8][9] CAM is the abbreviation for complementary and alternative medicine.[10][11] Integrative medicine (or integrative health) is the combination of the practices and methods of alternative medicine with conventional medicine.[12]
Alternative medical diagnoses and treatments are usually not included in the degree courses of medical schools, or used in conventional medicine, where treatments are based on what is proven using the scientific method. Alternative therapies lack such scientific validation, and their effectiveness is either unproved or disproved.[13][14][15] Alternative medicine is usually based on religion, tradition, superstition, belief in supernatural energies, pseudoscience, errors in reasoning, propaganda, or fraud.[13][16][17][18] Regulation and licensing of alternative medicine and health care providers varies from country to country, and state to state.
The scientific community has criticized alternative medicine as being based on misleading statements, quackery, pseudoscience, antiscience, fraud, or poor scientific methodology. Promoting alternative medicine has been called dangerous and unethical.[19] Testing alternative medicine has been called a waste of scarce medical research resources. Critics have said "there is really no such thing as alternative medicine, just medicine that works and medicine that doesn't",[20] and "Can there be any reasonable 'alternative' [to medicine based on evidence]?"[21]
Types of alternative medicine

A Botanica of traditional Hispanic medicines may look like a pharmacy of science based medicines. The difference is not in their appearance, but in the basis for belief that the medicines have a healing effect.
Alternative medicine consists of a wide range of health care practices, products, and therapies. The shared feature is a claim to heal that is not based on the scientific method. Alternative medicine practices are diverse in their foundations and methodologies.[3] Alternative medicine practices may be classified by their cultural origins or by the types of beliefs upon which they are based.[3][13][16][17] Methods may incorporate or base themselves on traditional medicinal practices of a particular culture, folk knowledge, supersition,[22] spiritual beliefs, belief in supernatural energies (antiscience), pseudoscience, errors in reasoning, propaganda, fraud, new or different concepts of health and disease, and any bases other than being proven by scientific methods.[13][16][17][18] Different cultures may have their own unique traditional or belief based practices developed recently or over thousands of years, and specific practices or entire systems of practices.
Systems based on unscientific beliefs or traditional practices
Alternative medical practices can be based on an underlying belief system inconsistent with science, or on traditional cultural practices.[3]Unscientific belief systems
Alternative medical systems can be based on a common belief systems that are not consistent with facts of science, such as in Naturopathy or Homeopathy.[3]Homeopathy
Homeopathy is a system developed in a belief that a substance that causes the symptoms of a disease in healthy people will cure similar symptoms in sick people.[23] It was developed before knowledge of atoms and molecules, and of basic chemistry, which shows that repeated dilution as practiced in homeopathy produces only water and that homeopathy is false.[24][25][26][27] Homeopathy is considered quackery in the medical community.[28]
Naturopathic medicine
Naturopathic medicine is based on a belief that the body heals itself using a supernatural vital energy that guides bodily processes,[29] a view in conflict with the paradigm of evidence-based medicine.[30] Many naturopaths have opposed vaccination,[31] and "scientific evidence does not support claims that naturopathic medicine can cure cancer or any other disease".[32]Traditional ethnic systems
Alternative medical systems may be based on traditional medicine practices, such as Traditional Chinese medicine, Ayurveda in India, or practices of other cultures around the world.[3]
Traditional Chinese Medicine
Traditional Chinese Medicine is a combination of traditional practices and beliefs developed over thousands of years in China, together with modifications made by the Communist party. Common practices include herbal medicine, acupuncture (insertion of needles in the body at specified points), massage (Tui na), exercise (qigong), and dietary therapy. The practices are based on belief in a supernatural energy called qi, considerations of Chinese Astrology and Chinese numerology, traditional use of herbs and other substances found in China, a belief that a map of the body is contained on the tongue which reflects changes in the body, and an incorrect model of the anatomy and physiology of internal organs.[13][33][34][35][36][37]
The Chinese Communist Party Chairman Mao Zedong, in response to the lack of modern medical practitioners, revived acupuncture and its theory was rewritten to adhere to the political, economic and logistic necessities of providing for the medical needs of China's population.[38] In the 1950s the "history" and theory of Traditional Chinese Medicine was rewritten as communist propaganda, at Mao's insistence, to correct the supposed "bourgeois thought of Western doctors of medicine" (p. 109).[39] Acupuncture gained attention in the United States when President Richard Nixon visited China in 1972, and the delegation was shown a patient undergoing major surgery while fully awake, ostensibly receiving acupuncture rather than anesthesia. Later it was found that the patients selected for the surgery had both a high pain tolerance and received heavy indoctrination before the operation; these demonstration cases were also frequently receiving morphine surreptitiously through an intravenous drip that observers were told contained only fluids and nutrients.[33]
Ayurvedic medicine
Ayurvedic medicine is a traditional medicine of India. It includes a belief that health can be influenced by use of traditional herbs. Ayurveda stresses the use of plant-based medicines and treatments, with some animal products, and added minerals, including sulfur, arsenic, lead, copper sulfate. Andrew Weil, an American promoter of alternative medicine, wrote that in Ayurvedic medicine, "being 'healthy' is more than the absence of disease - it is a radiant state of vigor and energy, which is achieved by balance, or moderation, in food intake, sleep, sexual intercourse and other activities of daily life, complemented by various treatments including a wide variety of plant-based medicines".[40]
Safety concerns have been raised about Ayurveda, with two U.S. studies finding about 20 percent of Ayurvedic Indian-manufactured patent medicines contained toxic levels of heavy metals such as lead, mercury and arsenic. Other concerns include the use of herbs containing toxic compounds and the lack of quality control in Ayurvedic facilities. Incidents of heavy metal poisoning have been attributed to the use of these compounds in the United States.[41][42][43][44][45][46][47]
Supernatural energies and misunderstanding of energy in physics
Bases of belief may include belief in existence of supernatural energies undetected by the science of physics, as in biofields, or in belief in properties of the energies of physics that are inconsistent with the laws of physics, as in energy medicine.[3]
Biofields
Biofield therapies are intended to influence energy fields that, it is purported, surround and penetrate the body.[3] Writers such as noted astrophysicist and advocate of skeptical thinking (Scientific skepticism) Carl Sagan (1934-1996) have described the lack of empirical evidence to support the existence of the putative energy fields on which these therapies are predicated.[48]Acupuncture is a component of Traditional Chinese Medicine. In acupuncture, it is believed that a supernatural energy called qi flows through the universe and through the body, and helps propel the blood, blockage of which leads to disease.[34] It is believed that insertion of needles at various parts of the body determined by astrological calculations can restore balance to the blocked flows, and thereby cure disease.[34]
Chiropractic was developed in the belief that manipulating the spine affects the flow of a supernatural vital energy and thereby affects health and disease.
In the western version of Japanese Reiki, the palms are placed on the patient near Chakras, believed to be centers of supernatural energies, in a belief that the supernatural energies can transfered from the palms of the practitioner, to heal the patient.
Energy medicines
Bioelectromagnetic-based therapies use verifiable electromagnetic fields, such as pulsed fields, alternating-current, or direct-current fields in an unconventional manner.[3] Magnetic healing does not claim existence of supernatural energies, but asserts that magnets can be used to defy the laws of physics to influence health and disease.Holistic health and mind body medicine
Mind-body medicine takes a holistic approach to health that explores the interconnection between the mind, body, and spirit. It works under the premise that the mind can affect "bodily functions and symptoms".[3] Mind body medicines includes healing claims made in yoga, meditation, deep-breathing exercises, guided imagery, hypnotherapy, progressive relaxation, qi gong, and tai chi.[3]
Yoga, a method of traditional stretches, exercises, and meditations in Hinduism, may also be classified as an energy medicine insofar as its healing effects are believed by to be due to a healing "life energy" that is absorbed into the body through the breath, and is thereby believed to treat a wide variety of illnesses and complaints.[49]
Since the 1990's, tai chi (t'ai chi ch'uan) classes that purely emphasise health have become popular in hospitals, clinics, as well as community and senior centers. This has occurred as the baby boomers generation has aged and the art's reputation as a low-stress training method for seniors has become better known.[50][51] There has been some divergence between those that say they practice t'ai chi ch'uan primarily for self-defence, those that practice it for its aesthetic appeal (see wushu below), and those that are more interested in its benefits to physical and mental health.
