| Autism therapies | |
|---|---|

A
three-year-old with autism points to fish in an aquarium, as part of an
experiment on the effect of intensive shared-attention training on
language development.
|
Autism therapies are interventions that attempt to lessen the deficits and problem behaviours associated with autism spectrum disorder (ASD) in order to increase the quality of life and functional independence of individuals with autism. Treatment is typically catered to the person's needs. Treatments fall into two major categories: educational interventions and medical management. Training and support are also given to families of those with ASD.
Studies of interventions have some methodological problems that prevent definitive conclusions about efficacy. Although many psychosocial interventions have some positive evidence, suggesting that some form of treatment is preferable to no treatment, the systematic reviews have reported that the quality of these studies has generally been poor, their clinical results are mostly tentative, and there is little evidence for the relative effectiveness of treatment options. Intensive, sustained special education programs and behavior therapy early in life can help children with ASD acquire self-care, social, and job skills, and often can improve functioning, and decrease symptom severity and maladaptive behaviors; claims that intervention by around age three years is crucial are not substantiated. Although, new research shows that Children who receive intervention can lose their diagnosis and be indistinguishable from their typically developing peers. The earlier the intervention the more likely this to occur. Available approaches include applied behavior analysis (ABA), developmental models, structured teaching, speech and language therapy, social skills therapy, and occupational therapy. Educational interventions have some effectiveness in children: intensive ABA treatment has demonstrated effectiveness in enhancing global functioning in preschool children, and is well established for improving intellectual performance of young children. Neuropsychological reports are often poorly communicated to educators, resulting in a gap between what a report recommends and what education is provided. The limited research on the effectiveness of adult residential programs shows mixed results.
Many medications are used to treat problems associated with ASD. More than half of U.S. children diagnosed with ASD are prescribed psychoactive drugs or anticonvulsants, with the most common drug classes being antidepressants, stimulants, and antipsychotics. Aside from antipsychotics, there is scant reliable research about the effectiveness or safety of drug treatments for adolescents and adults with ASD. A person with ASD may respond atypically to medications, the medications can have adverse effects, and no known medication relieves autism's core symptoms of social and communication impairments.
Some newer treatments are geared towards children with ASD and focus on community-based education and living, and early intervention. The treatments that may have the most benefit focus on early behavioral development and have shown significant improvements in communication and language. These treatments include parental involvement as well as special educational methods. Further research will examine the long term outcome of these treatments and the details surrounding the process and execution of them.
Many alternative therapies and interventions are available, ranging from elimination diets to chelation therapy. Few are supported by scientific studies. Treatment approaches lack empirical support in quality-of-life contexts, and many programs focus on success measures that lack predictive validity and real-world relevance. Scientific evidence appears to matter less to service providers than program marketing, training availability, and parent requests. Even if they do not help, conservative treatments such as changes in diet are expected to be harmless aside from their bother and cost. Dubious invasive treatments are a much more serious matter: for example, in 2005, botched chelation therapy killed a five-year-old boy with autism.
Treatment is expensive; indirect costs are more so. For someone born in 2000, a U.S. study estimated an average discounted lifetime cost of $4.39 million (2020 dollars, inflation-adjusted from 2003 estimate), with about 10% medical care, 30% extra education and other care, and 60% lost economic productivity. A UK study estimated discounted lifetime costs at £1.8 million and £1.16 million for an autistic person with and without intellectual disability, respectively (2020 pounds, inflation-adjusted from 2005/06 estimate). Legal rights to treatment are complex, vary with location and age, and require advocacy by caregivers. Publicly supported programs are often inadequate or inappropriate for a given child, and unreimbursed out-of-pocket medical or therapy expenses are associated with likelihood of family financial problems; one 2008 U.S. study found a 14% average loss of annual income in families of children with ASD, and a related study found that ASD is associated with higher probability that child care problems will greatly affect parental employment. After childhood, key treatment issues include residential care, job training and placement, sexuality, social skills, and estate planning.
Educational interventions
Educational interventions attempt to help children not only to learn
academic subjects and gain traditional readiness skills, but also to
improve functional communication and spontaneity, enhance social skills
such as joint attention,
gain cognitive skills such as symbolic play, reduce disruptive
behavior, and generalize learned skills by applying them to new
situations. Several model programs have been developed, which in
practice often overlap and share many features, including:
- early intervention that does not wait for a definitive diagnosis;
- intense intervention, at least 25 hours per week, 12 months per year;
- low student/teacher ratio;
- family involvement, including training of parents;
- interaction with neurotypical peers;
- social stories, ABA and other visually based training;
- structure that includes predictable routine and clear physical boundaries to lessen distraction; and
- ongoing measurement of a systematically planned intervention, resulting in adjustments as needed.
Several educational intervention methods are available, as discussed
below. They can take place at home, at school, or at a center devoted to
autism treatment; they can be done by parents, teachers, speech and language therapists, and occupational therapists. A 2007 study found that augmenting a center-based program with weekly home visits by a special education teacher improved cognitive development and behavior.
Studies of interventions have methodological problems that prevent definitive conclusions about efficacy. Although many psychosocial
interventions have some positive evidence, suggesting that some form of
treatment is preferable to no treatment, the methodological quality of systematic reviews
of these studies has generally been poor, their clinical results are
mostly tentative, and there is little evidence for the relative
effectiveness of treatment options.
Concerns about outcome measures, such as their inconsistent use, most
greatly affect how the results of scientific studies are interpreted.
A 2009 Minnesota study found that parents follow behavioral treatment
recommendations significantly less often than they follow medical
recommendations, and that they adhere more often to reinforcement than
to punishment recommendations.
Intensive, sustained special education programs and behavior therapy
early in life can help children acquire self-care, social, and job
skills, and often improve functioning and decrease symptom severity and maladaptive behaviors; claims that intervention by around age three years is crucial are not substantiated.
Applied behavior analysis
Applied behavior analysis (ABA) is the applied research field of the science of behavior analysis, and it underpins a wide range of techniques used to treat autism and many other behaviors and diagnoses, including those who are patients in rehab or in whom a behavior change is desired
. ABA-based interventions focus on teaching tasks one-on-one using the behaviorist principles of stimulus, response and reward, and on reliable measurement and objective evaluation of observed behavior. Applied Behavior Analysis is the only empirically proven method of treatment. There is wide variation in the professional practice of behavior analysis and among the assessments and interventions used in school-based ABA programs.
Conversely, various major figures within the autistic community
have written biographies detailing the harm caused by the provision of
ABA, including restraint, sometimes used with mild self stimulatory
behaviors such as hand flapping, and verbal abuse. The Autistic Self Advocacy Network campaigns against the use of ABA in autism
- punishment procedures are very rarely used within the field today.
These procedures were once used in the 70s and 80s however now there are
ethical guidelines in place to prohibit the use.
Discrete trial training
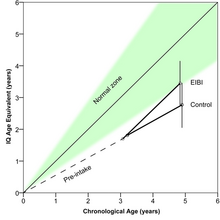
Developmental
trajectories (as measured with IQ-tests) of children with autism
receiving either early and intensive behavioral intervention (n=195) or
control treatment (n = 135)
Many intensive behavioral interventions rely heavily on discrete
trial teaching (DTT) methods, which use stimulus-response-reward
techniques to teach foundational skills such as attention, compliance,
and imitation. However, children have problems using DTT-taught skills in natural environments.
