| Date | October 2010 – present |
|---|---|
| Location | Haiti |
| Cause | Suspected contamination by United Nations peacekeepers. |
| Casualties | |
| 10,075 dead (all countries) | |
Cases: 809,262 (Haiti), 33,342 (DR), 678 (Cuba), 190 (Mexico) Cases recorded in: | |
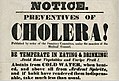
The 2010 Haitian cholera outbreak was the first modern large-scale outbreak of cholera – a disease once considered beaten back largely due to the invention of modern sanitation. Since its reintroduction to Haiti in October 2010, cholera has spread across the country and has become endemic, causing high levels of both morbidity and mortality. Since its reintroduction to Haiti following the 2010 Haitian earthquake, nearly 800,000 Haitians have been infected by cholera, and more than 9,000 have died, according to the United Nations (UN). Cholera transmission in Haiti today is largely a function of eradication efforts including WASH (water, sanitation, and hygiene), education, and oral vaccination, and climate variability. Early efforts were made to cover up the source of the epidemic, but thanks largely to the investigations of journalist Jonathan M. Katz and epidemiologist Renaud Piarroux, today it is widely believed to be the result of contamination by infected United Nations peacekeepers deployed from Nepal. In terms of total infections, the outbreak has since been surpassed by the war-fueled 2016–17 Yemen cholera outbreak, although the Haiti outbreak is still the most deadly modern outbreak.
Background
In January 2010, a 7.0 magnitude earthquake hit Haiti, killing over 100,000 people and further disrupting healthcare and sanitation infrastructure in the country.
In the aftermath of the earthquake, international workers from many
countries arrived in Haiti to assist in the response and recovery
efforts, including a number of workers from countries where cholera is endemic.
Before the outbreak, no cases of cholera had been identified in Haiti
for more than a century, and the Caribbean region as a whole had not
been affected by the cholera outbreak originating in Peru in 1991. The population's lack of prior exposure and acquired immunity contributed to the severity of the outbreak.
Outbreak
Cholera is caused by the bacterium Vibrio cholerae
that when ingested can cause diarrhea and vomiting within several hours
to 2–3 days. Without proper treatment including oral rehydration,
cholera can be fatal. The suspected source of Vibrio cholerae in Haiti was the Artibonite River, from which most of the affected people had consumed the water.
Each year, tens of thousands of Haitians bathe, wash their clothes and
dishes, obtain drinking water, and recreate in this river, therefore
resulting in high rates of exposure to Vibrio cholerae.
The cholera outbreak began ten months after the January 2010
earthquake, leading some observers to wrongly suspect it was a result of
the natural disaster. However, Haitians grew immediately suspicious of a UN peacekeeper base, home to Nepalese peacekeepers, positioned on a tributary of the Artibonite River.
Neighboring farmers reported an undeniable stench of human feces coming
from the base, to the extent that local Haitians began getting their
drinking water upstream from the base. In response, United Nations Stabilization Mission in Haiti (MINUSTAH)
officials issued a press statement denying the possibility that the
base could have caused the epidemic, citing stringent sanitation
standards. The next day, 27 October 2010, Jonathan M. Katz, an Associated Press
correspondent, visited the base and found gross inconsistencies between
the statement and the base's actual conditions. Katz also happened upon
UN military police
taking samples of ground water to test for cholera, despite UN
assertions that it was not concerned about a possible link between its
peacekeepers and the disease. Neighbors told the reporter that waste
from the base often spilled into the river. Later that day, a crew from Al Jazeera English, including reporter Sebastian Walker,
filmed the soldiers trying to excavate a leaking pipe; the video was
posted online the following day and, citing the AP report, drew
increased awareness to the base.
MINUSTAH spokesmen later contended that the samples taken from the base
proved negative for cholera. However, an AP investigation showed that
the tests were improperly done at a laboratory in the Dominican Republic, which had no prior experience of testing for cholera.
For three months, UN officials, the CDC, and others argued
against investigating the source of the outbreak. Gregory Hartl, a
spokesman for the World Health Organization
(WHO), said finding the cause of the outbreak was "not important".
Hartl said,"Right now, there is no active investigation. I cannot say
one way or another [if there will be]. It is not something we are
thinking about at the moment. What we are thinking about is the public
health response in Haiti." Jordan Tappero, the lead epidemiologist
at the CDC, said the main task was to control the outbreak, not to look
for the source of the bacteria and that "we may never know the actual
origin of this cholera strain."
