From Wikipedia, the free encyclopedia
Omega-3 fatty acids—also called ω-3 fatty acids or n-3 fatty acids[1]—are polyunsaturated fatty acids (PUFAs) with a double bond (C=C) at the third carbon atom from the end of the carbon chain.[2] The fatty acids have two ends, the carboxylic acid (-COOH) end, which is considered the beginning of the chain, thus "alpha", and the methyl (-CH3) end, which is considered the "tail" of the chain, thus "omega"; the double bond is at omega minus 3 (not dash 3). One way in which a fatty acid is named is determined by the location of the first double bond, counted from the methyl end, that is, the omega (ω-) or the n- end. However, the standard (IUPAC) chemical nomenclature system starts from the carbonyl end.
The three types of omega-3 fatty acids involved in human physiology are α-linolenic acid (ALA) (found in plant oils), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA) (both commonly found in marine oils). Marine algae and phytoplankton are primary sources of omega-3 fatty acids. Common sources of plant oils containing the omega-3 ALA fatty acid include walnut, edible seeds, clary sage seed oil, algal oil, flaxseed oil, Sacha Inchi oil, Echium oil, and hemp oil, while sources of animal omega-3 EPA and DHA fatty acids include fish, fish oils, eggs from chickens fed EPA and DHA, squid oils, and krill oil. Dietary supplementation with omega-3 fatty acids does not appear to affect the risk of death, cancer or heart disease.[3][4] Furthermore, fish oil supplement studies have failed to support claims of preventing heart attacks or strokes.[5]
Omega-3 fatty acids are important for normal metabolism.[6] Mammals are unable to synthesize omega-3 fatty acids, but can obtain the shorter-chain omega-3 fatty acid ALA (18 carbons and 3 double bonds) through diet and use it to form the more important long-chain omega-3 fatty acids, EPA (20 carbons and 5 double bonds) and then from EPA, the most crucial, DHA (22 carbons and 6 double bonds).[6] The ability to make the longer-chain omega-3 fatty acids from ALA may be impaired in aging.[7][8] In foods exposed to air, unsaturated fatty acids are vulnerable to oxidation and rancidity.[9]
Health effects
Supplementation does not appear to be associated with a lower risk of all-cause mortality.[3]Cancer
The evidence linking the consumption of fish to the risk of cancer is poor.[10] Supplementation with omega-3 fatty acids does not appear to affect this either.[4]A 2006 review concluded that there was no link between omega-3 fatty acids consumption and
cancer.[4] This is similar to the findings of a review of studies up to February 2002 that failed to find clear effects of long and shorter chain omega-3 fats on total risk of death, combined cardiovascular events and cancer.[11][12] In those with advanced cancer and cachexia, omega-3 fatty acids supplements may be of benefit, improving appetite, weight, and quality of life.[13] There is tentative evidence that marine omega-3 polyunsaturated fatty acids reduce the risk of breast cancer but this is not conclusive.[14][15]
The effect of consumption on prostate cancer is not conclusive.[15] There is a decreased risk with higher blood levels of DPA, but an increased risk of more aggressive prostate cancer with higher blood levels of combined EPA and DHA (found in fatty fish oil).[16]
Cardiovascular disease
Evidence, in the population generally, does not support a beneficial role for omega-3 fatty acid supplementation in preventing cardiovascular disease (including myocardial infarction and sudden cardiac death) or stroke.[3][17][18] However, omega-3 fatty acid supplementation greater than one gram daily for at least a year may be protective against cardiac death, sudden death, and myocardial infarction in people who have a history of cardiovascular disease.[19] No protective effect against the development of stroke or all-cause mortality was seen in this population.[19] Eating a diet high in fish that contain long chain omega-3 fatty acids does appear to decrease the risk of stroke.[20] Fish oil supplementation has not been shown to benefit revascularization or abnormal heart rhythms and has no effect on heart failure hospital admission rates.