From Wikipedia, the free encyclopedia
In vitro fertilisation (IVF) is a process of fertilisation where an egg is combined with sperm in vitro ("in glass"). The process involves monitoring and stimulating a person's ovulatory process, removing an ovum or ova (egg or eggs) from their ovaries and letting sperm fertilise them in a culture medium in a laboratory. After the fertilised egg (zygote) undergoes embryo culture for 2–6 days, it is implanted in the same or another person's uterus, with the intention of establishing a successful pregnancy.
IVF is a type of assisted reproductive technology used for infertility treatment and gestational surrogacy.
A fertilised egg may be implanted into a surrogate's uterus, and the
resulting child is genetically unrelated to the surrogate. Some
countries have banned or otherwise regulate the availability of IVF
treatment, giving rise to fertility tourism. Restrictions on the availability of IVF include costs and age, in order for a person to carry a healthy pregnancy to term.
In July 1978, Louise Brown was the first child successfully born after her mother received IVF treatment.
Brown was born as a result of natural-cycle IVF, where no stimulation
was made. The procedure took place at Dr Kershaw's Cottage Hospital (now
Dr Kershaw's Hospice) in Royton, Oldham, England. Robert G. Edwards was awarded the Nobel Prize in Physiology or Medicine in 2010. The physiologist co-developed the treatment together with Patrick Steptoe and embryologist Jean Purdy but the latter two were not eligible for consideration as they had died and the Nobel Prize is not awarded posthumously.
With egg donation
and IVF, people who are past their reproductive years, have infertile
partners, have idiopathic female-fertility issues, or have reached menopause can still become pregnant. After the IVF treatment, some couples get pregnant without any fertility treatments.
In 2018, it was estimated that eight million children had been born
worldwide using IVF and other assisted reproduction techniques.
However, a recent study that explores 10 adjuncts with IVF (screening
hysteroscopy, DHEA, testosterone, GH, aspirin, heparin, antioxidants in
males and females, seminal plasma, and PRP) suggests that until more
evidence is done to show that these adjuncts are safe and effective,
they should be avoided.
Terminology
The Latin term in vitro,
meaning "in glass", is used because early biological experiments
involving cultivation of tissues outside the living organism were
carried out in glass containers, such as beakers, test tubes, or Petri
dishes. Today, the scientific term "in vitro" is used to refer to any
biological procedure that is performed outside the organism in which it
would normally have occurred, to distinguish it from an in vivo procedure (such as in vivo fertilisation), where the tissue remains inside the living organism in which it is normally found.
A colloquial term for babies conceived as the result of IVF,
"test tube babies", refers to the tube-shaped containers of glass or
plastic resin, called test tubes, that are commonly used in chemistry and biology labs. However, IVF is usually performed in Petri dishes, which are both wider and shallower and often used to cultivate cultures.
In a broader sense, IVF is a form of assisted reproductive technology (ART).
Medical uses
Indications
IVF may be used to overcome female infertility when it is due to problems with the fallopian tubes, making in vivo fertilisation difficult. It can also assist in male infertility, in those cases where there is a defect in sperm quality; in such situations intracytoplasmic sperm injection
(ICSI) may be used, where a sperm cell is injected directly into the
egg cell. This is used when sperm has difficulty penetrating the egg. In
these cases the partner's or a donor's sperm may be used. ICSI is also
used when sperm numbers are very low. When indicated, the use of ICSI
has been found to increase the success rates of IVF.
According to UK's NICE
guidelines, IVF treatment is appropriate in cases of unexplained
infertility for people who have not conceived after 2 years of regular
unprotected sexual intercourse.
In people with anovulation, it may be an alternative after 7–12 attempted cycles of ovulation induction, since the latter is expensive and more easy to control.
Success rates
IVF
success rates are the percentage of all IVF procedures that result in a
favourable outcome. Depending on the type of calculation used, this
outcome may represent the number of confirmed pregnancies, called the pregnancy rate, or the number of live births, called the live birth rate.
The success rate depends on variable factors such as maternal age,
cause of infertility, embryo status, reproductive history, and lifestyle
factors.
Maternal age: Younger candidates of IVF are more likely to get
pregnant. Females older than 41 are more likely to get pregnant with a
donor egg.
Reproductive history: people who have been previously pregnant
are in many cases more successful with IVF treatments than those who
have never been pregnant.
Due to advances in reproductive technology, live birth rates by
cycle five of IVF have increased from 76% in 2005 to 80% in 2010 despite
a reduction in the number of embryos being transferred (which decreased
the multiple birth rate from 25% to 8%).
Live birth rate
The live birth rate is the percentage of all IVF cycles that lead to a live birth. This rate does not include miscarriage or stillbirth;
multiple-order births, such as twins and triplets, are counted as one
pregnancy. A 2017 summary compiled by the Society for Assisted
Reproductive Technology (SART) which reports the average IVF success
rates in the United States per age group using non-donor eggs compiled
the following data:
|
< 35 |
35–37 |
38–40 |
41–42 |
> 42
|
| Pregnancy rate (%) |
47.1 |
40.6 |
30.9 |
18.8 |
7.6
|
| Live birth rate (%) |
40.5 |
30.2 |
18.7 |
9.1 |
2.9
|
In 2006, Canadian clinics reported a live birth rate of 27%.
Birth rates in younger patients were slightly higher, with a success
rate of 35.3% for those 21 and younger, the youngest group evaluated.
Success rates for older patients were also lower and decrease with age,
with 37-year-olds at 27.4% and no live births for those older than 48,
the oldest group evaluated.
Some clinics exceeded these rates, but it is impossible to determine if
that is due to superior technique or patient selection, since it is
possible to artificially increase success rates by refusing to accept
the most difficult patients or by steering them into oocyte donation
cycles (which are compiled separately). Further, pregnancy rates can be
increased by the placement of several embryos at the risk of increasing
the chance for multiples.
The live birth rates using donor eggs are also given by the SART and include all age groups using either fresh or thawed eggs:
|
Fresh donor egg embryos |
Thawed donor egg embryos
|
| Live birth rate (%) |
40.3 |
36.3
|
Because not each IVF cycle that is started will lead to oocyte
retrieval or embryo transfer, reports of live birth rates need to
specify the denominator, namely IVF cycles started, IVF retrievals, or
embryo transfers. The SART summarised 2008–9 success rates for US
clinics for fresh embryo cycles that did not involve donor eggs and gave
live birth rates by the age of the prospective mother, with a peak at
41.3% per cycle started and 47.3% per embryo transfer for patients under
35 years of age.
IVF attempts in multiple cycles result in increased cumulative
live birth rates. Depending on the demographic group, one study reported
45% to 53% for three attempts, and 51% to 71% to 80% for six attempts.
Effective from 15 February 2021 the majority of Australian IVF
clinics publish their individual success rate online via
YourIVFSuccess.com.au. This site also contains a predictor tool.
Pregnancy rate
Pregnancy rate may be defined in various ways. In the United States, the pregnancy rate used by the SART and the Centers for Disease Control
(and appearing in the table in the Success Rates section above) are
based on fetal heart motion observed in ultrasound examinations.
The 2017 summary compiled by the SART the following data for the United States:
|
<35 |
35-37 |
38-40 |
41-42
|
>42
|
| Pregnancy rate (%) |
47.1 |
40.6 |
30.9 |
18.8
|
7.6
|
In 2006, Canadian clinics reported an average pregnancy rate of 35%.
A French study estimated that 66% of patients starting IVF treatment
finally succeed in having a child (40% during the IVF treatment at the
centre and 26% after IVF discontinuation). Achievement of having a child
after IVF discontinuation was mainly due to adoption (46%) or spontaneous pregnancy (42%).
Miscarriage rate
According to a study done by the Mayo Clinic miscarriage rates for IVF are somewhere between 15 and 25%.
Predictors of success
The main potential factors that influence pregnancy (and live birth) rates in IVF have been suggested to be maternal age, duration of infertility or subfertility, bFSH and number of oocytes, all reflecting ovarian function. Optimal woman's age is 23–39 years at time of treatment.
