From Wikipedia, the free encyclopedia
The
Food and Drug Administration (
FDA or
USFDA) is a
federal agency of the
United States Department of Health and Human Services, one of the
United States federal executive departments. The FDA is responsible for protecting and promoting
public health through the control and supervision of
food safety,
tobacco products,
dietary supplements,
prescription and
over-the-counter pharmaceutical drugs (medications),
vaccines,
biopharmaceuticals,
blood transfusions,
medical devices,
electromagnetic radiation emitting devices (ERED), cosmetics,
animal foods & feed and
veterinary products. As of 2017, 3/4th of the FDA budget (approximately $700 million) is funded by the pharmaceutical companies due to the
Prescription Drug User Fee Act.
The FDA was empowered by the
United States Congress to enforce the
Federal Food, Drug, and Cosmetic Act, which serves as the primary focus for the Agency; the FDA also enforces other laws, notably Section 361 of the
Public Health Service Act
and associated regulations, many of which are not directly related to
food or drugs. These include regulating lasers, cellular phones, condoms
and control of disease on products ranging from certain household
pets to
sperm donation for
assisted reproduction.
The FDA is led by the
Commissioner of Food and Drugs, appointed by the
President with the
advice and consent of the
Senate. The Commissioner reports to the
Secretary of Health and Human Services. Scott Gottlieb, M.D. is the current commissioner, who took over in May 2017.
The FDA has its
headquarters in unincorporated
White Oak, Maryland. The agency also has 223 field offices and 13
laboratories located throughout the 50
states, the
United States Virgin Islands, and
Puerto Rico.
In 2008, the FDA began to post employees to foreign countries,
including China, India, Costa Rica, Chile, Belgium, and the United
Kingdom.
Organizational chart
Location
Building 66 at the site of the former Naval Ordnance Laboratory
In recent years, the agency began undertaking a large-scale effort to consolidate its 25 operations in the
Washington metropolitan area, moving from its main headquarters in Rockville and several fragmented office buildings to the former site of the
Naval Ordnance Laboratory in the White Oak area of
Silver Spring, Maryland.
The site was renamed from the White Oak Naval Surface Warfare Center to
the Federal Research Center at White Oak. The first building, the Life
Sciences Laboratory, was dedicated and opened with 104 employees on the
campus in December 2003. Only one original building from the naval
facility was kept. All other buildings are new construction. The project is slated to be completed by 2017, assuming future Congressional funding
Regional facilities
The Arkansas Laboratory in Jefferson, Arkansas is the headquarters of the National Center for Toxicological Research
While most of the Centers are located in the
Washington, D.C. area as part of the Headquarters divisions, two offices – the Office of Regulatory Affairs (ORA) and the
Office of Criminal Investigations (OCI) – are primarily field offices with a workforce spread across the country.
The Office of Regulatory Affairs is considered the "eyes and
ears" of the agency, conducting the vast majority of the FDA's work in
the field. Consumer Safety Officers, more commonly called Investigators,
are the individuals who inspect production and warehousing facilities,
investigate complaints, illnesses, or outbreaks, and review
documentation in the case of medical devices, drugs, biological
products, and other items where it may be difficult to conduct a
physical examination or take a physical sample of the product.
The Office of Regulatory Affairs is divided into five regions,
which are further divided into 20 districts. Districts are based roughly
on the geographic divisions of the
federal court system.
Each district comprises a main district office and a number of Resident
Posts, which are FDA remote offices that serve a particular geographic
area. ORA also includes the Agency's network of regulatory laboratories,
which analyze any physical samples taken. Though samples are usually
food-related, some laboratories are equipped to analyze drugs,
cosmetics, and radiation-emitting devices.
The Office of Criminal Investigations was established in 1991 to
investigate criminal cases. Unlike ORA Investigators, OCI Special Agents
are armed, and don't focus on technical aspects of the regulated
industries. OCI agents pursue and develop cases where individuals and
companies have committed criminal actions, such as fraudulent claims, or
knowingly and willfully shipping known adulterated goods in interstate
commerce. In many cases, OCI pursues cases involving
Title 18
violations (e.g., conspiracy, false statements, wire fraud, mail
fraud), in addition to prohibited acts as defined in Chapter III of the
FD&C Act. OCI Special Agents often come from other criminal
investigations backgrounds, and work closely with the
Federal Bureau of Investigation,
Assistant Attorney General, and even
Interpol.