[21] Furthermore, fish oil supplement studies have failed to support claims of preventing heart attacks or strokes.[5]Evidence suggests that omega-3 fatty acids modestly lower blood pressure (systolic and diastolic) in people with hypertension and in people with normal blood pressure.[22] Some evidence suggests that people with certain circulatory problems, such as varicose veins, may benefit from the consumption of EPA and DHA, which may stimulate blood circulation and increase the breakdown of fibrin, a protein involved in blood clotting and scar formation.[23][24] Omega-3 fatty acids reduce blood triglyceride levels but do not significantly change the level of LDL cholesterol or HDL cholesterol in the blood.[25][26] The American Heart Association position (2011) is that borderline elevated triglycerides, defined as 150–199 mg/dL, can be lowered by 0.5-1.0 grams of EPA and DHA per day; high triglycerides 200–499 mg/dL benefit from 1-2 g/day; and >500 mg/dL be treated under a physician's supervision with 2-4 g/day using a prescription product.[27]
ALA does not confer the cardiovascular health benefits of EPA and DHAs.[28]
The effect of omega-3 polyunsaturated fatty acids on stroke is unclear, with a possible benefit in women.[29]
Inflammation
Some research suggests that the anti-inflammatory activity of long-chain omega-3 fatty acids may translate into clinical effects.[30] A 2013 systematic review found tentative evidence of benefit.[31] Consumption of omega-3 fatty acids from marine sources lowers markers of inflammation in the blood such as C-reactive protein, interleukin 6, and TNF alpha.[32]For rheumatoid arthritis (RA), one systematic review found consistent, but modest, evidence for the effect of marine n-3 PUFAs on symptoms such as "joint swelling and pain, duration of morning stiffness, global assessments of pain and disease activity" as well as the use of non-steroidal anti-inflammatory drugs.[33] The American College of Rheumatology (ACR) has stated that there may be modest benefit from the use of fish oils, but that it may take months for effects to be seen, and cautions for possible gastrointestinal side effects and the possibility of the supplements containing mercury or vitamin A at toxic levels. The National Center for Complementary and Integrative Health has concluded that "[n]o dietary supplement has shown clear benefits for RA", but that there is preliminary evidence that fish oil may be beneficial, and called for further study.[34]
Developmental disabilities
Although not supported by current scientific evidence as a primary treatment for ADHD, autism, and other developmental disabilities,[35][36] omega-3 fatty acid supplements are being given to children with these conditions.[35]One meta-analysis concluded that omega-3 fatty acid supplementation demonstrated a modest effect for improving ADHD symptoms.[37] A Cochrane review of PUFA (not necessarily omega-3) supplementation found "there is little evidence that PUFA supplementation provides any benefit for the symptoms of ADHD in children and adolescents",[38] while a different review found "insufficient evidence to draw any conclusion about the use of PUFAs for children with specific learning disorders".[39] Another review concluded that the evidence is inconclusive for the use of omega-3 fatty acids in behavior and non-neurodegenerative neuropsychiatric disorders such ADHD and depression.[40]
Fish oil has only a small benefit on the risk of early birth.[41][42] A 2015 meta-analysis of the effect of omega-3 supplementation during pregnancy did not demonstrate a decrease in the rate of preterm birth or improve outcomes in women with singleton pregnancies with no prior preterm births.[43] A systematic review and meta-analysis published the same year reached the opposite conclusion, specifically, that omega-3 fatty acids were effective in "preventing early and any preterm delivery".[44]
Mental health
