| Rheumatic fever | |
|---|---|
| Other names | Acute rheumatic fever (ARF) |
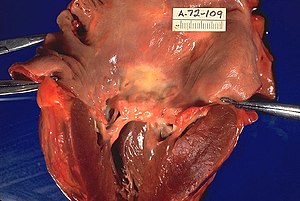 | |
| Rheumatic heart disease at autopsy with characteristic findings (thickened mitral valve, thickened chordae tendineae, hypertrophied left ventricular myocardium). | |
| Specialty | Cardiology |
| Symptoms | Fever, multiple painful joints, involuntary muscle movements, erythema marginatum |
| Complications | Rheumatic heart disease, heart failure, atrial fibrillation, infection of the valves |
| Usual onset | 2–4 weeks after a streptococcal throat infection, age 5-14 years |
| Causes | Autoimmune disease triggered by Streptococcus pyogenes |
| Risk factors | Genetics, malnutrition, poverty |
| Diagnostic method | Based on symptoms and infection history |
| Prevention | Antibiotics for strep throat, improved sanitation |
| Treatment | Prolonged periods of antibiotics, valve replacement surgery, valve repair |
| Frequency | 325,000 children a year |
| Deaths | 319,400 (2015) |
Rheumatic fever (RF) is an inflammatory disease that can involve the heart, joints, skin, and brain. The disease typically develops two to four weeks after a streptococcal throat infection. Signs and symptoms include fever, multiple painful joints, involuntary muscle movements, and occasionally a characteristic non-itchy rash known as erythema marginatum. The heart is involved in about half of the cases. Damage to the heart valves, known as rheumatic heart disease (RHD), usually occurs after repeated attacks but can sometimes occur after one. The damaged valves may result in heart failure, atrial fibrillation and infection of the valves.
Rheumatic fever may occur following an infection of the throat by the bacterium Streptococcus pyogenes. If the infection is left untreated, rheumatic fever occurs in up to three percent of people. The underlying mechanism is believed to involve the production of antibodies against a person's own tissues. Due to their genetics, some people are more likely to get the disease when exposed to the bacteria than others. Other risk factors include malnutrition and poverty. Diagnosis of RF is often based on the presence of signs and symptoms in combination with evidence of a recent streptococcal infection.
Treating people who have strep throat with antibiotics, such as penicillin, decreases the risk of developing rheumatic fever. In order to avoid antibiotic misuse this often involves testing people with sore throats for the infection; however, testing might not be available in the developing world. Other preventive measures include improved sanitation. In those with rheumatic fever and rheumatic heart disease, prolonged periods of antibiotics are sometimes recommended. Gradual return to normal activities may occur following an attack. Once RHD develops, treatment is more difficult.
Occasionally valve replacement surgery or valve repair is required.
Otherwise complications are treated as per normal.
Rheumatic fever occurs in about 325,000 children each year and about 33.4 million people currently have rheumatic heart disease. Those who develop RF are most often between the ages of 5 and 14, with 20% of first-time attacks occurring in adults. The disease is most common in the developing world and among indigenous peoples in the developed world. In 2015 it resulted in 319,400 deaths down from 374,000 deaths in 1990. Most deaths occur in the developing world where as many as 12.5% of people affected may die each year. Descriptions of the condition are believed to date back to at least the 5th century BCE in the writings of Hippocrates. The disease is so named because its symptoms are similar to those of some rheumatic disorders.
Signs and symptoms
A culture positive case of streptococcal pharyngitis with typical tonsillar exudate in a 16-year-old.
The disease typically develops two to four weeks after a throat infection. Symptoms include: fever, painful joints with those joints affected changing with time, involuntary muscle movements, and occasionally a characteristic non-itchy rash known as erythema marginatum.
The heart is involved in about half of the cases. Damage to the heart
valves usually occurs only after multiple attacks but may occasionally
occur after a single case of RF. The damaged valves may result in heart failure and also increase the risk of atrial fibrillation and infection of the valves.