Biomarkers that affect the pregnancy chances of IVF include:
- Antral follicle count, with higher count giving higher success rates.
- Anti-Müllerian hormone levels, with higher levels indicating higher chances of pregnancy, as well as of live birth after IVF, even after adjusting for age.
- Factors of semen quality for the sperm provider.
- Level of DNA fragmentation as measured, e.g. by Comet assay, advanced maternal age and semen quality.
- People with ovary-specific FMR1 genotypes including het-norm/low have significantly decreased pregnancy chances in IVF.
- Progesterone elevation on the day of induction of final maturation
is associated with lower pregnancy rates in IVF cycles in people
undergoing ovarian stimulation using GnRH analogues and gonadotrophins. At this time, compared to a progesterone level below 0.8 ng/ml, a level between 0.8 and 1.1 ng/ml confers an odds ratio
of pregnancy of approximately 0.8, and a level between 1.2 and
3.0 ng/ml confers an odds ratio of pregnancy of between 0.6 and 0.7.
On the other hand, progesterone elevation does not seem to confer a
decreased chance of pregnancy in frozen–thawed cycles and cycles with
egg donation.
- Characteristics of cells from the cumulus oophorus and the membrana granulosa, which are easily aspirated during oocyte retrieval.
These cells are closely associated with the oocyte and share the same
microenvironment, and the rate of expression of certain genes in such
cells are associated with higher or lower pregnancy rate.
- An endometrial thickness (EMT) of less than 7 mm decreases the
pregnancy rate by an odds ratio of approximately 0.4 compared to an EMT
of over 7 mm. However, such low thickness rarely occurs, and any routine
use of this parameter is regarded as not justified.
Other determinants of outcome of IVF include:
- As the maternal age increases, the likelihood of conception decreases and the chance of miscarriage increases.
- With increasing paternal age, especially 50 years and older, the rate of blastocyst formation decreases.
- Tobacco smoking reduces the chances of IVF producing a live birth by 34% and increases the risk of an IVF pregnancy miscarrying by 30%.
- A body mass index
(BMI) over 27 causes a 33% decrease in likelihood to have a live birth
after the first cycle of IVF, compared to those with a BMI between 20
and 27. Also, pregnant females who are obese have higher rates of miscarriage, gestational diabetes, hypertension, thromboembolism and problems during delivery, as well as leading to an increased risk of fetal congenital abnormality. Ideal body mass index is 19–30.
- Salpingectomy or laparoscopic tubal occlusion before IVF treatment increases chances for people with hydrosalpinges.
- Success with previous pregnancy and/or live birth increases chances.
- Low alcohol/caffeine intake increases success rate
- The number of embryos transferred in the treatment cycle
- Embryo quality
- Some studies also suggest that autoimmune disease may also play a role in decreasing IVF success rates by interfering with proper implantation of the embryo after transfer.
Aspirin is sometimes prescribed to people for the purpose of increasing the chances of conception by IVF, but as of 2016 there was no evidence to show that it is safe and effective.
A 2013 review and meta analysis of randomised controlled trials of acupuncture as an adjuvant therapy
in IVF found no overall benefit, and concluded that an apparent benefit
detected in a subset of published trials where the control group (those
not using acupuncture) experienced a lower than average rate of
pregnancy requires further study, due to the possibility of publication bias and other factors.
A Cochrane review
came to the result that endometrial injury performed in the month prior
to ovarian induction appeared to increase both the live birth rate and
clinical pregnancy rate in IVF compared with no endometrial injury.
There was no evidence of a difference between the groups in miscarriage,
multiple pregnancy or bleeding rates. Evidence suggested that
endometrial injury on the day of oocyte retrieval was associated with a
lower live birth or ongoing pregnancy rate.
For people, intake of antioxidants (such as N-acetyl-cysteine, melatonin, vitamin A, vitamin C, vitamin E, folic acid, myo-inositol, zinc or selenium) has not been associated with a significantly increased live birth rate or clinical pregnancy rate in IVF according to Cochrane reviews.
The review found that oral antioxidants given to men in couples with
male factor or unexplained subfertility may improve live birth rates,
but more evidence is needed.
A Cochrane review
in 2015 came to the result that there is no evidence identified
regarding the effect of preconception lifestyle advice on the chance of a
live birth outcome.
Complications
Multiple births
The major complication of IVF is the risk of multiple births.
This is directly related to the practice of transferring multiple
embryos at embryo transfer. Multiple births are related to increased
risk of pregnancy loss, obstetrical complications, prematurity,
and neonatal morbidity with the potential for long term damage. Strict
limits on the number of embryos that may be transferred have been
enacted in some countries (e.g. Britain, Belgium) to reduce the risk of
high-order multiples (triplets or more), but are not universally
followed or accepted. Spontaneous splitting of embryos in the womb after
transfer can occur, but this is rare and would lead to identical twins.
A double blind, randomised study followed IVF pregnancies that resulted
in 73 infants (33 boys and 40 girls) and reported that 8.7% of
singleton infants and 54.2% of twins had a birth weight of less than
2,500 grams (5.5 lb).
There is some evidence that making a double embryo transfer during one
cycle achieves a higher live birth rate than a single embryo transfer;
but making two single embryo transfers in two cycles has the same live
birth rate and would avoid multiple pregnancies.
Sex ratio distortions
Certain kinds of IVF, in particular ICSI (first applied in 1991) and blastocyst transfer (first applied in 1984) have been shown to lead to distortions in the sex ratio
at birth. ICSI leads to slightly more female births (51.3% female)
while blastocyst transfer leads to significantly more boys (56.1% male)
being born. Standard IVF done at the second or third day leads to a
normal sex ratio.
Epigenetic modifications caused by extended culture leading to
the death of more female embryos has been theorised as the reason why
blastocyst transfer leads to a higher male sex ratio, however adding
retinoic acid to the culture can bring this ratio back to normal.
Spread of infectious disease
By sperm washing,
the risk that a chronic disease in the male providing the sperm would
infect the female or offspring can be brought to negligible levels.
In males with hepatitis B,
The Practice Committee of the American Society for Reproductive
Medicine advises that sperm washing is not necessary in IVF to prevent
transmission, unless the female partner has not been effectively
vaccinated. In females with hepatitis B, the risk of vertical transmission during IVF is no different from the risk in spontaneous conception. However, there is not enough evidence to say that ICSI procedures are safe in females with hepatitis B in regard to vertical transmission to the offspring.
Regarding potential spread of HIV/AIDS,
Japan's government prohibited the use of IVF procedures for couples in
which both partners are infected with HIV. Despite the fact that the
ethics committees previously allowed the Ogikubo, Tokyo Hospital, located in Tokyo, to use IVF for couples with HIV, the Ministry of Health, Labour and Welfare
of Japan decided to block the practice. Hideji Hanabusa, the vice
president of the Ogikubo Hospital, states that together with his
colleagues, he managed to develop a method through which scientists are
able to remove HIV from sperm.
Other risks to the egg provider/retriever
A risk of ovarian stimulation is the development of ovarian hyperstimulation syndrome, particularly if hCG is used for inducing final oocyte maturation.
This results in swollen, painful ovaries. It occurs in 30% of patients.
Mild cases can be treated with over the counter medications and cases
can be resolved in the absence of pregnancy. In moderate cases, ovaries
swell and fluid accumulated in the abdominal cavities and may have
symptoms of heartburn, gas, nausea or loss of appetite. In severe cases
patients have sudden excess abdominal pain, nausea, vomiting and will
result in hospitalisation.
During egg retrieval, there exists a small chance of bleeding,
infection, and damage to surrounding structures such as bowel and
bladder (transvaginal ultrasound aspiration) as well as difficulty in
breathing, chest infection, allergic reactions to medication, or nerve
damage (laparoscopy).
Ectopic pregnancy
may also occur if a fertilised egg develops outside the uterus, usually
in the fallopian tubes and requires immediate destruction of the fetus.