There is some evidence that omega-3 fatty acids are related to mental health,[45] including that they may tentatively be useful as an add-on for the treatment of depression associated with bipolar disorder.[46] Significant benefits due to EPA supplementation were only seen, however, when treating depressive symptoms and not manic symptoms suggesting a link between omega-3 and depressive mood.[46] There is also preliminary evidence that EPA supplementation is helpful in cases of depression.[47] The link between omega-3 and depression has been attributed to the fact that many of the products of the omega-3 synthesis pathway play key roles in regulating inflammation such as prostaglandin E3 which have been linked to depression.[48] This link to inflammation regulation has been supported in both in vitro [49] and in vivo studies as well as in meta-analysis studies.[31] The exact mechanism in which omega-3 acts upon the inflammatory system is still controversial as it was commonly believed to have anti-inflammatory effects.[50]There is, however, significant difficulty in interpreting the literature due to participant recall and systematic differences in diets.[51] There is also controversy as to the efficacy of omega-3, with many meta-analysis papers finding heterogeneity among results which can be explained mostly by publication bias.[52][53] A significant correlation between shorter treatment trials was associated with increased omega-3 efficacy for treating depressed symptoms further implicating bias in publication.[53]
Very low quality evidence finds that omega-3 fatty acids might prevent psychosis.[54]
Cognitive aging
Epidemiological studies are inconclusive about an effect of omega-3 fatty acids on the mechanisms of Alzheimer's disease.[55] There is preliminary evidence of effect on mild cognitive problems, but none supporting an effect in healthy people or those with dementia.[56][57][58]Brain and visual functions
Brain function and vision rely on dietary intake of DHA to support a broad range of cell membrane properties, particularly in grey matter, which is rich in membranes.[59][60] A major structural component of the mammalian brain, DHA is the most abundant omega-3 fatty acid in the brain.[61] It is under study as a candidate essential nutrient with roles in neurodevelopment, cognition and neurodegenerative disorders.[59]Atopic diseases
Results of studies investigating the role of LCPUFA supplementation and LCPUFA status in the prevention and therapy of atopic diseases (allergic rhinoconjunctivitis, atopic dermatitis and allergic asthma) are controversial; therefore, at the present stage of our knowledge we cannot state either that the nutritional intake of n-3 fatty acids has a clear preventive or therapeutic role, or that the intake of n-6 fatty acids has a promoting role in context of atopic diseases.[62]Risk of deficiency
People with PKU often have low intake of omega-3 fatty acids, because nutrients rich in omega-3 fatty acids are excluded from their diet due to high protein content.[63]Chemistry
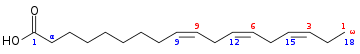
Chemical structure of alpha-linolenic acid (ALA), an essential omega-3
fatty acid, (18:3Δ9c,12c,15c, which means a chain of 18 carbons with 3
double bonds on carbons numbered 9, 12, and 15). Although chemists count
from the carbonyl carbon (blue numbering), biologists count from the n (ω) carbon (red numbering). Note that, from the n end (diagram right), the first double bond appears as the third carbon-carbon bond (line segment), hence the name "n-3". This is explained by the fact that the n
end is almost never changed during physiological transformations in the
human body, as it is more energy-stable, and other compounds can be
synthesized from the other carbonyl end, for example in glycerides, or
from double bonds in the middle of the chain.
Chemical structure of eicosapentaenoic acid (EPA)
Chemical structure of docosahexaenoic acid (DHA)
Omega-3 fatty acids that are important in human physiology[64] are α-linolenic acid (18:3, n-3; ALA), eicosapentaenoic acid (20:5, n-3; EPA), and docosahexaenoic acid (22:6, n-3; DHA). These three polyunsaturates have either 3, 5, or 6 double bonds in a carbon chain of 18, 20, or 22 carbon atoms, respectively. As with most naturally-produced fatty acids, all double bonds are in the cis-configuration, in other words, the two hydrogen atoms are on the same side of the double bond; and the double bonds are interrupted by methylene bridges (-CH
2-), so that there are two single bonds between each pair of adjacent double bonds.
