| Addison's disease | |
|---|---|
| Other names | Addison disease, chronic adrenal insufficiency, hypocortisolism, hypoadrenalism, primary adrenal insufficiency |
 | |
| Classic darkening of the skin due to increased pigment as seen in Addison's disease | |
| Specialty | Endocrinology |
| Symptoms | Abdominal pain, weakness, weight loss, darkening of the skin |
| Complications | Adrenal crisis |
| Usual onset | Middle-aged females |
| Causes | Problems with the adrenal gland |
| Diagnostic method | Blood tests, urine tests, medical imaging |
| Treatment | Corticosteroid such as hydrocortisone and fludrocortisone |
| Frequency | 0.9–1.4 per 10,000 people (developed world) |
Addison's disease, also known as primary adrenal insufficiency and hypocortisolism, is a long-term endocrine disorder in which the adrenal glands do not produce enough steroid hormones. Symptoms generally come on slowly and may include abdominal pain, weakness, and weight loss. Darkening of the skin in certain areas may also occur. Under certain circumstances, an adrenal crisis may occur with low blood pressure, vomiting, lower back pain, and loss of consciousness. An adrenal crisis can be triggered by stress, such as from an injury, surgery, or infection.
Addison's disease arises from problems with the adrenal gland such that not enough of the steroid hormone cortisol and possibly aldosterone are produced, most often due to damage by the body's own immune system in the developed world and tuberculosis in the developing world. Other causes include certain medications, sepsis, and bleeding into both adrenal glands. Secondary adrenal insufficiency is caused by not enough adrenocorticotropic hormone (ACTH) (produced by the pituitary gland) or CRH (produced by the hypothalamus). Despite this distinction, adrenal crises can happen in all forms of adrenal insufficiency. Addison's disease is generally diagnosed by blood tests, urine tests, and medical imaging.
Treatment involves replacing the absent hormones. This involves taking a corticosteroid such as hydrocortisone and fludrocortisone. These medications are usually taken by mouth. Lifelong, continuous steroid replacement therapy is required, with regular follow-up treatment and monitoring for other health problems. A high-salt diet may also be useful in some people. If symptoms worsen, an injection of corticosteroid is recommended and people should carry a dose with them. Often, large amounts of intravenous fluids with the sugar dextrose are also required. Without treatment, an adrenal crisis can result in death.
Addison's disease affects about 0.9 to 1.4 per 10,000 people in the developed world. It occurs most frequently in middle-aged females. Secondary adrenal insufficiency is more common. Long-term outcomes with treatment are typically good. It is named after Thomas Addison, a graduate of the University of Edinburgh Medical School, who first described the condition in 1855. The adjective "addisonian" is used to describe features of the condition, as well as people with Addison's disease.
Signs and symptoms
A Caucasian woman with Addison's disease
Legs of a Caucasian woman with Addison's disease
The symptoms of Addison's disease develop gradually and may become
established before they are recognized. They can be nonspecific and are
potentially attributable to other medical conditions.
The signs and symptoms include fatigue; lightheadedness upon standing or difficulty standing, muscle weakness, fever, weight loss, anxiety, nausea, vomiting, diarrhea, headache, sweating, changes in mood or personality, and joint and muscle pains. Some people have cravings for salt or salty foods due to the loss of sodium through their urine. Hyperpigmentation of the skin may be seen, particularly when the person lives in a sunny area, as well as darkening of the palmar crease, sites of friction, recent scars, the vermilion border of the lips, and genital skin. These skin changes are not encountered in secondary and tertiary hypoadrenalism.
