From Wikipedia, the free encyclopedia
| Type 1 diabetes |
|---|
| Other names | Diabetes mellitus type 1, insulin-dependent diabetes, juvenile diabetes |
|---|
 |
| A blue circle, the symbol for diabetes. |
| Pronunciation | |
|---|
| Specialty | Endocrinology |
|---|
| Symptoms | Frequent urination, increased thirst, increased hunger, weight loss |
|---|
| Complications | Diabetic ketoacidosis, nonketotic hyperosmolar coma, poor healing, cardiovascular disease, damage to the eyes |
|---|
| Usual onset | Relatively short period of time |
|---|
| Duration | Long term |
|---|
| Causes | Body does not produce enough insulin |
|---|
| Risk factors | Family history, celiac disease |
|---|
| Diagnostic method | Blood sugar, A1C |
|---|
| Prevention | Unknown |
|---|
| Treatment | Insulin, diabetic diet, exercise |
|---|
| Frequency | ~7.5% of diabetes cases |
|---|
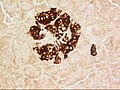
Type 1 diabetes (T1D), previously known as juvenile diabetes, is an autoimmune disease that is a form of diabetes in which very little or no insulin is produced by the islets of Langerhans (containing beta cells) in the pancreas. Insulin is a hormone required for the cells to use blood sugar for energy and it helps regulate normal glucose levels in the bloodstream. Before treatment this results in high blood sugar levels in the body. The common symptoms are frequent urination, increased thirst, increased hunger, and weight loss. Additional symptoms may include blurry vision, tiredness, and slow wound healing. Symptoms typically develop over a short period of time, often a matter of weeks.
The cause of type 1 diabetes is unknown, but it is believed to involve a combination of genetic and environmental factors. Risk factors include having a family member with the condition. The underlying mechanism involves an autoimmune destruction of the insulin-producing beta cells in the pancreas. Diabetes is diagnosed by testing the level of sugar or glycated hemoglobin (HbA1C) in the blood.Type 1 diabetes can be distinguished from type 2 by testing for the presence of autoantibodies.
There is no known way to prevent type 1 diabetes. Treatment with insulin is required for survival. Insulin therapy is usually given by injection just under the skin but can also be delivered by an insulin pump. A diabetic diet and exercise are important parts of management. If left untreated, diabetes can cause many complications. Complications of relatively rapid onset include diabetic ketoacidosis and nonketotic hyperosmolar coma. Long-term complications include heart disease, stroke, kidney failure, foot ulcers and damage to the eyes. Furthermore, since insulin lowers blood sugar levels, complications may arise from low blood sugar if excessive amount of insulin is taken than necessary.
Type 1 diabetes makes up an estimated 5–10% of all diabetes cases.
The number of people affected globally is unknown, although it is
estimated that about 80,000 children develop the disease each year. Within the United States the number of people affected is estimated at one to three million. Rates of disease vary widely, with approximately one new case per 100,000 per year in East Asia and Latin America and around 30 new cases per 100,000 per year in Scandinavia and Kuwait. It typically begins in children and young adults.
Signs and symptoms

Overview of the most significant symptoms of diabetes
A posterior subcapsular
cataract is a rare symptom in those with type 1 DM
The classic symptoms of type 1 diabetes include: polyuria (increased urination), polydipsia (increased thirst), dry mouth, polyphagia (increased hunger), fatigue, and weight loss.
Type 1 diabetes is often diagnosed when diabetic ketoacidosis occurs. The signs and symptoms of diabetic ketoacidosis include dry skin, rapid deep breathing, drowsiness, increased thirst, frequent urination, abdominal pain, and vomiting.
Some people with type 1 diabetes experience dramatic and recurrent swings in glucose levels, often occurring for no apparent reason; this is called "unstable diabetes", "labile diabetes" or "brittle diabetes". The results of such swings can be irregular and unpredictable hyperglycemias, sometimes involving ketoacidosis, and sometimes serious hypoglycemias. Brittle diabetes occurs no more frequently than in 1% to 2% of diabetics.