OCI receives cases from a variety of sources—including ORA, local
agencies, and the FBI—and works with ORA Investigators to help develop
the technical and science-based aspects of a case. OCI is a smaller
branch, comprising about 200 agents nationwide.
Scope and funding
The FDA regulates more than US$2.4 trillion worth of consumer goods, about 25% of consumer expenditures in the
United States.
This includes $466 billion in food sales, $275 billion in drugs, $60
billion in cosmetics and $18 billion in vitamin supplements. Much of
these expenditures are for goods imported into the United States; the
FDA is responsible for monitoring imports.
The FDA's federal budget request for fiscal year (FY) 2012 totaled $4.36 billion, while the proposed 2014 budget is $4.7 billion. About $2 billion of this budget is generated by user fees.
Pharmaceutical firms pay the majority of these fees, which are used to expedite drug reviews.
The FDA's federal budget request for fiscal year (FY) 2008 (October
2007 through September 2008) totaled $2.1 billion, a $105.8 million
increase from what it received for fiscal year 2007.
In February 2008, the FDA announced that the Bush
Administration's FY 2009 budget request for the agency was just under
$2.4 billion: $1.77 billion in budget authority (federal funding) and
$628 million in user fees. The requested budget authority was an
increase of $50.7 million more than the FY 2008 funding – about a three
percent increase. In June 2008, Congress gave the agency an emergency
appropriation of $150 million for FY 2008 and another $150 million.
Regulatory programs
As of 2015, the agency regulates more than $1 trillion in consumer products, including:
- $466 billion in food
- $275 billion in drugs
- $60 billion in cosmetics
- $18 billion in vitamin supplements
The programs for safety regulation vary widely by the type of
product, its potential risks, and the regulatory powers granted to the
agency. For example, the FDA regulates almost every facet of
prescription drugs, including testing, manufacturing, labeling,
advertising, marketing, efficacy, and safety—yet FDA regulation of
cosmetics focuses primarily on labeling and safety. The FDA regulates
most products with a set of published standards enforced by a modest
number of facility inspections. Inspection observations are documented
on
Form 483.
In June 2018, the FDA released a
statement
regarding new guidelines to help food and drug manufacturers "implement
protections against potential attacks on the U.S. food supply".
One of the new guidelines includes the Intentional Adulteration (IA)
rule, which requires strategies and procedures by the food industry to
reduce the risk of compromise in facilities and processes that are
significantly vulnerable.
Canada-United States Regulatory Cooperation Council
On February 4, 2011,
Prime Minister of Canada Stephen Harper and
United States President Barack Obama issued a "Declaration on a Shared Vision for Perimeter Security and Economic Competitiveness"
and announced the creation of the Canada-United States Regulatory
Cooperation Council (RCC) "to increase regulatory transparency and
coordination between the two countries".
Health Canada
and the United States Food and Drug Administration (FDA) under the RCC
mandate, undertook the "first of its kind" initiative by selecting "as
its first area of alignment common cold indications for certain
over-the-counter antihistamine ingredients (GC 2013-01-10)."
Food and dietary supplements
The regulation of food and dietary supplements by the U.S. Food and
Drug Administration is governed by various statutes enacted by the
United States Congress and interpreted by the FDA. Pursuant to the
Federal Food, Drug, and Cosmetic Act
("the Act") and accompanying legislation, the FDA has authority to
oversee the quality of substances sold as food in the United States, and
to monitor claims made in the
labeling about both the composition and the health benefits of foods.
The FDA subdivides substances that it regulates as food into various categories—including foods,
food additives, added substances (man-made substances that are not intentionally introduced into food, but nevertheless end up in it), and
dietary supplements.