These students are also taught with naturalistic teaching procedures to
help generalize these skills. In functional assessment, a common
technique, a teacher formulates a clear description of a problem
behavior, identifies antecedents, consequences, and other environmental
factors that influence and maintain the behavior, develops hypotheses
about what occasions and maintains the behavior, and collects
observations to support the hypotheses. A few more-comprehensive ABA programs use multiple assessment and intervention methods individually and dynamically.
ABA-based techniques have demonstrated effectiveness in several
controlled studies: children have been shown to make sustained gains in
academic performance, adaptive behavior, and language, with outcomes significantly better than control groups.
A 2009 review of educational interventions for children, whose mean age
was six years or less at intake, found that the higher-quality studies
all assessed ABA, that ABA is well-established and no other educational
treatment is considered probably efficacious, and that intensive ABA
treatment, carried out by trained therapists, is demonstrated effective
in enhancing global functioning in pre-school children. These gains maybe complicated by initial IQ.
A 2008 evidence-based review of comprehensive treatment approaches
found that ABA is well established for improving intellectual
performance of young children with ASD.
A 2009 comprehensive synthesis of early intensive behavioral
intervention (EIBI), a form of ABA treatment, found that EIBI produces
strong effects, suggesting that it can be effective for some children
with autism; it also found that the large effects might be an artifact
of comparison groups with treatments that have yet to be empirically
validated, and that no comparisons between EIBI and other widely
recognized treatment programs have been published.
A 2009 systematic review came to the same principal conclusion that
EIBI is effective for some but not all children, with wide variability
in response to treatment; it also suggested that any gains are likely to
be greatest in the first year of intervention. A 2009 meta-analysis concluded that EIBI has a large effect on full-scale intelligence and a moderate effect on adaptive behavior.
However, a 2009 systematic review and meta-analysis found that applied
behavior intervention (ABI), another name for EIBI, did not
significantly improve outcomes compared with standard care of preschool
children with ASD in the areas of cognitive outcome, expressive
language, receptive language, and adaptive behavior.
Applied behavior analysis is cost effective for administrators.
Recently behavior analysts have built comprehensive models of child development to generate models for prevention as well as treatment for autism.
Pivotal response training
Pivotal response treatment (PRT) is a naturalistic intervention
derived from ABA principles. Instead of individual behaviors, it targets
pivotal areas of a child's development, such as motivation,
responsivity to multiple cues, self-management, and social initiations;
it aims for widespread improvements in areas that are not specifically
targeted. The child determines activities and objects that will be used
in a PRT exchange. Intended attempts at the target behavior are rewarded
with a natural reinforcer: for example, if a child attempts a request
for a stuffed animal, the child receives the animal, not a piece of
candy or other unrelated reinforcer.
Aversive therapy
The Judge Rotenberg Educational Center uses aversion therapy, notably contingent shock (electric shock
delivered to the skin for a few seconds), to control the behavior of
its patients, many of whom are autistic. The practice is controversial and has not been popular or used elsewhere since the 1990s.
Communication interventions
The inability to communicate, verbally or non-verbally, is a core
deficit in autism. Children with autism are often engaged in repetitive
activity or other behaviors because they cannot convey their intent any
other way. They do not know how to communicate their ideas to caregivers
or others. Helping a child with autism learn to communicate their needs
and ideas is absolutely core to any intervention. Communication can
either be verbal or non-verbal. Children with autism require intensive
intervention to learn how to communicate their intent.
Communication interventions fall into two major categories.
First, many autistic children do not speak, or have little speech, or
have difficulties in effective use of language. Social skills have been shown to be effective in treating children with autism.
Interventions that attempt to improve communication are commonly
conducted by speech and language therapists, and work on joint
attention, communicative intent, and alternative or augmentative and alternative communication (AAC) methods such as visual methods, for example visual schedules. AAC methods do not appear to impede speech and may result in modest gains. A 2006 study reported benefits both for joint attention intervention and for symbolic play intervention,
and a 2007 study found that joint attention intervention is more likely
than symbolic play intervention to cause children to engage later in
shared interactions.
Second, social skills treatment attempts to increase social and
communicative skills of autistic individuals, addressing a core deficit
of autism. A wide range of intervention approaches is available,
including modeling and reinforcement, adult and peer mediation
strategies, peer tutoring, social games and stories, self-management, pivotal response therapy, video modeling, direct instruction, visual cuing, Circle of Friends and social-skills groups.
A 2007 meta-analysis of 55 studies of school-based social skills
intervention found that they were minimally effective for children and
adolescents with ASD, and a 2007 review found that social skills training has minimal empirical support for children with Asperger syndrome or high-functioning autism.
SCERTS
The SCERTS model
is an educational model for working with children with autism spectrum
disorder (ASD). It was designed to help families, educators and
therapists work cooperatively together to maximize progress in
supporting the child.
The acronym refers to the focus on:
- SC – social communication – the development of functional communication and emotional expression.
- ER – emotional regulation – the development of well-regulated emotions and ability to cope with stress.
- TS – transactional support – the implementation of supports to help families, educators and therapists respond to children's needs, adapt the environment and provide tools to enhance learning.
The evidence base for the efficacy of the SCERTS Model Practice in
the SCERTS model is based on evidence from multiple sources. Efficacy of
implementation of practices in the SCERTS Model is supported by
empirical evidence from contemporary treatment research in ASD and
related disabilities. Currently, federally funded, large sample research
has been published and longitudinal studies continue that specifically
addresses the effectiveness of SCERTS as a comprehensive treatment
framework. The emphasis of current research is to demonstrate the
effectiveness of SCERTS for infants, toddlers and school age students in
home, school and community settings. This body of research is
summarized below. Second, it is rooted in research on child development
as well as research addressing the core challenges of ASD. Third, it
incorporates the documentation of meaningful change through the
collection of clinical and educational data, and programmatic decisions
are made based on objective measurement of change. Finally, given that
it is not an exclusive model, evidence-based practices (i.e., focused
intervention strategies) from other approaches are easily infused in a
program plan for an individual.
Empirical Research on the Efficacy of The SCERTS Model
In recent years a number of studies have been published that
highlight the efficacy of the SCERTS model. Two randomized controlled
trials have been published demonstrating the efficacy of the SCERTS
Model in the home and classroom settings. The first randomized trial
adapted the SCERTS framework for delivery within early intervention
settings (Wetherby et al., 2014). Specifically, this study examined the
effectiveness of the model when implemented by parents for toddlers with
autism within natural settings. Eighty-two autistic children aged 19
months (SD = 1.93 mos) participated in a 9-month longitudinal study with
their primary caregiver. Children were randomized into two groups – an
individual coaching format and a group coaching format, both focused on
teaching parents how to support active engagement within natural
contexts using the SCERTS framework. Individual coaching consisted of
in-home support from an interventionist 2-3 times weekly using a
collaborative coaching model to build parent capacity and independence
in implementation of supports within natural routines geared at
facilitating SC and ER development. Parents in this condition were
encouraged to deliver intervention by embedding evidence-based
strategies for their child’s SC and ER targets in everyday activities
for at least 25 hours. This is consistent with the SCERTS Model
recommendations. Results found individual coaching was more efficacious
than the group-based format. Outcomes for social communication,
receptive language, and adaptive behavior reached statistical
significance (Wetherby et al., 2014).