Qigong, chi kung, or chi gung, is a practice of aligning body, breath, and mind for health, meditation, and martial arts training. With roots in Chinese Traditional Chinese Medicine, philosophy, and martial arts, qigong is traditionally viewed as a practice to cultivate and balance qi (chi) or what has been translated as "life energy".[52]
Herbal remedies and other substances used
Substance based practices use substances found in nature such as herbs, foods, non-vitamin supplements and megavitamins, and minerals, and includes traditional herbal remedies with herbs specific to regions in which the cultural practices arose.[3]
Herbalism, herbology, or herbal medicine, is use of plants for medicinal purposes, and the study of such use. Plants have been the basis for medical treatments through much of human history, and such traditional medicine is still widely practiced today.
Nonvitamin supplements include fish oil, Omega-3 fatty acid, glucosamine, echinacea, flaxseed oil or pills, and ginseng, when used under a claim to have healing effects.[53]
Although the practice of herbalism is not strictly based on evidence gathered using the scientific method, modern medicine, does, however, make use of many plant-derived compounds as the basis for evidence-tested pharmaceutical drugs, and phytotherapy works to apply modern standards of effectiveness testing to herbs and medicines that are derived from natural sources.
The scope of herbal medicine is sometimes extended to include fungal and bee products, as well as minerals, shells and certain animal parts. "Herbal" remedies in this case, may include use of nonherbal toxic chemicals from a nonbiological sources, such as use of the poison lead in Traditional Chinese Medicine.[53]
Body manipulation
Manipulative and body-based practices feature manipulation or movement of body parts, such as is done in bodywork and chiropractic manipulation.Osteopathic manipulative medicine, also known as osteopathic manipulative treatment, is a core set of techniques of osteopathy and osteopathic medicine distinguishing these fields from mainstream medicine.[54]
Religion, faith healing, and prayer
Religion based healing practices, such as use of prayer and the laying of hands in Christian faith healing, and shamanism, rely on belief in divine or spiritual intervention for healing.
Shamanism is a practice of many cultures around the world, in which a practitioner reaches an altered states of consciousness in order to encounter and interact with the spirit world or channel supernatural energies in the belief they can heal.[55]
Alternative medicines based on exploitation of ignorance and flawed reasoning
Some alternative medicine practices may be based on pseudoscience, ignorance, or flawed reasoning.[56] This can lead to fraud.[13]Homeopathy was developed prior to knowledge of the theory of molecules and basic chemistry, which proved that its "remedies" contained nothing more than distilled water.[24][25][26][27]
Practitioners of electricity and magnetism based healing methods may deliberately exploit a patient's ignorance of physics in order to defraud them.[16]
Definitions and terminology
Terms and definitions
The expression "complementary and alternative medicine" (CAM) resists easy definition because the health systems and practices to which it refers are diffuse and its boundaries are poorly defined.[57][58][59][n 2] Healthcare practices categorized as alternative may differ in their historical origin, theoretical basis, diagnostic technique, therapeutic practice and in their relationship to the medical mainstream.[61] Some alternative therapies, including traditional Chinese Medicine (TCM) and Ayurveda, have antique origins in East or South Asia and are entirely alternative medical systems;[62] others, such as homeopathy and chiropractic, have origins in Europe or the United States and emerged in the eighteenth and nineteenth centuries.[63] Some, such as osteopathy and chiropractic, employ manipulative physical methods of treatment; others, such as meditation and prayer, are based on mind-body interventions.[64] Treatments considered alternative in one location may be considered conventional in another.[65] Thus, chiropractic is not considered alternative in Denmark and likewise osteopathic medicine is no longer thought of as an alternative therapy in the United States.[65]One common feature of all definitions of alternative medicine is its designation as "other than" conventional medicine.[66] For example, the widely referenced [67][68] descriptive definition of complementary and alternative medicine devised by the US National Center for Complementary and Alternative Medicine (NCCAM) of the National Institutes of Health (NIH), states that it is "a group of diverse medical and health care systems, practices, and products that are not generally considered part of conventional medicine."[3] This definition has been criticized as, if an alternative therapy, both effective and safe, is adopted by conventional medical practitioners, it does not necessarily follow that either it or its practitioners would no longer be considered alternative.[n 3]
Some definitions seek to specify alternative medicine in terms of its social and political marginality to mainstream healthcare.[71] This can refer to the lack of support that alternative therapies receive from the medical establishment and related bodies regarding access to research funding, sympathetic coverage in the medical press, or inclusion in the standard medical curriculum.[71] In 1993, the British Medical Association (BMA), one among many professional organizations who have attempted to define alternative medicine, stated that it[n 4] referred to "those forms of treatment which are not widely used by the conventional healthcare professions, and the skills of which are not taught as part of the undergraduate curriculum of conventional medical and paramedical healthcare courses".[72] In a US context, an influential definition coined in 1993 by the Harvard-based physician,[73] David M. Eisenberg,[74] characterized alternative medicine "as interventions neither taught widely in medical schools nor generally available in US hospitals".[75] These descriptive definitions are inadequate in the present-day when some conventional doctors offer alternative medical treatments and CAM introductory courses or modules can be offered as part of standard undergraduate medical training;[76] alternative medicine is taught in more than 50 per cent of US medical schools and increasingly US health insurers are willing to provide reimbursement for CAM therapies.[77] In 1999, 7.7% of US hospitals reported using some form of CAM therapy; this proportion had risen to 37.7% by 2008.[78]
An expert panel at a conference hosted in 1995 by the US Office for Alternative Medicine (OAM),[n 5] devised a theoretical definition of alternative medicine as "a broad domain of healing resources ... other than those intrinsic to the politically dominant health system of a particular society or culture in a given historical period."[79] This definition has been widely adopted by CAM researchers,[80] cited by official government bodies such as the UK Department of Health,[81] attributed as the definition used by the Cochrane Collaboration,[82] and, with slight modification, was preferred in the 2005 consensus report of the US Institute of Medicine, Complementary and Alternative Medicine in the United States.[n 6]
The 1995 OAM conference definition, an expansion of Eisenberg's 1993 formulation, is silent regarding questions of the medical effectiveness of alternative therapies.[84] Its proponents hold that it thus avoids relativism about differing forms of medical knowledge and, while it is an essentially political definition, this should not imply that the dominance of mainstream biomedicine is solely due to political forces.[84] According to this definition, alternative and mainstream medicine can only be differentiated with reference to what is "intrinsic to the politically dominant health system of a particular society of culture".[85] However, there is neither a reliable method to distinguish between cultures and subcultures, nor to attribute them as dominant or subordinate, nor any accepted criteria to determine the dominance of a cultural entity.[85] If the culture of a politically dominant healthcare system is held to be equivalent to the perspectives of those charged with the medical management of leading healthcare institutions and programs, the definition fails to recognize the potential for division either within such an elite or between a healthcare elite and the wider population.[85]
Normative definitions distinguish alternative medicine from the biomedical mainstream in its provision of therapies that are unproven, unvalidated or ineffective and support of theories which have no recognized scientific basis.[83] These definitions characterize practices as constituting alternative medicine when, used independently or in place of evidence-based medicine, they are put forward as having the healing effects of medicine, but which are not based on evidence gathered with the scientific method.[1][3][86][87][88] Exemplifying this perspective, a 1998 editorial co-authored by Marcia Angell, a former editor of the New England Journal of Medicine, argued that:
- "It is time for the scientific community to stop giving alternative medicine a free ride. There cannot be two kinds of medicine – conventional and alternative. There is only medicine that has been adequately tested and medicine that has not, medicine that works and medicine that may or may not work. Once a treatment has been tested rigorously, it no longer matters whether it was considered alternative at the outset. If it is found to be reasonably safe and effective, it will be accepted. But assertions, speculation, and testimonials do not substitute for evidence. Alternative treatments should be subjected to scientific testing no less rigorous than that required for conventional treatments."[89]
Paul Offit, while criticizing alternative medicine, has provided a similar type of definition:
- "...there's no such thing as conventional or alternative or complementary or integrative or holistic medicine. There's only medicine that works and medicine that doesn't. And the best way to sort it out is by carefully evaluating scientific studies--not by visiting Internet chat rooms, reading magazine articles, or talking to friends."[91]
"Complementary medicine" refers to use of alternative medicine alongside conventional science based medicine, in the belief that it "may help patients feel better and recover faster."[86] In Science and Technology: Public Attitudes and Public Understanding, chapter 7 of a report Science and Engineering Indicators – 2002, issued by a US government agency (The National Science Foundation), it was stated that the term "alternative medicine" was there being used to refer to all treatments that had not been proven effective using scientific methods.[1]
Regional definitions
Public information websites maintained by the governments of the US and of the UK make a distinction between "alternative medicine" and "complementary medicine", but mention that these two overlap. The National Center for Complementary and Alternative Medicine (NCCAM) of the National Institutes of Health (NIH) (a part of the US Department of Health and Human Services) states that "alternative medicine" refers to using a non-mainstream approach in place of conventional medicine and that "complementary medicine" generally refers to using a non-mainstream approach together with conventional medicine, and comments that the boundaries between complementary and conventional medicine overlap and change with time.[3]The National Health Service (NHS) website NHS Choices (owned by the UK Department of Health), adopting the terminology of NCCAM, states that when a treatment is used alongside conventional treatments, to help a patient cope with a health condition, and not as an alternative to conventional treatment, this use of treatments can be called "complementary medicine"; but when a treatment is used instead of conventional medicine, with the intention of treating or curing a health condition, the use can be called "alternative medicine".[93]
Similarly, the public information website maintained by the National Health and Medical Research Council (NHMRC) of the Commonwealth of Australia uses the acronym "CAM" for a wide range of health care practices, therapies, procedures and devices not within the domain of conventional medicine. In the Australian context this is stated to include acupuncture; aromatherapy; chiropractic; homeopathy; massage; meditation and relaxation therapies; naturopathy; osteopathy; reflexology, traditional Chinese medicine; and the use of vitamin supplements.[94]
The Danish National Board of Health's "Council for Alternative Medicine" (Sundhedsstyrelsens Råd for Alternativ Behandling (SRAB)), an independent institution under the National Board of Health (Danish: Sundhedsstyrelsen), uses the term "alternative medicine" for:[95]
- Treatments performed by therapists that are not authorized healthcare professionals.