Type 1 diabetes is associated with alopecia areata (AA). Type 1 diabetes is also more common in the family members of people with AA.
Cause
The cause of type 1 diabetes is not yet known.
A number of explanatory theories have been put forward, and the cause
may be one or more of the following: genetic susceptibility, a
diabetogenic trigger, and exposure to an antigen.
Genetics
Type 1 diabetes is a disease that involves many genes.
The risk of a child developing type 1 diabetes is about 5% if the
father has it, about 8% if a sibling has it, and about 3% if the mother
has it. If one identical twin is affected there is about a 40% to 50% chance the other will be too. Some studies of heritability have estimated it at 80 to 86%.
More than 50 genes are associated with type 1 diabetes. Depending
on locus or combination of loci, they can be dominant, recessive, or
somewhere in between. The strongest gene, IDDM1, is located in the MHC Class II region on chromosome 6, at staining region 6p21. Certain variants of this gene increase the risk for decreased histocompatibility
characteristic of type 1. Such variants include DRB1 0401, DRB1 0402,
DRB1 0405, DQA 0301, DQB1 0302 and DQB1 0201, which are common in North
Americans of European ancestry and in Europeans. Some variants also appear to be protective.
Environmental
There is on the order of a 10-fold difference in occurrence among Caucasians living in different areas of Europe. Environmental triggers and protective factors under research include dietary agents such as proteins in gluten, time of weaning, gut microbiota, viral infections, and bacterial infections like paratuberculosis.
Chemicals and drugs
Some chemicals and drugs selectively destroy pancreatic cells. Pyrinuron
(Vacor), a rodenticide introduced in the United States in 1976,
selectively destroys pancreatic beta cells, resulting in type 1 diabetes
after accidental poisoning. Pyrinuron was withdrawn from the U.S. market in 1979 and it is not approved by the Environmental Protection Agency for use in the U.S. Streptozotocin (Zanosar), an antineoplastic agent, is selectively toxic to the beta cells of the pancreatic islets. It is used in research for inducing type 1 diabetes on rodents and for treating metastatic cancer of the pancreatic islet cells in patients whose cancer cannot be removed by surgery. Other pancreatic problems, including trauma, pancreatitis, or tumors (either malignant or benign) can also lead to loss of insulin production.
Monoclonal antibodies used for the treatment of cancer (checkpoint inhibitors inhibiting PD-1 and PD-L1), especially nivolumab and pembrolizumab have been reported to occasionally induce autoimmune diabetes.
Pathophysiology
The pathophysiology in diabetes type 1 is a destruction of beta cells in the pancreas, regardless of which risk factors or causative entities have been present.
Individual risk factors can have separate pathophysiological
processes to, in turn, cause this beta cell destruction. Still, a
process that appears to be common to most risk factors is a type IV hypersensitivity autoimmune response towards beta cells, involving an expansion of autoreactive CD4+ T helper cells and CD8+ T cells, autoantibody-producing B cells and activation of the innate immune system.
After starting treatment with insulin a person's own insulin levels may temporarily improve. This is believed to be due to altered immunity and is known as the "honeymoon phase".
Alpha cell dysfunction
Onset of autoimmune diabetes is accompanied by impaired ability to regulate the hormone glucagon,
which acts in antagonism with insulin to regulate blood sugar and
metabolism. While the causes and mechanisms are still being studied and
hypotheses abound, what is clear and agreed upon is that progressive
beta cell destruction leads to dysfunction in the neighboring alpha cells
which secrete glucagon, exacerbating excursions away from euglycemia in
both directions; overproduction of glucagon after meals causes sharper
hyperglycemia, and failure to stimulate glucagon upon incipient
hypoglycemia prevents a glucagon-mediated rescue of glucose levels.