The efficacy of the SCERTS Model in classrooms was the focus of
another large longitudinal randomized control trial. Morgan et al.
(2018) conducted a cluster randomized controlled trial for 197 diverse
students with ASD in 129 classrooms across 66 schools in the US. Mean
age of the students was 6.76 years (SD = 1.05years). Classrooms were
randomly assigned to the Classroom SCERTS Intervention (CSI) or Autism
Training Modules (ATM) condition. Special education and general
education teachers assigned to the CSI condition in this study were
trained on the model and provided coaching throughout the school year.
ATM teachers engaged in usual school-based educational practices and had
access to online training resources related to autism treatment
practices. Notably, in this study active engagement was used as an
outcome measure and was measured by the Classroom Measure of Active
Engagement (CMAE; Morgan, Wetherby & Holland, 2010). Additional
outcome measures examining adaptive behavior, social skills, and ratings
of executive functioning were also used.
Results of Morgan et al. (2018) revealed that students in the CSI
condition showed statistically significant better outcomes on observed
measures of adaptive communication, social skills and executive
functioning than students within the ATM condition. These data
demonstrate the positive impact of SCERTS within a natural environment,
that is, the classroom setting, for a heterogeneous sample of students
with ASD (Morgan et al., 2018). This study was chosen by the
Interagency Autism Coordinating Committee in the US for their 2018
Summary of Advances in Autism Spectrum Disorder Research Report as a key
study addressing the question “Which treatments and interventions will
help?” In their review, the Committee highlighted that 70 percent of
teachers trained in CSI implemented with fidelity indicating scalability
of the model and also reflecting feasibility with teacher commitment to
the model. They also acknowledged that this is one of the largest
studies to measure the effect of school-based active engagement
intervention in children with ASD and that the results appear
generalizable to a diverse population (Interagency Autism Coordinating
Committee (IACC), 2019).
The prioritization of active engagement as a measure of
effectiveness for educational programs for students with ASD aligns with
work by Sparapani and colleagues (2015) that identifies the challenges
students diagnosed with autism face in terms of maintaining active
engagement and the resulting impact on learning and educational
outcomes. In fact, results suggest typically students with autism
actively engage less than half of the time in the classroom (Sparapani,
Morgan, Reinhardt, Schatschneider, & Wetherby, 2015). Consideration
of this finding in the context of additional research suggests that
increasing active engagement is critical to positive educational
outcomes in ASD and reveals a clear need for approaches such as SCERTS
that focus on active engagement (National Research Council, 2001).
The SCERTS Model has also been the object of international study.
A pilot study was implemented in Hong Kong examining the effectiveness
of the SCERTS® Model for children with ASD (Yu & Zhu, 2018). This
study examined the implementation of SCERTS® for 2 different durations
(5 months versus 10 months) for children with an average age of 53
months in preschool settings. Special education teachers, occupational
therapists, speech pathologists, and physiotherapists were recruited
from 10 special child care centers in Hong Kong. Participating
professionals received initial training and then were provided coaching
throughout the school year. Each participating special education teacher
taught 5-7 children. Results showed that participating children
improved significantly in their social communication and emotional
behavior after intervention.
The SCERTS Model has also been the subject of a multiple case
study design (O’Neill et al., 2010). Implementation of SCERTS in this
study followed a multi-disciplinary team training for the teams of four
pupils. All four pupils made progress in Joint Attention, Symbol Use,
Mutual Regulation, and Self-Regulation as well as in other measures of
receptive communication, expressive communication, play, and coping
skills. Qualitative methods were used to gain insights from the staff
related to their experiences in implementing SCERTS. Central findings
from the focus groups with the multidisciplinary team members revealed
increased understanding of emotional regulation as a developmental
construct, as well as increased clarity of team member roles in
supporting children when dysregulated.
Researchers in the United Kingdom (Molteni, Guldberg, &
Logan, 2013) also examined the feasibility of implementing SCERTS as an
ecologically valid model in an independent residential school. This
study aimed to understand how teams work together while learning to
implement the SCERTS Model. At the conclusion of the study, 89% of the
team members said they felt comfortable using SCERTS and 78% said the
framework improved teamwork in collaborating with colleagues.
Specifically, teams highlighted that the quality and accuracy of
assessment improved collaboration and understanding of students and
their environment.
Summary
The SCERTS Model meets criteria for evidence-based practice and
offers a framework to directly address the core challenges of ASD,
focusing on building an individual’s capacity to initiate communication
with a conventional symbolic system and to be actively engaged in
emotionally satisfying relationships based on effective reciprocal
communication. Emotional regulation goals focus on capacities to
regulate attention, arousal and emotional state to cope with everyday
stresses in life, and therefore, to be most available for learning and
engaging. Transactional supports are identified, developed and
implemented to support individuals of all ages in social engagement and
learning, to promote generalization of acquired abilities, and to
support their caregivers service providers. The model provides a
roadmap for individualized education and treatment based on a person’s
strengths and needs guided by research on child and human development.
The SCERTS Model was designed to motivate professionals and families to
focus their efforts on enhancing quality of life by addressing the core
challenges faced by autistic children, adults and their caregivers, and
therefore, to move the field to a new generation of more integrated,
comprehensive programs.
Disley, B. Weston, B., Kolandai-Matchett, K., Vermillion Peirce,
P. (2011). Evaluation of the use of the Social Communication, Emotional
Regulation and Transactional Support (SCERTS) Framework in New Zealand.
Prepared for: Warwick Phillips Professional Practice Unit, Special
Education Ministry of Education. Cognition Education Limited 2011. http://onlinelibrary.wiley.com/doi/10.1111/1467-8578.12030/abstract
Fukuzawa, Y. (2017). Enhancing the active engagement of students with
special needs through emotional regulation : The SCERTS Model in special
needs school. Study Report: Shizuoka University.
Harrison, P. (2015, May). Classroom-Based intervention improves core
autism deficits; summary of classroom SCERTS intervention (CSI) data
presented at IMFAR in May 2015; Medscape. Accessible via: http://www.medscape.com/viewarticle/844530
Molteni, P., Guldberg, K., and Logan, N. (2013). Autism and
multidisciplinary teamwork through the SCERTS Model, British Journal of
Special Education. DOI: 10.1111/1467-8578.12030. Accessible via: http://onlinelibrary.wiley.com/doi/10.1111/1467-8578.12030/abstract
Morgan L, Hooker JL, Sparapani N, et al., (2018) Cluster randomized
trial of the classroom SCERTS intervention for elementary students with
autism spectrum disorder. Journal of Consulting and Clinical Psychology.
J86(7):631-644.