A CDC spokesperson, Kathryn Harben, added that "at some point in the
future, when many different analyses of the strain are complete, it may
be possible to identify the origin of the strain causing the outbreak in
Haiti."
Paul Farmer, co-founder of the medical organization Partners In Health, and a UN official himself who served Bill Clinton's deputy at the Office of the Special Envoy for Haiti,
told the AP's Katz on 3 November 2010 that there was no reason to wait.
Farmer stated, "The idea that we'd never know is not very likely.
There's got to be a way to know the truth without pointing fingers."
A cholera expert, John Mekalanos, supported the assertion that it was
important to know where and how the disease emerged because the strain
is a "novel, virulent strain previously unknown in the Western
Hemisphere and health officials need to know how it spreads."
Some US professors have disagreed with the contention that Nepalese soldiers
caused the outbreak. Some said it was more likely dormant cholera
bacteria had been aroused by various environmental incidents in Haiti. Before studying the case, they said a sequence of events, including changes in climate triggered by the La Niña
climate pattern and unsanitary living conditions for those affected by
the earthquake, triggered bacteria already present in the water and soil
to multiply and infect humans.
However, a study unveiled in December and conducted by French epidemiologist Renaud Piarroux
contended that UN troops from Nepal, rather than environmental factors,
had started the epidemic as waste from outhouses at their base flowed
into and contaminated the Artibonite River. A separate study published in December in the New England Journal of Medicine
presented DNA sequence data for the Haitian cholera isolate, finding
that it was most closely related to a cholera strain found in Bangladesh
in 2002 and 2008. It was more distantly related to existing South
American strains of cholera, the authors reported, adding that "the
Haitian epidemic is probably the result of the introduction, through
human activity, of a V. cholerae strain from a distant geographic
source."
Under intense pressure, the UN relented, and said it would appoint a panel to investigate the source of the cholera strain.
That panel's report, issued in May 2011, confirmed substantial evidence
that the Nepalese troops had brought the disease to Haiti. The U.S. Centers for Disease Control and Prevention (CDC) utilized DNA fingerprinting
to tests various samples of cholera from Haitian patients to pinpoint
the specific strand of cholera found in Haiti. During an epidemiological
outbreak investigation, DNA fingerprinting of bacteria can be extremely
helpful in identifying the source of an outbreak. The results of the
CDC tests showed that the specific strain of cholera found in samples
taken from Haitian patients was Vibrio cholerae serogroup O1, serotype Ogawa, a strain found in South Asia.
This specific strain of cholera is endemic in Nepal, therefore
supporting the Haitian suspicion that Nepalese peacekeepers were the
source of the outbreak. However, in the report's concluding remarks, the
authors hedged to say that a "confluence of circumstances" was to
blame.
Rita Colwell, former director of the National Science Foundation
and climate change expert, still contends that climate changes were an
important factor in cholera's spread, stating in an interview with
UNEARTH News in August 2013 that the outbreak was "triggered by a
complicated set of factors. The precipitation and temperatures were
above average during 2010 and that, in conjunction with a destroyed
water and sanitation infrastructure, can be considered to have
contributed to this major disease outbreak."
In August 2016, after Katz obtained a leaked copy of a report by United Nations Special Rapporteur Philip Alston, Secretary General of the United Nations Ban Ki-moon
accepted responsibility for the UN's role in the initial outbreak and
stated that a "significant new set of U.N. actions" will be required to
help solve the problem.
In 2017, Katz also revealed the existence of emails that showed that
“officials at the highest levels of the U.S. government were aware
almost immediately that U.N. forces likely played a role in the
outbreak.” Katz reported that these emails showed “multiple federal
agencies, from national security officials to scientists on the front
lines, shielded the United Nations from accountability to protect the
organization and themselves.”
Reactions
At
the beginning of the outbreak, widespread panic regarding the virulence
of the disease and the UN's denial of the blame caused increased tension
between the UN and the Haitian community. On 15 November 2010, a riot
broke out in Cap-Haïtien
following the death of a young Haitian inside the Cap-Haïtien UN base
and rumours that the outbreak was caused by UN soldiers from Nepal. Protesters demanded that the Nepalese brigade of the UN leave the country. At least 5 people were killed in the riots, including 1 UN personnel. Riots then continued for a second day.
Following the riots, the UN continued their position that the Nepalese
soldiers were not to blame, and rather said that the riots was being
staged for "political reasons because of forthcoming elections", as the
Haitian government sent its own forces to "protest" the UN peacekeepers.
