From Wikipedia, the free encyclopedia
Galen
|
|---|
Eighteenth-century portrait by Georg Paul Busch
|
| Born | September 129 AD
|
|---|
| Died | c. 210 AD |
|---|
| Occupation | Physician |
|---|
Aelius Galenus or
Claudius Galenus (
Greek:
Κλαύδιος Γαληνός; September 129 AD –
c. 200/
c. 216), often
Anglicized as
Galen and better known as
Galen of Pergamon (
), was a
Greek physician,
surgeon and
philosopher in the
Roman Empire. Arguably the most accomplished of all
medical researchers of
antiquity, Galen influenced the development of various scientific disciplines, including
anatomy,
physiology,
pathology,
pharmacology, and
neurology, as well as philosophy and
logic.
The son of
Aelius Nicon,
a wealthy architect with scholarly interests, Galen received a
comprehensive education that prepared him for a successful career as a
physician and philosopher. Born in
Pergamon (present-day
Bergama,
Turkey), Galen travelled extensively, exposing himself to a wide variety of medical theories and discoveries before settling in
Rome, where he served prominent members of Roman society and eventually was given the position of personal physician to several
emperors.
Galen's understanding of anatomy and
medicine was principally influenced by the then-current theory of
humorism (also known as the four humors – black bile, yellow bile, blood, and phlegm), as advanced by ancient Greek physicians such as
Hippocrates. His theories dominated and influenced
Western medical science for more than 1,300 years. His anatomical reports, based mainly on
dissection of
monkeys, especially the
Barbary macaque, and
pigs,
remained uncontested until 1543, when printed descriptions and
illustrations of human dissections were published in the seminal work
De humani corporis fabrica by
Andreas Vesalius where Galen's physiological theory was accommodated to these new observations. Galen's theory of the physiology of the
circulatory system remained unchallenged until ca. 1242, when
Ibn al-Nafis published his book
Sharh tashrih al-qanun li’ Ibn Sina (
Commentary on Anatomy in Avicenna's Canon), in which he reported his discovery of the
pulmonary circulation.
Galen saw himself as both a physician and a philosopher, as he wrote in his treatise entitled
That the Best Physician Is Also a Philosopher. Galen was very interested in the debate between the
rationalist and
empiricist medical sects, and his use of direct observation, dissection and
vivisection represents a complex middle ground between the extremes of those two viewpoints.
Many of his works have been preserved and/or translated from the
original Greek, although many were destroyed and some credited to him
are believed to be spurious. Although there is some debate over the date
of his death, he was no younger than seventy when he died.
In
medieval
Europe, Galen's writings on anatomy became the mainstay of the medieval
physician's university curriculum, but because of the collapse of the
Roman Empire in the West they suffered greatly from stasis and
intellectual stagnation. However, in the
Eastern Roman Empire and the
Abbasid Caliphate they continued to be studied and followed. Some of Galen's ideas were incorrect, as he did not dissect a human body.
Greek and Roman taboos had meant that dissection was usually banned in
ancient times, but in Middle Ages it changed: medical teachers and
students at Bologna began to open human bodies, and
Mondino de Luzzi (ca. 1275–1326) produced the first known anatomy textbook based on human dissection.
Galen's original Greek texts gained renewed prominence during the
early modern period. In the 1530s, Belgian anatomist and physician
Andreas Vesalius took on a project to translate many of Galen's Greek texts into Latin. Vesalius's most famous work,
De humani corporis fabrica, was greatly influenced by Galenic writing and form.
Early life: AD 129–161
Galen's name Γαληνός, Galēnos comes from the adjective "γαληνός", "calm".
Galen describes his early life in
On the affections of the mind. He was born in September AD 129. His father,
Aelius Nicon, was a wealthy
patrician,
an architect and builder, with eclectic interests including philosophy,
mathematics, logic, astronomy, agriculture and literature. Galen
describes his father as a "highly amiable, just, good and benevolent
man". At that time
Pergamon (modern-day
Bergama,
Turkey) was a major cultural and intellectual centre, noted for its
library, second only to that in Alexandria,
and attracted both
Stoic and
Platonic
philosophers, to whom Galen was exposed at age 14. His studies also
took in each of the principal philosophical systems of the time,
including
Aristotelian and
Epicurean.