O’Neill, J., Bergstrand, L., Bowman, K., Elliott, K., Mavin, L.,
Stephenson, S., Wayman, C. (2010). The SCERTS model: Implementation and
evaluation in a primary special school. Good Autism Practice (GAP),
11,1, 2010. Accessible on the Autism Education Trust website at: http://www.aettraininghubs.org.uk/wp-content/uploads/2012/05/31.1-ONeill-Evaluating-practice.pdf
Sparapani, N, Morgan, L., Reinhardt, V., Schatschneider, C., &
Wetherby, A.M. (2015). Evaluation of Classroom Active Engagement in
Elementary Students with Autism Spectrum Disorder. Journal of Autism and
Developmental Disorders,
Wetherby, A,M., Guthrie, W., Woods, J., Schatschneider, C., Holland, R.,
Morgan, L. & Lord, C. (2014). Parent-Implemented Social
Intervention for Toddlers With Autism: An RCT. Pediatrics
Yu, L., and Zhu, X. (2018). Effectiveness of a SCERTS Model-based
intervention for children with Autism Spectrum Disorder (ASD) in Hong
Kong: A pilot study, Journal of Autism and Developmental Disorders,
1-14.
Computer-assisted therapy for reasoning about communicative actions
Many
remediation strategies have not taken into account that people with
autism suffer from difficulties in learning social rules from examples.
Computer-assisted autism therapy has been proposed to teach not simply
via examples but to teach the rule along with it.
A reasoning rehabilitation strategy, based on playing with a computer
based mental simulator that is capable of modeling mental and emotional
states of the real world, has been subject to short-term and long-term
evaluations. The simulator performs the reasoning in the framework of belief-desire-intention model.
Learning starts from the basic concepts of knowledge and intention and
proceeds to more complex communicative actions such as explaining,
agreeing, and pretending.
Relationship based, developmental models
Relationship
based models give importance to the relationships that help children
reach and master early developmental milestones. These are often missed
or not mastered in children with ASD. Examples of these early milestones
are engagement and interest in the world, intimacy with a caregiver,
intentionality of action.
Relationship Development Intervention
Relationship development intervention
is a family-based treatment program for children with autism spectrum
disorder (ASD). This program is based on the belief that the development
of dynamic intelligence (the ability to think flexibly, take different
perspectives, cope with change and process information simultaneously)
is key to improving the quality of life of children with autism.
Floortime/DIR
The Floortime/DIR (Developmental, Individual Differences based,
Relationship based ) approach is a developmental intervention to autism
developed by Stanley Greenspan and Serena Weider. This approach is based on the idea that the core deficits in autism are individual differences in the sensory system, motor planning
problems, difficulties in communication and relation to others, and the
inability to connect ones desire to intentional action and
communication. When addressed through a combination of sensory support
and DIR/Floortime techniques, the facilitator is playfully obstructive
to redirect the child to play and relate to their therapist. The primary
goal of Floortime is to improve the child's cognitive, language, and
social abilities.
However, these claims should be regarded with some scepticism, owing to
a lack of independent scientific research into the efficacy of the
floortime approach.
The DIR model is based on the model of a developmental 'tree',
the central notion being that Autistic children have yet to master
certain early developmental milestones, or 'branches' of the tree, which
are as follows:
- Stage One: Regulation and Interest in the World: Being calm and feeling well enough to attend to a caregiver and surroundings. Have shared attention.
- Stage Two: Engagement and Relating: Interest in another person and in the world, developing a special bond with preferred caregivers. Distinguishing inanimate objects from people.
- Stage Three: Two way intentional communication: Simple back and forth interactions between child and caregiver. Smiles, tickles, anticipatory play.
- Stage Four: Social Problem solving: Using gestures, interaction, babble to indicate needs, wants, pleasure, upset. Get a caregiver to help with a problem. Using pre-language skills to show intention.
- Stage Five: Symbolic Play: Using words, pictures, symbols to communicate an intention, idea. Communicate ideas and thoughts, not just wants and needs.
- Stage Six: Bridging Ideas: This stage is the foundation of logic, reasoning, emotional thinking and a sense of reality.
Exponents of the floortime approach argue that children with ASD
struggle with or have missed some of these vital developmental stages.
An introduction to DIR/Floortime can be found in the book - Engaging
Autism: Using the Floortime Approach to Help Children Relate,
Communicate, and Think, by Stanley Greenspan, M.D. and Serena Wieder, PhD.
The PLAY Project
The PLAY Project (an acronym for PLAY and Language for Autistic Youngsters) is a community-based, national autism training and early childhood intervention program established in 2001 by Richard Solomon. Based on the DIR (Developmental, Individualized, Relationship-based) theory of Stanley Greenspan MD,
the program is designed to train parents and professionals to implement
intensive, developmental interventions for young children (18 months to
6 years) with autism. The program is operating in nearly 100 agencies
worldwide including 25 states and in 5 countries outside of the U.S.
(Australia, Canada, England, Ireland, Switzerland, the Netherlands, and
China). The PLAY Project has been operating since 2001 from its headquarters in Ann Arbor, MI.
Some preliminary research on the program was published by the peer-reviewed British journal, Autism (May, 2007).
Son-Rise
Son-Rise is a home-based program that emphasizes on implementing a
color- and sensory-free playroom. Before implementing the home-based
program, an institute trains the parents how to accept their child
without judgment through a series of dialogue sessions. Like Floortime,
parents join their child's ritualistic behavior for
relationship-building. To gain the child's "willing engagement", the
facilitator continues to join them only this time through parallel play.
Proponents claim that children will become non-autistic after parents
accept them for who they are and engage them in play. The program was
started by the parents of Raun Kaufman, who is claimed to have gone from being autistic to normal via the treatment in the early 1970s.
No independent study has tested the efficacy of the program, but a 2003
study found that involvement with the program led to more drawbacks
than benefits for the involved families over time,
and a 2006 study found that the program is not always implemented as it
is typically described in the literature, which suggests it will be
difficult to evaluate its efficacy.
TEACCH
Treatment and Education of Autistic and Related Communication
Handicapped Children (TEACCH), which has come to be called "structured
teaching", emphasises structure by using organized physical
environments, predictably sequenced activities, visual schedules and
visually structured activities, and structured work/activity systems
where each child can practice various tasks.
Parents are taught to implement the treatment at home. A 1998
controlled trial found that children treated with a TEACCH-based home
program improved significantly more than a control group.
A 2013 meta-analysis compiling all the clinical trials of TEACCH
indicated that it has small or no effects on perceptual, motor, verbal,
cognitive, and motor functioning, communication skills, and activities
of daily living. There were positive effects in social and maladaptive
behavior, but these required further replication due to the
methodological limitations of the pool of studies analysed.
Sensory integration
Unusual responses to sensory stimuli
are more common and prominent in children with autism, although there
is not good evidence that sensory symptoms differentiate autism from
other developmental disorders. Several therapies have been developed to treat Sensory processing disorder. Some of these treatments (for example, sensorimotor
handling) have a questionable rationale and have no empirical evidence.
Other treatments have been studied, with small positive outcomes, but
few conclusions can be drawn due to methodological problems with the
studies. These treatments include prism lenses, physical exercise, auditory integration training,
and sensory stimulation or inhibition techniques such as "deep
pressure"—firm touch pressure applied either manually or via an
apparatus such as a hug machine or a pressure garment.