According to one author, rather than confront the inescapable
conclusion that the UN was indeed the cause, "the world’s preeminent
humanitarian organization continued to dissemble." During a third day of riots, UN personnel were blamed for shooting at least 5 protestors, but denied responsibility. On the fourth day of demonstrations against the UN presence, police fired tear gas into an IDP camp in the capital.
The outbreak of cholera became an issue for Haitian candidates to answer in the 2010 general election. There were fears that the election could be postponed. The head of MINUSTAH, Edmond Mulet said that it should not be delayed as that could lead to a political vacuum with untold potential problems.
In November 2011, the UN received a petition from 5,000 victims
for hundreds of millions of dollars in reparations over the outbreak
thought to have been caused by UN members of MINUSTAH. In February 2013, the United Nations responded by invoking its immunity from lawsuits under the Convention on the Privileges and Immunities of the United Nations. On 9 October 2013, Bureau des Avocats Internationaux (BAI), the Institute for Justice & Democracy in Haiti (IJDH), and civil rights lawyer Ira Kurzban's law firm Kurzban Kurzban Weinger Tetzeli & Pratt, P.A.(KKWT) filed a lawsuit against the UN in the Southern District of New York. The lawsuit was dismissed, but an appeal was filed in the Second Circuit. In October 2016, the Second Circuit Court of Appeals upheld the United Nations' immunity from claims. On March 11, 2014, a second lawsuit was filed, Laventure v. United Nations, in the Eastern District of New York, on behalf of more than 1,500 victims of the disaster. In an opinion piece in the Wall Street Journal, an attorney for the plaintiffs wrote:
"Imagine if the United Nations killed thousands on the streets of New York. Or London. Or Paris. And sickened nearly a million more. Would the U.N. claim it was not liable? Of course not. The international community wouldn't allow it."
A lead lawyer for the plaintiffs also noted that the lawsuit was
different from the one filed by the IDJH, in that it alleged that
liability had been accepted by the U.N. the 1990s. The lawyer stated
that immunity: “should not be a shield to hide behind because the United
Nations (or the U.S. government) doesn’t like the price tag that comes
with the U.N.’s indisputable gross negligence in this case."
This case, too, was dismissed by the U.S. District Court, and the Court of Appeals. The appeal is currently before the United States Supreme Court.
In December 2016, the then UN Secretary-General Ban Ki-moon finally apologized on behalf of UN, saying he was "profoundly sorry" for the outbreak.
The Secretary-General promised to spend $400 million to aid the
victims and to improve the nation's crumbling sanitation and water
systems. As of March 2017, the UN has come through with only 2 percent
of that amount.
Morbidity and mortality
Domestic
On
October 21, 2010, the Haitian Ministry of Public Health and Population
(MSPP) confirmed the first case of cholera in Haiti in over a century. The outbreak began in the rural Center department of Haiti, about 100 kilometres (62 mi) north of the capital, Port-au-Prince. By the first 10 weeks of the epidemic, cholera spread to all of Haiti's 10 departments or provinces. It had killed 4,672 people by March 2011 and hospitalized thousands more.
The outbreak in Haiti was the most severe in recent history prior to
2010; the World Health Organization reported that from 2010 to 2011, the
outbreak in Haiti accounted for 57% of all cases and 45% of all deaths
from cholera worldwide.
When the outbreak began in October 2010, more than 6% of Haitians resulted in acquiring the disease.
The highest incidence of cholera occurred in 2011 immediately following
the introduction of the primary exposure. The rate of incidence slowly
declined thereafter, with spikes resulting from rainy seasons and
hurricanes. As reported by the Haitian Health Ministry, as of August
2012, the outbreak had caused 586,625 cholera cases and 7,490 deaths. According to the Pan American Health Organization, as of 21 November 2013, there had been 689,448 cholera cases in Haiti, leading to 8,448 deaths.
While there had been an apparent lull in cases in 2014, by August 2015
the rainy season brought a spike in the number of cases. At that time
more than 700,000 Haitians had become ill with the disease and the death
toll had climbed to 9,000.
As of March 2017, around 7% of Haiti's population (around 800,665
people) have been affected with cholera, and 9,480 Haitians have died.
Latest epidemiological report by WHO in 2018 indicate a total of
812,586 cases of cholera in Haiti since October 2010, resulting in 9,606
deaths.