Hyperglucagonemia
Onset
of type 1 diabetes is followed by an increase in glucagon secretion
after meals. Increases have been measured up to 37% during the first
year of diagnosis, while c-peptide levels (indicative of islet-derived
insulin), decline by up to 45%.
Insulin production will continue to fall as the immune system follows
its course of progressive beta cell destruction, and islet-derived
insulin will continue to be replaced by therapeutic exogenous insulin.
Simultaneously, there is measurable alpha cell hypertrophy and
hyperplasia in the early overt stage of the disease, leading to expanded
alpha cell mass. This, together with failing beta cell insulin
secretion, begins to account for rising glucagon levels that contribute
to hyperglycemia. Some researchers believe glucagon dysregulation to be the primary cause of early stage hyperglycemia.
Leading hypotheses for the cause of postprandial hyperglucagonemia
suggest that exogenous insulin therapy is inadequate to replace the lost
intraislet signalling to alpha cells previously mediated by beta
cell-derived pulsatile insulin secretion.
Under this working hypothesis intensive insulin therapy has attempted
to mimic natural insulin secretion profiles in exogenous insulin
infusion therapies.
Hypoglycemic glucagon impairment
Hypoglycemia
in type 1 diabetics is often a result of over-administered insulin
therapy, though being in a fasting state, exercising without proper
adjustment of insulin, sleep, and alcohol can also contribute.
The normal counter regulatory responses to hypoglycemia are impaired in
type 1 diabetics. Glucagon secretion is normally increased upon falling
glucose levels, but normal glucagon response to hypoglycemia is blunted
when measured in type 1 diabetics and compared to healthy individuals
experiencing an equal insulin-induced hypoglycemic trigger.
Beta cell glucose sensing and subsequent suppression of administered
insulin secretion is absent, leading to islet hyperinsulinemia which
inhibits glucagon release.
Autonomic inputs to alpha cells are much more important for
glucagon stimulation in the moderate to severe ranges of hypoglycemia,
yet the autonomic response is blunted in a number of ways. Recurrent
hypoglycemia leads to metabolic adjustments in the glucose sensing areas
of the brain, shifting the threshold for counter regulatory activation
of the sympathetic nervous system to lower glucose concentration.
This is known as hypoglycemic unawareness. Subsequent hypoglycemia is
met with impairment in sending of counter regulatory signals to the
islets and adrenal cortex.
This accounts for the lack of glucagon stimulation and epinephrine
release that would normally stimulate and enhance glucose release and
production from the liver, rescuing the diabetic from severe
hypoglycemia, coma, and death. Numerous hypotheses have been produced
in the search for a cellular mechanism of hypoglycemic unawareness, and a
consensus has yet to be reached. The major hypotheses are summarized in the following table:
| Mechanisms of hypoglycemic unawareness
|
| Glycogen supercompensation
|
Increased glycogen stores in astrocytes might contribute supplementary glycosyl units for metabolism, counteracting the central nervous system perception of hypoglycemia.
|
| Enhanced glucose metabolism
|
Altered glucose transport and enhanced metabolic efficiency upon
recurring hypoglycemia relieves oxidative stress that would activate
sympathetic response.
|
| Alternative fuel hypothesis
|
Decreased reliance on glucose, supplementation of lactate from
astrocytes, or ketones meet metabolic demands and reduce stress to
brain.
|
| Brain neuronal communication
|
Hypothalamic inhibitory GABA
normally decreases during hypoglycemia, disinhibiting signals for
sympathetic tone. Recurrent episodes of hypoglycemia result in increased
basal GABA which fails to decrease normally during subsequent
hypoglycemia. Inhibitory tone remains and sympathetic tone is not
increased.
|
In addition, autoimmune diabetes is characterized by a loss of islet specific sympathetic innervation.
This loss constitutes an 80-90% reduction of islet sympathetic nerve
endings, happens early in the progression of the disease, and is
persistent though the life of the patient.