Weighted vests, a popular deep-pressure therapy, have only a limited
amount of scientific research available, which on balance indicates that
the therapy is ineffective.
Although replicable treatments have been described and valid outcome
measures are known, gaps exist in knowledge related to Sensory
processing disorder and therapy.
In a 2011 Cochrane review, no evidence was found to support the use of
auditory integration training as an ASD treatment method. Because empirical support is limited, systematic evaluation is needed if these interventions are used.
The term multisensory integration in simple terms means the ability to use all of ones senses to accomplish a task. Occupational therapists
sometimes prescribe sensory treatments for children with Autism however
in general there has been little or no scientific evidence of
effectiveness.
Animal-assisted therapy
Animal-assisted therapy,
where an animal such as a dog or a horse becomes a basic part of a
person's treatment, is a controversial treatment for some symptoms. A
2007 meta-analysis found that animal-assisted therapy is associated with a moderate improvement in autism spectrum symptoms. Reviews of published dolphin-assisted
therapy (DAT) studies have found important methodological flaws and
have concluded that there is no compelling scientific evidence that DAT
is a legitimate therapy or that it affords any more than fleeting
improvements in mood.
Neurofeedback
Neurofeedback
attempts to train individuals to regulate their brainwave patterns by
letting them observe their brain activity more directly. In its most
traditional form, the output of EEG electrodes is fed into a computer
that controls a game-like audiovisual display. Neurofeedback has been
evaluated with positive results for ASD, but studies have lacked random
assignment to controls.
Patterning
Patterning
is a set of exercises that attempts to improve the organization of a
child's neurologic impairments. It has been used for decades to treat
children with several unrelated neurologic disorders, including autism.
The method, taught at The Institutes for the Achievement of Human Potential, is based on oversimplified theories and is not supported by carefully designed research studies.
Packing
In
packing, children are wrapped tightly for up to an hour in wet sheets
that have been refrigerated, with only their heads left free. The
treatment is repeated several times a week, and can continue for years.
It is intended as treatment for autistic children who harm themselves;
most of these children cannot speak. Similar envelopment techniques have
been used for centuries, such as to calm violent patients in Germany in
the 19th century; its modern use in France began in the 1960s, based on
psychoanalytic theories such as the theory of the refrigerator mother.
Packing is currently used in hundreds of French clinics. There is no
scientific evidence for the effectiveness of packing, and some concern
about risk of adverse health effects.
Other methods
There
are many simple methods such as priming, prompt delivery, picture
schedules, peer tutoring, and cooperative learning, that have been
proven to help autistic students to prepare for class and to understand
the material better. Priming is done by allowing the students to see the
assignment or material before they are shown in class. Prompt delivery
consists of giving prompts to the autistic children in order to elicit a
response to the academic material. Picture schedules are used to
outline the progression of a class and are visual cues to allow autistic
children to know when changes in the activity are coming up. This
method has proven to be very useful in helping the students follow the
activities. Peer tutoring and cooperative learning are ways in which an
autistic student and a nonhandicapped student are paired together in the
learning process. This has shown be very effective for “increasing both
academic success and social interaction.” There are more specific strategies that have been shown to improve an autistic’s education, such as LEAP, Treatment and Education of Autistic and Related Communication Handicapped Children,
and Non-Model-Specific Special Education Programs for preschoolers.
LEAP is “an intensive 12-month program that focuses on providing a
highly structured and safe environment that helps students to
participate in and derive benefit from educational programming” and
focuses on children from 5-21 who have a more severe case of autism.
The goal of the program is to develop functional independence through
academic instruction, vocational/translational curriculum,
speech/language services, and other services personalized for each
student.
While LEAP, TEACCH, and Non-Model Specific Special Education Programs
are all different strategies, there has been no evidence that one is
more effective than the other.
Societal aspects
Martha
Nussbaum discusses how education is one of the fertile functions that
is important for the development of a person and their ability to
achieve a multitude of other capabilities within society.
Autism causes many symptoms that interfere with a child’s ability to
receive a proper education such as deficits in imitation, observational
learning, and receptive and expressive communication. Of all
disabilities affecting the population, autism ranks third lowest in
acceptance into a postsecondary education institution.
In a study funded by the National Institute of Health, Shattuck et al.
found that only 35% of autistics are enrolled in a 2 or 4 year college
within the first two years after leaving high school compared to 40% of
children who have a learning disability.
Due to the growing need for a college education to obtain a job, this
statistic shows how autistics are at a disadvantage in gaining many of
the capabilities that Nussbaum discusses and makes education more than
just a type of therapy for those with autism.
According to the study by Shattuck, only 55% of children with autism
participated in any paid employment within the first two years after
high school. Furthermore, those with autism that come from low income
families tend to have lower success in postsecondary schooling. Due to these issues, education has become more than just an issue of therapy for those with autism but also a social issue.
Disadvantages
Oftentimes,
schools simply lack the resources to create an optimal classroom
setting for those in need of special education. In the United States, it
can cost between $6595 to $10,421 extra to educate a child with autism.
In the 2011-2012 school year, the average cost of education for a
public school student was $12,401. In some cases, the extra cost
required to educate a child with autism nearly doubles the average cost
to educate the average public school student.
As the range of those with autism can widely vary, it is very difficult
to create an autism program that is well suited to the entire
population of autistics as well as those with other disabilities. In the
United States, many school districts are requiring schools to meet the
needs of disabled students, regardless of the number of children with
disabilities there are in the school.
This combined with a shortage of licensed special education teachers
has created a deficiency in the special education system. The shortage
has caused some states to give temporary special education licenses to
teachers with the caveat that they receive a license within a few years.
Policies
In
the United States, there have been three major policies addressing
special education in the United States. These policies were the Education for All Handicapped Children Act in 1975, the Individuals with Disabilities Education Act in 1997, and the No Child Left Behind
in 2001. The development of these policies showed increased guidelines
for special education and requirements; such as requiring states to fund
special education, equality of opportunities, help with transitions
after secondary schooling, requiring extra qualifications for special
education teachers, and creating a more specific class setting for those
with disabilities. The Individuals with Disabilities Education Act,
specifically had a large impact on special education as public schools
were then required to employ high qualified staff. For one to be a
Certified Autism Specialist, one must have a master's degree, two years
of career experience working with the autism population, earn 14
continuing education hours in autism every two years, and register with
the International Institute of Education.
In 1993, Mexico passed an education law that called for the inclusion
of those with disabilities. This law was very important for Mexico
education, however, there have been issues in implementing it due to a
lack of resources.
There have also been multiple international groups that have
issued reports addressing issues in special education. The United
Nations on “International Norms and Standards relating to Disability” in
1998. This report cites multiple conventions, statements, declarations,
and other reports such as: The Universal Declaration of Human Rights,
The Salamanca Statement, the Sundberg Declaration, the Copenhagen
Declaration and Programme of Action, and many others. One main point
that the report emphasizes is the necessity for education to be a human
right. The report also states that the “quality of education should be
equal to that of persons without disabilities.” The other main points
brought up by the report discuss integrated education, special education
classes as supplementary, teacher training, and equality for vocational education.