Specific standards the FDA exercises differ from one category to the
next. Furthermore, legislation had granted the FDA a variety of means to
address violations of standards for a given substance category.
"FDA-Approved" vs. "FDA-Accepted in Food Processing"
The FDA does not approve applied coatings used in the
food processing industry.
There is no review process to approve the composition of nonstick
coatings, nor does the FDA inspect or test these materials. Through
their governing of processes, however, the FDA does have a set of
regulations that cover the formulation, manufacturing, and use of
nonstick coatings. Hence, materials like
Polytetrafluoroethylene (Teflon) are not, and cannot be, considered as FDA Approved, rather, they are "FDA Compliant" or "FDA Acceptable".
Medications
FDA Building 51 houses the Center for Drug Evaluation and Research.
The
Center for Drug Evaluation and Research
uses different requirements for the three main drug product types: new
drugs, generic drugs, and over-the-counter drugs. A drug is considered
"new" if it is made by a different manufacturer, uses different
excipients
or inactive ingredients, is used for a different purpose, or undergoes
any substantial change. The most rigorous requirements apply to
new molecular entities: drugs that are not based on existing medications.
New medications
New drugs receive extensive scrutiny before FDA approval in a process called a
new drug application (NDA).
Critics, however, argue that the FDA standards are not sufficiently
rigorous, allowing unsafe or ineffective drugs to be approved.
New drugs are available only by prescription by default. A change to
over-the-counter (OTC) status is a separate process, and the drug must
be approved through an NDA first. A drug that is approved is said to be
"safe and effective when used as directed".
Some very rare limited exceptions to this multi-step process
involving animal testing and controlled clinical trials can be granted
out of compassionate use protocols, as was the case during the 2015
Ebola epidemic with the use, by prescription and authorization, of
ZMapp
and other experimental treatments, and for new drugs that can be used
to treat debilitating and/or very rare conditions for which no existing
remedies or drugs are satisfactory, or where there has not been an
advance in a long period of time. The studies are progressively longer,
gradually adding more individuals as they progress from stage I to stage
III, normally over a period of years, and normally involve drug
companies, the government and its laboratories, and often medical
schools and hospitals and clinics. However, any exceptions to the
aforementioned process are subject to strict review and scrutiny and
conditions, and are only given if a substantial amount of research and
at least some preliminary human testing has shown that they are believed
to be somewhat safe and possibly effective.
Advertising and promotion
The
FDA's Office of Prescription Drug Promotion reviews and regulates
prescription drug advertising and promotion through surveillance
activities and issuance of enforcement letters to pharmaceutical
manufacturers. Advertising and promotion for over-the-counter drugs is
regulated by the
Federal Trade Commission.
The drug advertising regulation
contains two broad requirements: (1) a company may advertise or promote
a drug only for the specific indication or medical use for which it was
approved by FDA. Also, an advertisement must contain a "fair balance"
between the benefits and the risks (side effects) of a drug.
The term
off-label refers to drug usage for indications other than those approved by the FDA.
Postmarket safety surveillance
After
NDA approval, the sponsor must review and report to the FDA every
patient adverse drug experience it learns of. They must report
unexpected serious and fatal adverse drug events within 15 days, and
other events on a quarterly basis.
The FDA also receives directly adverse drug event reports through its
MedWatch program. These reports are called "spontaneous reports" because reporting by consumers and health professionals is voluntary.
While this remains the primary tool of
postmarket safety surveillance, FDA requirements for postmarketing risk management are increasing.
As a condition of approval, a sponsor may be required to conduct additional
clinical trials,
called Phase IV trials.
In some cases, the FDA requires risk management plans ("Risk Evaluation
and Mitigation Strategy" or "REMS") for some drugs that require actions
to be taken to ensure that the drug is used safely. For example,
thalidomide
can cause birth defects but has uses that outweigh the risks if men and
women taking the drugs do not conceive a child; a REMS program for
thalidomide mandates an auditable process to ensure that people taking
the drug take action to avoid pregnancy; many
opioid drugs have REMS programs to avoid addiction and diversion of drugs. There is also a REMS program called
iPLEDGE for the drug,
isotretinoin.