It is linked to the autoimmune aspect of type 1 diabetics and fails to
occur in type 2 diabetics. Early in the autoimmune event, the axon
pruning is activated in islet sympathetic nerves. Increased BDNF and ROS that result from insulitis and beta cell death stimulate the p75 neurotrophin receptor (p75NTR),
which acts to prune off axons. Axons are normally protected from
pruning by activation of tropomyosin receptor kinase A (Trk A) receptors
by NGF,
which in islets is primarily produced by beta cells. Progressive
autoimmune beta cell destruction, therefore, causes both the activation
of pruning factors and the loss of protective factors to the islet
sympathetic nerves. This unique form of neuropathy is a hallmark of type
1 diabetes, and plays a part in the loss of glucagon rescue of severe
hypoglycemia.
Diagnosis
WHO diabetes diagnostic criteria
| Condition
|
2-hour glucose
|
Fasting glucose
|
HbA1c
|
| Unit
|
mmol/L |
mg/dL
|
mmol/L |
mg/dL
|
mmol/mol |
DCCT %
|
| Normal |
< 7.8 |
< 140 |
< 6.1 |
< 110 |
< 42 |
< 6.0
|
| Impaired fasting glycaemia |
< 7.8 |
< 140 |
6.1–7.0 |
110–125 |
42–46 |
6.0–6.4
|
| Impaired glucose tolerance |
≥ 7.8 |
≥ 140 |
< 7.0 |
< 126 |
42–46 |
6.0–6.4
|
| Diabetes mellitus |
≥ 11.1 |
≥ 200 |
≥ 7.0 |
≥ 126 |
≥ 48 |
≥ 6.5
|
Diabetes is characterized by recurrent or persistent hyperglycemia, and is diagnosed by demonstrating any one of the following:
- Fasting plasma glucose level at or above 7.0 mmol/L (126 mg/dL).
- Plasma glucose at or above 11.1 mmol/L (200 mg/dL) two hours after a 75 g oral glucose load as in a glucose tolerance test.
- Symptoms of hyperglycemia and casual plasma glucose at or above 11.1 mmol/L (200 mg/dL).
- Glycated hemoglobin (hemoglobin A1C) at or above 48 mmol/mol (≥ 6.5 DCCT %). (This criterion was recommended by the American Diabetes Association in 2010, although it has yet to be adopted by the WHO.)
About a quarter of people with new type 1 diabetes have developed some degree of diabetic ketoacidosis (a type of metabolic acidosis which is caused by high concentrations of ketone bodies, formed by the breakdown of fatty acids and the deamination of amino acids)
by the time the diabetes is recognized. The diagnosis of other types of
diabetes is usually made in other ways. These include ordinary health
screening, detection of hyperglycemia during other medical
investigations, and secondary symptoms such as vision changes or
unexplained fatigue. Diabetes is often detected when a person suffers a
problem that may be caused by diabetes, such as a heart attack, stroke, neuropathy, poor wound healing or a foot ulcer, certain eye problems, certain fungal infections, or delivering a baby with macrosomia or hypoglycemia (low blood sugar).
A positive result, in the absence of unequivocal hyperglycemia,
should be confirmed by a repeat of any of the above-listed methods on a
different day. Most physicians prefer to measure a fasting glucose level
because of the ease of measurement and the considerable time commitment
of formal glucose tolerance testing, which takes two hours to complete
and offers no prognostic advantage over the fasting test.
According to the current definition, two fasting glucose measurements
above 126 mg/dL (7.0 mmol/L) is considered diagnostic for diabetes.
In type 1, pancreatic beta cells in the islets of Langerhans are destroyed, decreasing endogenous insulin
production. This distinguishes type 1's origin from type 2. Type 2
diabetes is characterized by insulin resistance, while type 1 diabetes
is characterized by insulin deficiency, generally without insulin
resistance. Another hallmark of type 1 diabetes is islet autoreactivity,
which is generally measured by the presence of autoantibodies directed
towards the beta cells.