List of omega-3 fatty acids
This table lists several different names for the most common omega-3 fatty acids found in nature.| Common name | Lipid name | Chemical name |
|---|---|---|
| Hexadecatrienoic acid (HTA) | 16:3 (n-3) | all-cis-7,10,13-hexadecatrienoic acid |
| α-Linolenic acid (ALA) | 18:3 (n-3) | all-cis-9,12,15-octadecatrienoic acid |
| Stearidonic acid (SDA) | 18:4 (n-3) | all-cis-6,9,12,15-octadecatetraenoic acid |
| Eicosatrienoic acid (ETE) | 20:3 (n-3) | all-cis-11,14,17-eicosatrienoic acid |
| Eicosatetraenoic acid (ETA) | 20:4 (n-3) | all-cis-8,11,14,17-eicosatetraenoic acid |
| Eicosapentaenoic acid (EPA) | 20:5 (n-3) | all-cis-5,8,11,14,17-eicosapentaenoic acid |
| Heneicosapentaenoic acid (HPA) | 21:5 (n-3) | all-cis-6,9,12,15,18-heneicosapentaenoic acid |
| Docosapentaenoic acid (DPA), Clupanodonic acid |
22:5 (n-3) | all-cis-7,10,13,16,19-docosapentaenoic acid |
| Docosahexaenoic acid (DHA) | 22:6 (n-3) | all-cis-4,7,10,13,16,19-docosahexaenoic acid |
| Tetracosapentaenoic acid | 24:5 (n-3) | all-cis-9,12,15,18,21-tetracosapentaenoic acid |
| Tetracosahexaenoic acid (Nisinic acid) | 24:6 (n-3) | all-cis-6,9,12,15,18,21-tetracosahexaenoic acid |
Forms
Triglycerides
Marine fish oils naturally contain triglycerides with omega-3 fatty acids. There are processes by which the fatty acids can be separated from glycerol, concentrated to a higher EPA and DHA content and reassembled into high omega-3 triglycerides. There are no prescription products of this nature, only dietary supplements. There are disputed claims for superiority - absorption and function - of natural marine oil triglycerides, omega-3 enriched triglycerides, ethyl ester products and free fatty acid products.[citation needed]Ethyl esters
Omega-3 acid ethyl esters are created by starting with a marine oil, converting the triglycerides to free fatty acids, concentrating the omega-3 fatty acids, and attaching an ethanol molecule to each FA. Available in U.S. as prescription product and dietary supplement. Prescription product brand names Lovaza (had been Omacor),[65] OMTRYG,[66] four generic versions [67] and Ethyl eicosapentaenoic acid (Vascepa)[68] A review compares the prescription products.[69]Free fatty acids
Omega-3 carboxylic acids are created by starting with a marine oil, disassociating the triglycerides into free fatty acids and concentrating the omega-3 fatty acids. The product is free fatty acids.Prescribed use at 2 or 4 grams per day.[70] The prescription product is named Epanova.[71]Phospholipids
Phospholipid omega-3 is composed of two fatty acids attached to a phosphate and choline, versus the three fatty acids attached to glycerol in triglycerides. There are no prescription products of this nature, only dietary supplements. One source of phospholipid omega-3 is krill oil.Biochemistry
Transporters
DHA in the form of lysophosphatidylcholine is transported into the brain by a membrane transport protein, MFSD2A, which is exclusively expressed in the endothelium of the blood–brain barrier.[72][73]Mechanism of action
The 'essential' fatty acids were given their name when researchers found that they are essential to normal growth in young children and animals. The omega-3 fatty acid DHA, also known as docosahexaenoic acid, is found in high abundance in the human brain.[74] It is produced by a desaturation process, but humans lack the desaturase enzyme, which acts to insert double bonds at the ω6 and ω3 position.[74] Therefore, the ω6 and ω3 polyunsaturated fatty acids cannot be synthesized and are appropriately called essential fatty acids.[74]In 1964 it was discovered that enzymes found in sheep tissues convert omega-6 arachidonic acid into the inflammatory agent called prostaglandin E2[75] which both causes the sensation of pain and expedites healing and immune response in traumatized and infected tissues.[76] By 1979 more of what are now known as eicosanoids were discovered: thromboxanes, prostacyclins, and the leukotrienes.[76] The eicosanoids, which have important biological functions, typically have a short active lifetime in the body, starting with synthesis from fatty acids and ending with metabolism by enzymes. If the rate of synthesis exceeds the rate of metabolism, the excess eicosanoids may, however, have deleterious effects.[76] Researchers found that certain omega-3 fatty acids are also converted into eicosanoids, but at a much slower rate. Eicosanoids made from omega-3 fatty acids are often referred to as anti-inflammatory, but in fact they are just less inflammatory than those made from omega-6 fats. If both omega-3 and omega-6 fatty acids are present, they will "compete" to be transformed,[76] so the ratio of long-chain omega-3:omega-6 fatty acids directly affects the type of eicosanoids that are produced.[76]