Pathophysiology
Rheumatic fever is a systemic disease affecting the connective tissue around arterioles, and can occur after an untreated strep throat infection, specifically due to group A streptococcus (GAS), Streptococcus pyogenes. It is believed to be caused by antibody cross-reactivity. This cross-reactivity is a type II hypersensitivity reaction and is termed molecular mimicry. Usually, self reactive B cells remain anergic in the periphery without T cell co-stimulation. During a streptococcal infection, mature antigen-presenting cells such as B cells present the bacterial antigen to CD4+T cells which differentiate into helper T2 cells. Helper T2 cells subsequently activate the B cells to become plasma cells
and induce the production of antibodies against the cell wall of
Streptococcus. However the antibodies may also react against the
myocardium and joints, producing the symptoms of rheumatic fever. S. pyogenes is a species of aerobic, cocci, gram-positive bacteria that are non-motile, non-spore forming, and forms chains and large colonies.
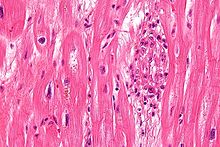
S. pyogenes has a cell wall composed of branched polymers which sometimes contain M protein, a virulence factor that is highly antigenic. The antibodies which the immune system generates against the M protein may cross-react with heart muscle cell protein myosin, heart muscle glycogen and smooth muscle cells of arteries, inducing cytokine release and tissue destruction. However, the only proven cross-reaction is with perivascular connective tissue. This inflammation occurs through direct attachment of complement and Fc receptor-mediated recruitment of neutrophils and macrophages. Characteristic Aschoff bodies, composed of swollen eosinophilic collagen surrounded by lymphocytes and macrophages can be seen on light microscopy. The larger macrophages may become Anitschkow cells or Aschoff giant cells. Rheumatic valvular lesions may also involve a cell-mediated immunity reaction as these lesions predominantly contain T-helper cells and macrophages.
In rheumatic fever, these lesions can be found in any layer of the heart causing different types of carditis. The inflammation may cause a serofibrinous pericardial exudate described as "bread-and-butter" pericarditis, which usually resolves without sequelae. Involvement of the endocardium typically results in fibrinoid necrosis and wart
formation along the lines of closure of the left-sided heart valves.
Warty projections arise from the deposition, while subendocardial
lesions may induce irregular thickenings called MacCallum plaques.
Rheumatic heart disease
Pathophysiology of rheumatic heart disease
Chronic rheumatic heart disease (RHD) is characterized by repeated
inflammation with fibrinous repair. The cardinal anatomic changes of
the valve include leaflet thickening, commissural fusion, and shortening
and thickening of the tendinous cords. It is caused by an autoimmune reaction to Group A β-hemolytic streptococci (GAS) that results in valvular damage. Fibrosis and scarring of valve leaflets, commissures and cusps leads to abnormalities that can result in valve stenosis or regurgitation.
The inflammation caused by rheumatic fever, usually during childhood,
is referred to as rheumatic valvulitis. About half of patients with
rheumatic fever develop inflammation involving valvular endothelium.
The majority of morbidity and mortality associated with rheumatic fever
is caused by its destructive effects on cardiac valve tissue. The pathogenesis of RHD is complex and not fully understood, but it is known to involve molecular mimicry and genetic predisposition that lead to autoimmune reactions.
Molecular mimicry occurs when epitopes are shared between host antigens and Streptococcus antigens.
This causes an autoimmune reaction against native tissues in the heart
that are incorrectly recognized as "foreign" due to the cross-reactivity
of antibodies generated as a result of epitope sharing. The valvular
endothelium is a prominent site of lymphocyte-induced damage. CD4+ T cells are the major effectors of heart tissue autoimmune reactions in RHD.
Normally, T cell activation is triggered by the presentation of
bacterial antigens. In RHD, molecular mimicry results in incorrect T
cell activation, and these T lymphocytes can go on to activate B cells,
which will begin to produce self-antigen-specific antibodies. This
leads to an immune response attack mounted against tissues in the heart
that have been misidentified as pathogens. Rheumatic valves display
increased expression of VCAM-1, a protein that mediates the adhesion of lymphocytes.
Self-antigen-specific antibodies generated via molecular mimicry
between human proteins and streptococcal antigens up-regulate VCAM-1
after binding to the valvular endothelium. This leads to the
inflammation and valve scarring observed in rheumatic valvulitis, mainly
due to CD4+ T cell infiltration.