Autoantibodies
The appearance of diabetes-related autoantibodies has been shown to be able to predict the appearance of diabetes type 1 before any hyperglycemia arises, the main ones being islet cell autoantibodies, insulin autoantibodies, autoantibodies targeting the 65-kDa isoform of glutamic acid decarboxylase (GAD), autoantibodies targeting the phosphatase-related IA-2 molecule, and zinc transporter autoantibodies (ZnT8).
By definition, the diagnosis of diabetes type 1 can be made first at
the appearance of clinical symptoms and/or signs, but the emergence of
autoantibodies may itself be termed "latent autoimmune diabetes".
Not everyone with autoantibodies progresses to diabetes type 1, but the
risk increases with the number of antibody types, with three to four
antibody types giving a risk of progressing to diabetes type 1 of
60–100%.
The time interval from emergence of autoantibodies to clinically
diagnosable diabetes can be a few months in infants and young children,
but in some people, it may take years – in some cases more than 10
years. Islet cell autoantibodies are detected by conventional immunofluorescence, while the rest are measured with specific radiobinding assays.
Prevention
Type 1 diabetes is not currently preventable. Some researchers believe it might be prevented at the latent autoimmune stage, before it starts destroying beta cells.
Immunosuppressive drugs
Cyclosporine A, an immunosuppressive agent, has apparently halted destruction of beta cells (on the basis of reduced insulin usage), but its kidney toxicity and other side effects make it highly inappropriate for long-term use.
Anti-CD3 antibodies, including teplizumab and otelixizumab, had suggested evidence of preserving insulin production (as evidenced by sustained C-peptide production) in newly diagnosed type 1 diabetes patients. A probable mechanism of this effect was believed to be preservation of regulatory T cells that suppress activation of the immune system and thereby maintain immune system homeostasis and tolerance to self-antigens. The duration of the effect is still unknown, however.
In 2011, Phase III studies with otelixizumab and teplizumab both failed
to show clinical efficacy, potentially due to an insufficient dosing
schedule.
An anti-CD20 antibody, rituximab, inhibits B cells and has been shown to provoke C-peptide responses three months after diagnosis of type 1 diabetes, but long-term effects of this have not been reported.
Diet
Some research has suggested breastfeeding decreases the risk in later life and early introduction of gluten-containing cereals in the diet increases the risk of developing islet cell autoantibodies; various other nutritional risk factors are being studied, but no firm evidence has been found.
Giving children 2000 IU of vitamin D
daily during their first year of life is associated with reduced risk
of type 1 diabetes, though the causal relationship is obscure.
Children with antibodies to beta cell proteins (i.e. at early
stages of an immune reaction to them) but no overt diabetes, and treated
with niacinamide (vitamin B3),
had less than half the diabetes onset incidence in a seven-year time
span than did the general population, and an even lower incidence
relative to those with antibodies as above, but who received no
niacinamide.
People with type 1 diabetes and undiagnosed celiac disease have worse glycaemic control and a higher prevalence of nephropathy and retinopathy. Gluten-free diet,
when performed strictly, improves diabetes symptoms and appears to have
a protective effect against developing long-term complications.
Nevertheless, dietary management of both these diseases is challenging
and these patients have poor compliance of the diet.
Management
Diabetes is often managed by a number of health care providers
including a dietitian, nurse educator, eye doctor, endocrinologist, and
podiatrist.
Lifestyle
There is limited evidence for the usefulness of routine use of low-carbohydrate dieting for people with type 1 diabetes. Although for certain individuals it may be feasible to follow a low-carbohydrate regime combined with carefully managed insulin dosing, this is hard to maintain and there are concerns about possible adverse health effects caused by the diet. In general, people with type 1 diabetes are advised to follow an individualized eating plan rather than a pre-decided one.