IVF does not seem to be associated with an elevated risk of cervical cancer, nor with ovarian cancer or endometrial cancer when neutralising the confounder of infertility itself. Nor does it seem to impart any increased risk for breast cancer.
Regardless of pregnancy result, IVF treatment is usually stressful for patients. Neuroticism and the use of escapist coping strategies are associated with a higher degree of distress, while the presence of social support has a relieving effect. A negative pregnancy test after IVF is associated with an increased risk for depression in women, but not with any increased risk of developing anxiety disorders. Pregnancy test results do not seem to be a risk factor for depression or anxiety among men.
Studies show that there is an increased risk of venous thrombosis or pulmonary embolism during the first trimester of IVF.
When looking at long-term studies comparing people who received or did
not receive IVF, there seems to be no correlation with increased risk
of cardiac events. There are more ongoing studies to solidify this.
Spontaneous pregnancy has occurred after successful and unsuccessful IVF treatments. Within 2 years of delivering an infant conceived through IVF, subfertile couples had a conception rate of 18%.
Birth defects
A review in 2013 came to the result that infants resulting from IVF (with or without ICSI) have a relative risk of birth defects of 1.32 (95% confidence interval 1.24–1.42) compared to naturally conceived infants.
In 2008, an analysis of the data of the National Birth Defects Study in
the US found that certain birth defects were significantly more common
in infants conceived through IVF, notably septal heart defects, cleft lip with or without cleft palate, esophageal atresia, and anorectal atresia; the mechanism of causality is unclear.
However, in a population-wide cohort study of 308,974 births (with
6,163 using assisted reproductive technology and following children from
birth to age five) researchers found: "The increased risk of birth
defects associated with IVF was no longer significant after adjustment
for parental factors."
Parental factors included known independent risks for birth defects
such as maternal age, smoking status, etc. Multivariate correction did
not remove the significance of the association of birth defects and ICSI
(corrected odds ratio 1.57), although the authors speculate that
underlying male infertility factors (which would be associated with the
use of ICSI) may contribute to this observation and were not able to
correct for these confounders. The authors also found that a history of
infertility elevated risk itself in the absence of any treatment (odds
ratio 1.29), consistent with a Danish national registry study and "implicates patient factors in this increased risk." The authors of
the Danish national registry study speculate: "our results suggest that
the reported increased prevalence of congenital malformations seen in
singletons born after assisted reproductive technology is partly due to
the underlying infertility or its determinants."
Other risks to the offspring
If the underlying infertility is related to abnormalities in spermatogenesis, it is plausible, but too early to examine that male offspring are at higher risk for sperm abnormalities.
IVF does not seem to confer any risks regarding cognitive development, school performance, social functioning, and behaviour.
Also, IVF infants are known to be as securely attached to their parents
as those who were naturally conceived, and IVF adolescents are as
well-adjusted as those who have been naturally conceived.
Limited long-term follow-up data suggest that IVF may be associated with an increased incidence of hypertension, impaired fasting glucose, increase in total body fat composition, advancement of bone age, subclinical thyroid disorder, early adulthood clinical depression and binge drinking in the offspring.
It is not known, however, whether these potential associations are
caused by the IVF procedure in itself, by adverse obstetric outcomes
associated with IVF, by the genetic origin of the children or by yet
unknown IVF-associated causes.
Increases in embryo manipulation during IVF result in more deviant
fetal growth curves, but birth weight does not seem to be a reliable
marker of fetal stress.
IVF, including ICSI, is associated with an increased risk of imprinting disorders (including Prader-Willi syndrome and Angelman syndrome), with an odds ratio of 3.7 (95% confidence interval 1.4 to 9.7).
An IVF-associated incidence of cerebral palsy and neurodevelopmental delay are believed to be related to the confounders of prematurity and low birthweight. Similarly, an IVF-associated incidence of autism and attention-deficit disorder are believed to be related to confounders of maternal and obstetric factors.
Overall, IVF does not cause an increased risk of childhood cancer. Studies have shown a decrease in the risk of certain cancers and an increased risks of certain others including retinoblastoma, hepatoblastoma and rhabdomyosarcoma.
Method
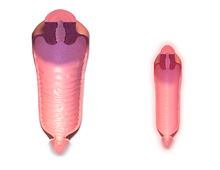
A depiction of the procedure of in-vitro fertilisation.
Theoretically, IVF could be performed by collecting the contents from
a woman's fallopian tubes or uterus after natural ovulation, mixing it
with sperm,
and reinserting the fertilised ova into the uterus. However, without
additional techniques, the chances of pregnancy would be extremely
small. The additional techniques that are routinely used in IVF include ovarian hyperstimulation to generate multiple eggs, ultrasound-guided transvaginal oocyte retrieval directly from the ovaries, co-incubation of eggs and sperm, as well as culture and selection of resultant embryos before embryo transfer into a uterus.
Ovarian hyperstimulation
Ovarian hyperstimulation is the stimulation to induce development of
multiple follicles of the ovaries. It should start with response
prediction by e.g. age, antral follicle count and level of anti-Müllerian hormone.
The resulting prediction of e.g. poor or hyper-response to ovarian
hyperstimulation determines the protocol and dosage for ovarian
hyperstimulation.
Ovarian hyperstimulation also includes suppression of spontaneous
ovulation, for which two main methods are available: Using a (usually
longer) GnRH agonist protocol or a (usually shorter) GnRH antagonist protocol.
In a standard long GnRH agonist protocol the day when hyperstimulation
treatment is started and the expected day of later oocyte retrieval can
be chosen to conform to personal choice, while in a GnRH antagonist
protocol it must be adapted to the spontaneous onset of the previous
menstruation. On the other hand, the GnRH antagonist protocol has a
lower risk of ovarian hyperstimulation syndrome (OHSS), which is a life-threatening complication.
For the ovarian hyperstimulation in itself, injectable gonadotropins (usually FSH analogues) are generally used under close monitoring. Such monitoring frequently checks the estradiol level and, by means of gynecologic ultrasonography, follicular growth. Typically approximately 10 days of injections will be necessary.
Natural IVF
There are several methods termed natural cycle IVF:
IVF using no drugs for ovarian hyperstimulation was the method for the conception of Louise Brown.
This method can be successfully used when people want to avoid taking
ovarian stimulating drugs with its associated side-effects. HFEA has estimated the live birth rate to be approximately 1.3% per IVF cycle using no hyperstimulation drugs for people aged between 40 and 42.
Mild IVF
is a method where a small dose of ovarian stimulating drugs are used
for a short duration during a woman's natural cycle aimed at producing
2–7 eggs and creating healthy embryos. This method appears to be an
advance in the field to reduce complications and side-effects for people
and it is aimed at quality, and not quantity of eggs and embryos. One
study comparing a mild treatment (mild ovarian stimulation with GnRH
antagonist co-treatment combined with single embryo transfer) to a standard treatment (stimulation with a GnRH agonist
long-protocol and transfer of two embryos) came to the result that the
proportions of cumulative pregnancies that resulted in term live birth after 1 year were 43.4% with mild treatment and 44.7% with standard treatment. Mild IVF can be cheaper than conventional IVF and with a significantly reduced risk of multiple gestation and OHSS.
Final maturation induction
When the ovarian follicles have reached a certain degree of development, induction of final oocyte maturation is performed, generally by an injection of human chorionic gonadotropin (hCG). Commonly, this is known as the "trigger shot." hCG acts as an analogue of luteinising hormone, and ovulation would occur between 38 and 40 hours after a single HCG injection,
but the egg retrieval is performed at a time usually between 34 and 36
hours after hCG injection, that is, just prior to when the follicles
would rupture. This avails for scheduling the egg retrieval procedure at
a time where the eggs are fully mature. HCG injection confers a risk of
ovarian hyperstimulation syndrome. Using a GnRH agonist
instead of hCG eliminates most of the risk of ovarian hyperstimulation
syndrome, but with a reduced delivery rate if the embryos are
transferred fresh. For this reason, many centers will freeze all oocytes or embryos following agonist trigger.