His father had planned a traditional career for Galen in philosophy or
politics and took care to expose him to literary and philosophical
influences. However, Galen states that in around AD 145 his father had a
dream in which the god
Asclepius
(Aesculapius) appeared and commanded Nicon to send his son to study
medicine. Again, no expense was spared, and following his earlier
liberal education, at 16 he began studies at the prestigious local
sanctuary or
Asclepieum dedicated to Asclepius, god of medicine, as a θεραπευτής (
therapeutes, or attendant) for four years. There he came under the influence of men like
Aeschrion of Pergamon,
Stratonicus and Satyrus. Asclepiea functioned as spas or sanitoria to
which the sick would come to seek the ministrations of the priesthood.
Romans frequented the temple at Pergamon in search of medical relief
from illness and disease. It was also the haunt of notable people such
as Claudius Charax the historian,
Aelius Aristides the orator,
Polemo the sophist, and Cuspius Rufinus the Consul.
Galen's father died in 148, leaving Galen independently wealthy
at the age of 19. He then followed the advice he found in Hippocrates'
teaching and travelled and studied widely including such destinations as
Smyrna (now
Izmir),
Corinth,
Crete,
Cilicia (now
Çukurova),
Cyprus, and finally the great medical school of
Alexandria,
exposing himself to the various schools of thought in medicine. In 157,
aged 28, he returned to Pergamon as physician to the gladiators of the
High Priest of Asia, one of the most influential and wealthy men in
Asia. Galen claims that the High Priest chose him over other physicians
after he eviscerated an ape and challenged other physicians to repair
the damage. When they refused, Galen performed the
surgery
himself and in so doing won the favor of the High Priest of Asia. Over
his four years there, he learned the importance of diet, fitness,
hygiene and preventive measures, as well as living anatomy, and the
treatment of fractures and severe trauma, referring to their
wounds
as "windows into the body". Only five deaths among the gladiators
occurred while he held the post, compared to sixty in his predecessor's
time, a result that is in general ascribed to the attention he paid to
their wounds. At the same time he pursued studies in theoretical
medicine and philosophy.
Later years: AD 162–217
Modern statue of Galen in his home town, Pergamon
Galen went to
Rome
in 162 and made his mark as a practicing physician. His impatience
brought him into conflict with other doctors and he felt menaced by
them. His demonstrations there antagonized the less skilled and more
conservative physicians in the city. When Galen's animosity with the
Roman medical practitioners became serious, he feared he might be exiled
or poisoned, so he left the city.
Rome had engaged in foreign wars in 161;
Marcus Aurelius and his colleague
Lucius Verus were in the north fighting the
Marcomanni. During the autumn of 169 when Roman troops were returning to
Aquileia,
a great plague broke out, and the emperor summoned Galen back to Rome.
He was ordered to accompany Marcus and Verus to Germany as the court
physician. The following spring Marcus was persuaded to release Galen
after receiving a report that
Asclepius was against the project. He was left behind to act as physician to the imperial heir
Commodus.
It was here in court that Galen wrote extensively on medical subjects.
Ironically, Lucius Verus died in 169, and Marcus Aurelius himself died
in 180, both victims of the plague.
Galen was the physician to Commodus for much of the emperor’s
life and treated his common illnesses. According to Dio Cassius
72.14.3–4, in about 189, under Commodus’ reign, a pestilence occurred
which at its height killed 2,000 people a day in Rome. This was most
likely the same plague that struck Rome during Marcus Aurelius’ reign.
Galen became physician to
Septimius Severus during his reign in Rome. Galen compliments Severus and
Caracalla on keeping a supply of drugs for their friends and mentions three cases in which they had been of use in 198.
The Antonine Plague
The 'Galen' group of physicians in an image from the Vienna Dioscurides; he is depicted top center.
The Antonine Plague was named after Marcus Aurelius’ family name of
Antoninus. It was also known as the Plague of Galen and held an
important place in medicinal history because of its association with
Galen. He had first-hand knowledge of the disease, and was present in
Rome when it first struck in 166 AD, and was also present in the winter
of 168–69 during an outbreak among troops stationed at
Aquileia.
He had experience with the epidemic, referring to it as very long
lasting, and described its symptoms and his treatment of it.
Unfortunately, his references to the plague are scattered and brief.
Galen was not trying to present a description of the disease so that it
could be recognized in future generations; he was more interested in the
treatment and physical effects of the disease. For example, in his
writings about a young man afflicted with the plague, he concentrated on
the treatment of internal and external ulcerations. According to
Niebuhr, "this pestilence must have raged with incredible fury; it
carried off innumerable victims. The ancient world never recovered from
the blow inflicted upon it by the plague that visited it in the reign of
M. Aurelius."
The mortality rate of the plague was 7–10 percent; the outbreak in
165–168 would have caused approximately 3.5 to 5 million deaths.