Interconversion
Conversion efficiency of ALA to EPA and DHA
Humans can convert short-chain omega-3 fatty acids to long-chain forms (EPA, DHA) with an efficiency below 5%.[77][78] The omega-3 conversion efficiency is greater in women than in men, but less-studied.[79] Higher ALA and DHA values found in plasma phospholipids of women may be due to the higher activity of desaturases, especially that of delta-6-desaturase.[80]These conversions occur competitively with omega-6 fatty acids, which are essential closely related chemical analogues that are derived from linoleic acid. They both utilize the same desaturase and elongase proteins in order to synthesize inflammatory regulatory proteins.[48] The products of both pathways are vital for growth making a balanced diet of omega-3 and omega-6 important to an individual’s health.[81] A balanced intake ratio of 1:1 was believed to be ideal in order for proteins to be able to synthesize both pathways sufficiently, but this has been controversial as of recent research.[82]
The conversion of ALA to EPA and further to DHA in humans has been reported to be limited, but varies with individuals.[83][84] Women have higher ALA conversion efficiency than men, which is presumed[85] to be due to the lower rate of use of dietary ALA for beta-oxidation. This suggests that biological engineering of ALA conversion efficiency is possible. Goyens et al. argue that the absolute amounts of ALA and LA each influence conversion rates separately, rather than simply the ratio between the two.[86]
Omega-6 to omega-3 ratio
Human diet has changed rapidly in recent centuries resulting in a reported increased diet of omega-6 in comparison to omega-3.[87] The rapid evolution of human diet away from a 1:1 omega-3 and omega-6 ratio, such as during the Neolithic Agricultural Revolution, has presumably been too fast for humans to have adapted to biological profiles adept at balancing omega-3 and omega-6 ratios of 1:1.[88] This is commonly believed to be the reason why modern diets are correlated with many inflammatory disorders.[87] While omega-3 polyunsaturated fatty acids may be beneficial in preventing heart disease in humans, the level of omega-6 polyunsaturated fatty acids (and, therefore, the ratio) does not matter.[82][89]Both omega-6 and omega-3 fatty acids are essential: humans must consume them in their diet. Omega-6 and omega-3 eighteen-carbon polyunsaturated fatty acids compete for the same metabolic enzymes, thus the omega-6:omega-3 ratio of ingested fatty acids has significant influence on the ratio and rate of production of eicosanoids, a group of hormones intimately involved in the body's inflammatory and homeostatic processes, which include the prostaglandins, leukotrienes, and thromboxanes, among others. Altering this ratio can change the body's metabolic and inflammatory state.[11] In general, grass-fed animals accumulate more omega-3 than do grain-fed animals, which accumulate relatively more omega-6.[90] Metabolites of omega-6 are more inflammatory (esp. arachidonic acid) than those of omega-3. This necessitates that omega-6 and omega-3 be consumed in a balanced proportion; healthy ratios of omega-6:omega-3, according to some authors, range from 1:1 to 1:4.[91] Other authors believe that a ratio of 4:1 (4 times as much omega-6 as omega-3) is already healthy.[92][93] Studies suggest the evolutionary human diet, rich in game animals, seafood, and other sources of omega-3, may have provided such a ratio.[94][95]
Typical Western diets provide ratios of between 10:1 and 30:1 (i.e., dramatically higher levels of omega-6 than omega-3).[96] The ratios of omega-6 to omega-3 fatty acids in some common vegetable oils are: canola 2:1, hemp 2-3:1,[97] soybean 7:1, olive 3–13:1, sunflower (no omega-3), flax 1:3,[98] cottonseed (almost no omega-3), peanut (no omega-3), grapeseed oil (almost no omega-3) and corn oil 46:1 ratio of omega-6 to omega-3.[99]
History
Although omega-3 fatty acids have been known as essential to normal growth and health since the 1930s, awareness of their health benefits has dramatically increased since the 1980s.[100][101]On September 8, 2004, the U.S. Food and Drug Administration gave "qualified health claim" status to EPA and DHA omega-3 fatty acids, stating, "supportive but not conclusive research shows that consumption of EPA and DHA [omega-3] fatty acids may reduce the risk of coronary heart disease".[102] This updated and modified their health risk advice letter of 2001 (see below).