There are camps for children to teach them how and when to use or monitor their insulin without parental help.
As psychological stress may have a negative effect on diabetes, a
number of measures have been recommended including: exercising, taking
up a new hobby, or joining a charity, among others.
Insulin
Injections of insulin – via subcutaneous injection using either a syringe or using an insulin pump – are necessary for those living with type 1 diabetes because it cannot be treated by diet and exercise alone. Insulin dosage is adjusted taking into account food intake, blood glucose levels and physical activity.
Untreated type 1 diabetes can commonly lead to diabetic ketoacidosis which can result in death. Diabetic ketoacidosis can cause cerebral edema
(accumulation of liquid in the brain). This is a life-threatening issue
and children are at a higher risk for cerebral edema than adults,
causing ketoacidosis to be the most common cause of death in pediatric
diabetes.
Treatment of diabetes focuses on lowering blood sugar or glucose
(BG) to the near normal range, approximately 80–140 mg/dL
(4.4–7.8 mmol/L).
The ultimate goal of normalizing BG is to avoid long-term complications
that affect the nervous system (e.g. peripheral neuropathy leading to
pain and/or loss of feeling in the extremities), and the cardiovascular
system (e.g. heart attacks, vision loss). This level of control over a
prolonged period of time can be varied by a target HbA1c level of less than 7.5%.
There are four main types of insulin: rapid acting insulin,
short-acting insulin, intermediate-acting insulin, and long-acting
insulin. The rapid acting insulin is used as a bolus dosage.
The action onsets in 15 minutes with peak actions in 30 to 90 minutes.
Short acting insulin action onsets within 30 minutes with the peak
action around 2 to 4 hours. Intermediate acting insulin action onsets
within one to two hours with peak action of four to 10 hours.
Long-acting insulin is usually given at the same time once per day.
The action onset is roughly 1 to 2 hours with a sustained action of up
to 24 hours. Some insulins are biosynthetic products produced using
genetic recombination techniques; formerly, cattle or pig insulins were
used, and even sometimes insulin from fish.
People with type 1 diabetes always need to use insulin, but treatment can lead to low BG (hypoglycemia),
i.e. BG less than 70 mg/dL (3.9 mmol/L). Hypoglycemia is a very common
occurrence in people with diabetes, usually the result of a mismatch in
the balance among insulin, food and physical activity. Symptoms include
excess sweating, excessive hunger, fainting, fatigue, lightheadedness
and shakiness.
Mild cases are self-treated by eating or drinking something high in
sugar. Severe cases can lead to unconsciousness and are treated with
intravenous glucose or injections with glucagon. Continuous glucose monitors
can alert patients to the presence of dangerously high or low blood
sugar levels, but continuous glucose monitors still have a margin of
error.
As of 2016 an artificial pancreas continues to look promising with safety issues still being studied. In 2018 they were deemed to be relatively safe.
Pancreas transplantation
In some cases, a pancreas transplant can restore proper glucose regulation. However, the surgery and accompanying immunosuppression required may be more dangerous than continued insulin replacement therapy, so is generally only used with or some time after a kidney transplant. One reason for this is that introducing a new kidney requires taking immunosuppressive drugs
such as cyclosporine, which allows the introduction of a new pancreas
to a person with diabetes without any additional immunosuppressive
therapy. However, pancreas transplants alone may be beneficial in people
with extremely labile type 1 diabetes.
Islet cell transplantation
Islet cell transplantation may be an option for some people with type 1 diabetes that is not well controlled with insulin.
Difficulties include finding donors that are compatible, getting the
new islets to survive, and the side effects from the medications used to
prevent rejection.
Success rates, defined as not needing insulin at 3 years following the
procedure, occurred in 44% of people on registry from 2010. In the United States, as of 2016, it is considered an experimental treatment.