The United Nations also releases a report by the Special Rapporteur
that has a focus on persons with disabilities. In 2015, a report titled
“Report of the Special Rapporteur to the 52nd Session of the Commission
for Social Development: Note by the Secretary-General on Monitoring of
the implementation of the Standard Rules on the Equalization of
Opportunities for Persons with Disabilities” was released. This report
focused on looking at how the many countries involved, with a focus on
Africa, have handled policy regarding persons with disabilities. In this
discussion, the author also focuses on the importance of education for
persons with disabilities as well as policies that could help improve
the education system such as a move towards a more inclusive approach.
The World Health Organization has also published a report addressing
people with disabilities and within this there is a discussion on
education in their “World Report on Disability” in 201. Other organizations that have issued reports discussing the topic are UNESCO, UNICEF, and the World Bank.
Environmental enrichment
Environmental enrichment is concerned with how the brain is affected by the stimulation of its information processing
provided by its surroundings (including the opportunity to interact
socially). Brains in richer, more-stimulating environments, have
increased numbers of synapses, and the dendrite arbors upon which they reside are more complex. This effect happens particularly during neurodevelopment,
but also to a lesser degree in adulthood. With extra synapses there is
also increased synapse activity and so increased size and number of glial energy-support cells. Capillary vasculation also is greater to provide the neurons and glial cells with extra energy. The neuropil
(neurons, glial cells, capillaries, combined together) expands making
the cortex thicker. There may also exist (at least in rodents) more neurons.
Research on nonhuman animals finds that more-stimulating
environments could aid the treatment and recovery of a diverse variety
of brain-related dysfunctions, including Alzheimer's disease and those connected to aging, whereas a lack of stimulation might impair cognitive development.
Research on humans suggests that lack of stimulation
(deprivation—such as in old-style orphanages) delays and impairs
cognitive development. Research also finds that higher levels of
education (which is both cognitively stimulating in itself, and
associates with people engaging in more challenging cognitive
activities) results in greater resilience (cognitive reserve) to the effects of aging and dementia.
Massage therapy
A review of massage therapy
as a symptomatic treatment of autism found limited evidence of benefit.
There were few high quality studies, and due to the risk of bias found in the studies analyzed, no firm conclusions about the efficacy of massage therapy could be drawn.
Music
Music therapy
uses the elements of music to let people express their feelings and
communicate. A 2014 review found that music therapy may help in social
interactions and communication.
Music therapy can involve various techniques depending on where the subject is sitting on the ASD scale.
Somebody who may be considered as 'low-functioning' would require
vastly different treatment to somebody on the ASD scale who is
'high-functioning'. Examples of these types of therapeutic techniques
include:
- Free improvisation - No boundaries or skills required
- Structured improvisation - Some established parameters within the music
- Performing or recreating music - Reproducing a pre-composed piece of music or song with associated activities
- Composing music - Creating music that caters to the specific needs of that person using instruments or the voice
- Listening - Engaging in specific musical listening base exercises
Improvisational Music Therapy (IMT), is increasing in popularity as a
therapeutic technique being applied to children with ASD. The process
of IMT occurs when the client and therapist make up music, through the
use of various instruments, song and movement. The specific needs of
each child or client need to be taken into consideration. Some children
with ASD find their different environments chaotic and confusing,
therefore, IMT sessions require the presence of a certain routine and be
predictable in nature, within their interactions and surroundings.
Music can provide all of this, it can be very predicable, it is highly
repetitious with its melodies and sounds, but easily varied with
phrasing, rhythm and dynamics giving it a controlled flexibility. The
allowance of parents or caregivers to sessions can put the child at ease
and allow for activities to be incorporated into everyday life.
Sensory enrichment therapy
In
all interventions for autistic children, the main strategy is to aim
towards the improvement on sensitivity in all senses. Autistic children
suffer from a lack of the ability to derive and sort out their senses as
well as the feelings and moods of the people around them. Many children with autism suffer from this Sensory Processing Disorder.
In sensory-based interventions, there have been signs of progress in
children responding with an appropriate response when given a stimulus
after being in sensory-based therapies for a period of time. However, at
this time, there is no concrete evidence that these therapies are
effective for children with Autism.
Autism is a very complex disorder and differs from child to child. This
makes the effectiveness of each type of therapy and even therapy
activity vary.
The purpose of these differentiated interventions are to
intervene at the neurological level of the brain in hopes to develop
appropriate responses to the different sensations from one's body and
also to outside stimuli in one's environment. Scientist have used music
therapies, massage therapies, occupational therapies and more. With the
Autistic Spectrum being so diverse and widespread, each case or scenario
is different.
Parent mediated interventions
Parent mediated interventions offer support and practical advice to parents of autistic children. A 2002 Cochrane Review
found only two relevant studies, with small numbers of participants,
and no clinical recommendations could be made due to these limitations.
A very small number of randomized and controlled studies suggest that
parent training can lead to reduced maternal depression, improved
maternal knowledge of autism and communication style, and improved child
communicative behavior, but due to the design and number of studies
available, definitive evidence of effectiveness is not available.
Early detection of ASD in children can often occur before a child
reaches the age of three years old. Methods that target early behavior
can influence the quality of life for a child with ASD. Parents can
learn methods of interaction and behavior management to best assist
their child's development. A 2013 Cochrance review concluded that there
were some improvements when parent intervention was used.
Medical management
Drugs,
supplements, or diets are often used to alter physiology in an attempt
to relieve common autistic symptoms such as seizures, sleep
disturbances, irritability, and hyperactivity that can interfere with
education or social adaptation or (more rarely) cause autistic
individuals to harm themselves or others.
There is plenty of anecdotal evidence to support medical treatment;
many parents who try one or more therapies report some progress, and
there are a few well-publicized reports of children who are able to
return to mainstream education after treatment, with dramatic
improvements in health and well-being. However, this evidence may be
confounded by improvements seen in autistic children who grow up without
treatment, by the difficulty of verifying reports of improvements, and
by the lack of reporting of treatments' negative outcomes. Only a very few medical treatments are well supported by scientific evidence using controlled experiments.
Prescription medication
Many medications are used to treat problems associated with ASD. More than half of U.S. children diagnosed with ASD are prescribed psychoactive drugs or anticonvulsants, with the most common drug classes being antidepressants, stimulants, and antipsychotics. Only the antipsychotics have clearly demonstrated efficacy.
Research has focused on atypical antipsychotics, especially risperidone,
which has the largest amount of evidence that consistently shows
improvements in irritability, self-injury, aggression, and tantrums
associated with ASD. Risperidone is approved by the Food and Drug Administration (FDA) for treating symptomatic irritability in autistic children and adolescents. In short-term trials (up to six months) most adverse events were mild to moderate, with weight gain, drowsiness, and high blood sugar requiring monitoring; long term efficacy and safety have not been fully determined. It is unclear whether risperidone improves autism's core social and communication deficits.
The FDA's decision was based in part on a study of autistic children
with severe and enduring problems of tantrums, aggression, and
self-injury; risperidone is not recommended for autistic children with
mild aggression and explosive behavior without an enduring pattern.