- Treatments performed by authorized healthcare professionals, but those based on methods otherwise used mainly outside the healthcare system. People without a healthcare authorisation are [also] allowed to perform the treatments.
Institutions
In General Guidelines for Methodologies on Research and Evaluation of Traditional Medicine, published in 2000 by the World Health Organization (WHO), complementary and alternative medicine were there defined as a broad set of health care practices that are not part of that country's own tradition and are not integrated into the dominant health care system.[96][97]Some herbal therapies are mainstream in Europe but are alternative in the US.[98]
Special terminology used by selected individuals
Two advocates of integrative medicine, writing in 2002 of the American healthcare system, claimed that it also addresses alleged problems with medicine based on science, which are not addressed by CAM; Ralph Snyderman and Andrew Weil stated that "integrative medicine is not synonymous with complementary and alternative medicine. It has a far larger meaning and mission in that it calls for restoration of the focus of medicine on health and healing and emphasizes the centrality of the patient-physician relationship."[99]History – 19th century onwards
Dating from the 1970s, medical professionals, sociologists, anthropologists and other commentators noted the increasing visibility of a wide variety of health practices that had neither derived directly from nor been verified by biomedical science.[100] Since that time, those who have analyzed this trend have deliberated over the most apt language with which to describe this emergent health field.[100] A variety of terms have been used, including heterodox, irregular, fringe and alternative medicine while others, particularly medical commentators, have been satisfied to label them as instances of quackery.[100] The most persistent term has been alternative medicine but its use is problematic as it assumes a value-laden dichotomy between a medical fringe, implicitly of borderline acceptability at best, and a privileged medical orthodoxy, associated with validated medico-scientific norms.[101] The use of the category of alternative medicine has also been criticized as it cannot be studied as an independent entity but must be understood in terms of a regionally and temporally specific medical orthodoxy.[102] Its use can also be misleading as it may erroneously imply that a real medical alternative exists.[103] As with near-synonymous expressions, such as unorthodox, complementary, marginal, or quackery, these linguistic devices have served, in the context of processes of professionalisation and market competition, to establish the authority of official medicine and police the boundary between it and its unconventional rivals.[101]An early instance of the influence of this modern, or western, scientific medicine outside Europe and North America is Peking Union Medical College.[104][n 7][n 8]
From a historical perspective, the emergence of alternative medicine, if not the term itself, is typically dated to the 19th century.[105] This is despite the fact that there are variants of Western non-conventional medicine that arose in the late-eighteenth century or earlier and some non-Western medical traditions, currently considered alternative in the West and elsewhere, which boast extended historical pedigrees.[101] Alternative medical systems, however, can only be said to exist when there is an identifiable, regularized and authoritative standard medical practice, such as arose in the West during the nineteenth-century, to which they can function as an alternative.[106]
During the late eighteenth and nineteenth centuries regular and irregular medical practitioners became more clearly differentiated throughout much of Europe and,[107] as the nineteenth century progressed, most Western states converged in the creation of legally delimited and semi-protected medical markets.[108] It is at this point that an "official" medicine, created in cooperation with the state and employing a scientific rhetoric of legitimacy, emerges as a recognizable entity and that the concept of alternative medicine as a historical category becomes tenable.[109]
As part of this process, professional adherents of mainstream medicine in countries such as Germany, France, and Britain increasingly invoked the scientific basis of their discipline as a means of engendering internal professional unity and of external differentiation in the face of sustained market competition from homeopaths, naturopaths, mesmerists and other nonconventional medical practitioners, finally achieving a degree of imperfect dominance through alliance with the state and the passage of regulatory legislation.[101][103] In the US the Johns Hopkins University School of Medicine, based in Baltimore, Maryland, opened in 1893,with William H. Welch and William Osler among the founding physicians, and was the first medical school devoted to teaching "German scientific medicine".[110]
Buttressed by the increased authority consequent to the significant advances in the medical sciences of the late 19th century onwards—including the development and application of the germ theory of disease by the chemist Louis Pasteur and the surgeon Joseph Lister, 1st Baron Lister, of microbiology co-founded by Robert Koch (in 1885 appointed professor of hygiene at the University of Berlin), and of the use of X-rays (Röntgen rays)—the 1910 Flexner Report called upon American medical schools to follow the model set by the Johns Hopkins School of Medicine and adhere to mainstream science in their teaching and research. This was in a belief, mentioned in the Report's introduction, that the preliminary and professional training then prevailing in medical schools should be reformed in view of the new means for diagnosing and combating disease being made available to physicians and surgeons by the sciences on which medicine depended.[n 9][112]
Among putative medical practices available at the time which later became known as "alternative medicine" were homeopathy (founded in Germany in the early 19c.) and chiropractic (founded in North America in the late 19c.). These conflicted in principle with the developments in medical science upon which the Flexner reforms were based, and they have not become compatible with further advances of medical science such as listed in Timeline of medicine and medical technology, 1900–1999 and 2000–present, nor have Ayurveda, acupuncture or other kinds of alternative medicine.