Egg retrieval
The eggs are retrieved from the patient using a transvaginal technique called transvaginal oocyte retrieval,
involving an ultrasound-guided needle piercing the vaginal wall to
reach the ovaries. Through this needle follicles can be aspirated, and
the follicular fluid is passed to an embryologist to identify ova. It is
common to remove between ten and thirty eggs. The retrieval procedure
usually takes between 20 and 40 minutes, depending on the number of
mature follicles, and is usually done under conscious sedation or general anaesthesia.
Egg and sperm preparation
In the laboratory, for ICSI treatments, the identified eggs are stripped of surrounding cells (also known as cumulus cells) and prepared for fertilisation. An oocyte selection
may be performed prior to fertilisation to select eggs that can be
fertilized, as it is required they are in metaphase II. There are cases
in which if oocytes are in the metaphase I stage, they can be kept being
cultured so as to undergo a posterior sperm injection. In the meantime,
semen is prepared for fertilisation by removing inactive cells and seminal fluid in a process called sperm washing. If semen is being provided by a sperm donor, it will usually have been prepared for treatment before being frozen and quarantined, and it will be thawed ready for use.
Co-incubation
The sperm and the egg are incubated together at a ratio of about 75,000:1 in a culture media in order for the actual fertilisation
to take place. A review in 2013 came to the result that a duration of
this co-incubation of about 1 to 4 hours results in significantly higher
pregnancy rates than 16 to 24 hours. In most cases, the egg will be fertilised during co-incubation and will show two pronuclei. In certain situations, such as low sperm count or motility, a single sperm may be injected directly into the egg using intracytoplasmic sperm injection
(ICSI). The fertilised egg is passed to a special growth medium and
left for about 48 hours until the egg consists of six to eight cells.
In gamete intrafallopian transfer,
eggs are removed from the woman and placed in one of the fallopian
tubes, along with the man's sperm. This allows fertilisation to take
place inside the woman's body. Therefore, this variation is actually an
in vivo fertilisation, not in vitro.
Embryo culture
The main durations of embryo culture are until cleavage stage (day two to four after co-incubation) or the blastocyst stage (day five or six after co-incubation). Embryo culture until the blastocyst stage confers a significant increase in live birth rate per embryo transfer, but also confers a decreased number of embryos available for transfer and embryo cryopreservation, so the cumulative clinical pregnancy rates are increased with cleavage stage transfer. Transfer day two instead of day three after fertilisation has no differences in live birth rate. There are significantly higher odds of preterm birth (odds ratio 1.3) and congenital anomalies (odds ratio 1.3) among births having from embryos cultured until the blastocyst stage compared with cleavage stage.
Embryo selection
Laboratories have developed grading methods to judge ovocyte and embryo quality. In order to optimise pregnancy rates, there is significant evidence that a morphological scoring system is the best strategy for the selection of embryos. Since 2009 where the first time-lapse microscopy system for IVF was approved for clinical use, morphokinetic scoring systems has shown to improve to pregnancy rates further. However, when all different types of time-lapse embryo imaging
devices, with or without morphokinetic scoring systems, are compared
against conventional embryo assessment for IVF, there is insufficient
evidence of a difference in live-birth, pregnancy, stillbirth or
miscarriage to choose between them.
Active efforts to develop a more accurate embryo selection analysis
based on Artificial Intelligence and Deep Learning are underway. Embryo Ranking Intelligent Classification Assistant (ERICA),
is a clear example. This Deep Learning software substitutes manual
classifications with a ranking system based on an individual embryo's
predicted genetic status in a non-invasive fashion. Studies on this area are still pending and current feasibility studies support its potential.
Embryo transfer
The number to be transferred depends on the number available, the age
of the woman and other health and diagnostic factors. In countries such
as Canada, the UK, Australia and New Zealand, a maximum of two embryos
are transferred except in unusual circumstances. In the UK and according
to HFEA
regulations, a woman over 40 may have up to three embryos transferred,
whereas in the US, there is no legal limit on the number of embryos
which may be transferred, although medical associations have provided
practice guidelines. Most clinics and country regulatory bodies seek to
minimise the risk of multiple pregnancy, as it is not uncommon for
multiple embryos to implant if multiple embryos are transferred. Embryos
are transferred to the patient's uterus through a thin, plastic catheter, which goes through her vagina and cervix. Several embryos may be passed into the uterus to improve chances of implantation and pregnancy.
Luteal support
Luteal support is the administration of medication, generally progesterone, progestins, hCG, or GnRH agonists, and often accompanied by estradiol, to increase the success rate of implantation and early embryogenesis, thereby complementing and/or supporting the function of the corpus luteum. A Cochrane review found that hCG or progesterone given during the luteal phase may be associated with higher rates of live birth or ongoing pregnancy, but that the evidence is not conclusive. Co-treatment with GnRH agonists appears to improve outcomes, by a live birth rate RD of +16% (95% confidence interval +10 to +22%). On the other hand, growth hormone or aspirin as adjunctive medication in IVF have no evidence of overall benefit.
Expansions
There
are various expansions or additional techniques that can be applied in
IVF, which are usually not necessary for the IVF procedure itself, but
would be virtually impossible or technically difficult to perform
without concomitantly performing methods of IVF.
Preimplantation genetic screening or diagnosis
Preimplantation genetic screening
(PGS) or preimplantation genetic diagnosis (PGD) has been suggested to
be able to be used in IVF to select an embryo that appears to have the
greatest chances for successful pregnancy. However, a systematic review
and meta-analysis of existing randomised controlled trials came to the result that there is no evidence of a beneficial effect of PGS with cleavage-stage biopsy as measured by live birth rate. On the contrary, for people of advanced maternal age, PGS with cleavage-stage biopsy significantly lowers the live birth rate. Technical drawbacks, such as the invasiveness of the biopsy, and non-representative samples because of mosaicism are the major underlying factors for inefficacy of PGS.
Still, as an expansion of IVF, patients who can benefit from PGS/PGD include:
- Couples who have a family history of inherited disease
- Couples who want prenatal sex discernment. This can be used to diagnose monogenic disorders with sex linkage. It can potentially be used for sex selection, wherein a fetus is aborted if having an undesired sex.
- Couples who already have a child with an incurable disease and need
compatible cells from a second healthy child to cure the first,
resulting in a "saviour sibling" that matches the sick child in HLA type.
PGS screens for numeral chromosomal abnormalities while PGD diagnosis
the specific molecular defect of the inherited disease. In both PGS and
PGD, individual cells from a pre-embryo, or preferably trophectoderm
cells biopsied from a blastocyst,
are analysed during the IVF process. Before the transfer of a
pre-embryo back to a woman's uterus, one or two cells are removed from
the pre-embryos (8-cell stage), or preferably from a blastocyst.
These cells are then evaluated for normality. Typically within one to
two days, following completion of the evaluation, only the normal
pre-embryos are transferred back to the woman's uterus. Alternatively, a
blastocyst can be cryopreserved via vitrification and transferred at a
later date to the uterus. In addition, PGS can significantly reduce the
risk of multiple pregnancies because fewer embryos, ideally just one,
are needed for implantation.
Cryopreservation
Cryopreservation can be performed as oocyte cryopreservation before fertilisation, or as embryo cryopreservation after fertilisation.
The Rand Consulting Group has estimated there to be 400,000 frozen embryos in the United States in 2006.
The advantage is that patients who fail to conceive may become pregnant
using such embryos without having to go through a full IVF cycle. Or,
if pregnancy occurred, they could return later for another pregnancy.
Spare oocytes or embryos resulting from fertility treatments may be used
for oocyte donation or embryo donation
to another woman or couple, and embryos may be created, frozen and
stored specifically for transfer and donation by using donor eggs and
sperm. Also, oocyte cryopreservation can be used for people who are
likely to lose their ovarian reserve due to undergoing chemotherapy.