On physical examination, these clinical signs may be noticed:
- Low blood pressure with or without orthostatic hypotension (blood pressure that decreases with standing)
- Darkening (hyperpigmentation) of the skin, including areas not exposed to the sun. Characteristic sites of darkening are skin creases (e.g., of the hands), nipple, and the inside of the cheek (buccal mucosa); also, old scars may darken. This occurs because melanocyte-stimulating hormone (MSH) and ACTH share the same precursor molecule, pro-opiomelanocortin (POMC). After production in the anterior pituitary gland, POMC gets cleaved into gamma-MSH, ACTH, and beta-lipotropin. The subunit ACTH undergoes further cleavage to produce alpha-MSH, the most important MSH for skin pigmentation. In secondary and tertiary forms of adrenal insufficiency, skin darkening does not occur, as ACTH is not overproduced.
Addison's disease is associated with the development of other autoimmune diseases, such as type I diabetes, thyroid disease (Hashimoto's thyroiditis), celiac disease, or vitiligo. Addison's disease may be the only manifestation of undiagnosed celiac disease. Both diseases share the same genetic risk factors (HLA-DQ2 and HLA-DQ8 haplotypes).
The presence of Addison's in addition to mucocutaneous candidiasis, hypoparathyroidism, or both, is called autoimmune polyendocrine syndrome type 1. The presence of Addison's in addition to autoimmune thyroid disease, type 1 diabetes, or both, is called autoimmune polyendocrine syndrome type 2.
Addisonian crisis
An "Addisonian crisis" or "adrenal crisis" is a constellation of
symptoms that indicates severe adrenal insufficiency. This may be the
result of either previously undiagnosed Addison's disease, a disease
process suddenly affecting adrenal function (such as adrenal
hemorrhage), or an intercurrent problem (e.g., infection, trauma) in
someone known to have Addison's disease. It is a medical emergency and
potentially life-threatening situation requiring immediate emergency
treatment.
Characteristic symptoms are:
- Sudden penetrating pain in the legs, lower back, or abdomen
- Severe vomiting and diarrhea, resulting in dehydration
- Low blood pressure
- Syncope (loss of consciousness and ability to stand)
- Hypoglycemia (reduced level of blood glucose)
- Confusion, psychosis, slurred speech
- Severe lethargy
- Hyponatremia (low sodium level in the blood)
- Hyperkalemia (elevated potassium level in the blood)
- Hypercalcemia (elevated calcium level in the blood)
- Convulsions
- Fever
Causes
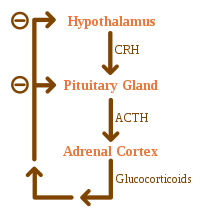
The negative feedback loop for glucocorticoids
Causes of adrenal insufficiency can be categorized by the mechanism
through which they cause the adrenal glands to produce insufficient
cortisol. These are adrenal dysgenesis (the gland has not formed
adequately during development), impaired steroidogenesis (the gland is
present but is biochemically unable to produce cortisol) or adrenal
destruction (disease processes leading to glandular damage).
Adrenal destruction
Autoimmune adrenalitis is the most common cause of Addison's disease in the industrialized world. Autoimmune destruction of the adrenal cortex is caused by an immune reaction against the enzyme 21-hydroxylase (a phenomenon first described in 1992). This may be isolated or in the context of autoimmune polyendocrine syndrome (APS type 1 or 2), in which other hormone-producing organs, such as the thyroid and pancreas, may also be affected.
Adrenal destruction is also a feature of adrenoleukodystrophy, and when the adrenal glands are involved in metastasis (seeding of cancer cells from elsewhere in the body, especially lung), hemorrhage (e.g., in Waterhouse–Friderichsen syndrome or antiphospholipid syndrome), particular infections (tuberculosis, histoplasmosis, coccidioidomycosis), or the deposition of abnormal protein in amyloidosis.
Adrenal dysgenesis
All causes in this category are genetic, and generally very rare. These include mutations to the SF1 transcription factor, congenital adrenal hypoplasia due to DAX-1 gene mutations and mutations to the ACTH receptor gene (or related genes, such as in the Triple-A or Allgrove syndrome). DAX-1 mutations may cluster in a syndrome with glycerol kinase deficiency with a number of other symptoms when DAX-1 is deleted together with a number of other genes.