At the same time "Tropical medicine" was being developed as a specialist branch of western medicine in research establishments such as Liverpool School of Tropical Medicine founded in 1898 by Alfred Lewis Jones, London School of Hygiene & Tropical Medicine, founded in 1899 by Patrick Manson and Tulane University School of Public Health and Tropical Medicine, instituted in 1912. A distinction was being made between western scientific medicine and indigenous systems. An example is given by an official report about indigenous systems of medicine in India, including Ayurveda, submitted by Mohammad Usman of Madras and others in 1923. This stated that the first question the Committee considered was "to decide whether the indigenous systems of medicine were scientific or not".[113][114][115] By the later twentieth century the term 'alternative medicine' had come into use for the purposes of public discussion,[n 10][117] but it was not always being used with the same meaning by all parties. Arnold S. Relman remarked in 1998 that in the best kind of medical practice, all proposed treatments must be tested objectively, and that in the end there will only be treatments that pass and those that do not, those that are proven worthwhile and those that are not. He asked 'Can there be any reasonable "alternative"?'[21] But also in 1998 the then Surgeon General of the United States, David Satcher,[118] issued public information about eight common alternative treatments (including acupuncture, holistic and massage), together with information about common diseases and conditions, on nutrition, diet, and lifestyle changes, and about helping consumers to decipher fraud and quackery, and to find healthcare centers and doctors who practiced alternative medicine.[119]
By 1990, approximately 60 million Americans had used one or more complementary or alternative therapies to address health issues, according to a nationwide survey in the US published in 1993 by David Eisenberg.[120] A study published in the November 11, 1998 issue of the Journal of the American Medical Association reported that 42% of Americans had used complementary and alternative therapies, up from 34% in 1990.[121] However, despite the growth in patient demand for complementary medicine, most of the early alternative/complementary medical centers failed.[122]
Medical education since 1910
Mainly as a result of reforms following the Flexner Report of 1910[123] medical education in established medical schools in the US has generally not included alternative medicine as a teaching topic.[n 11] Typically, their teaching is based on current practice and scientific knowledge about: anatomy, physiology, histology, embryology, neuroanatomy, pathology, pharmacology, microbiology and immunology.[125] Medical schools' teaching includes such topics as doctor-patient communication, ethics, the art of medicine,[126] and engaging in complex clinical reasoning (medical decision-making).[127] Writing in 2002, Snyderman and Weil remarked that by the early twentieth century the Flexner model had helped to create the 20th-century academic health center in which education, research and practice were inseparable. While this had much improved medical practice by defining with increasing certainty the pathophysiological basis of disease, a single-minded focus on the pathophysiological had diverted much of mainstream American medicine from clinical conditions which were not well understood in mechanistic terms and were not effectively treated by conventional therapies.[99]By 2001 some form of CAM training was being offered by at least 75 out of 125 medical schools in the US.[128] Exceptionally, the School of Medicine of the University of Maryland, Baltimore includes a research institute for integrative medicine (a member entity of the Cochrane Collaboration).[129][130] Medical schools are responsible for conferring medical degrees, but a physician typically may not legally practice medicine until licensed by the local government authority. Licensed physicians in the US who have attended one of the established medical schools there have usually graduated Doctor of Medicine (MD).[131] All states require that applicants for MD licensure be graduates of an approved medical school and complete the United States Medical Licensing Exam (USMLE).[131]
The British Medical Association, in its publication Complementary Medicine, New Approach to Good Practice (1993), gave as a working definition of non-conventional therapies (including acupuncture, chiropractic and homeopathy): "those forms of treatment which are not widely used by the orthodox health-care professions, and the skills of which are not part of the undergraduate curriculum of orthodox medical and paramedical health-care courses".[132] By 2000 some medical schools in the UK were offering CAM familiarisation courses to undergraduate medical students while some were also offering modules specifically on CAM.[133]
Proponents and opponents
The Cochrane Collaboration Complementary Medicine Field explains its "Scope and Topics" by giving a broad and general definition for complementary medicine as including practices and ideas which are outside the domain of conventional medicine in several countries and defined by its users as preventing or treating illness, or promoting health and well being, and which complement mainstream medicine in three ways: by contributing to a common whole, by satisfying a demand not met by conventional practices, and by diversifying the conceptual framework of medicine.[134]Proponents of an evidence-base for medicine[n 12][136][137][138][139] such as the Cochrane Collaboration (founded in 1993 and from 2011 providing input for WHO resolutions) take a position that all systematic reviews of treatments, whether "mainstream" or "alternative", ought to be held to the current standards of scientific method.[130] In a study titled Development and classification of an operational definition of complementary and alternative medicine for the Cochrane Collaboration (2011) it was proposed that indicators that a therapy is accepted include government licensing of practitioners, coverage by health insurance, statements of approval by government agencies, and recommendation as part of a practice guideline; and that if something is currently a standard, accepted therapy, then it is not likely to be widely considered as CAM.[80]
That alternative medicine has been on the rise "in countries where Western science and scientific method generally are accepted as the major foundations for healthcare, and 'evidence-based' practice is the dominant paradigm" was described as an "enigma" in the Medical Journal of Australia.[140]
Critics in the US say the expression is deceptive because it implies there is an effective alternative to science-based medicine, and that complementary is deceptive because the word implies that the treatment increases the effectiveness of (complements) science-based medicine, while alternative medicines which have been tested nearly always have no measurable positive effect compared to a placebo.[141][142][143][144]
Some opponents, focused upon health fraud, misinformation, and quackery as public health problems in the US, are highly critical of alternative medicine, notably Wallace Sampson and Paul Kurtz founders of Scientific Review of Alternative Medicine and Stephen Barrett, co-founder of The National Council Against Health Fraud and webmaster of Quackwatch.[145] Grounds for opposing alternative medicine which have been stated in the US and elsewhere are:
- that it is usually based on religion, tradition, superstition, belief in supernatural energies, pseudoscience, errors in reasoning, propaganda, or fraud.[1][141][146][147]
- that alternative therapies typically lack any scientific validation, and their effectiveness is either unproved or disproved.[141][148][149][dubious ]
- that the treatments are those that are not part of the conventional, science-based healthcare system.[3][96][150][4]
- that research on alternative medicine is frequently of low quality and methodologically flawed.[151][full citation needed]
- that where alternative treatments are used in place of conventional science-based medicine, even with the very safest alternative medicines, failure to use or delay in using conventional science-based medicine has resulted in deaths.[152][153]
- that methods may incorporate or base themselves on traditional medicine, folk knowledge, spiritual beliefs, ignorance or misunderstanding of scientific principles, errors in reasoning, or newly conceived approaches claiming to heal.[141][146][154]
- "...by recommending against conventional therapies that are helpful."
- "...by promoting potentially harmful therapies without adequate warning."
- "...by draining patients' bank accounts,..."
- "...by promoting magical thinking,..."
The NCCAM classification system
A United States government agency, the National Center on Complementary and Alternative Medicine (NCCAM), has created its own classification system for branches of complementary and alternative medicine. It classifies complementary and alternative therapies into five major groups, which have some overlap and two types of energy medicine are distinguished: one, "Veritable" involving scientifically observable energy, including magnet therapy, colorpuncture and light therapy; the other "Putative" which invoke physically undetectable or unverifiable energy.[155]Alternative medicine practices and beliefs are diverse in their foundations and methodologies. The wide range of treatments and practices referred to as alternative medicine includes some stemming from nineteenth century North America, such as chiropractic and naturopathy, others, mentioned by Jütte, that originated in eighteenth- and nineteenth-century Germany, such as homeopathy and hydropathy,[103] and some that have originated in China or India, while African, Caribbean, Pacific Island, Native American, and other regional cultures have traditional medical systems as diverse as their diversity of cultures.[3]
Examples of CAM as a broader term for unorthodox treatment and diagnosis of illnesses, disease, infections, etc.,[156] include yoga, acupuncture, aromatherapy, chiropractic, herbalism, homeopathy, hypnotherapy, massage, osteopathy, reflexology, relaxation therapies, spiritual healing and tai chi.[156] CAM differs from conventional medicine. It is normally private medicine and not covered by health insurance.[156] It is paid out of pocket by the patient and is an expensive treatment.[156] CAM tends to be a treatment for upper class or more educated people.[121]
The NCCAM classification system is -
- Whole medical systems: cut across more than one of the other groups; examples include traditional Chinese medicine, naturopathy, homeopathy, and ayurveda
- Mind-body interventions: explore the interconnection between the mind, body, and spirit, under the premise that the mind can affect "bodily functions and symptoms"
- "Biology"-based practices: use substances found in nature such as herbs, foods, vitamins, and other natural substances. (Note that as used here, "biology" does not refer to the science of biology, but is a usage newly coined by NCAAM in the primary source used for this article. "Biology-based" as coined by NCCAM may refer to chemicals from a nonbiological source, such as use of the poison lead in Traditional Chinese Medicine, and to other nonbiological substances.)
- Manipulative and body-based practices: feature manipulation or movement of body parts, such as is done in chiropractic and osteopathic manipulation
- Energy medicine: is a domain that deals with putative and verifiable energy fields:
- Biofield therapies are intended to influence energy fields that, it is purported, surround and penetrate the body. No empirical evidence has been found to support the existence of the putative energy fields on which these therapies are predicated.
- Bioelectromagnetic-based therapies use verifiable electromagnetic fields, such as pulsed fields, alternating-current, or direct-current fields in an unconventional manner.