International
The first case of cholera was reported in the Dominican Republic in mid-November 2010, following the Pan-America Health Organization's prediction. By January 2011, the Dominican Republic had reported 244 cases of cholera. The first man to die of it there died in the province of Altagracia on 23 January 2011.
The Dominican Republic was particularly vulnerable to exposure of
cholera due to sharing a border with Haiti, and a large Haitian refugee
population displaced following the 2010 earthquake. As of the latest
epidemiological report by WHO in 2018, there has been a total of 33,188
cases of cholera in the Dominican Republic resulting in 504 deaths.
In late January 2011, more than 20 Venezuelans were reported to
have been taken to hospital after contracting cholera after visiting the
Dominican Republic. 37 cases were reported in total. Contaminated food was blamed for the spread of the disease. Venezuelan health minister Eugenia Sader gave a news conference which was broadcast on VTV during which she described all 37 people as "doing well".
The minister had previously observed that the last time cholera was
recorded in Venezuela was twenty years before this, in 1991.
In late June 2012, Cuba confirmed three deaths and 53 cases of cholera in Manzanillo; in 2013 there were 51 cases of cholera reported in Havana. Vaccination of half the population was urged by the University of Florida to stem the epidemic.
Vulnerabilities
Infrastructure
Before
the outbreak, Haiti suffered from relatively poor public health and
sanitation infrastructure. In 2002, Haiti was ranked 147th out of 147
countries for water security. As of 2008, 37% of Haiti's population lacked access to adequate drinking water, and 83% lacked improved sanitation facilities. As such, families often obtain their water from natural sources, such as rivers, that may be contaminated with V. cholerae.
Poor sanitation infrastructure allows cholera bacterium to enter these
waterways. Persons are subsequently infected via the fecal-oral route
when the water is used for drinking and cooking, and poor hygiene often
contributes to the spread of cholera through the household or community.
There is also a chronic shortage of health care personnel, and
hospitals lack adequate resources to treat those infected with cholera- a
situation that became readily apparent after the January 2010
earthquake.
Insufficient water and sanitation infrastructure, coupled with a
massive earthquake in 2010, made Haiti particularly vulnerable to an
outbreak of waterborne disease.
Physiological
Malnutrition
of the population, another pre-existing condition that was exacerbated
by the earthquake, may have also contributed to the severity of the
outbreak.
Research from previous outbreaks shows that duration of diarrhea can be
prolonged by up to 70% in individuals suffering from severe
malnutrition.
Furthermore, Haitians had no biological immunity to the strain of
cholera introduced since they had no previous exposure to it. Therefore,
physiological factors including malnutrition and lack of immunity may
have allowed cholera to spread rapidly throughout the country.
Information
Lack
of information and limited access to some rural areas can also be a
barrier to care. Some aid agencies have reported that mortality and
morbidity tolls may be higher than the official figures because the
government does not track deaths in rural areas where people never
reached a hospital or emergency treatment center.
Limitations in the data from Haiti stem from a lack of pre-outbreak
lack of surveillance infrastructure and laboratories to properly test
samples and diagnose cases.
Haiti was tasked with developing surveillance systems and laboratories
after the 2010 earthquake and cholera outbreak which caused difficulties
tracking the progression and scale of the outbreak. Because of the
lack of established surveillance, much of the case report data is
anecdotal and potentially underestimated. Also, because of lack of
laboratory confirmation for the vast majority of cases of cholera, it is
possible that other diarrheal diseases were being falsely classified as
cholera.
Environmental
Rainy
seasons and hurricanes continue to cause a temporary spike in incident
cases and deaths. Moreover, as a result of global warming and climate
change, Haiti is at an increased risk of cholera transmission. The
Intergovernmental Panel on Climate Change (IPCC) advances that global
warming between 1.5-2 degrees Celsius will very likely lead to an
increase in frequency and intensity of natural disasters and extreme
weather events. Resource-poor countries are poised to be affected more so than more developed and economically secure countries.
Environmental factors such as temperature increases, severe
weather events, and natural disasters have a two-fold impact on the
transmission potential of cholera in Haiti: 1) they present conditions
favorable to the persistence and growth of V. cholerae in the environment, and 2) they devastate a country's infrastructure and strain public health and health care resources.
An exhaustive study into environmental factors influencing the spread
of cholera in Haiti cites above average air temperatures following the
earthquake, “anomalously high rainfall” from September to October 2010,
and damage to the limited water and sanitation infrastructure as likely
converging to create conditions favorable to a cholera outbreak.