Otto Seeck
believes that over half the population of the empire perished. J. F.
Gilliam believes that the Antonine plague probably caused more deaths
than any other epidemic during the empire before the mid-3rd century. Although Galen's description is incomplete, it is sufficient to enable a firm identification of the disease as
smallpox.
Galen notes that the
exanthema
covered the victim's entire body and was usually black. The exanthem
became rough and scabby where there was no ulceration. He states that
those who were going to survive developed a black exanthem. According to
Galen, it was black because of a remnant of blood putrefied in a fever
blister that was pustular. His writings state that raised blisters were
present in the Antonine plague, usually in the form of a blistery rash.
Galen states that the skin rash was close to the one
Thucydides
described. Galen describes symptoms of the alimentary tract via a
patient's diarrhea and stools. If the stool was very black, the patient
died. He says that the amount of black stools varied. It depended on the
severity of the intestinal lesions. He observes that in cases where the
stool was not black, the black exanthema appeared. Galen describes the
symptoms of fever, vomiting, fetid breath,
catarrh, cough, and ulceration of the larynx and trachea.
Eudemus
When the
Peripatetic philosopher Eudemus became ill with
quartan fever, Galen felt obliged to treat him "since he was my teacher and I happened to live nearby."
Galen wrote: "I return to the case of Eudemus. He was thoroughly
attacked by the three attacks of quartan ague, and the doctors had given
him up, as it was now mid-winter." Some Roman physicians criticized Galen for his use of the
prognosis in his treatment of Eudemus. This practice conflicted with the then-current
standard of care, which relied upon
divination and
mysticism.
Galen retaliated against his detractors by defending his own methods.
Garcia-Ballester quotes Galen as saying: "In order to diagnose, one must
observe and reason. This was the basis of his criticism of the doctors
who proceeded alogos and askeptos."
However, Eudemus warned Galen that engaging in conflict with these
physicians could lead to his assassination. "Eudemus said this, and more
to the same effect; he added that if they were not able to harm me by
unscrupulous conduct they would proceed to attempts at poisoning. Among
other things he told me that, some ten years before, a young man had
come to the city and had given, like me practical demonstrations of the
resources of our art; this young man was put to death by poison,
together with two servants who accompanied him."
Garcia-Ballester says the following of Galen’s use of prognosis:
"In modern medicine, we are used to distinguishing between the
diagnostic judgment (the scientific knowledge of what a patient has) and
the prognostic judgment (the conjecture about what will happen to him.)
For Galen, to understand a clinical case technically, ‘to diagnose’,
was, among other things, to know with greater or lesser certainty the
outcome for the patient, ‘to prognosticate’. Prognosis, then, is one of
the essential problems and most important objectives of Galenic
diagnosis. Galen was concerned with distinguishing prognosis from
divination or prophecy, both to improve diagnosis technically and to
enhance the physician's reputation."
Death
The 11th-century
Suda
lexicon states that Galen died at the age of 70, which would place his
death in about the year 199. However, there is a reference in Galen's
treatise
"On Theriac to Piso" (which may, however, be spurious) to events of 204. There are also statements in Arabic sources
that he died in Sicily at age 87, after 17 years studying medicine and
70 practicing it, which would mean he died about 217. According to these
sources, the tomb of Galenus in
Palermo was still well preserved in tenth century. Nutton believes that
"On Theriac to Piso" is genuine, that the Arabic sources are correct, and that the
Suda
has erroneously interpreted the 70 years of Galen's career in the
Arabic tradition as referring to his whole lifespan. Boudon-Millot more or less concurs and favours a date of 216.
Contributions to medicine
Galen contributed a substantial amount to the Hippocratic understanding of pathology. Under
Hippocrates' bodily
humors theory, differences in human moods come as a consequence of imbalances in one of the four
bodily fluids: blood, yellow bile, black bile, and phlegm. Galen promoted this theory and the typology of
human temperaments.
In Galen's view, an imbalance of each humor corresponded with a
particular human temperament (blood—sanguine, black bile—melancholic,
yellow bile—choleric, and phlegm—phlegmatic). Thus, individuals with
sanguine temperaments are extroverted and social; choleric people have
energy, passion, and charisma; melancholics are creative, kind, and
considerate; and phlegmatic temperaments are characterized by
dependability, kindness, and affection.