Examples classified under the NCCAM system
Alternative therapies based on electricity or magnetism use verifiable electromagnetic fields, such as pulsed fields, alternating-current, or direct-current fields in an unconventional manner rather than claiming the existence of imponderable or supernatural energies.[3]Substance based practices use substances found in nature such as herbs, foods, non-vitamin supplements and megavitamins, and minerals, and includes traditional herbal remedies with herbs specific to regions in which the cultural practices arose.[3] Nonvitamin supplements include fish oil, Omega-3 fatty acid, glucosamine, echinacea, flaxseed oil or pills, and ginseng, when used under a claim to have healing effects.[157]
Mind-body interventions, working under the premise that the mind can affect "bodily functions and symptoms",[3] include healing claims made in hypnotherapy,[158] and in guided imagery, meditation, progressive relaxation, qi gong, tai chi and yoga.[3] Meditation practices including mantra meditation, mindfulness meditation, yoga, tai chi, and qi gong have many uncertainties. According to an AHRQ review, the available evidence on meditation practices through September 2005 is of poor methodological quality and definite conclusions on the effects of meditation in healthcare cannot be made using existing research.[159][160]
Naturopathy is based on a belief in vitalism, which posits that a special energy called vital energy or vital force guides bodily processes such as metabolism, reproduction, growth, and adaptation.[161] The term was coined in 1895 [162] by John Scheel and popularized by Benedict Lust, the "father of U.S. naturopathy".[163] Today, naturopathy is primarily practiced in the United States and Canada.[164] Naturopaths in unregulated jurisdictions may use the Naturopathic Doctor designation or other titles regardless of level of education.[165]
Traditional Chinese medicine is based on a concept of vital energy, or Qi,[166] flowing in the body along specific pathways. These purported pathways consist of 12 primary meridians. TCM has many branches including, acupuncture, massage, feng shui, herbs, as well as Chinese astrology.[167] TCM diagnosis is primarily based on looking at the tongue, which is claimed to show the condition of the organs, as well as feeling the pulse of the radial artery, which is also claimed to show the condition of the organs.[168]
Criticism
-
- "There is no alternative medicine. There is only scientifically proven, evidence-based medicine supported by solid data or unproven medicine, for which scientific evidence is lacking.[169] - P.B. Fontanarosa, Journal of the American Medical Association (1998)
CAM is not as well researched as conventional medicine which undergoes intense research before being released to the public.[156] Funding for research is also sparse making it difficult to do further research for effectiveness of CAM.[170] Most funding for CAM is funded by government agencies.[156] Proposed research for CAM are rejected by most private funding agencies because the results of research are not reliable.[156] The research for CAM has to meet certain standards from research ethics committees which most CAM researchers find almost impossible to meet.[156] Because the results of CAM are not quantifiable, it is hard to prove its effectiveness and it appears to work in a more holistic sense.[156] CAM is thought to help the patient in a mental or psychological sense since the research for CAM is hit and miss.[156] Even with the little research done on it, CAM has not been proven to be effective.[171] This creates an issue of whether the patient is receiving all the information about the treatment that is necessary for the patient to be well informed.[156]
CAM is not as well regulated as conventional medicine.[156] There are ethical concerns about whether people who perform CAM have the proper knowledge to perform the treatments they give to patients.[156] CAM is often done by non-physicians and does not operate with the same medical licensing laws as conventional medicine.[156] It is an issue of non-maleficence.[172]
In the USA
A 2002 report on public attitudes and understanding issued by the US National Science Foundation defines the term "alternative medicine" as treatments that had not been proven effective using scientific methods, and described them as giving more weight to ancient traditions and anecdotes over biological science and clinical trials.[1]Criticisms have come from individuals such as Wallace Sampson in an article in Annals of the New York Academy of Sciences, June 1995.[141] Sampson argued that proponents of alternative medicine often used terminology which was loose or ambiguous to create the appearance that a choice between "alternative" effective treatments existed when it did not, or that there was effectiveness or scientific validity when it did not exist, or to suggest that a dichotomy existed when it did not, or to suggest that consistency with science existed when it might not; that the term "alternative" was to suggest that a patient had a choice between effective treatments when there was not; that use of the word "conventional" or "mainstream" was to suggest that the difference between alternative medicine and science based medicine was the prevalence of use, rather than lack of a scientific basis of alternative medicine as compared to "conventional" or "mainstream" science based medicine; that use of the term "complementary" or "integrative" was to suggest that purported supernatural energies of alternative medicine could complement or be integrated into science based medicine. "Integrative medicine" or "integrated medicine" is used to refer to the belief that medicine based on science would be improved by "integration" with alternative medical treatments practices that are not, and is substantially similar in use to the term "complementary and alternative medicine".[12] Sampson has also written that CAM is the "propagation of the absurd", and argues that alternative and complementary have been substituted for quackery, dubious, and implausible.[173]
Another critic, with reference to government funding studies of integrating alternative medicine techniques into the mainstream, Steven Novella, a neurologist at Yale School of Medicine, wrote that it "is used to lend an appearance of legitimacy to treatments that are not legitimate." Another, Marcia Angell, argued that it was "a new name for snake oil."[174] Angell considered that critics felt that healthcare practices should be classified based solely on scientific evidence, and if a treatment had been rigorously tested and found safe and effective, science based medicine will adopt it regardless of whether it was considered "alternative" to begin with.[89] It was thus possible for a method to change categories (proven vs. unproven), based on increased knowledge of its effectiveness or lack thereof. Prominent supporters of this position include George D. Lundberg, former editor of the Journal of the American Medical Association (JAMA).[169]
In an article first published in CA: A Cancer Journal for Clinicians in 1999, "Evaluating complementary and alternative therapies for cancer patients.", Barrie R. Cassileth mentioned that a 1997 letter to the US Senate Subcommittee on Public Health and Safety, which had deplored the lack of critical thinking and scientific rigor in OAM-supported research, had been signed by four Nobel Laureates and other prominent scientists. (This was supported by the National Institutes of Health (NIH).)[175]
In March 2009 a Washington Post staff writer reported that the impending national discussion about broadening access to health care, improving medical practice and saving money was giving a group of scientists an opening to propose shutting down the National Center for Complementary and Alternative Medicine, quoting one of them, Steven Salzberg, a genome researcher and computational biologist at the University of Maryland, saying "One of our concerns is that NIH is funding pseudoscience." They argued that the vast majority of studies were based on fundamental misunderstandings of physiology and disease, and have shown little or no effect.[174] Stephen Barrett, founder and operator of Quackwatch, has argued that practices labeled "alternative" should be reclassified as either genuine, experimental, or questionable. Here he defines genuine as being methods that have sound evidence for safety and effectiveness, experimental as being unproven but with a plausible rationale for effectiveness, and questionable as groundless without a scientifically plausible rationale.[176] Sampson has also pointed out that CAM tolerated contradiction without thorough reason and experiment.[173] Barrett has pointed out that there is a policy at the NIH of never saying something doesn't work only that a different version or dose might give different results.[177] Barrett also expressed concern that, just because some "alternatives" have merit, there is the impression that the rest deserve equal consideration and respect even though most are worthless, since they are all classified under the one heading of alternative medicine.[176]
Writers such as Carl Sagan (1934-1996), a noted astrophysicist, advocate of skeptical thinking (Scientific skepticism) and the author of The Demon–Haunted World: Science as a Candle in the Dark (1996), have described the lack of empirical evidence to support the existence of the putative energy fields on which these therapies are predicated.[178]
According to two writers, Wallace Sampson and K. Butler, marketing is part of the medical training required in chiropractic education, and propaganda methods in alternative medicine have been traced back to those used by Hitler and Goebels in their promotion of pseudoscience in medicine.[141][179]
The NCCAM budget has been criticized[174] because, despite the duration and intensity of studies to measure the efficacy of alternative medicine, there had been no effective CAM treatments supported by scientific evidence as of 2002, according to the QuackWatch website; the NCCAM budget has been on a sharp and sustained rise.[180] Critics of the Center argue that the plausibility of interventions such as botanical remedies, diet, relaxation therapies and yoga should not be used to support research on implausible interventions based on superstition and belief in the supernatural, and that the plausible methods can be studied just as well in other parts of NIH, where they should be made to compete on an equal footing with other research projects.[174]
In the UK