Challenges and solutions to eradication
Hundreds
of thousands of dollars have been dedicated towards eradicating cholera
in Haiti since its introduction in 2010, yet unsanitary conditions and
climate-driven forces allow cholera transmission to continue. While the
number of new cases of cholera has drastically decreased from 2010, and
is currently the lowest it has been since the outbreak began, the
incidence remains at 25.5 per 100,000 population as of October 2018.
Over time, there has been significant progress in the reduction of
caseloads and overall number of deaths. According to one PAHO/WHO
report, “the cumulative case-fatality rate (CFR) has remained around 1%
since 2011.”
These achievements can be contributed to intensified international and
local medical efforts and an increased emphasis on preventative
measures, including improved sanitation, such as latrines, and changes
in Haitian behaviors such as treating water, thoroughly cooking food,
and rigorous hand-washing. Despite these progresses, cholera remains
endemic in Haiti, and further resources are needed to fully eradicate
it.
After former UN Secretary General Ban Ki Moon accepted UN
responsibility for the introduction of cholera in Haiti in December
2016, Moon projected a necessary $400 million in funding over two years
in order to fully eradicate cholera in Haiti.
The Government of Haiti has dedicated itself to the complete
eradication of cholera from Haiti by 2022 as presented in the Cholera
Elimination Plan (PNEC) 2013 – 2022. UN Secretary-General Antonio
Guterres, successor to Ban Ki Moon, took up Moon's commitment to assist
Haiti in the eradication of cholera when he took office in 31 December
2016, as demonstrated by strategic objective 2 of the 2017- 2018 Haiti
Revised Humanitarian Plan. Strategic objective 2 reads, “Save lives from
epidemics – Reduce mortality and morbidity due to cholera outbreaks and
other waterborne diseases through the reduction of vulnerability,
strengthening of epidemiological surveillance and ensuring of rapid and
effective response.”
The 2017 – 2018 Haiti Revised Humanitarian Plan identifies 1.9 million
people in need of assistance for the protection from cholera, of which,
1.5 million people are targeted through programming totaling US$21.7
million.
Currently, the UN and Government of Haiti are on target to reach the
2016 – 2018 midterm goal to reduce the incidence of cholera to less than
0.1% by the end of 2018. However,
any disruption in funding of support services may result in a spike in
transmission and the interruption of the downward trend.
Challenges
Protracted crises: Hurricane Matthew 2016
The
first challenge to the eradication of cholera in Haiti is the country's
vulnerability to disasters, putting it in a state of protracted crises.
The climax of cholera incidence in Haiti was in 2011 with 352,000 new
cases following the introduction of cholera in Haiti in late 2010.
Incidence rates gradually declined until 2016 when there was another
spike in the transmission and incidence of cholera following Hurricane
Matthew's destruction in Haiti from October 2–5, 2016. There was a rise in cholera incidence from 32,000 new cases in 2015 to 42,000 new cases in 2016.
By re-damaging Haiti's fragile water and sanitation infrastructure,
Hurricane Matthew allowed cholera to rear its head. These figures
demonstrate that the fight against cholera in Haiti, while improving, is
on unstable ground. This indicates that while eradication efforts have
largely been focused on vaccination and community education to prevent
transmission, and oral rehydration to reduce mortality, the underlying
vulnerabilities that perpetuate the disaster remain, particularly
insufficient and unequal access to improved water and sanitation.
Funding
While
the Government of Haiti's Cholera Elimination Plan (PNEC) 2013 – 2022
and the New UN System Approach on Cholera in Haiti (see solutions below
for more information) lay out plans for the elimination of cholera in
Haiti by 2022, these are entirely dependent on funding. In former
Secretary General Moon's December 5, 2016 remarks he says, “Without
political will and financial support from the membership of the United
Nations, we have only good intentions and words. Words are powerful —
but they cannot replace action and material support.” Due to the infectious nature of cholera, any lapse in funding for programming will likely result in setbacks in elimination.
As of 2017, funding for cholera is at risk due to increasing food
insecurity and shelter needs for Haitian refugees returning from the
Dominican Republic. In the 2017 – 2018 Revised Haiti Humanitarian Plan,
funding requirements for cholera programming is the third largest at
$21.7 million, behind $76.6 million for food security and $103.8 million
for shelter/NFI needs.