By 2017, many centers have adopted embryo cryopreservation as
their primary IVF therapy, and perform few or no fresh embryo transfers.
The two main reasons for this have been better endometrial receptivity
when embryos are transferred in cycles without exposure to ovarian
stimulation and also the ability to store the embryos while awaiting the
results of pre-implantation genetic testing.
The outcome from using cryopreserved embryos has uniformly been
positive with no increase in birth defects or development abnormalities.
Other expansions
- Intracytoplasmic sperm injection (ICSI) is where a single sperm is injected directly into an egg.
Its main usage as an expansion of IVF is to overcome male infertility
problems, although it may also be used where eggs cannot easily be
penetrated by sperm, and occasionally in conjunction with sperm donation. It can be used in teratozoospermia, since once the egg is fertilised abnormal sperm morphology does not appear to influence blastocyst development or blastocyst morphology.
- Additional methods of embryo profiling. For example, methods are emerging in making comprehensive analyses of up to entire genomes, transcriptomes, proteomes and metabolomes
which may be used to score embryos by comparing the patterns with ones
that have previously been found among embryos in successful versus
unsuccessful pregnancies.
- Assisted zona hatching
(AZH) can be performed shortly before the embryo is transferred to the
uterus. A small opening is made in the outer layer surrounding the egg
in order to help the embryo hatch out and aid in the implantation
process of the growing embryo.
- In egg donation and embryo donation,
the resultant embryo after fertilisation is inserted in another woman
than the one providing the eggs. These are resources for people with no
eggs due to surgery, chemotherapy, or genetic causes; or with poor egg
quality, previously unsuccessful IVF cycles or advanced maternal age.
In the egg donor process, eggs are retrieved from a donor's ovaries,
fertilised in the laboratory with the sperm from the recipient's
partner, and the resulting healthy embryos are returned to the
recipient's uterus.
- In oocyte selection, the oocytes with optimal chances of live birth can be chosen. It can also be used as a means of preimplantation genetic screening.
- Embryo splitting can be used for twinning to increase the number of available embryos.
- Cytoplasmic transfer is where the cytoplasm from a donor egg is injected into an egg with compromised mitochondria. The resulting egg is then fertilised with sperm and implanted in a womb, usually that of the woman who provided the recipient egg and nuclear DNA. Cytoplasmic transfer was created to aid people who experience infertility due to deficient or damaged mitochondria, contained within an egg's cytoplasm.
Leftover embryos or eggs
There may be leftover embryos or eggs from IVF procedures if the
woman for whom they were originally created has successfully carried one
or more pregnancies to term, and no longer wishes to use them. With the
woman's or couple's permission, these may be donated to help other
people or couples as a means of third party reproduction.
In embryo donation, these extra embryos are given to other couples or people for transfer,
with the goal of producing a successful pregnancy. Embryo recipients
typically have genetic issues or poor-quality embryos or eggs of their
own. The resulting child is considered the child of the woman who
carries it and gives birth, and not the child of the donor, the same as
occurs with egg donation or sperm donation.
Typically, genetic parents donate the eggs or embryos to a fertility clinic where they are preserved by oocyte cryopreservation or embryo cryopreservation
until a carrier is found for them. Typically the process of matching
the donation with the prospective parents is conducted by the agency
itself, at which time the clinic transfers ownership of the embryos to
the prospective parents.
In the United States, people seeking to be an embryo recipient undergo infectious disease screening required by the Food and Drug Administration
(FDA), and reproductive tests to determine the best placement location
and cycle timing before the actual embryo transfer occurs. The amount of
screening the embryo has already undergone is largely dependent on the
genetic parents' own IVF clinic and process. The embryo recipient may
elect to have her own embryologist conduct further testing.
Alternatives to donating unused embryos are destroying them (or
having them implanted at a time when pregnancy is very unlikely), keeping them frozen indefinitely, or donating them for use in research (which results in their unviability). Individual moral views on disposing of leftover embryos may depend on personal views on the beginning of human personhood and the definition and/or value of potential future persons,
and on the value that is given to fundamental research questions. Some
people believe donation of leftover embryos for research is a good
alternative to discarding the embryos when patients receive proper,
honest and clear information about the research project, the procedures
and the scientific values.
History
The first successful birth of a child after IVF treatment, Louise Brown,
occurred in 1978. Louise Brown was born as a result of natural cycle
IVF where no stimulation was made. The procedure took place at Dr
Kershaw's Cottage Hospital (now Dr Kershaw's Hospice) in Royton, Oldham, England. Robert G. Edwards was awarded the Nobel Prize in Physiology or Medicine in 2010, the physiologist who co-developed the treatment together with Patrick Steptoe and embryologist Jean Purdy; Steptoe and Purdy were not eligible for consideration as the Nobel Prize is not awarded posthumously.
The second successful birth of a test tube baby occurred in India just 67 days after Louise Brown was born. The girl, named Durga conceived in vitro using a method developed independently by Dr. Subhash Mukhopadhyay, a physician and researcher from Kolkata, India.
With egg donation
and IVF, people who are past their reproductive years, have infertile
male partners, have idiopathic female-fertility issues, or have reached menopause can still become pregnant. Adriana Iliescu
held the record as the oldest woman to give birth using IVF and a donor
egg, when she gave birth in 2004 at the age of 66, a record passed in
2006. After the IVF treatment some couples are able to get pregnant
without any fertility treatments.
In 2018 it was estimated that eight million children had been born
worldwide using IVF and other assisted reproduction techniques.
Ethics
Mix-ups
In
some cases, laboratory mix-ups (misidentified gametes, transfer of
wrong embryos) have occurred, leading to legal action against the IVF
provider and complex paternity suits. An example is the case of a woman
in California who received the embryo of another couple and was notified
of this mistake after the birth of her son. This has led to many authorities and individual clinics implementing procedures to minimise the risk of such mix-ups. The HFEA,
for example, requires clinics to use a double witnessing system, the
identity of specimens is checked by two people at each point at which
specimens are transferred. Alternatively, technological solutions are
gaining favour, to reduce the manpower cost of manual double witnessing,
and to further reduce risks with uniquely numbered RFID
tags which can be identified by readers connected to a computer. The
computer tracks specimens throughout the process and alerts the
embryologist if non-matching specimens are identified. Although the use
of RFID tracking has expanded in the US, it is still not widely adopted.
Preimplantation genetic diagnosis or screening
While
PGD was originally designed to screen for embryos carrying hereditary
genetic diseases, the method has been applied to select features that
are unrelated to diseases, thus raising ethical questions. Examples of
such cases include the selection of embryos based on histocompatibility (HLA) for the donation of tissues to a sick family member, the diagnosis of genetic susceptibility to disease, and sex selection.
These examples raise ethical issues because of the morality of eugenics.
It becomes frowned upon because of the advantage of being able to
eliminate unwanted traits and selecting desired traits. By using PGD,
individuals are given the opportunity to create a human life unethically
and rely on science and not by natural selection.
For example, a deaf British couple, Tom and Paula Lichy, have petitioned to create a deaf baby using IVF. Some medical ethicists have been very critical of this approach. Jacob M. Appel
wrote that "intentionally culling out blind or deaf embryos might
prevent considerable future suffering, while a policy that allowed deaf
or blind parents to select for such traits intentionally would be far more troublesome."
Profit desire of the industry
In 2008, a California physician transferred 12 embryos to a woman who gave birth to octuplets (Suleman octuplets).
This led to accusations that a doctor is willing to endanger the health
and even life of people in order to gain money. Robert Winston,
professor of fertility studies at Imperial College London, had called
the industry "corrupt" and "greedy" stating that "one of the major
problems facing us in healthcare is that IVF has become a massive
commercial industry," and that "what has happened, of course, is that
money is corrupting this whole technology", and accused authorities of
failing to protect couples from exploitation: "The regulatory authority
has done a consistently bad job. It's not prevented the exploitation of
people, it's not put out very good information to couples, it's not
limited the number of unscientific treatments people have access to". The IVF industry has been described as a market-driven construction of health, medicine and the human body.