Other drugs are prescribed off-label in the U.S., which means they have not been approved for treating ASD. Large placebo-controlled studies of olanzapine and aripiprazole were underway in early 2008.
Aripiprazole may be effective for treating autism in the short term,
but is also associated with side effects, such as weight gain and
sedation. Some selective serotonin reuptake inhibitors (SSRIs) and dopamine blockers can reduce some maladaptive behaviors associated with ASD. Although SSRIs reduce levels of repetitive behavior in autistic adults, a 2009 multisite randomized controlled study found no benefit and some adverse effects in children from the SSRI citalopram, raising doubts whether SSRIs are effective for treating repetitive behavior in autistic children.
A further study of related medical reviews determined that the
prescription of SSRI antidepressants for treating autistic spectrum
disorders in children lacked any evidence, and could not be recommended. Reviews of evidence found that the psychostimulant methylphenidate
may be efficacious against hyperactivity and possibly impulsivity
associated with ASD, although the findings were limited by low quality
evidence.
There was no evidence that methylphenidate "has a negative impact on
the core symptoms of ASD, or that it improves social interaction,
stereotypical behaviours, or overall ASD."
Of the many medications studied for treatment of aggressive and
self-injurious behavior in children and adolescents with autism, only
risperidone and methylphenidate demonstrate results that have been
replicated. A 1998 study of the hormone secretin reported improved symptoms and generated tremendous interest, but several controlled studies since have found no benefit. Oxytocin may play a role in autism and may be an effective treatment for repetitive and affiliative behaviors;
two related studies in adults found that oxytocin decreased repetitive
behaviors and improved interpretation of emotions, but these preliminary
results do not necessarily apply to children. An experimental drug STX107 has stopped overproduction of metabotropic glutamate receptor 5
in rodents, and it has been hypothesized that this may help in about 5%
of autism cases, but this hypothesis has not been tested in humans.
Aside from antipsychotics, there is scant reliable research about the effectiveness or safety of drug treatments for adolescents and adults with ASD. Results of the handful of randomized controlled trials that have been performed suggest that risperidone, the SSRI fluvoxamine, and the typical antipsychotic haloperidol may be effective in reducing some behaviors, that haloperidol may be more effective than the tricyclic antidepressant clomipramine, and that the opioid antagonist naltrexone hydrochloride is not effective. In small studies, memantine has been shown to significantly improve language function and social behavior in children with autism. Research is underway on the effects of memantine in adults with autism spectrum disorders. A person with ASD may respond atypically to medications and the medications can have adverse side effects.
Prosthetics
Unlike conventional neuromotor prostheses,
neurocognitive prostheses would sense or modulate neural function in
order to physically reconstitute cognitive processes such as executive function
and language. No neurocognitive prostheses are currently available but
the development of implantable neurocognitive brain-computer interfaces
has been proposed to help treat conditions such as autism.
Affective computing
devices, typically with image or voice recognition capabilities, have
been proposed to help autistic individuals improve their social
communication skills. These devices are still under development. Robots have also been proposed as educational aids for autistic children.
Transcranial magnetic stimulation
Transcranial magnetic stimulation, which is a somewhat well established treatment for depression, has been proposed, and used, as a treatment for autism. A review published in 2013 found insufficient evidence to support its widespread use for autism spectrum disorders. A 2015 review found tentative but insufficient evidence to justify its use outside of clinical studies.
Alternative medicine
Acupuncture has not been found to be helpful. A number of naturopathic practitioners claim that CEASE therapy,
a mixture of homeopathy, supplements and 'vaccine detoxing', can help
people with autism however no robust evidence is available for this. A
podiatrist in East Preston, West Sussex was reported to be suggesting the administration of chlorine dioxide, orally and through an enema, to cure children of autism in January 2020. Chlorine dioxide is toxic.
Emerging evidence for mindfulness-based
interventions for improving mental health in adults with autism has
support through a recent systematic review. This includes evidence for
decreasing stress, anxiety, ruminating thoughts, anger, and aggression.
Hyperbaric Oxygen
A boy with ASD, and his father, in a hyperbaric oxygen chamber.
One small 2009 double-blind study of autistic children found that 40
hourly treatments of 24% oxygen at 1.3 atmospheres provided significant
improvement in the children's behavior immediately after treatment
sessions but this study has not been independently confirmed.
More recent, relatively large-scale controlled studies have also
investigated HBOT using treatments of 24% oxygen at 1.3 atmospheres and
have found less promising results. A 2010 double-blind study compared
HBOT to a placebo treatment in children with autistic disorder. Both
direct observational measures of behavioral symptoms and standardized
psychological assessments were used to evaluate the treatment. No
differences were found between the HBOT group and the placebo group on
any of the outcome measures.
A second 2011 single-subject design study also investigated the effects
of 40 HBOT treatments of 24% oxygen at 1.3 atmospheres on directly
observed behaviors using multiple baselines across 16 participants.
Again, no consistent outcomes were observed across any group and
further, no significant improvements were observed within any individual
participant.
Together these studies suggest that HBOT at 24% oxygen at 1.3
atmospheric pressure does not result in a clinically significant
improvement of the behavioral symptoms of autistic disorder.
Nonetheless, news reports and related blogs indicate that HBOT is used
for many cases of children with autism. HBOT can cost up to $150 per
hour with individuals using anywhere from 40 to 120 hours as a part of
their integrated treatment programs. In addition, purchasing (at
$8,495–27,995) and renting ($1,395 per month) of the HBOT chambers is
another option some families use.
When considering the financial and time investments required in order
to participate in this treatment and the inconsistency of the present
findings, HBOT seems to be a riskier and thus, often less favorable
alternative treatment for autism. Further studies are needed in order
for practitioners and families to make more conclusive and valid
decisions concerning HBOT treatments.
Chiropractic
Chiropractic
is an alternative medical practice whose main hypothesis is that
mechanical disorders of the spine affect general health via the nervous
system, and whose main treatment is spinal manipulation. A significant portion of the profession rejects vaccination, as traditional chiropractic philosophy equates vaccines to poison. Most chiropractic writings on vaccination focus on its negative aspects, claiming that it is hazardous, ineffective, and unnecessary, and in some cases suggesting that vaccination causes autism or that chiropractors should be the primary contact for treatment of autism and other neurodevelopmental disorders. Chiropractic treatment has not been shown to be effective for medical conditions other than back pain, and there is insufficient scientific evidence to make conclusions about chiropractic care for autism.
Craniosacral therapy
Craniosacral therapy is an alternative medical practice whose main hypothesis is that restrictions at cranial sutures of the skull affect rhythmic impulses conveyed via cerebrospinal fluid,
and that gentle pressure on external areas can improve the flow and
balance of the supply of this fluid to the brain, relieving symptoms of
many conditions. There is no scientific support for major elements of the underlying model,
there is little scientific evidence to support the therapy, and
research methods that could conclusively evaluate the therapy's
effectiveness have not been applied. No published studies are available on the use of this therapy for autism.