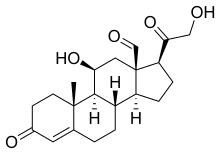
Impaired steroidogenesis
To form cortisol, the adrenal gland requires cholesterol, which is then converted biochemically into steroid hormones. Interruptions in the delivery of cholesterol include Smith–Lemli–Opitz syndrome and abetalipoproteinemia.
Of the synthesis problems, congenital adrenal hyperplasia is the most common (in various forms: 21-hydroxylase, 17α-hydroxylase, 11β-hydroxylase and 3β-hydroxysteroid dehydrogenase), lipoid CAH due to deficiency of StAR and mitochondrial DNA mutations. Some medications interfere with steroid synthesis enzymes (e.g., ketoconazole), while others accelerate the normal breakdown of hormones by the liver (e.g., rifampicin, phenytoin).
Diagnosis
Suggestive features
Routine laboratory investigations may show:
- Hypoglycemia, low blood sugar (worse in children due to loss of glucocorticoid's glucogenic effects)
- Hyponatremia (low blood sodium levels), due to loss of production of the hormone aldosterone, to the kidney's inability to excrete free water in the absence of sufficient cortisol, and also the effect of corticotropin-releasing hormone to stimulate secretion of ADH.
- Hyperkalemia (raised blood potassium levels), due to loss of production of the hormone aldosterone.
- Eosinophilia and lymphocytosis (increased number of eosinophils or lymphocytes, two types of white blood cells)
- Metabolic acidosis (increased blood acidity), also is due to loss of the hormone aldosterone because sodium reabsorption in the distal tubule is linked with acid/hydrogen ion (H+) secretion. Absent or insufficient levels of aldosterone stimulation of the renal distal tubule leads to sodium wasting in the urine and H+ retention in the serum.
Testing
In suspected cases of Addison's disease, demonstration of low adrenal
hormone levels even after appropriate stimulation (called the ACTH stimulation test or synacthen test) with synthetic pituitary ACTH hormone tetracosactide
is needed for the diagnosis. Two tests are performed, the short and the
long test. Dexamethasone does not cross-react with the assay and can be
administered concomitantly during testing.
The short test compares blood cortisol levels before and after
250 micrograms of tetracosactide (intramuscular or intravenous) is
given. If, one hour later, plasma
cortisol exceeds 170 nmol/l and has risen by at least 330 nmol/l to at
least 690 nmol/l, adrenal failure is excluded. If the short test is
abnormal, the long test is used to differentiate between primary adrenal
insufficiency and secondary adrenocortical insufficiency.
The long test uses 1 mg tetracosactide (intramuscular). Blood is
taken 1, 4, 8, and 24 hr later. Normal plasma cortisol level should
reach 1000 nmol/l by 4 hr. In primary Addison's disease, the cortisol
level is reduced at all stages, whereas in secondary corticoadrenal
insufficiency, a delayed but normal response is seen.
Other tests may be performed to distinguish between various causes of hypoadrenalism, including renin and adrenocorticotropic hormone levels, as well as medical imaging - usually in the form of ultrasound, computed tomography or magnetic resonance imaging.
Adrenoleukodystrophy, and the milder form, adrenomyeloneuropathy,
cause adrenal insufficiency combined with neurological symptoms. These
diseases are estimated to be the cause of adrenal insufficiency in about
35% of diagnosed male with idiopathic Addison’s disease, and should be
considered in the differential diagnosis of any male with adrenal
insufficiency. Diagnosis is made by a blood test to detect very long chain fatty acids.
Treatment
Maintenance
Treatment for Addison's disease involves replacing the missing cortisol, sometimes in the form of hydrocortisone tablets, or prednisone tablets in a dosing regimen that mimics the physiological concentrations of cortisol. Alternatively, one-quarter as much prednisolone may be used for equal glucocorticoid effect as hydrocortisone. Treatment is usually lifelong. In addition, many people require fludrocortisone as replacement for the missing aldosterone.