While the mechanisms of genetic predisposition remain unclear, a
few genetic factors have been found to increase susceptibility to
autoimmune reactions in RHD. The dominant contributors are a component
of MHC class II molecules, found on lymphocytes and antigen-presenting cells, specifically the DR and DQ alleles on human chromosome 6. Certain allele combinations appear to increase RHD autoimmune susceptibility. Human leukocyte antigen (HLA) class II allele DR7 (HLA-DR7)
is most often associated with RHD, and its combination with certain DQ
alleles is seemingly associated with the development of valvular
lesions.
The mechanism by which MHC class II molecules increase a host's
susceptibility to autoimmune reactions in RHD is unknown, but it is
likely related to the role HLA molecules play in presenting antigens to T
cell receptors, thus triggering an immune response. Also found on
human chromosome 6 is the cytokine TNF-α which is also associated with RHD. High expression levels of TNF-α may exacerbate valvular tissue inflammation, contributing to RHD pathogenesis. Mannose-binding lectin
(MBL) is an inflammatory protein involved in pathogen recognition.
Different variants of MBL2 gene regions are associated in RHD.
RHD-induced mitral valve stenosis has been associated with MBL2 alleles encoding for high production of MBL.
Aortic valve regurgitation in RHD patients has been associated with
different MBL2 alleles that encode for low production of MBL. Other genes are also being investigated to better understand the complexity of autoimmune reactions that occur in RHD.
Diagnosis
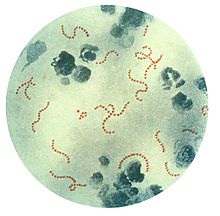
Streptococcus pyogenes bacteria (Pappenheim's stain) the trigger for rheumatic fever.
Modified Jones criteria were first published in 1944 by T. Duckett Jones, MD. They have been periodically revised by the American Heart Association in collaboration with other groups.
According to revised Jones criteria, the diagnosis of rheumatic fever
can be made when two of the major criteria, or one major criterion plus
two minor criteria, are present along with evidence of streptococcal
infection: elevated or rising antistreptolysin O titre or DNAase. Exceptions are chorea and indolent carditis, each of which by itself can indicate rheumatic fever. An April 2013 review article in the Indian Journal of Medical Research
stated that echocardiographic and Doppler (E & D) studies, despite
some reservations about their utility, have identified a massive burden
of rheumatic heart disease, which suggests the inadequacy of the 1992
Jones' criteria. E & D studies have identified subclinical carditis
in patients with rheumatic fever, as well as in follow-ups of rheumatic
heart disease patients who initially presented as having isolated cases
of Sydenham's chorea. Signs of a preceding streptococcal infection include: recent scarlet fever, raised antistreptolysin O or other streptococcal antibody titre, or positive throat culture.
Major criteria
- Polyarthritis: A temporary migrating inflammation of the large joints, usually starting in the legs and migrating upwards.
- Carditis: Inflammation of the heart muscle (myocarditis) which can manifest as congestive heart failure with shortness of breath, pericarditis with a rub, or a new heart murmur.
- Subcutaneous nodules: Painless, firm collections of collagen fibers over bones or tendons. They commonly appear on the back of the wrist, the outside elbow, and the front of the knees.
- Erythema marginatum: A long-lasting reddish rash that begins on the trunk or arms as macules, which spread outward and clear in the middle to form rings, which continue to spread and coalesce with other rings, ultimately taking on a snake-like appearance. This rash typically spares the face and is made worse with heat.
- Sydenham's chorea (St. Vitus' dance): A characteristic series of involuntary rapid movements of the face and arms. This can occur very late in the disease for at least three months from onset of infection.
Minor criteria
- Fever of 38.2–38.9 °C (100.8–102.0 °F)
- Arthralgia: Joint pain without swelling (Cannot be included if polyarthritis is present as a major symptom)
- Raised erythrocyte sedimentation rate or C reactive protein
- Leukocytosis
- ECG showing features of heart block, such as a prolonged PR interval (Cannot be included if carditis is present as a major symptom)
- Previous episode of rheumatic fever or inactive heart disease
Prevention
Rheumatic fever can be prevented by effectively and promptly treating strep throat with antibiotics.
In those who have previously had rheumatic fever, antibiotics in a preventative manner are occasionally recommended. As of 2017 the evidence to support long term antibiotics in those with underlying disease is poor.
The American Heart Association suggests that dental health be maintained, and that people with a history of bacterial endocarditis,
a heart transplant, artificial heart valves, or "some types of
congenital heart defects" may wish to consider long-term antibiotic
prophylaxis.