The Canadian Food Inspection Agency has recognized the importance of DHA omega-3 and permits the following claim for DHA: "DHA, an omega-3 fatty acid, supports the normal physical development of the brain, eyes and nerves primarily in children under two years of age."[103]
Dietary sources
| Common name | grams omega-3 |
|---|---|
| Flax | 11.4 [106] |
| Hemp | 11.0 |
| Herring, sardines | 1.3–2 |
| Mackerel: Spanish/Atlantic/Pacific | 1.1–1.7 |
| Salmon | 1.1–1.9 |
| Halibut | 0.60–1.12 |
| Tuna | 0.21–1.1 |
| Swordfish | 0.97 |
| Greenshell/lipped mussels | 0.95[106] |
| Tilefish | 0.9 |
| Tuna (canned, light) | 0.17–0.24 |
| Pollock | 0.45 |
| Cod | 0.15–0.24 |
| Catfish | 0.22–0.3 |
| Flounder | 0.48 |
| Grouper | 0.23 |
| Mahi mahi | 0.13 |
| Orange roughy | 0.028 |
| Red snapper | 0.29 |
| Shark | 0.83 |
| King mackerel | 0.36 |
| Hoki (blue grenadier) | 0.41[106] |
| Gemfish | 0.40[106] |
| Blue eye cod | 0.31[106] |
| Sydney rock oysters | 0.30[106] |
| Tuna, canned | 0.23[106] |
| Snapper | 0.22[106] |
| Mutton | 0.12[107] |
| Eggs, large regular | 0.109[106] |
| Strawberry or Kiwifruit | 0.10-0.20 |
| Broccoli | 0.10-0.20 |
| Barramundi, saltwater | 0.100[106] |
| Giant tiger prawn | 0.100[106] |
| Lean red meat | 0.031[106] |
| Turkey | 0.030[106] |
| Cereals, rice, pasta, etc. | 0.00[106] |
| Fruit | 0.00[106] |
| Milk, regular | 0.00[106] |
| Bread, regular | 0.00[106] |
| Vegetables | 0.00[106] |
Daily values
In the United States, the Institute of Medicine publishes a system of Dietary Reference Intakes, which includes Recommended Dietary Allowances (RDAs) for individual nutrients, and Acceptable Macronutrient Distribution Ranges (AMDRs) for certain groups of nutrients, such as fats. When there is insufficient evidence to determine an RDA, the institute may publish an Adequate Intake (AI) instead, which has a similar meaning, but is less certain. The AI for α-linolenic acid is 1.6 grams/day for men and 1.1 grams/day for women, while the AMDR is 0.6% to 1.2% of total energy.Because the physiological potency of EPA and DHA is much greater than that of ALA, it is not possible to estimate one AMDR for all omega-3 fatty acids. Approximately 10 percent of the AMDR can be consumed as EPA and/or DHA.[108] The Institute of Medicine has not established a RDA or AI for EPA, DHA or the combination, so there is no Daily Value (DVs are derived from RDAs), no labeling of foods or supplements as providing a DV percentage of these fatty acids per serving, and no labeling a food or supplement as an excellent source, or "High in..."[citation needed] As for safety, there was insufficient evidence as of 2005 to set an upper tolerable limit for omega-3 fatty acids,[108] although the FDA has advised that adults can safely consume up to a total of 3 grams per day of combined DHA and EPA, with no more than 2 g from dietary supplements.[6]Recommendations
The American Heart Association (AHA) has made recommendations for EPA and DHA due to their cardiovascular benefits: individuals with no history of coronary heart disease or myocardial infarction should consume oily fish two times per week; and "Treatment is reasonable" for those having been diagnosed with coronary heart disease. For the latter the AHA does not recommend a specific amount of EPA + DHA, although it notes that most trials were at or close to 1000 mg/day. The benefit appears to be on the order of a 9% decrease in relative risk.[109] The European Food Safety Authority (EFSA) approved a claim "EPA and DHA contributes to the normal function of the heart" for products that contain at least 250 mg EPA + DHA. The report did not address the issue of people with pre-existing heart disease. The World Health Organization recommends regular fish consumption (1-2 servings per week, equivalent to 200 to 500 mg/day EPA + DHA) as protective against coronary heart disease and ischaemic stroke.Contamination