Galen's principal interest was in human anatomy, but Roman law had
prohibited the dissection of human cadavers since about 150 BC. Because of this restriction, Galen performed anatomical dissections on living (
vivisection) and dead animals, mostly focusing on pigs and
primates.
This work was useful because Galen believed that the anatomical
structures of these animals closely mirrored those of humans. Galen
clarified the anatomy of the
trachea and was the first to demonstrate that the
larynx generates the voice. In one experiment, Galen used bellows to inflate the lungs of a dead animal.
Galen's work on the anatomy remained largely unsurpassed and
unchallenged up until the 16th century in Europe. In the middle of the
16th century, the anatomist
Andreas Vesalius
challenged the anatomical knowledge of Galen by conducting dissections
on human cadavers. These investigations allowed Vesalius to refute
aspects of Galen's anatomy.
Among Galen's major contributions to medicine was his work on the
circulatory system. He was the first to recognize that there are distinct differences between
venous (dark) and
arterial
(bright) blood. Although his anatomical experiments on animal models
led him to a more complete understanding of the circulatory system,
nervous system,
respiratory system, and other structures, his work contained scientific errors.
Galen believed the circulatory system to consist of two separate
one-way systems of distribution, rather than a single unified system of
circulation. He believed venous blood to be generated in the liver, from
where it was distributed and consumed by all organs of the body. He
posited that arterial blood originated in the heart, from where it was
distributed and consumed by all organs of the body. The blood was then
regenerated in either the liver or the heart, completing the cycle.
Galen also believed in the existence of a group of blood vessels he
called the
rete mirabile in the carotid sinus. Both of these theories of the circulation of blood were later (beginning with works of
Ibn al-Nafis published ca. 1242) shown to be incorrect.
Galen was a skilled surgeon, operating on human patients. Many of
his procedures and techniques would not be used again for centuries,
such as the procedures he performed on brains and eyes. To correct
cataracts
in patients, Galen performed an operation similar to a modern one.
Using a needle-shaped instrument, Galen attempted to remove the
cataract-affected lens of the eye. His surgical experiments included ligating the arteries of living animals.
Although many 20th century historians have claimed that Galen believed
the lens to be in the exact center of the eye, Galen actually
understood that the crystalline lens is located in the anterior aspect
of the human eye.
At first reluctantly but then with increasing vigour, Galen promoted Hippocratic teaching, including
venesection and
bloodletting, then unknown in Rome. This was sharply criticised by the
Erasistrateans, who predicted dire outcomes, believing that it was not blood but
pneuma that flowed in the veins. Galen, however, staunchly defended venesection in his three books on the subject and in his demonstrations and public disputations.
Contributions to philosophy
Although the main focus of his work was on medicine, anatomy, and
physiology, Galen also wrote about logic and philosophy. His writings
were influenced by earlier Greek and Roman thinkers, including
Plato,
Aristotle, and the
Stoics. Galen was concerned to combine philosophical thought with medical practice, as in his brief work
That the Best Physician is also a Philosopher
he took aspects from each group and combined them with his original
thought. He regarded medicine as an interdisciplinary field that was
best practiced by utilizing theory, observation, and experimentation in
conjunction.
Several schools of thought existed within the medical field
during Galen's lifetime, the main two being the Empiricists and
Rationalists (also called Dogmatists or Philosophers), with the
Methodists being a smaller group. The Empiricists emphasized the
importance of physical practice and experimentation, or "active
learning" in the medical discipline. In direct opposition to the
Empiricists were the Rationalists, who valued the study of established
teachings in order to create new theories in the name of medical
advancements. The Methodists formed somewhat of a middle ground, as they
were not as experimental as the Empiricists, nor as theoretical as the
Rationalists. The Methodists mainly utilized pure observation, showing
greater interest in studying the natural course of ailments than making
efforts to find remedies. Galen's education had exposed him to the five
major schools of thought (Platonists, Peripatetics, Stoics, Epicureans,
Pyrrhonists), with teachers from the Rationalist sect and from the
Empiricist sect.
Opposition to the Stoics
Galen
was well known for his advancements in medicine and the circulatory
system, but he was also concerned with philosophy. He developed his own
tripartite soul model following the examples of Plato; some scholars
refer to him as a Platonist.
Galen developed a theory of personality based on his understanding of
fluid circulation in humans, and he believed that there was a
physiological basis for mental disorders. Galen connected many of his theories to the
pneuma and he opposed the
Stoics' definition of and use of the pneuma.