Richard Dawkins, an English evolutionary biologist and author, in an essay in his book A Devil's Chaplain (2003) (chapter 4.4), has defined alternative medicine as a "set of practices that cannot be tested, refuse to be tested, or consistently fail tests."[181] Another essay in the same book (chapter 1.4) quoted from an article by John Diamond in The Independent: "There is really no such thing as alternative medicine, just medicine that works and medicine that doesn't."[20] Dawkins has argued that, if a technique is demonstrated effective in properly performed trials, it ceases to be alternative and simply becomes medicine.[182]As it relates to ethics, in November 2011 Edzard Ernst stated that the "level of misinformation about alternative medicine has now reached the point where it has become dangerous and unethical. So far, alternative medicine has remained an ethics-free zone. It is time to change this."[183] Ernst requested that Prince Charles recall two guides to alternative medicine published by the Foundation for Integrated Health, on the grounds that "[t]hey both contain numerous misleading and inaccurate claims concerning the supposed benefits of alternative medicine" and that "[t]he nation cannot be served by promoting ineffective and sometimes dangerous alternative treatments."[184] In general, he believes that CAM can and should be subjected to scientific testing.[185][n 13]
Placebo effect
A research methods expert and author of "Snake Oil Science", R. Barker Bausell, has stated that "it's become politically correct to investigate nonsense."[177] There are concerns that just having NIH support is being used to give unfounded "legitimacy to treatments that are not legitimate."[174]Use of placebos in order to achieve a placebo effect in integrative medicine has been criticized as "diverting research time, money, and other resources from more fruitful lines of investigation in order to pursue a theory that has no basis in biology".[143][144]
Another critic has argued that academic proponents of integrative medicine sometimes recommend misleading patients by using known placebo treatments in order to achieve a placebo effect.[n 14] However, a 2010 survey of family physicians found that 56% of respondents said they had used a placebo in clinical practice as well. Eighty-five percent of respondents believed placebos can have both psychological and physical benefits.[188]
Integrative medicine has been criticized in that its practitioners, trained in science based medicine, deliberately mislead patients by pretending placebos are not. "Quackademic medicine" is a pejorative term used for "integrative medicine", which is considered to be an infiltration of quackery into academic science-based medicine.[144]
An analysis of trends in the criticism of complementary and alternative medicine (CAM) in five prestigious American medical journals during the period of reorganization within medicine (1965–1999) was reported as showing that the medical profession had responded to the growth of CAM in three phases, and that in each phase there had been changes in the medical marketplace which influenced the type of response in the journals.[189] Changes included relaxed medical licensing, the development of managed care, rising consumerism, and the establishment of the USA Office of Alternative Medicine (now National Center for Complementary and Alternative Medicine).[n 15] In the "condemnation" phase, from the late 1960s to the early 1970s, authors had ridiculed, exaggerated the risks, and petitioned the state to contain CAM; in the "reassessment" phase (mid-1970s through early 1990s), when increased consumer utilization of CAM was prompting concern, authors had pondered whether patient dissatisfaction and shortcomings in conventional care contributed to the trend; in the "integration" phase of the 1990s physicians began learning to work around or administer CAM, and the subjugation of CAM to scientific scrutiny had become the primary means of control.
Use and regulation
Prevalence of use
Complementary and alternative medicine (CAM) has been described as a broad domain of healing resources that encompasses all health systems, modalities, and practices and their accompanying theories and beliefs, other than those intrinsic to the politically dominant health system of a particular society or culture in a given historical period. CAM includes all such practices and ideas self-defined by their users as preventing or treating illness or promoting health and well-being. Boundaries within CAM and between the CAM domain and that of the dominant system are not always sharp or fixed.[80][dubious ]About 50% of people in developed countries use some kind of complementary and alternative medicine other than prayer for health.[191][192][193] A British telephone survey by the BBC of 1209 adults in 1998 shows that around 20% of adults in Britain had used alternative medicine in the past 12 months.[194] About 40% of cancer patients use some form of CAM.[195]
In developing nations, access to essential medicines is severely restricted by lack of resources and poverty. Traditional remedies, often closely resembling or forming the basis for alternative remedies, may comprise primary healthcare or be integrated into the healthcare system. In Africa, traditional medicine is used for 80% of primary healthcare, and in developing nations as a whole over one-third of the population lack access to essential medicines.[196]
In the USA
In the United States, the 1974 Child Abuse Prevention and Treatment Act (CAPTA) required states to grant religious exemptions to child neglect and abuse laws, regarding religion-based healing practices, in order to receive federal money.[197] Thirty-one states have child-abuse religious exemptions.[198]In respect of taxation in the USA, the Internal Revenue Service has discriminated in favour of medical expenses for acupuncture and chiropractic (and others including Christian Science practitioners) but against homeopathy and the use of non-prescription required medicine.[n 16]
The use of alternative medicine in the US has increased,[1][121] with a 50 percent increase in expenditures and a 25 percent increase in the use of alternative therapies between 1990 and 1997 in America.[121] Americans spend many billions on the therapies annually.[121] Most Americans used CAM to treat and/or prevent musculoskeletal conditions or other conditions associated with chronic or recurring pain.[192] In America, women were more likely than men to use CAM, with the biggest difference in use of mind-body therapies including prayer specifically for health reasons".[192] In 2008, more than 37% of American hospitals offered alternative therapies, up from 26.5 percent in 2005, and 25% in 2004.[200][201] More than 70% of the hospitals offering CAM were in urban areas.[201]
A survey of Americans found that 88 percent agreed that "there are some good ways of treating sickness that medical science does not recognize".[1] Use of magnets was the most common tool in energy medicine in America, and among users of it, 58 percent described it as at least "sort of scientific", when it is not at all scientific.[1] In 2002, at least 60 percent of US medical schools have at least some class time spent teaching alternative therapies.[1] "Therapeutic touch", was taught at more than 100 colleges and universities in 75 countries before the practice was debunked by a nine-year-old child for a school science project.[1][202]
A 1997 survey found that 13.7% of respondents in the US had sought the services of both a medical doctor and an alternative medicine practitioner. The same survey found that 96% of respondents who sought the services of an alternative medicine practitioner also sought the services of a medical doctor in the past 12 months. Medical doctors are often unaware of their patient's use of alternative medical treatments as only 38.5% of the patients alternative therapies were discussed with their medical doctor.[121]
According to Michael H. Cohen, US regulation of alternative includes state licensure of healthcare providers and scope of practice limits on practice by non-MD healthcare professionals; state-law malpractice rules (standard of care limits on professional negligence); discipline of practitioners by state regulatory boards; and federal regulation such as food and drug law.[203] He argues that US regulation of alternative medicine "seeks to integrate biomedical, holistic, and social models of health care in ways that maximize patients’ well-being [w]hile still protecting patients from fraud."[204]
Prevalence of use of specific therapies
The most common CAM therapies used in the US in 2002 were prayer (45.2%), herbalism (18.9%), breathing meditation (11.6%), meditation (7.6%), chiropractic medicine (7.5%), yoga (5.1%-6.1%), body work (5.0%), diet-based therapy (3.5%), progressive relaxation (3.0%), mega-vitamin therapy (2.8%) and Visualization (2.1%)[192][205]In Britain, the most often used alternative therapies were Alexander technique, Aromatherapy, Bach and other flower remedies, Body work therapies including massage, Counseling stress therapies, hypnotherapy, Meditation, Reflexology, Shiatsu, Ayurvedic medicine, Nutritional medicine, and Yoga.[206] Ayurvedic medicine remedies are mainly plant based with some use of animal materials.[207] Safety concerns include the use of herbs containing toxic compounds and the lack of quality control in Ayurvedic facilities.[47][208]
According to the National Health Service (England), the most commonly used complementary and alternative medicines (CAM) supported by the NHS in the UK are: acupuncture, aromatherapy, chiropractic, homeopathy, massage, osteopathy and clinical hypnotherapy.[209]
"Complementary medicine treatments used for pain include: acupuncture, low-level laser therapy, meditation, aroma therapy, Chinese medicine, dance therapy, music therapy, massage, herbalism, therapeutic touch, yoga, osteopathy, chiropractic, naturopathy, and homeopathy."[210]
In palliative care
Complementary therapies are often used in palliative care or by practitioners attempting to manage chronic pain in patients. Integrative medicine is considered more acceptable in the interdisciplinary approach used in palliative care than in other areas of medicine. "From its early experiences of care for the dying, palliative care took for granted the necessity of placing patient values and lifestyle habits at the core of any design and delivery of quality care at the end of life. If the patient desired complementary therapies, and as long as such treatments provided additional support and did not endanger the patient, they were considered acceptable."[211] The non-pharmacologic interventions of complementary medicine can employ mind-body interventions designed to "reduce pain and concomitant mood disturbance and increase quality of life."[212]Regulation
In Austria and Germany complementary and alternative medicine is mainly in the hands of doctors with MDs,[10] and half or more of the American alternative practitioners are licensed MDs.[213] In Germany herbs are tightly regulated: half are prescribed by doctors and covered by health insurance.[214]Some professions of complementary/traditional/alternative medicine, such as chiropractic, have achieved full regulation in North America and other parts of the world[215] and are regulated in a manner similar to that governing science-based medicine. In contrast, other approaches may be partially recognized and others have no regulation at all. Regulation and licensing of alternative medicine ranges widely from country to country, and state to state.[215]
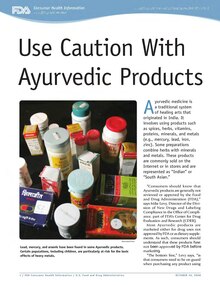
Health campaign flyers, as in this example from the Food and Drug Administration, warn the public about unsafe products.