Chelation therapy
Based on the speculation that heavy metal poisoning
may trigger the symptoms of autism, particularly in small subsets of
individuals who cannot excrete toxins effectively, some parents have
turned to alternative medicine practitioners who provide detoxification treatments via chelation therapy. However, evidence to support this practice has been anecdotal and not rigorous. Strong epidemiological evidence refutes links between environmental triggers, in particular thiomersal-containing vaccines,
and the onset of autistic symptoms. No scientific data supports the
claim that the mercury in the vaccine preservative thiomersal causes
autism or its symptoms, and there is no scientific support for chelation therapy as a treatment for autism.
Thiamine
tetrahydrofurfuryl disulfide (TTFD) is hypothesized to act as a
chelating agent in children with autism. A 2002 pilot study administered
TTFD rectally to ten autism spectrum children, and found beneficial clinical effect.
This study has not been replicated, and a 2006 review of thiamine by
the same author did not mention thiamine's possible effect on autism. There is not sufficient evidence to support the use of thiamine (vitamin B1) to treat autism.
Dietary supplements
Many parents give their children dietary supplements
in an attempt to treat autism or to alleviate its symptoms. The range
of supplements given is wide; few are supported by scientific data, but
most have relatively mild side effects.
A review found some low-quality evidence to support the use of vitamin B6 in combination with magnesium at high doses, but the evidence was equivocal and the review noted the possible danger of fatal hypermagnesemia. A Cochrane Review
of the evidence for the use of B6 and magnesium found that "[d]ue to
the small number of studies, the methodological quality of studies, and
small sample sizes, no recommendation can be advanced regarding the use
of B6-Mg as a treatment for autism."
Dimethylglycine (DMG) is hypothesized to improve speech and reduce autistic behaviors, and is a commonly used supplement. Two double-blind, placebo-controlled studies found no statistically significant effect on autistic behaviors, and reported few side effects. No peer-reviewed studies have addressed treatment with the related compound trimethylglycine.
Vitamin C decreased stereotyped behavior in a small 1993 study.
The study has not been replicated, and vitamin C has limited popularity
as an autism treatment. High doses might cause kidney stones or
gastrointestinal upset such as diarrhea.
Probiotics containing potentially beneficial bacteria are hypothesized to relieve some symptoms of autism by minimizing yeast overgrowth in the colon. The hypothesized yeast overgrowth has not been confirmed by endoscopy,
the mechanism connecting yeast overgrowth to autism is only
hypothetical, and no clinical trials to date have been published in the
peer-reviewed literature. No negative side effects have been reported.
Melatonin
is sometimes used to manage sleep problems in developmental disorders.
Adverse effects are generally reported to be mild, including drowsiness,
headache, dizziness, and nausea; however, an increase in seizure
frequency is reported among susceptible children.
Several small RCTs have indicated that melatonin is effective in
treating insomnia in autistic children, but further large studies are
needed.
A 2013 literature review found 20 studies that reported improvements
in sleep parameters as a result of melatonin supplementation, and
concluded that "the administration of exogenous melatonin for abnormal
sleep parameters in ASD is evidence-based."
Although omega-3 fatty acids, which are polyunsaturated fatty acids
(PUFA), are a popular treatment for children with ASD, there is very
little high-quality scientific evidence supporting their effectiveness, and further research is needed.
Several other supplements have been hypothesized to relieve autism symptoms, including BDTH2, carnosine, cholesterol, cyproheptadine, D-cycloserine, folic acid, glutathione, metallothionein promoters, other PUFA such as omega-6 fatty acids, tryptophan, tyrosine, thiamine (see Chelation therapy), vitamin B12, and zinc. These lack reliable scientific evidence of efficacy or safety in treatment of autism.
Diets
Atypical eating behavior occurs in about three-quarters of children
with ASD, to the extent that it was formerly a diagnostic indicator.
Selectivity is the most common problem, although eating rituals and food
refusal also occur; this does not appear to result in malnutrition. Although some children with autism also have gastrointestinal
(GI) symptoms, there is a lack of published rigorous data to support
the theory that autistic children have more or different GI symptoms
than usual; studies report conflicting results, and the relationship between GI problems and ASD is unclear.
In the early 1990s, it was hypothesized that autism can be caused or aggravated by opioid peptides like casomorphine that are metabolic products of gluten and casein.
Based on this hypothesis, diets that eliminate foods containing either
gluten or casein, or both, are widely promoted, and many testimonials
can be found describing benefits in autism-related symptoms, notably
social engagement and verbal skills. Studies supporting these claims
have had significant flaws, so these data are inadequate to guide
treatment recommendations.
Other elimination diets have also been proposed, targeting salicylates, food dyes, yeast,
and simple sugars. No scientific evidence has established the efficacy
of such diets in treating autism in children. An elimination diet may
create nutritional deficiencies that harm overall health unless care is
taken to assure proper nutrition.
For example, a 2008 study found that autistic boys on casein-free diets
have significantly thinner bones than usual, presumably because the
diets contribute to calcium and vitamin D deficiencies.
Electroconvulsive therapy
Studies indicate that 12–17% of adolescents and young adults with autism satisfy diagnostic criteria for catatonia, which is loss of or hyperactive motor activity. Electroconvulsive therapy
(ECT) has been used to treat cases of catatonia and related conditions
in people with autism. However, no controlled trials have been performed
of ECT in autism, and there are serious ethical and legal obstacles to
its use.
Stem cell therapy
Mesenchymal stem cells and cord blood CD34+ cells have been proposed to treat autism, but this proposal has not been tested. They may represent a future treatment.
Since immune system deregulation has been implicated in autism,
mesenchymal stem cells show the greatest promise as treatment for the
disorder. Changes in the innate and adaptive immune system have been
observed. Those with autism show an imbalance in CD3+, CD4+, and CD8+ T
cells, as well as in NK cells. In addition, peripheral blood mononuclear cells (PBMCs) overproduce IL-1β. MSC mediated immune suppressive activity could restore this immune imbalance.
Religious interventions
The Table Talk of Martin Luther contains the story of a twelve-year-old boy who some believe was severely autistic. According to Luther's notetaker Mathesius, Luther thought the boy was a soulless mass of flesh possessed by the devil, and suggested that he be suffocated. In 2003, an autistic boy in Wisconsin suffocated during an exorcism by an Evangelical minister in which he was wrapped in sheets.
Ultraorthodox Jewish parents sometimes use spiritual and mystical
interventions such as prayers, blessings, recitations of religious
text, amulets, changing the child's name, and exorcism.
One study has suggested that spirituality and not religious activities involving the mothers of autistic children were associated with better outcomes for the child.
Anti-cure perspective
The exact cause of autism
is unclear, yet some organizations advocate researching a cure. Some
autism rights organizations view autism as a way of life rather than as a
mental disorder and thus advocate acceptance over a search for a cure.
Historical approach
Before
autism was well understood, children in Britain and America would often
be put in institutions on the instruction of doctors and the parents
told to forget about them. Observer journalist Christopher Stevens,
father of an autistic child, reports how a British doctor told him that
after a child was admitted, usually "nature would take its course" and
the child would die due to the prevalence of tuberculosis.
Research
Environmental enrichment has found to be useful in animal models of autism. Two human trials also found benefit in some children.
Between the 1950s and 1970s LSD was studied, however, has not been studied since.