The Stoics, according to Galen, failed to give a credible answer
for the localization of functions of the psyche, or the mind. Through
his use of medicine, he was convinced that he came up with a better
answer, the brain.
The Stoics only recognized the soul as having one part, which was the
rational soul and they claimed it would be found in the heart. Galen,
following Plato's idea, came up with two more parts to the soul.
Galen also rejected Stoic propositional logic and instead
embraced a hypothetical syllogistic which was strongly influenced by the
Peripatetics and based on elements of Aristotelian logic.
Localization of function
One of Galen's major works, On the Doctrines of Hippocrates and Plato,
sought to demonstrate the unity of the two subjects and their views.
Using their theories, combined with Aristotle's, Galen developed a
tripartite soul consisting of similar aspects.
He used the same terms as Plato, referring to the three parts as
rational, spiritual, and appetitive. Each corresponded to a localized
area of the body. The rational soul was in the brain, the spiritual soul
was in the heart, and the appetitive soul was in the liver. Galen was
the first scientist and philosopher to assign specific parts of the soul
to locations in the body because of his extensive background in
medicine. This idea is now referred to as localization of function. Galen's assignments were revolutionary for the time period, which set the precedent for future localization theories.
Galen believed each part of this tripartite soul controlled
specific functions within the body and that the soul, as a whole,
contributed to the health of the body, strengthening the "natural
functioning capacity of the organ or organs in question".
The rational soul controlled higher level cognitive functioning in an
organism, for example, making choices or perceiving the world and
sending those signals to the brain.
He also listed "imagination, memory, recollection, knowledge, thought,
consideration, voluntary motion and sensation" as being found within the
rational soul. The functions of "growing or being alive" resided in the spirited soul.
The spirited soul also contained our passions, such as anger. These
passions were considered to be even stronger than regular emotions, and,
as a consequence, more dangerous. The third part of the soul, or the appetitive spirit, controlled the living forces in our body, most importantly blood.
The appetitive spirit also regulated the pleasures of the body and was
moved by feelings of enjoyment. This third part of the soul is the
animalistic, or more natural, side of the soul; it deals with the
natural urges of the body and survival instincts. Galen proposed that
when the soul is moved by too much enjoyment, it reaches states of
"incontinence" and "licentiousness", the inability to willfully cease
enjoyment, which was a negative consequence of too much pleasure.
In order to unite his theories about the soul and how it operated within the body, he adapted the theory of the pneuma,
which he used to explain how the soul operated within its assigned
organs, and how those organs, in turn, interacted together. Galen then
distinguished the vital pneuma, in the arterial system, from the psychic
pneuma, in the brain and nervous system.
Galen placed the vital pneuma in the heart and the psychic pneuma
within the brain. He conducted many anatomical studies on animals, most
famously an ox, to study the transition from vital to psychic pneuma.
Although highly criticized for comparing animal anatomy to human
anatomy, Galen was convinced that his knowledge was abundant enough in
both anatomies to base one on the other.
Mind–body problem
Galen believed there to be no distinction between the mental and the physical.
This was a controversial argument of the time, and Galen fell with the
Greeks in believing that the mind and body were not separate faculties. He believed that this could be scientifically proven. This was where his opposition to the Stoics became most prevalent.
Galen proposed organs within the body to be responsible for specific
functions, rather than individual parts. According to Galen, the Stoics'
lack of scientific justification discredited their claims of the
separateness of mind and body, which is why he spoke so strongly against
them.
Psychotherapy
Another one of Galen's major works,
On the Diagnosis and Cure of the Soul's Passion, discussed how to approach and treat psychological problems. This was Galen's early attempt at what would later be called
psychotherapy.
His book contained directions on how to provide counsel to those with
psychological issues to prompt them to reveal their deepest passions and
secrets, and eventually cure them of their mental deficiency. The
leading individual, or therapist, had to be a male, preferably of an
older, wiser, age, as well as free from the control of the passions. These passions, according to Galen, caused the psychological problems that people experienced.
Published works
Galen may have produced more work than any author in antiquity, rivaling the quantity of work issued from
Augustine of Hippo. So profuse was Galen's output that the surviving texts represent nearly half of all the
extant literature from ancient Greece. It has been reported that Galen employed twenty
scribes to write down his words. Galen may have written as many as 500 treatises, amounting to some 10 million words. Although his surviving works amount to some 3 million words, this is thought to represent less than a third of his complete writings. In AD 191, a fire in the
Temple of Peace destroyed many of his works, in particular treatises on philosophy.