Complications
Complications of poorly managed type 1 diabetes may include cardiovascular disease, diabetic neuropathy, and diabetic retinopathy, among others. However, cardiovascular disease as well as neuropathy may have an autoimmune basis, as well. Women with type 1 DM have a 40% higher risk of death as compared to men with type 1 DM. The life expectancy of an individual with type 1 diabetes is 11 years less for men and 13 years less for women. People with type 1 diabetes are higher risk for other autoimmune diseases, such as autoimmune thyroid disease, celiac disease, rheumatoid arthritis, and lupus.
About 12 percent of people with type 1 diabetes have clinical depression. About 6 percent of people with type 1 diabetes also have celiac disease, but in most cases there are no digestive symptoms or are mistakenly attributed to poor control of diabetes, gastroparesis or diabetic neuropathy.
In most cases, celiac disease is diagnosed after onset of type 1
diabetes. The association of celiac disease with type 1 diabetes
increases the risk of complications, such as retinopathy
and mortality. This association can be explained by shared genetic
factors, and inflammation or nutritional deficiencies caused by
untreated celiac disease, even if type 1 diabetes is diagnosed first.
Urinary tract infection
People with diabetes show an increased rate of urinary tract infection.
The reason is bladder dysfunction is more common in people with
diabetes than people without diabetes due to diabetes nephropathy. When
present, nephropathy can cause a decrease in bladder sensation, which in
turn, can cause increased residual urine, a risk factor for urinary
tract infections.
Sexual dysfunction
Sexual dysfunction
in people with diabetes is often a result of physical factors such as
nerve damage and poor circulation, and psychological factors such as
stress and/or depression caused by the demands of the disease.
Males
The most
common sexual issues in males with diabetes are problems with erections
and ejaculation: "With diabetes, blood vessels supplying the penis’s
erectile tissue can get hard and narrow, preventing the adequate blood
supply needed for a firm erection. The nerve damage caused by poor blood
glucose control can also cause ejaculate to go into the bladder instead
of through the penis during ejaculation, called retrograde ejaculation.
When this happens, semen leaves the body in the urine." Another cause
of erectile dysfunction is reactive oxygen species created as a result
of the disease. Antioxidants can be used to help combat this.
Females
Sexual problems are common in women who have diabetes,
including reduced sensation in the genitals, dryness,
difficulty/inability to orgasm, pain during sex, and decreased libido.
Diabetes sometimes decreases estrogen levels in females, which can
affect vaginal lubrication. Less is known about the correlation between
diabetes and sexual dysfunction in females than in males.
Oral contraceptive pills
can cause blood sugar imbalances in women who have diabetes. Dosage
changes can help address that, at the risk of side effects and
complications.
Women with type 1 diabetes show a higher than normal rate of polycystic ovarian syndrome (PCOS).
The reason may be that the ovaries are exposed to high insulin
concentrations since women with type 1 diabetes can have frequent
hyperglycemia.
Epidemiology
Type 1 diabetes makes up an estimated 5–10% of all diabetes cases or 11–22 million worldwide.
In 2006 it affected 440,000 children under 14 years of age and was the
primary cause of diabetes in those less than 10 years of age. The incidence of type 1 diabetes has been increasing by about 3% per year.
Rates vary widely by country. In Finland, the incidence is a high
of 57 per 100,000 per year, in Japan and China a low of 1 to 3 per
100,000 per year, and in Northern Europe and the U.S., an intermediate
of 8 to 17 per 100,000 per year.
In the United States, type 1 and 2 diabetes affected about
208,000 youths under the age of 20 in 2015. Over 18,000 youths are
diagnosed with Type 1 diabetes every year. Every year about 234,051
Americans die due to diabetes (type I or II) or diabetes-related
complications, with 69,071 having it as the primary cause of death.
In Australia, about one million people have been diagnosed with
diabetes and of this figure 130,000 people have been diagnosed with type
1 diabetes. Australia ranks 6th-highest in the world with children
under 14 years of age. Between 2000 and 2013, 31,895 new cases were
established, with 2,323 in 2013, a rate of 10–13 cases per 100,00 people
each year. Aboriginals and Torres Strait Islander people are less
affected.