In the US, the Copyright Clause
provides innovators with a temporary monopoly over their respective
work. As a result, IVF is prohibitively expensive for patients as
providers have to also cover the costs of patents. For example, 23andMe has patented a process used to calculate the probability of gene inheritance.
The industry has been accused of making unscientific claims, and
distorting facts relating to infertility, in particular through widely
exaggerated claims about how common infertility is in society, in an
attempt to get as many couples as possible and as soon as possible to
try treatments (rather than trying to conceive naturally for a longer
time). This risks removing infertility from its social context and
reducing the experience to a simple biological malfunction, which not
only can be treated through bio-medical procedures, but should be treated by them.
Indeed, there are serious concerns about the overuse of treatments, for
instance Dr Sami David, a fertility specialist, has expressed
disappointment over the current state of the industry, and said many
procedures are unnecessary; he said: "It's being the first choice of
treatment rather than the last choice. When it was first opening up in
late 1970s, early 80s, it was meant to be the last resort. Now it's a
first resort. I think that it can harm women in the long run."
IVF thus raises ethical issues concerning the abuse of bio-medical
facts to 'sell' corrective procedures and treatments for conditions that
deviate from a constructed ideal of the 'healthy' or 'normal' body
i.e., fertile females and males with reproductive systems capable of
co-producing offspring.
IVF over age 40
All
pregnancies can be risky, but there are greater risk for people who are
older and are over the age of 40. The older the people the riskier the
pregnancy. As people get older, they are more likely to suffer from
conditions such as gestational diabetes and pre-eclampsia. If older
people do conceive over the age of 40, their offspring may be of lower
birth weight, and more likely to requires intensive care. Because of
this, the increased risk is a sufficient cause for concern. The high
incidence of caesarean in older mothers is commonly regarded as a risk.
Though there are some risk with olderpeaople pregnancies, there
are some benefits associated with caesareans. A study has shown that
births over 40 have a lower rate of birth trauma due to increased
delivery by caesarean. Though caesarean is seen to benefit mothers over
40, there are still many risk factors to consider. Caesarean section may
be a risk in the same way that gestational diabetes is.
People conceiving at 40 have a greater risk of gestational
hypertension and premature birth. The offspring is at risk when being
born from older mothers, and the risks associated with being conceived
through IVF.
Normal Vaginal Canal Vs Menopause
Adriana Iliescu
held the record for a while as the oldest woman to give birth using IVF
and a donor egg, when she gave birth in 2004 at the age of 66. In
September 2019, a 74-year-old woman became the oldest-ever to give
birth after she delivered twins at a hospital in Guntur, Andhra Pradesh.
Pregnancy after menopause
Although
menopause is a natural barrier to further conception, IVF has allowed
people to be pregnant in their fifties and sixties. People whose
uteruses have been appropriately prepared receive embryos that
originated from an egg of an egg donor. Therefore, although these people
do not have a genetic link with the child, they have a physical link
through pregnancy and childbirth. In many cases the genetic father of
the child is the woman's partner. Even after menopause the uterus is
fully capable of carrying out a pregnancy.
Same-sex couples, single and unmarried parents
A 2009 statement from the ASRM
found no persuasive evidence that children are harmed or disadvantaged
solely by being raised by single parents, unmarried parents, or
homosexual parents. It did not support restricting access to assisted
reproductive technologies on the basis of a prospective parent's marital
status or sexual orientation.
Ethical concerns include reproductive rights, the welfare of
offspring, nondiscrimination against unmarried individuals, homosexual,
and professional autonomy.
A recent controversy in California focused on the question of
whether physicians opposed to same-sex relationships should be required
to perform IVF for a lesbian couple. Guadalupe T. Benitez, a lesbian
medical assistant from San Diego, sued doctors Christine Brody and
Douglas Fenton of the North Coast Woman's Care Medical Group after Brody
told her that she had "religious-based objections to treating her and
homosexuals in general to help them conceive children by artificial
insemination," and Fenton refused to authorise a refill of her
prescription for the fertility drug Clomid on the same grounds. The California Medical Association had initially sided with Brody and Fenton, but the case, North Coast Women's Care Medical Group v. Superior Court, was decided unanimously by the California State Supreme Court in favour of Benitez on 19 August 2008.
IVF is increasingly being used to allow lesbian and other LGBT
couples to share in the reproductive process through a technique called reciprocal IVF. The eggs of one partner are used to create embryos which the other partner carries through pregnancy.
Nadya Suleman
came to international attention after having twelve embryos implanted,
eight of which survived, resulting in eight newborns being added to her
existing six-child family. The Medical Board of California sought to
have fertility doctor Michael Kamrava, who treated Suleman, stripped of
his licence. State officials allege that performing Suleman's procedure
is evidence of unreasonable judgment, substandard care, and a lack of
concern for the eight children she would conceive and the six she was
already struggling to raise. On 1 June 2011 the Medical Board issued a
ruling that Kamrava's medical licence be revoked effective 1 July 2011.
Anonymous donors
Some children conceived by IVF using anonymous donors
report being troubled over not knowing about their donor parent as well
any genetic relatives they may have and their family history.
Alana Stewart, who was conceived using donor sperm, began an
online forum for donor children called AnonymousUS in 2010. The forum
welcomes the viewpoints of anyone involved in the IVF process.
Olivia Pratten, a donor-conceived Canadian, sued the province of
British Columbia for access to records on her donor father's identity in
2008. "I'm not a treatment, I'm a person, and those records belong to me," Pratten said.
In May 2012, a court ruled in Pratten's favour, agreeing that the laws
at the time discriminated against donor children and making anonymous
sperm and egg donation in British Columbia illegal.
In the U.K., Sweden, Norway, Germany, Italy, New Zealand, and
some Australian states, donors are not paid and cannot be anonymous.
In 2000, a website called Donor Sibling Registry was created to help biological children with a common donor connect with each other.
In 2012, a documentary called Anonymous Father's Day was released that focuses on donor-conceived children.
Unwanted embryos
During the selection
and transfer phases, many embryos may be discarded in favour of others.
This selection may be based on criteria such as genetic disorders or
the sex.
One of the earliest cases of special gene selection through IVF was the
case of the Collins family in the 1990s, who selected the sex of their
child.
The ethic issues remain unresolved as no consensus exists in science,
religion, and philosophy on when a human embryo should be recognised as a
person. For those who believe that this is at the moment of conception,
IVF becomes a moral question when multiple eggs are fertilised, begin
development, and only a few are chosen for implantation.
If IVF were to involve the fertilisation of only a single egg, or
at least only the number that will be implanted, then this would not be
an issue. However, this has the chance of increasing costs dramatically
as only a few eggs can be attempted at a time. As a result, the couple
must decide what to do with these extra embryos. Depending on their
view of the embryo's humanity or the chance the couple will want to try
to have another child, the couple has multiple options for dealing with
these extra embryos. Couples can choose to keep them frozen, donate them
to other infertile couples, thaw them, or donate them to medical
research.
Keeping them frozen costs money, donating them does not ensure they
will survive, thawing them renders them immediately unviable, and
medical research results in their termination. In the realm of medical
research, the couple is not necessarily told what the embryos will be
used for, and as a result, some can be used in stem cell research, a field perceived to have ethical issues.
Religious response
The Catholic Church opposes all kinds of assisted reproductive technology and artificial contraception, on the grounds that they separate the procreative goal of marital sex from the goal of uniting married couples.
The Catholic Church permits the use of a small number of reproductive technologies and contraceptive methods such as natural family planning,
which involves charting ovulation times, and allows other forms of
reproductive technologies that allow conception to take place from
normative sexual intercourse, such as a fertility lubricant. Pope
Benedict XVI had publicly re-emphasised the Catholic Church's opposition
to in vitro fertilisation, saying that it replaces love between a
husband and wife.