Because Galen's works were not translated into Latin in the
ancient period, and because of the collapse of the Roman Empire in the
West, the study of Galen, along with the Greek medical tradition as a
whole, went into decline in Western Europe during the
Early Middle Ages, when very few Latin scholars could read Greek. However, in general, Galen and the
ancient Greek medical tradition continued to be studied and followed in the
Eastern Roman Empire,
commonly known as the Byzantine Empire. All of the extant Greek
manuscripts of Galen were copied by Byzantine scholars. In the Abbasid
period (after AD 750)
Arab Muslims
began to be interested in Greek scientific and medical texts for the
first time, and had some of Galen's texts translated into Arabic, often
by Syrian Christian scholars (see below). As a result, some texts of
Galen exist only in Arabic translation,
while others exist only in medieval Latin translations of the Arabic.
In some cases scholars have even attempted to translate from the Latin
or Arabic back into Greek where the original is lost. For some of the ancient sources, such as
Herophilus, Galen's account of their work is all that survives.
Even in his own time, forgeries and unscrupulous editions of his work were a problem, prompting him to write
On his Own Books. Forgeries in Latin, Arabic or Greek continued until the
Renaissance.
Some of Galen's treatises have appeared under many different titles
over the years. Sources are often in obscure and difficult-to-access
journals or repositories. Although written in Greek, by convention the
works are referred to by Latin titles, and often by merely abbreviations
of those. No single authoritative collection of his work exists, and
controversy remains as to the authenticity of a number of works
attributed to Galen. As a consequence, research on Galen's work is
fraught with hazard.
Various attempts have been made to classify Galen's vast output.
For instance Coxe (1846) lists a Prolegomena, or introductory books,
followed by 7 classes of treatise embracing Physiology (28 vols.),
Hygiene (12), Aetiology (19), Semeiotics (14), Pharmacy (10), Blood
letting (4) and Therapeutics (17), in addition to 4 of aphorisms, and
spurious works. The most complete
compendium of Galen's writings, surpassing even modern projects like the
Corpus Medicorum Graecorum, is the one compiled and translated by
Karl Gottlob Kühn of
Leipzig between 1821 and 1833.
This collection consists of 122 of Galen's treatises, translated from
the original Greek into Latin (the text is presented in both languages).
Over 20,000 pages in length, it is divided into 22 volumes, with 676
index pages. Many of Galen's works are included in the
Thesaurus Linguae Graecae, a digital library of Greek literature started in 1972. Another useful modern source is the French
Bibliothèque interuniversitaire de médecine (BIUM).
Legacy
Late antiquity
In his time, Galen's reputation as both physician and philosopher was legendary,
the Emperor Marcus Aurelius describing him as "Primum sane medicorum
esse, philosophorum autem solum" (first among doctors and unique among
philosophers
Praen 14: 660). Other contemporary authors in the Greek world confirm this including
Theodotus the Shoemaker,
Athenaeus and
Alexander of Aphrodisias. The 7th-century poet
George of Pisida went so far as to refer to Christ as a second and neglected Galen.
Galen continued to exert an important influence over the theory and
practice of medicine until the mid-17th century in the Byzantine and
Arabic worlds and Europe. Hippocrates and Galen form important landmarks
of 600 years of Greek medicine. A. J. Brock describes them as
representing the foundation and apex respectively. A few centuries after Galen,
Palladius Iatrosophista stated, in his commentary on Hippocrates, that Hippocrates sowed and Galen reaped.
Thus Galen summarised and synthesised the work of his
predecessors, and it is in Galen's words (Galenism) that Greek medicine
was handed down to subsequent generations, such that Galenism became the
means by which Greek medicine was known to the world. Often, this was
in the form of restating and reinterpreting, such as in
Magnus of Nisibis' 4th-century work on urine, which was in turn translated into Arabic. Yet the full importance of his contributions was not appreciated till long after his death.
Galen's rhetoric and prolificity were so powerful as to convey the
impression that there was little left to learn. The term Galenism has
subsequently taken on both a positive and pejorative meaning as one that
transformed medicine in late antiquity yet so dominated subsequent
thinking as to stifle further progress.
After the collapse of the Western Empire the study of Galen and
other Greek works almost disappeared in the Latin West. In contrast, in
the predominantly Greek-speaking eastern half of the Roman empire
(Byzantium), many commentators of the subsequent centuries, such as
Oribasius, physician to the emperor
Julian who compiled a
Synopsis
in the 4th century, preserved and disseminated Galen's works, making
Galenism more accessible. Nutton refers to these authors as the "medical
refrigerators of antiquity".