Heavy metal poisoning by the body's accumulation of traces of heavy metals, in particular mercury, lead, nickel, arsenic, and cadmium, is a possible risk from consuming fish oil supplements.[medical citation needed] Also, other contaminants (PCBs, furans, dioxins, and PBDEs) might be found, especially in less-refined fish oil supplements.[citation needed] However, heavy metal toxicity from consuming fish oil supplements is highly unlikely, because heavy metals selectively bind with protein in the fish flesh rather than accumulate in the oil. An independent test in 2005 of 44 fish oils on the US market found all of the products passed safety standards for potential contaminants.[110][unreliable source?]Throughout their history, the Council for Responsible Nutrition and the World Health Organization have published acceptability standards regarding contaminants in fish oil. The most stringent current standard is the International Fish Oils Standard.[111][non-primary source needed] Fish oils that are molecularly distilled under vacuum typically make this highest-grade; levels of contaminants are stated in parts per billion per trillion.[citation needed]
Fish
The most widely available dietary source of EPA and DHA is oily fish, such as salmon, herring, mackerel, anchovies, menhaden, and sardines. Oils from these fish have a profile of around seven times as much omega-3 as omega-6. Other oily fish, such as tuna, also contain n-3 in somewhat lesser amounts. Consumers of oily fish should be aware of the potential presence of heavy metals and fat-soluble pollutants like PCBs and dioxins, which are known to accumulate up the food chain. After extensive review, researchers from Harvard's School of Public Health in the Journal of the American Medical Association (2006) reported that the benefits of fish intake generally far outweigh the potential risks. Although fish are a dietary source of omega-3 fatty acids, fish do not synthesize them; they obtain them from the algae (microalgae in particular) or plankton in their diets.[112]Fish oil

Fish oil capsules
Marine and freshwater fish oil vary in content of arachidonic acid, EPA and DHA.[113] They also differ in their effects on organ lipids.[113] Not all forms of fish oil may be equally digestible. Of four studies that compare bioavailability of the glyceryl ester form of fish oil vs. the ethyl ester form, two have concluded the natural glyceryl ester form is better, and the other two studies did not find a significant difference. No studies have shown the ethyl ester form to be superior, although it is cheaper to manufacture.[114][115]
Krill
Krill oil is a source of omega-3 fatty acids.[116] The effect of krill oil, at a lower dose of EPA + DHA (62.8%), was demonstrated to be similar to that of fish oil on blood lipid levels and markers of inflammation in healthy humans.[117] While not an endangered species, krill are a mainstay of the diets of many ocean-based species including whales, causing environmental and scientific concerns about their sustainability.[118][119][120]Plant sources
Chia is grown commercially for its seeds rich in ALA.
Flax seeds contain linseed oil which has high ALA content
| Common name | Alternative name | Linnaean name | % ALA |
|---|---|---|---|
| Kiwifruit seed oil | Chinese gooseberry | Actinidia deliciosa | 63[122] |
| Perilla | shiso | Perilla frutescens | 61 |
| Chia seed | chia sage | Salvia hispanica | 58 |
| Flax | linseed | Linum usitatissimum | 53[87] – 59[123] |
| Lingonberry | Cowberry | Vaccinium vitis-idaea | 49 |
| Fig seed oil | Common Fig | Ficus carica | 47.7[124] |
| Camelina | Gold-of-pleasure | Camelina sativa | 36 |
| Purslane | Portulaca | Portulaca oleracea | 35 |
| Black raspberry | Rubus occidentalis | 33 | |
| Hemp | Cannabis sativa | 19 | |
| Canola | mostly Brassica napus | 9[87] – 11 |
Table 2. ALA content as the percentage of the whole food.[87][125]
| Common name | Linnaean name | % ALA |
|---|---|---|
| Flaxseed | Linum usitatissimum | 18.1 |
| Hempseed | Cannabis sativa | 8.7 |
| Butternuts | Juglans cinerea | 8.7 |
| Persian walnuts | Juglans regia | 6.3 |
| Pecan nuts | Carya illinoinensis | 0.6 |
| Hazel nuts | Corylus avellana | 0.1 |
Flaxseed (or linseed) (Linum usitatissimum) and its oil are perhaps the most widely available botanical source of the omega-3 fatty acid ALA. Flaxseed oil consists of approximately 55% ALA, which makes it six times richer than most fish oils in omega-3 fatty acids.[126] A portion of this is converted by the body to EPA and DHA, though the actual converted percentage may differ between men and women.[127]