The Catechism of the Catholic Church, in accordance with the Catholic understanding of natural law, teaches that reproduction has an "inseparable connection" to the sexual union of married couples.
In addition, the church opposes IVF because it might result in the
disposal of embryos; in Catholicism, an embryo is viewed as an
individual with a soul that must be treated as a person.
The Catholic Church maintains that it is not objectively evil to be
infertile, and advocates adoption as an option for such couples who
still wish to have children.
Hindus welcome IVF as a gift for those who are unable to bear children and have declared doctors related to IVF to be conducting punya as there are several characters who were claimed to be born without intercourse, mainly Kaurav and five Pandavas.
Regarding the response to IVF by Islam,
a general consensus from the contemporary Sunni scholars concludes that
IVF methods are immoral and prohibited. However, Gad El-Hak Ali Gad
El-Hak's ART fatwa includes that:
- IVF of an egg from the wife with the sperm of her husband and
the transfer of the fertilised egg back to the uterus of the wife is
allowed, provided that the procedure is indicated for a medical reason
and is carried out by an expert physician.
- Since marriage is a contract between the wife and husband during the
span of their marriage, no third party should intrude into the marital
functions of sex and procreation. This means that a third party donor is
not acceptable, whether he or she is providing sperm, eggs, embryos, or
a uterus. The use of a third party is tantamount to zina, or adultery.
Within the Orthodox Jewish community the concept is debated as there is little precedent in traditional Jewish legal textual sources. Regarding laws of sexuality, religious challenges include masturbation (which may be regarded as "seed wasting"), laws related to sexual activity and menstruation (niddah)
and the specific laws regarding intercourse. An additional major issue
is that of establishing paternity and lineage. For a baby conceived
naturally, the father's identity is determined by a legal presumption (chazakah) of legitimacy: rov bi'ot achar ha'baal – a woman's sexual relations are assumed to be with her husband. Regarding an IVF child, this assumption does not exist and as such Rabbi Eliezer Waldenberg (among others) requires an outside supervisor to positively identify the father. Reform Judaism has generally approved IVF.
Society and culture
Many
people of sub-Saharan Africa choose to foster their children to
infertile people. IVF enables these infertile women to have their own
children, which imposes new ideals to a culture in which fostering
children is seen as both natural and culturally important. Many
infertile women are able to earn more respect in their society by taking
care of the children of other mothers, and this may be lost if they
choose to use IVF instead. As IVF is seen as unnatural, it may even
hinder their societal position as opposed to making them equal with
fertile women. It is also economically advantageous for infertile people
to raise foster children as it gives these children greater ability to
access resources that are important for their development and also aids
the development of their society at large. If IVF becomes more popular
without the birth rate decreasing, there could be more large family
homes with fewer options to send their newborn children. This could
result in an increase of orphaned children and/or a decrease in
resources for the children of large families. This would ultimately
stifle the children's and the community's growth.
In the US, the pineapple
has emerged as a symbol of IVF users, possibly because some people
thought, without scientific evidence, that eating pineapple might
slightly increase the success rate for the procedure.
Emotional involvement with children
Studies
have indicated that IVF mothers show greater emotional involvement with
their child, and they enjoy motherhood more than mothers by natural
conception. Similarly, studies have indicated that IVF fathers express
more warmth and emotional involvement than fathers by adoption and
natural conception and enjoy fatherhood more. Some IVF parents become
overly involved with their children.
Men and IVF
Research has shown that men largely view themselves as "passive contributors" since they have "less physical involvement"
in IVF treatment. Despite this, many men feel distressed after seeing
the toll of hormonal injections and ongoing physical intervention on
their female partner.
Fertility was found to be a significant factor in a man's
perception of his masculinity, driving many to keep the treatment a
secret.
In cases where the men did share that he and his partner were
undergoing IVF, they reported to have been teased, mainly by other men,
although some viewed this as an affirmation of support and friendship.
For others, this led to feeling socially isolated. In comparison with women, men showed less deterioration in mental health in the years following a failed treatment.
However, many men did feel guilt, disappointment and inadequacy,
stating that they were simply trying to provide an "emotional rock" for
their partners.
Cost of IVF
Costs
of IVF can be broken down into direct and indirect costs. Direct costs
include the medical treatments themselves, including doctor
consultations, medications, ultrasound scanning, laboratory tests, the
actual IVF procedure, and any associated hospital charges and
administrative costs. Indirect costs includes the cost of addressing any
complications with treatments, patients' travel costs and lost hours of
productivity.
These costs can be exaggerated by the increasing age of the woman
undergoing IVF treatment (particularly those over the age of 40), and
the increase costs associated with multiple births. For instance, a
pregnancy with twins can cost up to three times that of a singleton
pregnancy.
Availability and utilisation
High
costs keep IVF out of reach for many developing countries, but research
by the Genk Institute for Fertility Technology, in Belgium, claim to
have found a much lower cost methodology (about 90% reduction) with
similar efficacy, which may be suitable for some fertility treatment.
Moreover, the laws of many countries permit IVF for only single women,
lesbian couples, and persons participating in surrogacy arrangements.
Using PGD gives members of these select demographic groups
disproportionate access to a means of creating a child possessing
characteristics that they consider "ideal," raising issues of equal
opportunity for both the parents'/parent's and the child's generation.
Many fertile couples
now demand equal access to embryonic screening so that their child can
be just as healthy as one created through IVF. Mass use of PGD,
especially as a means of population control or in the presence of legal measures related to population or demographic control, can lead to intentional or unintentional demographic effects such as the skewed live-birth sex ratios seen in communist China following implementation of its one-child policy.
Australia
In
Australia, the average age of people undergoing ART treatment is 35.5
years among those using their own eggs (one in four being 40 or older)
and 40.5 years among those using donated eggs. While IVF is available in Australia, Australians using IVF are unable to choose their baby's gender.
Cameroon
Ernestine Gwet Bell supervised the first Cameroonian child born by IVF in 1998.
Canada
In
Canada, one cycle of IVF treatment can cost between $7,750 to $12,250
CAD, and medications alone can cost between $2,500 to over $7,000 CAD.
The funding mechanisms that influence accessibility in Canada vary by
province and territory, with some provinces providing full, partial or
no coverage.
New Brunswick
provides partial funding through their Infertility Special Assistance
Fund – a one time grant of up to $5,000. Patients may only claim up to
50% of treatment costs or $5,000 (whichever is less) occurred after
April 2014. Eligible patients must be a full-time New Brunswick resident
with a valid Medicare card and have an official medical infertility diagnosis by a physician.
In December 2015, the Ontario
provincial government enacted the Ontario Fertility Program for
patients with medical and non-medical infertility, regardless of sexual
orientation, gender or family composition. Eligible patients for IVF
treatment must be Ontario residents under the age of 43 and have a valid
Ontario Health Insurance Plan
card and have not already undergone any IVF cycles. Coverage is
extensive, but not universal. Coverage extends to certain blood and
urine tests, physician/nurse counselling and consultations, certain
ultrasounds, up to two cycle monitorings, embryo thawing, freezing and
culture, fertilisation and embryology services, single transfers of all
embryos, and one surgical sperm retrieval using certain techniques only
if necessary. Drugs and medications are not covered under this Program,
along with psychologist or social worker counselling, storage and
shipping of eggs, sperm or embryos, and the purchase of donor sperm or
eggs.
India
The
penetration of the IVF market in India is quite low at present with only
2,800 cycles/million infertile people in the reproductive age group
(20–44 years) as compared to China which has 6,500 cycles. The key
challenges are lack of awareness, affordability and accessibility.
India in 2018 becomes the destination for Fertility Tourism because of
most affordable IVF treatment cost. IVF treatment cost in India varies
from $2000 to $4000 (roughly between 150000/- INR to 250000/- INR
including all aspects of IVF treatment with medicines which is almost 5
times lower than IVF Cost in Western part of the world.