In late antiquity, medical writing veered increasingly in the direction
of the theoretical at the expense of the practical, with many authors
merely debating Galenism. Magnus of Nisibis was a pure theorist, as were
John of Alexandria and Agnellus of Ravenna with their lectures on Galen's
De Sectis.
So strong was Galenism that other authors such as Hippocrates began to
be seen through a Galenic lens, while his opponents became marginalised
and other medical sects such as Asclepiadism slowly disappeared. Greek medicine was part of Greek culture, and Syrian Eastern Christians came in contact with it while the
Eastern Roman Empire
(Byzantium) ruled Syria and Western Mesopotamia, regions that were
conquered from Byzantium in the 7th century by Arab Muslims. After AD
750, Muslims had these Syrian Christians make the first translations of
Galen into Arabic. From then on, Galen and the Greek medical tradition
in general became assimilated into the medieval and early modern Islamic
Middle East.
Influence on medicine in the Islamic world
Galen's approach to medicine became and remains influential in the
Islamic world. The first major translator of Galen into Arabic was the
Arab Christian
Hunayn ibn Ishaq. He translated (c. 830–870) 129 works of "Jalinos" into
Arabic. Arabic sources, such as
Muhammad ibn Zakarīya al-Rāzi (AD 865–925), continue to be the source of discovery of new or relatively inaccessible Galenic writings. One of Hunayn's Arabic translations,
Kitab ila Aglooqan fi Shifa al Amrad, which is extant in the Library of
Ibn Sina Academy of Medieval Medicine & Sciences,
is regarded as a masterpiece of Galen's literary works. A part of the
Alexandrian compendium of Galen's work, this 10th-century manuscript
comprises two parts that include details regarding various types of
fevers (Humyat) and different inflammatory conditions of the body. More
important is that it includes details of more than 150 single and
compound formulations of both herbal and animal origin. The book
provides an insight into understanding the traditions and methods of
treatment in the Greek and Roman eras. In addition, this book provides a
direct source for the study of more than 150 single and compound drugs
used during the Greco-Roman period.
The influence of Galen's writings, including humorism, remains strong in modern
Unani medicine, now closely identified with Islamic culture, and widely practiced from India (where it is officially recognized) to Morocco.
Reintroduction to the Latin West

From the 11th century onwards,
Latin translations of Islamic medical texts began to appear in the West, alongside the
Salerno school of thought, and were soon incorporated into the curriculum at the universities of
Naples and
Montpellier.
From that time, Galenism took on a new, unquestioned authority, Galen
even being referred to as the "Medical Pope of the Middle Ages".
Constantine the African
was amongst those who translated both Hippocrates and Galen from
Arabic. In addition to the more numerous translations of Arabic texts in
this period, there were a few translations of Galenic works directly
from the Greek, such as
Burgundio of Pisa's translation of
De complexionibus.
Galen's works on anatomy and medicine became the mainstay of the
medieval physician's university curriculum, alongside Ibn Sina's
The Canon of Medicine,
which elaborated on Galen's works. Unlike pagan Rome, Christian Europe
did not exercise a universal prohibition of the dissection and autopsy
of the human body and such examinations were carried out regularly from
at least the 13th century.
However, Galen's influence was so great that when dissections
discovered anomalies compared with Galen's anatomy, the physicians often
tried to fit these into the Galenic system. An example of this is
Mondino de Liuzzi,
who describes rudimentary blood circulation in his writings but still
asserts that the left ventricle should contain air. Some cited these
changes as proof that human anatomy had changed since the time of Galen.
The most important translator of Galen's works into Latin was
Niccolò di Deoprepio da Reggio, who spent several years working on
Galen. Niccolò worked at the Angevin Court during the reign of king
Robert of Naples. Among Niccolò's translations is a piece from a medical treatise by Galen, of which the original text is lost.