People with Addison's are often advised to carry information on them (e.g., in the form of a MedicAlert bracelet or information card) for the attention of emergency medical services personnel who might need to attend to their needs. It is also recommended that a needle, syringe, and injectable form of cortisol be carried for emergencies.
People with Addison's disease are advised to increase their medication
during periods of illness or when undergoing surgery or dental
treatment.
Immediate medical attention is needed when severe infections, vomiting,
or diarrhea occur, as these conditions can precipitate an Addisonian
crisis. A person who is vomiting may require injections of
hydrocortisone instead.
Crisis
Standard
therapy involves intravenous injections of glucocorticoids and large
volumes of intravenous saline solution with dextrose (glucose).
This treatment usually brings rapid improvement. If intravenous access
is not immediately available, intramuscular injection of glucocorticoids
can be used. When the person can take fluids and medications by mouth,
the amount of glucocorticoids is decreased until a maintenance dose is
reached. If aldosterone is deficient, maintenance therapy also includes
oral doses of fludrocortisone acetate.
Prognosis
Outcomes
are typically good when treated. Most can expect to live relatively
normal lives. Someone with the disease should be observant of symptoms
of an "Addison's crisis" while the body is strained, as in rigorous
exercise or being sick, the latter often needing emergency treatment
with intravenous injections to treat the crisis.
Individuals with Addison's disease have more than a doubled mortality rate. Furthermore, individuals with Addison's disease and diabetes mellitus have an almost 4 time increase in mortality compared to individuals with only diabetes.
Epidemiology
The frequency rate of Addison's disease in the human population is sometimes estimated at roughly one in 100,000. Some put the number closer to 40–144 cases per million population (1/25,000–1/7,000). Addison's can affect persons of any age, sex, or ethnicity, but it typically presents in adults between 30 and 50 years of age. Research has shown no significant predispositions based on ethnicity.
History
Discovery
Addison’s disease is named after Thomas Addison, the British physician who first described the condition in On the Constitutional and Local Effects of Disease of the Suprarenal Capsules (1855). He originally described it as "melasma suprarenale," but later physicians gave it the medical eponym "Addison's disease" in recognition of Addison's discovery.
All six of the original people under Addison's care had tuberculosis of the adrenal glands.
While the six under Addison in 1855 all had adrenal tuberculosis, the
term "Addison's disease" does not imply an underlying disease process.
The condition was initially considered a form of anemia
associated with the adrenal glands. Because little was known at the time
about the adrenal glands (then called "Supra-Renal Capsules"),
Addison’s monograph describing the condition was an isolated insight.
As the adrenal function became better known, Addison’s monograph became
known as an important medical contribution and a classic example of
careful medical observation.
Other animals
Hypoadrenocorticism is uncommon in dogs, and rare in cats. Individual cases have been reported in a grey seal, a red panda, a flying fox, and a sloth.
In dogs, hypoadrenocorticism has been diagnosed in many breeds. Vague symptoms which wax and wane can cause delay in recognition of the presence of the disease. Female dogs appear more affected than male dogs, though this may not be the case in all breeds.
The disease is most often diagnosed in dogs which are young to middle
aged, but it can occur at any age from 4 months to 14 years. Treatment of hypoadrenocorticism must replace the hormones (cortisol and aldosterone) which the dog cannot produce itself. This is achieved either by daily treatment with fludrocortisone, or monthly injections with desoxycorticosterone pivalate (DOCP) and daily treatment with a glucocorticoid, such as prednisone.
Several follow-up blood tests are required so that the dose can be
adjusted until the dog is receiving the correct amount of treatment,
because the medications used in the therapy of hypoadrenocorticism can
cause excessive thirst and urination if not prescribed at the lowest
effective dose. In anticipation of stressful situations, such as staying in a boarding kennel, dogs require an increased dose of prednisone. Lifelong treatment is required, but the prognosis for dogs with hypoadrenocorticism is very good.