In 2013 Rothamsted Research in the UK reported they had developed a genetically modified form of the plant Camelina that produced EPA and DHA. Oil from the seeds of this plant contained on average 11% EPA and 8% DHA in one development and 24% EPA in another.[128][129]
Eggs
Eggs produced by hens fed a diet of greens and insects contain higher levels of omega-3 fatty acids than those produced by chickens fed corn or soybeans.[130] In addition to feeding chickens insects and greens, fish oils may be added to their diets to increase the omega-3 fatty acid concentrations in eggs.[131]The addition of flax and canola seeds to the diets of chickens, both good sources of alpha-linolenic acid, increases the omega-3 content of the eggs, predominantly DHA.[132]
The addition of green algae or seaweed to the diets boosts the content of DHA and EPA, which are the forms of omega-3 approved by the FDA for medical claims. A common consumer complaint is "Omega-3 eggs can sometimes have a fishy taste if the hens are fed marine oils".[133]
Meat
Omega-3 fatty acids are formed in the chloroplasts of green leaves and algae. While seaweeds and algae are the source of omega-3 fatty acids present in fish, grass is the source of omega-3 fatty acids present in grass fed animals.[134] When cattle are taken off omega-3 fatty acid rich grass and shipped to a feedlot to be fattened on omega-3 fatty acid deficient grain, they begin losing their store of this beneficial fat. Each day that an animal spends in the feedlot, the amount of omega-3 fatty acids in its meat is diminished.[135]The omega-6:omega-3 ratio of grass-fed beef is about 2:1, making it a more useful source of omega-3 than grain-fed beef, which usually has a ratio of 4:1.[90]
In a 2009 joint study by the USDA and researchers at Clemson University in South Carolina, grass-fed beef was compared with grain-finished beef. The researchers found that grass-finished beef is higher in moisture content, 42.5% lower total lipid content, 54% lower in total fatty acids, 54% higher in beta-carotene, 288% higher in vitamin E (alpha-tocopherol), higher in the B-vitamins thiamin and riboflavin, higher in the minerals calcium, magnesium, and potassium, 193% higher in total omega-3s, 117% higher in CLA (cis-9 trans-11, which is a potential cancer fighter), 90% higher in vaccenic acid (which can be transformed into CLA), lower in the saturated fats linked with heart disease, and has a healthier ratio of omega-6 to omega-3 fatty acids (1.65 vs 4.84). Protein and cholesterol content were equal.[90]
In most countries, commercially available lamb is typically grass-fed, and thus higher in omega-3 than other grain-fed or grain-finished meat sources. In the United States, lamb is often finished (i.e., fattened before slaughter) with grain, resulting in lower omega-3.[136]
The omega-3 content of chicken meat may be enhanced by increasing the animals' dietary intake of grains high in omega-3, such as flax, chia, and canola.[137]
Kangaroo meat is also a source of omega-3, with fillet and steak containing 74 mg per 100 g of raw meat.[138]
Seal oil
Seal oil is a source of EPA, DPA, and DHA. According to Health Canada, it helps to support the development of the brain, eyes, and nerves in children up to 12 years of age.[139] Like all seal products, it is not allowed to be imported into the European Union.[140]Other sources
A recent trend has been to fortify food with omega-3 fatty acid supplements. Global food companies have launched omega-3 fatty acid fortified bread, mayonnaise, pizza, yogurt, orange juice, children's pasta, milk, eggs, popcorn, confections, and infant formula.[citation needed]The microalgae Crypthecodinium cohnii and Schizochytrium are rich sources of DHA but not EPA, and can be produced commercially in bioreactors. Oil from brown algae (kelp) is a source of EPA.[141] The alga Nannochloropsis also has high levels of EPA.[142]
In 2006 the Journal of Dairy Science published a study which found that butter made from the milk of grass-fed cows contains substantially more α-linolenic acid than butter made from the milk of cows that have limited access to pasture.[143]