History
Type 1 diabetes was described as an autoimmune disease in the 1970s,
based on observations that autoantibodies against islets were discovered
in diabetics with other autoimmune deficiencies.
It was also shown in the 1980s that immunosuppressive therapies could
slow disease progression, further supporting the idea that type 1
diabetes is an autoimmune disorder. The name juvenile diabetes was used earlier as it often first is diagnosed in childhood.
Society and culture
Type 1 and 2 diabetes was estimated to cause $10.5 billion in annual
medical costs ($875 per month per diabetic) and an additional $4.4
billion in indirect costs ($366 per month per person with diabetes) in
the U.S.
In the United States $245 billion every year is attributed to diabetes.
Individuals diagnosed with diabetes have 2.3 times the health care
costs as individuals who do not have diabetes. One in ten health care
dollars are spent on individuals with type 1 and 2 diabetes.
Research
Funding
for research into type 1 diabetes originates from government, industry
(e.g., pharmaceutical companies), and charitable organizations.
Government funding in the United States is distributed via the National Institutes of Health, and in the UK via the National Institute for Health Research or the Medical Research Council. The Juvenile Diabetes Research Foundation
(JDRF), founded by parents of children with type 1 diabetes, is the
world's largest provider of charity-based funding for type 1 diabetes
research. Other charities include the American Diabetes Association, Diabetes UK, Diabetes Research and Wellness Foundation, Diabetes Australia, the Canadian Diabetes Association.
A number of approaches have been explored to understand causes and provide treatments for type 1.
Diet
Data suggest that gliadin (a protein present in gluten) might play a role in the development of type 1 diabetes, but the mechanism is not fully understood. Increased intestinal permeability
caused by gluten and the subsequent loss of intestinal barrier
function, which allows the passage of pro-inflammatory substances into
the blood, may induce the autoimmune response in genetically predisposed
individuals to type 1 diabetes. There is evidence from experiments conducted in animal models that removal of gluten from the diet may prevent the onset of type 1 diabetes but there has been conflicting research in humans.
Virus
One theory proposes that type 1 diabetes is a virus-triggered autoimmune response in which the immune system attacks virus-infected cells along with the beta cells in the pancreas. Several viruses have been implicated, including enteroviruses (especially coxsackievirus B), cytomegalovirus, Epstein–Barr virus, mumps virus, rubella virus and rotavirus, but to date there is no stringent evidence to support this hypothesis in humans.
A 2011 systematic review and meta-analysis showed an association
between enterovirus infections and type 1 diabetes, but other studies
have shown that, rather than triggering an autoimmune process,
enterovirus infections, as coxsackievirus B, could protect against onset
and development of type 1 diabetes. Some studies have found a decreased risk with oral rotavirus vaccine while others found no effect.
Gene therapy
Gene therapy has also been proposed as a possible cure for type 1 diabetes.
Stem cells
Pluripotent stem cells can be used to generate beta cells but previously these cells did not function as well as normal beta cells. In 2014 more mature beta cells were produced which released insulin in response to blood sugar when transplanted into mice. Before these techniques can be used in humans more evidence of safety and effectiveness is needed.
Vaccine
Vaccines are being looked at to treat or prevent type 1 diabetes by inducing immune tolerance to insulin or pancreatic beta cells. While Phase II clinical trials of a vaccine containing alum and recombinant GAD65, an autoantigen involved in type 1 diabetes, were promising, as of 2014 Phase III had failed. As of 2014, other approaches, such as a DNA vaccine encoding proinsulin and a peptide fragment of insulin, were in early clinical development. The rotavirus vaccine and BCG vaccine are associated with a lower risk of type 1 diabetes. Research continues to look at the BCG vaccine in type 1 diabetes as of 2019.