Solutions
Vaccination campaigns
In
2013, the Government of Haiti launched an oral cholera vaccination
(OCV) campaign in two regions: Cerca Caravajal and Petite Anse. These
regions were chosen because of particularly high attack rates,
sanitation infrastructure, and access to healthcare. This vaccination
effort was slightly controversial because the WHO guidelines at the time
did not encourage mass vaccination campaigns in areas where outbreaks
had already occurred. Prior to the 2010 outbreak in Haiti, vaccination campaigns were thought
to detract from more important prevention measures like water treatment
and good hygiene. Relative success rates (up to 65% or higher protective effectiveness 5 years after vaccination)
in recent vaccination campaigns in Haiti and other countries affected
by cholera has led to more widespread use of oral cholera vaccine
programs and a change in the WHO guidelines to encourage use of vaccines
in addition to other prevention and treatment strategies.
UN approach
At the end of 2016, former UN Secretary General Ban Ki Moon presented the “New UN System Approach on Cholera in Haiti.”
This two-track approach marked the UN's acceptance of responsibility
for the introduction of cholera in Haiti and demonstrated its commitment
to the eradication of the disease in Haiti. Since the 2016 admission of
guilt, there has been increased coordination and goodwill between the
Government of Haiti and UN, resulting in great strides towards the
elimination of cholera. 2017 was a hallmark year in the elimination of
cholera from Haiti. The 2017 – 2018 Haiti Revised Humanitarian Plan
reports, “As of 31 December 2017, 13,682 suspected cholera cases and 150
deaths had been registered in the country in 2017 compared to 41,955
cases and 451 deaths for the same period in 2016, a decrease of 67% in
both cases.” Newly developed rapid response teams are largely to credit for the reduction in disease incidence.
The ability for the humanitarian sector to act quickly and bounce
back following Hurricane Matthew in 2016, as well as to maintain the
downward trend during the heavy rain season, demonstrates progress in
the eradication of cholera in Haiti.
Track 1
Track 1
of the New UN System Approach on Cholera in Haiti aims to “intensify
efforts to respond to and reduce the incidence of cholera in Haiti”
through three main projects.
The first is strengthening and supporting the rapid response framework
developed by the Haitian Government which deploys to communities where
cholera is suspected within 48-hours. There are currently 13 government
led rapid response teams, and 60 mobile teams of humanitarian actors
that support the rapid response teams. The goal of rapid response teams is to cut the transmission of cholera by first setting up a perimeter called a cordon sanitaire
and investigating the source of the outbreak at the household level.
This investigation is coupled with education and awareness raising on
cholera prevention, administering oral prophylaxis and distribution of
WASH kits.
If an outbreak is confirmed, temporary chlorination points are
installed on community water sources. People treated for cholera by the
rapid response teams are then recruited to Community Engagement &
Hygiene Awareness (CEHA) teams. The CEHA teams return to their
communities to conduct outreach and sensitization on how to cut
transmission and assist the government in monitoring water sources. This
rapid response design with the assistance of the CEHA teams is
responsible for a major decline in disease incidence in the Ouest
department in 2017. As long as funding continues to support rapid response, a continued decline in disease incidence can be suspected.
The second project of track 1 is the continued support of oral cholera vaccination campaigns as a preventative measure.
In 2018, the oral cholera vaccine campaign will focus on departments
with the highest incidence of disease, particularly Artibonite and
Centre departments.
The final aim of track 1 is to “more effectively address… the
medium/longer term issues of water, sanitation and health systems.”
The 2010 earthquake and subsequent cholera outbreak/epidemic exposed to
the international community how vulnerable the Haitian water,
sanitation, and health infrastructure was. Cholera and other water-borne
diseases will continue to circulate in Haiti as long as large sections
of their population do not have access to improved water and sanitation
facilities. As part of the UN's “New Way of Working” which aims to
bridge the development and humanitarian gap, the UN will be working with
major development actors including the World Bank and the International
Development Bank to address infrastructure vulnerabilities that put
Haiti at risk of protracted crisis.
The “New Way of Working” aims to draw from funding sources on both
sides of the spectrum, both development and humanitarian, to work
towards the Sustainable Development Goals. No joint funded projects
have been reported in Haiti yet.
Track 2
The second
track of the New UN System Approach on Cholera in Haiti proposes to
provide material assistance to individuals and families who were most
affected by cholera.
The material assistance package is the UN's attempt at reparations
after accepting responsibility for the introduction of cholera in Haiti.
The UN reports, “nearly 800,000 Haitians have been infected by cholera
since 2010 [as of 2016] and more than 9,000 have died.” First, consultations will be conducted with the community to identify what materials will be of greatest impact.