Israel
Israel
has the highest rate of IVF in the world, with 1657 procedures performed
per million people per year. Couples without children can receive
funding for IVF for up to two children. The same funding is available
for people without children who will raise up to 2 children in a single parent home. IVF is available for people aged 18 to 45. The Israeli Health Ministry says it spends roughly $3450 per procedure.
Sweden
One, two
or three IVF treatments are government subsidised for people who are
younger than 40 and have no children. The rules for how many treatments
are subsidised, and the upper age limit for the people, vary between
different county councils. Single people are treated, and embryo adoption is allowed. There are also private clinics that offer the treatment for a fee.
United Kingdom
Availability of IVF in England is determined by Clinical commissioning groups. The National Institute for Health and Care Excellence
recommends up to 3 cycles of treatment for people under 40 years old
with minimal success conceiving after 2 years of unprotected sex.
Cycles will not be continued for people who are older than 40 years old. CCGs in Essex, Bedfordshire and Somerset
have reduced funding to one cycle, or none, and it is expected that
reductions will become more widespread. Funding may be available in
"exceptional circumstances" – for example if a male partner has a
transmittable infection or one partner is affected by cancer treatment.
According to the campaign group Fertility Fairness "at the end of 2014
every CCG in England was funding at least one cycle of IVF". Prices paid by the NHS in England varied between under £3,000 to more than £6,000 in 2014/5.
In February 2013, the cost of implementing the NICE guidelines for IVF
along with other treatments for infertility was projected to be £236,000
per year per 100,000 members of the population.
IVF increasingly appears on NHS treatments blacklists. In August 2017 five of the 208 CCGs had stopped funding IVF completely and others were considering doing so. By October 2017 only 25 CCGs were delivering the three recommended NHS IVF cycles to eligible people under 40. Policies could fall foul of discrimination laws if they treat same sex couples differently from heterosexual ones. In July 2019 Jackie Doyle-Price said that women were registering with surgeries further away from their own home in order to get around CCG rationing policies.
The Human Fertilisation and Embryology Authority
said in September 2018 that parents who are limited to one cycle of
IVF, or have to fund it themselves, are more likely choose to implant
multiple embryos in the hope it increases the chances of pregnancy.
This significantly increases the chance of multiple births and the
associated poor outcomes, which would increase NHS costs. The president
of the Royal College of Obstetricians and Gynaecologists
said that funding 3 cycles was "the most important factor in
maintaining low rates of multiple pregnancies and reduce(s) associated
complications".
United States
In
the United States, overall availability of IVF in 2005 was 2.5 IVF
physicians per 100,000 population, and utilisation was 236 IVF cycles
per 100,000.
126 procedures are performed per million people per year. Utilisation
highly increases with availability and IVF insurance coverage, and to a
significant extent also with percentage of single persons and median
income.
In the US, an average cycle, from egg retrieval to embryo
implantation, costs $12,400, and insurance companies that do cover
treatment, even partially, usually cap the number of cycles they pay
for. As of 2015, more than 1 million babies had been born utilising IVF technologies.
The cost of IVF rather reflects the costliness of the underlying healthcare system than the regulatory or funding environment,
and ranges, on average for a standard IVF cycle and in 2006 United
States dollars, between $12,500 in the United States to $4,000 in Japan. In Ireland, IVF costs around €4,000, with fertility drugs, if required, costing up to €3,000. The cost per live birth is highest in the United States ($41,000) and United Kingdom ($40,000) and lowest in Scandinavia and Japan (both around $24,500).
Many fertility clinics in the United States limit the upper age at which people are eligible for IVF to 50 or 55 years. These cut-offs make it difficult for people older than fifty-five to utilise the procedure.
Alternatives
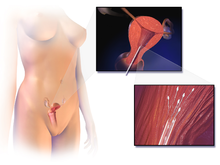
Schematic illustration of artificial insemination.
Alternatives to IVF are mainly:
- Artificial insemination, including intracervical insemination and intrauterine insemination of semen. It requires that a woman ovulates,
but is a relatively simple procedure, and can be used in the home for
self-insemination without medical practitioner assistance.
The beneficiaries of artificial insemination are people who desire to
give birth to their own child who may be single, women who are in a lesbian relationship or females who are in a heterosexual relationship but with a male partner who is infertile or who has a physical impairment which prevents full intercourse from taking place.
- Ovulation induction
(in the sense of medical treatment aiming for the development of one or
two ovulatory follicles) is an alternative for people with anovulation or oligoovulation, since it is less expensive and more easy to control. It generally involves antiestrogens such as clomifene citrate or letrozole, and is followed by natural or artificial insemination.
- Surrogacy,
where the surrogate mother agrees to bear a child for another person or
persons, who will become the child's parent(s) after birth. People may
seek a surrogacy arrangement when pregnancy is medically impossible,
when pregnancy risks are too dangerous for the intended mother, or when a single man or a male couple wish to have a child.
- Adoption whereby a person assumes the parenting of another, usually a child, from that person's biological or legal parent or parents.
Legal status
Government
agencies in China passed bans on the use of IVF in 2003 by unmarried
people or by couples with certain infectious diseases.
In India, the use of IVF as a means of sex selection (preimplantation genetic diagnosis) is banned under the Pre-Conception and Pre-Natal Diagnostic Techniques Act, 1994
Sunni Muslim nations generally allow IVF between married couples
when conducted with their own respective sperm and eggs, but not with
donor eggs from other couples. But Iran, which is Shi'a Muslim, has a
more complex scheme. Iran bans sperm donation but allows donation of
both fertilised and unfertilised eggs. Fertilised eggs are donated from
married couples to other married couples, while unfertilised eggs are
donated in the context of mut'ah or temporary marriage to the father.
By 2012 Costa Rica
was the only country in the world with a complete ban on IVF
technology, it having been ruled unconstitutional by the nation's
Supreme Court because it "violated life."
Costa Rica had been the only country in the western hemisphere that
forbade IVF. A law project sent reluctantly by the government of
President Laura Chinchilla
was rejected by parliament. President Chinchilla has not publicly
stated her position on the question of IVF. However, given the massive
influence of the Catholic Church in her government any change in the
status quo seems very unlikely.
In spite of Costa Rican government and strong religious opposition, the
IVF ban has been struck down by the Inter-American Court of Human
Rights in a decision of 20 December 2012.
The court said that a long-standing Costa Rican guarantee of protection
for every human embryo violated the reproductive freedom of infertile
couples because it prohibited them from using IVF, which often involves
the disposal of embryos not implanted in a patient's uterus.
On 10 September 2015, President Luis Guillermo Solís signed a decree
legalising in-vitro fertilization. The decree was added to the country's
official gazette on 11 September. Opponents of the practice have since
filed a lawsuit before the country's Constitutional Court.
All major restrictions on single but infertile people using IVF
were lifted in Australia in 2002 after a final appeal to the Australian
High Court was rejected on procedural grounds in the Leesa Meldrum case.
A Victorian
federal court had ruled in 2000 that the existing ban on all single
people and lesbians using IVF constituted sex discrimination.
Victoria's government announced changes to its IVF law in 2007
eliminating remaining restrictions on fertile single people and
lesbians, leaving South Australia as the only state maintaining them.
Federal regulations in the United States include screening requirements and restrictions on donations, but generally do not affect sexually intimate partners. However, doctors may be required to provide treatments due to nondiscrimination laws, as for example in California. The US state of Tennessee proposed a bill in 2009 that would have defined donor IVF as adoption.
During the same session another bill proposed barring adoption from any
unmarried and cohabitating couple, and activist groups stated that
passing the first bill would effectively stop unmarried people from
using IVF. Neither of these bills passed.
Few American courts have addressed the issue of the "property"
status of a frozen embryo. This issue might arise in the context of a
divorce case, in which a court would need to determine which spouse
would be able to decide the disposition of the embryos. It could also
arise in the context of a dispute between a sperm donor and egg donor,
even if they were unmarried. In 2015, an Illinois court held that such
disputes could be decided by reference to any contract between the
parents-to-be. In the absence of a contract, the court would weigh the
relative interests of the parties.