Treatment
The management of rheumatic fever is directed toward the reduction of inflammation with anti-inflammatory medications such as aspirin or corticosteroids. Individuals with positive cultures for strep throat should also be treated with antibiotics.
Aspirin is the drug of choice and should be given at high doses.
One should watch for side effects like gastritis and salicylate poisoning. In children and teenagers, the use of aspirin and aspirin-containing products can be associated with Reye's syndrome,
a serious and potentially deadly condition. The risks, benefits, and
alternative treatments must always be considered when administering
aspirin and aspirin-containing products in children and teenagers.
Ibuprofen for pain and discomfort and corticosteroids for moderate to
severe inflammatory reactions manifested by rheumatic fever should be
considered in children and teenagers.
Vaccine
No vaccines are currently available to protect against S. pyogenes infection, although research is underway to develop one. Difficulties in developing a vaccine include the wide variety of strains of S. pyogenes
present in the environment and the large amount of time and people that
will be needed for appropriate trials for safety and efficacy of the
vaccine.
Infection
People with positive cultures for Streptococcus pyogenes should be treated with penicillin as long as allergy is not present. The use of antibiotics will not alter cardiac involvement in the development of rheumatic fever. Some suggest the use of benzathine benzylpenicillin.
Monthly injections of long-acting penicillin must be given for a
period of five years in patients having one attack of rheumatic fever.
If there is evidence of carditis, the length of therapy may be up to 40
years.
Another important cornerstone in treating rheumatic fever includes the
continual use of low-dose antibiotics (such as penicillin, sulfadiazine, or erythromycin) to prevent recurrence.
Inflammation
While corticosteroids are often used, evidence to support this is poor. Salicylates are useful for pain.
Steroids are reserved for cases where there is evidence of an
involvement of the heart. The use of steroids may prevent further
scarring of tissue and may prevent the development of sequelae such as
mitral stenosis.
Heart failure
Some patients develop significant carditis which manifests as congestive heart failure. This requires the usual treatment for heart failure: ACE inhibitors, diuretics, beta blockers, and digoxin. Unlike typical heart failure, rheumatic heart failure responds well to corticosteroids.
Epidemiology
Deaths from rheumatic heart disease per million persons in 2012
0–7
8–14
15–20
21–25
26–32
33–38
39–45
46–52
53–63
64–250
Disability-adjusted life year for rheumatic heart disease per 100,000 inhabitants in 2004.
no data
less than 20
20–40
40–60
60–80
80–100
100–120
120–140
140–160
160–180
180–200
200–330
more than 330
About 33 million people are affected by rheumatic heart disease with an additional 47 million having asymptomatic damage to their heart valves. As of 2010 globally it resulted in 345,000 deaths, down from 463,000 in 1990.
In Western countries, rheumatic fever has become fairly rare
since the 1960s, probably due to the widespread use of antibiotics to
treat streptococcus infections. While it has been far less common in the United States since the beginning of the 20th century, there have been a few outbreaks since the 1980s. The disease is most common among Indigenous Australians (particularly in central and northern Australia), Māori, and Pacific Islanders, and is also common in Sub-Saharan Africa, Latin America, the Indian Subcontinent, the Middle East, and North Africa.
Rheumatic fever primarily affects children between ages 5 and 17
years and occurs approximately 20 days after strep throat. In up to a
third of cases, the underlying strep infection may not have caused any
symptoms.
The rate of development of rheumatic fever in individuals with
untreated strep infection is estimated to be 3%. The incidence of
recurrence with a subsequent untreated infection is substantially
greater (about 50%).
The rate of development is far lower in individuals who have received
antibiotic treatment. Persons who have suffered a case of rheumatic
fever have a tendency to develop flare-ups with repeated strep
infections.
The recurrence of rheumatic fever is relatively common in the
absence of maintenance of low dose antibiotics, especially during the
first three to five years after the first episode. Recurrent bouts of
rheumatic fever can lead to valvular heart disease.
Heart complications may be long-term and severe, particularly if valves
are involved. In countries in Southeast-Asia, sub-saharan Africa, and
Oceania, the percentage of people with rheumatic heart disease detected
by listening to the heart was 2.9 per 1000 children and by
echocardiography it was 12.9 per 1000 children.