Renaissance
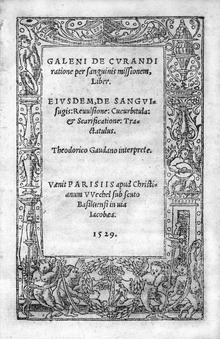
Galen's Opera omnia, dissection of a pig. Venice, 1565
The Renaissance, and the
fall of the Byzantine Empire
(1453), were accompanied by an influx of Greek scholars and manuscripts
to the West, allowing direct comparison between the Arabic commentaries
and the original Greek texts of Galen. This
New Learning and the
Humanist movement, particularly the work of
Linacre, promoted
literae humaniores including Galen in the Latin scientific canon,
De Naturalibus Facultatibus
appearing in London in 1523. Debates on medical science now had two
traditions, the more conservative Arabian and the liberal Greek. The more extreme liberal movements began to challenge the role of authority in medicine, as exemplified by
Paracelsus' symbolically burning the works of Avicenna and Galen at his medical school in
Basle.
Nevertheless, Galen's pre-eminence amongst the great thinkers of the
millennium is exemplified by a 16th-century mural in the refectory of
the
Great Lavra of
Mt Athos. It depicts pagan sages at the foot of the
Tree of Jesse, with Galen between the
Sibyl and
Aristotle.
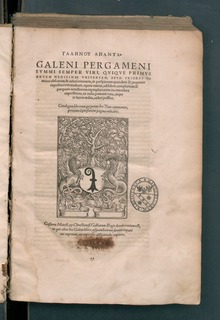
Galen.
De pulsibus. (Manuscript; Venice, c. 1550). This Greek manuscript of
Galen’s treatise on the pulse is interleaved with a Latin translation.
Galenism's final defeat came from a combination of the negativism of
Paracelsus and the constructivism of the Italian Renaissance anatomists,
such as
Vesalius in the 16th century.
In the 1530s, the Flemish anatomist and physician Andreas Vesalius took
on a project to translate many of Galen's Greek texts into Latin.
Vesalius' most famous work,
De humani corporis fabrica, was
greatly influenced by Galenic writing and form. Seeking to examine
critically Galen's methods and outlook, Vesalius turned to human cadaver
dissection as a means of verification. Galen's writings were shown by
Vesalius to describe details present in monkeys but not in humans, and
he demonstrated Galen's limitations through books and hands-on
demonstrations despite fierce opposition from orthodox pro-Galenists
such as
Jacobus Sylvius.
Since Galen states that he is using observations of monkeys (human
dissection was prohibited) to give an account of what the body looks
like, Vesalius could portray himself as using Galen's approach of
description of direct observation to create a record of the exact
details of the human body, since he worked in a time when human
dissection was allowed. Galen argued that monkey anatomy was close
enough to humans for physicians to learn anatomy with monkey dissections
and then make observations of similar structures in the wounds of their
patients, rather than trying to learn anatomy only from wounds in human
patients, as would be done by students trained in the Empiricist model. The examinations of Vesalius also disproved medical theories of
Aristotle and
Mondino de Liuzzi. One of the best known examples of Vesalius' overturning of Galenism was his demonstration that the
interventricular septum of the heart was not permeable, as Galen had taught (
Nat Fac III xv). However, this had been revealed two years before by Michael Servetus in his fateful "
Christianismi restitutio"
(1553) with only three copies of the book surviving, but these
remaining hidden for decades; the rest were burned shortly after its
publication because of persecution of Servetus by religious authorities.
Michael Servetus, using the name "Michel de Villeneuve" during his stay in France, was
Vesalius' fellow student and the best Galenist at the University of Paris, according to
Johann Winter von Andernach, who taught both. In the Galenism of the Renaissance, editions of the
Opera Omnia
by Galen were very important. It was begun in Venice in 1541–1542 by
the Guinta. There were fourteen editions of the book from that date
until 1625. Just one edition was produced from Lyon between 1548 and
1551. The Lyon edition has commentaries on breathing and blood streaming
that correct the work of earlier renowned authors such as
Vesalius,
Caius or
Janus Cornarius.
"Michel De Villeneuve" had contracts with Jean Frellon for that work,
and the Servetus scholar-researcher Francisco Javier González Echeverría presented research that became an accepted communication in the
International Society for the History of Medicine, which concluded that Michael De Villeneuve (
Michael Servetus) is the author of the commentaries of this edition of Frellon, in
Lyon.
Another convincing case where understanding of the body was
extended beyond where Galen had left it came from these demonstrations
of the nature of human circulation and the subsequent work of
Andrea Cesalpino,
Fabricio of Acquapendente and
William Harvey. Some Galenic teaching, such as his emphasis on
bloodletting as a remedy for many ailments, however, remained influential until well into the 19th century.
Contemporary scholarship
Copies of his works translated by Robert M. Green are held at the National Library of Medicine in Bethesda, Maryland.