Government bodies in the USA and elsewhere have published information or guidance about alternative medicine. One of those is the U.S. Food and Drug Administration (FDA), which mentions specifically homeopathic products, traditional Chinese medicine and Ayurvedic products.[216] A document which the FDA has issued for comment is headed Guidance for Industry: Complementary and Alternative Medicine Products and Their Regulation by the Food and Drug Administration, last updated on March 2, 2007. The document opens with three preliminary paragraphs which explain that in the document:
- "complementary and alternative medicine" (CAM) are being used to encompass a wide array of health care practices, products, and therapies which are distinct from those used in "conventional" or "allopathic" medicine.
- some forms of CAM, such as traditional Chinese medicine and Ayurvedic medicine, have been practiced for centuries, and others, such as electrotherapy, are of more recent origin.
- in a publication of The Institute of Medicine it has been stated that more than one-third of American adults reported using some form of CAM and that visits to CAM providers each year exceed those to primary care physicians (Institute of Medicine, Complementary and Alternative Medicine in the United States, pages 34–35, 2005).
- no mention (in the document) of a particular CAM therapy, practice or product should be taken as expressing FDA's support or endorsement of it or as an agency determination that a particular product is safe and effective.[2]
Efficacy
Alternative therapies lack the requisite scientific validation, and their effectiveness is either unproved or disproved.[1][141][148][149] Many of the claims regarding the efficacy of alternative medicines are controversial, since research on them is frequently of low quality and methodologically flawed.[151][full citation needed] Selective publication of results (misleading results from only publishing positive results, and not all results), marked differences in product quality and standardisation, and some companies making unsubstantiated claims, call into question the claims of efficacy of isolated examples where herbs may have some evidence of containing chemicals that may affect health.[220] The Scientific Review of Alternative Medicine points to confusions in the general population - a person may attribute symptomatic relief to an otherwise-ineffective therapy just because they are taking something (the placebo effect); the natural recovery from or the cyclical nature of an illness (the regression fallacy) gets misattributed to an alternative medicine being taken; a person not diagnosed with science based medicine may never originally have had a true illness diagnosed as an alternative disease category.[221]Edzard Ernst characterized the evidence for many alternative techniques as weak, nonexistent, or negative[185] and in 2011 published his estimate that about 7.4% were based on "sound evidence", although he believes that may be an overestimate due to various reasons.[222] Ernst has concluded that 95% of the alternative treatments he and his team studied, including acupuncture, herbal medicine, homeopathy, and reflexology, are "statistically indistinguishable from placebo treatments", but he also believes there is something that conventional doctors can usefully learn from the chiropractors and homeopath: this is the therapeutic value of the placebo effect, one of the strangest phenomena in medicine.[223][224]
In 2003, a project funded by the CDC identified 208 condition-treatment pairs, of which 58% had been studied by at least one randomized controlled trial (RCT), and 23% had been assessed with a meta-analysis.[225] According to a 2005 book by a US Institute of Medicine panel, the number of RCTs focused on CAM has risen dramatically. The book cites Vickers (1998), who found that many of the CAM-related RCTs are in the Cochrane register, but 19% of these trials were not in MEDLINE, and 84% were in conventional medical journals.[226]
As of 2005, the Cochrane Library had 145 CAM-related Cochrane systematic reviews and 340 non-Cochrane systematic reviews. An analysis of the conclusions of only the 145 Cochrane reviews was done by two readers. In 83% of the cases, the readers agreed. In the 17% in which they disagreed, a third reader agreed with one of the initial readers to set a rating. These studies found that, for CAM, 38.4% concluded positive effect or possibly positive (12.4%), 4.8% concluded no effect, 0.69% concluded harmful effect, and 56.6% concluded insufficient evidence. An assessment of conventional treatments found that 41.3% concluded positive or possibly positive effect, 20% concluded no effect, 8.1% concluded net harmful effects, and 21.3% concluded insufficient evidence. However, the CAM review used the more developed 2004 Cochrane database, while the conventional review used the initial 1998 Cochrane database.[227]
Most alternative medical treatments are not patentable, which may lead to less research funding from the private sector. In addition, in most countries, alternative treatments (in contrast to pharmaceuticals) can be marketed without any proof of efficacy—also a disincentive for manufacturers to fund scientific research.[228] Some have proposed adopting a prize system to reward medical research.[229] However, public funding for research exists. Increasing the funding for research on alternative medicine techniques is the purpose of the US National Center for Complementary and Alternative Medicine. NCCAM and its predecessor, the Office of Alternative Medicine, have spent more than $2.5 billion on such research since 1992; this research has largely not demonstrated the efficacy of alternative treatments.[177][230][231]
In the same way as for conventional therapies, drugs, and interventions, it can be difficult to test the efficacy of alternative medicine in clinical trials. In instances where an established, effective, treatment for a condition is already available, the Helsinki Declaration states that withholding such treatment is unethical in most circumstances. Use of standard-of-care treatment in addition to an alternative technique being tested may produce confounded or difficult-to-interpret results.[232]
Cancer researcher Andrew J. Vickers has stated:
- "Contrary to much popular and scientific writing, many alternative cancer treatments have been investigated in good-quality clinical trials, and they have been shown to be ineffective. In this article, clinical trial data on a number of alternative cancer cures including Livingston-Wheeler, Di Bella Multitherapy, antineoplastons, vitamin C, hydrazine sulfate, Laetrile, and psychotherapy are reviewed. The label 'unproven' is inappropriate for such therapies; it is time to assert that many alternative cancer therapies have been 'disproven'."[233]
Adequacy of regulation and CAM safety
Many of the claims regarding the safety and efficacy of alternative medicine are controversial. Some alternative treatments have been associated with unexpected side effects, which can be fatal.[citation needed]One of the commonly voiced concerns about complementary alternative medicine (CAM) is the manner in which is regulated. There have been significant developments in how CAMs should be assessed prior to re-sale in the United Kingdom and the European Union (EU) in the last 2 years. Despite this, it has been suggested that current regulatory bodies have been ineffective in preventing deception of patients as many companies have re-labelled their drugs to avoid the new laws.[240] There is no general consensus about how to balance consumer protection (from false claims, toxicity, and advertising) with freedom to choose remedies.
Advocates of CAM suggest that regulation of the industry will adversely affect patients looking for alternative ways to manage their symptoms, even if many of the benefits may represent the placebo affect.[241] Some contend that alternative medicines should not require any more regulation than over-the-counter medicines that can also be toxic in overdose (such as paracetamol).[242]
Interactions with conventional pharmaceuticals
Forms of alternative medicine that are biologically active can be dangerous even when used in conjunction with conventional medicine. Examples include immuno-augmentation therapy, shark cartilage, bioresonance therapy, oxygen and ozone therapies, insulin potentiation therapy. Some herbal remedies can cause dangerous interactions with chemotherapy drugs, radiation therapy, or anesthetics during surgery, among other problems.[11] An anecdotal example of these dangers was reported by Associate Professor Alastair MacLennan of Adelaide University, Australia regarding a patient who almost bled to death on the operating table after neglecting to mention that she had been taking "natural" potions to "build up her strength" before the operation, including a powerful anticoagulant that nearly caused her death.[243]To ABC Online, MacLennan also gives another possible mechanism:
- And lastly [sic] there's the cynicism and disappointment and depression that some patients get from going on from one alternative medicine to the next, and they find after three months the placebo effect wears off, and they're disappointed and they move on to the next one, and they're disappointed and disillusioned, and that can create depression and make the eventual treatment of the patient with anything effective difficult, because you may not get compliance, because they've seen the failure so often in the past.[244]
Potential side-effects
Conventional treatments are subjected to testing for undesired side-effects, whereas alternative treatments, in general, are not subjected to such testing at all. Any treatment – whether conventional or alternative – that has a biological or psychological effect on a patient may also have potential to possess dangerous biological or psychological side-effects. Attempts to refute this fact with regard to alternative treatments sometimes use the appeal to nature fallacy, i.e., "that which is natural cannot be harmful".An exception to the normal thinking regarding side-effects is Homeopathy. Since 1938, the U.S. Food and Drug Administration (FDA) has regulated homeopathic products in "several significantly different ways from other drugs."[245] Homeopathic preparations, termed "remedies", are extremely dilute, often far beyond the point where a single molecule of the original active (and possibly toxic) ingredient is likely to remain. They are, thus, considered safe on that count, but "their products are exempt from good manufacturing practice requirements related to expiration dating and from finished product testing for identity and strength", and their alcohol concentration may be much higher than allowed in conventional drugs.[245]
Treatment delay
Those having experienced or perceived success with one alternative therapy for a minor ailment may be convinced of its efficacy and persuaded to extrapolate that success to some other alternative therapy for a more serious, possibly life-threatening illness.[246] For this reason, critics argue that therapies that rely on the placebo effect to define success are very dangerous. According to mental health journalist Scott Lilienfeld in 2002, "unvalidated or scientifically unsupported mental health practices can lead individuals to forgo effective treatments" and refers to this as "opportunity cost".Individuals who spend large amounts of time and money on ineffective treatments may be left with precious little of either, and may forfeit the opportunity to obtain treatments that could be more helpful. In short, even innocuous treatments can indirectly produce negative outcomes.[152] Between 2001 and 2003, four children died in Australia because their parents chose ineffective naturopathic, homeopathic, or other alternative medicines and diets rather than conventional therapies.[153]
Unconventional cancer "cures"
There have always been "many therapies offered outside of conventional cancer treatment centers and based on theories not found in biomedicine. These alternative cancer cures have often been described as 'unproven,' suggesting that appropriate clinical trials have not been conducted and that the therapeutic value of the treatment is unknown." However, "many alternative cancer treatments have been investigated in good-quality clinical trials, and they have been shown to be ineffective....The label 'unproven' is inappropriate for such therapies; it is time to assert that many alternative cancer therapies have been 'disproven'."[233]Edzard Ernst has stated:
- "... any alternative cancer cure is bogus by definition. There will never be an alternative cancer cure. Why? Because if something looked halfway promising, then mainstream oncology would scrutinize it, and if there is anything to it, it would become mainstream almost automatically and very quickly. All curative "alternative cancer cures" are based on false claims, are bogus, and, I would say, even criminal."[247]
Research funding
Funding for research into effectiveness of alternative treatments comes from a variety of public and private sources. In the USA, one conduit for funding and information is the National Center for Complementary and Alternative Medicine (NCCAM), a division of DHS's National Institutes of Health (NIH).[248] Other governments have various levels of funding; the Dutch government funded CAM research between 1986 and 2003, but formally ended it in 2006.[249]Appeal
Physicians who practice complementary medicine usually discuss and advise patients as to available complementary therapies. Patients often express interest in mind-body complementary therapies because they offer a non-drug approach to treating some health conditions.[250] Some mind-body techniques, such as cognitive-behavioral therapy, were once considered complementary medicine, but are now a part of conventional medicine in the United States.[251]Against alternative medicine it has been argued that in addition to the social-cultural underpinnings of the popularity of alternative medicine, there are several psychological issues that are critical to its growth. One of the most critical is the placebo effect, which is a well-established observation in medicine.[252] Related to it are similar psychological effects such as the will to believe,[253] cognitive biases that help maintain self-esteem and promote harmonious social functioning,[253] and the post hoc, ergo propter hoc fallacy.[253]
In the UK
CAM's popularity may be related to other factors which Edzard Ernst mentioned in an interview in The Independent:Why is it so popular, then? Ernst blames the providers, customers and the doctors whose neglect, he says, has created the opening into which alternative therapists have stepped. "People are told lies. There are 40 million websites and 39.9 million tell lies, sometimes outrageous lies. They mislead cancer patients, who are encouraged not only to pay their last penny but to be treated with something that shortens their lives. "At the same time, people are gullible. It needs gullibility for the industry to succeed. It doesn't make me popular with the public, but it's the truth.[254]In a paper published in October 2010 entitled The public's enthusiasm for complementary and alternative medicine amounts to a critique of mainstream medicine, Ernst described these views in greater detail and concluded:
[CAM] is popular. An analysis of the reasons why this is so points towards the therapeutic relationship as a key factor. Providers of CAM tend to build better therapeutic relationships than mainstream healthcare professionals. In turn, this implies that much of the popularity of CAM is a poignant criticism of the failure of mainstream healthcare. We should consider it seriously with a view of improving our service to patients.[255]
In the USA and Canada
A study published in 1998 indicates that a majority of alternative medicine use was in conjunction with standard medical treatments.[193] Approximately 4.4 percent of those studied used alternative medicine as a replacement for conventional medicine. The research found that those having used alternative medicine tended to have higher education or report poorer health status. Dissatisfaction with conventional medicine was not a meaningful factor in the choice, but rather the majority of alternative medicine users appear to be doing so largely because "they find these healthcare alternatives to be more congruent with their own values, beliefs, and philosophical orientations toward health and life." In particular, subjects reported a holistic orientation to health, a transformational experience that changed their worldview, identification with a number of groups committed to environmentalism, feminism, psychology, and/or spirituality and personal growth, or that they were suffering from a variety of common and minor ailments – notable ones being anxiety, back problems, and chronic pain.Authors have speculated on the socio-cultural and psychological reasons for the appeal of alternative medicines among that minority using them in lieu of conventional medicine. There are several socio-cultural reasons for the interest in these treatments centered on the low level of scientific literacy among the public at large and a concomitant increase in antiscientific attitudes and new age mysticism.[253] Related to this are vigorous marketing[256] of extravagant claims by the alternative medical community combined with inadequate media scrutiny and attacks on critics.[146][253]
There is also an increase in conspiracy theories toward conventional medicine and pharmaceutical companies, mistrust of traditional authority figures, such as the physician, and a dislike of the current delivery methods of scientific biomedicine, all of which have led patients to seek out alternative medicine to treat a variety of ailments.[146] Many patients lack access to contemporary medicine, due to a lack of private or public health insurance, which leads them to seek out lower-cost alternative medicine.[192] Medical doctors are also aggressively marketing alternative medicine to profit from this market.[256]
Patients can also be averse to the painful, unpleasant, and sometimes-dangerous side effects of biomedical treatments. Treatments for severe diseases such as cancer and HIV infection have well-known, significant side-effects. Even low-risk medications such as antibiotics can have potential to cause life-threatening anaphylactic reactions in a very few individuals. Also, many medications may cause minor but bothersome symptoms such as cough or upset stomach. In all of these cases, patients may be seeking out alternative treatments to avoid the adverse effects of conventional treatments.[146][253]
Schofield and others, in a systematic review published in 2011, make ten recommendations which they think may increase the effectiveness of consultations in a conventional (here: oncology) setting, such as "Ask questions about CAM use at critical points in the illness trajectory"; "Respond to the person's emotional state"; and "Provide balanced, evidence-based advice". They suggest that this approach may address "... concerns surrounding CAM use [and] encourage informed decision-making about CAM and ultimately, improve outcomes for patients".[257]