Generic drugs
Generic drugs are chemical equivalents of
name-brand drugs whose patents have expired.
In general, they are less expensive than their name brand counterparts,
are manufactured and marketed by other companies and, in the 1990s,
accounted for about a third of all prescriptions written in the United
States.
For approval of a generic drug, the U.S. Food and Drug Administration
(FDA) requires scientific evidence that the generic drug is
interchangeable with or therapeutically equivalent to the originally
approved drug. This is called an "ANDA" (
Abbreviated New Drug Application). As of 2012 80% of all FDA approved drugs are available in generic form.
Generic drug scandal
In 1989, a major scandal erupted involving the procedures used by the FDA to approve generic drugs for sale to the public.
Charges of corruption in generic drug approval first emerged in 1988,
in the course of an extensive congressional investigation into the FDA.
The oversight subcommitee of the
United States House Energy and Commerce Committee resulted from a complaint brought against the FDA by
Mylan Laboratories Inc.
of Pittsburgh. When its application to manufacture generics were
subjected to repeated delays by the FDA, Mylan, convinced that it was
being discriminated against, soon began its own private investigation of
the agency in 1987. Mylan eventually filed suit against two former FDA
employees and four drug-manufacturing companies, charging that
corruption within the federal agency resulted in
racketeering and in violations of
antitrust law.
"The order in which new generic drugs were approved was set by the FDA
employees even before drug manufacturers submitted applications" and,
according to Mylan, this illegal procedure was followed to give
preferential treatment to certain companies. During the summer of 1989,
three FDA officials (Charles Y. Chang, David J. Brancato, Walter Kletch)
pleaded guilty to criminal charges of accepting bribes from generic
drugs makers, and two companies (
Par Pharmaceutical and its subsidiary Quad Pharmaceuticals) pleaded guilty to giving bribes.
Furthermore, it was discovered that several manufacturers had
falsified data submitted in seeking FDA authorization to market certain
generic drugs. Vitarine Pharmaceuticals of New York, which sought
approval of a generic version of the drug
Dyazide,
a medication for high blood pressure, submitted Dyazide, rather than
its generic version, for the FDA tests. In April 1989, the FDA
investigated 11 manufacturers for irregularities; and later brought that
number up to 13. Dozens of drugs were eventually suspended or recalled
by manufacturers. In the early 1990s, the
U.S. Securities and Exchange Commission
filed securities fraud charges against the Bolar Pharmaceutical
Company, a major generic manufacturer based in Long Island, New York.
Over-the-counter drugs
Over-the-counter (OTC) drugs like
aspirin are drugs and combinations that do not require a doctor's prescription.
The FDA has a list of approximately 800 approved ingredients that are
combined in various ways to create more than 100,000 OTC drug products.
Many OTC drug ingredients had been previously approved prescription
drugs now deemed safe enough for use without a
medical practitioner's supervision like
ibuprofen.
Ebola treatment
In 2014, the FDA added an
Ebola treatment being developed by Canadian pharmaceutical company Tekmira to the
Fast Track program,
but halted the phase 1 trials in July pending the receipt of more
information about how the drug works. This is seen as increasingly
important in the face of a
major outbreak of the disease in West Africa that began in late March 2014 and continued as of August 2014.
Vaccines, blood and tissue products, and biotechnology
FDA scientist prepares blood donation samples for testing
The
Center for Biologics Evaluation and Research is the branch of the FDA responsible for ensuring the safety and efficacy of biological therapeutic agents.
These include blood and blood products, vaccines, allergenics, cell and
tissue-based products, and gene therapy products. New biologics are
required to go through a premarket approval process called a Biologics
License Application (BLA), similar to that for drugs.
Medical and radiation-emitting devices
The Center for Devices and Radiological Health
CDRH regulatory powers include the authority to require certain
technical reports from the manufacturers or importers of regulated
products, to require that radiation-emitting products meet mandatory
safety performance standards, to declare regulated products defective,
and to order the recall of defective or noncompliant products. CDRH also
conducts limited amounts of direct product testing.
"FDA-Cleared" vs "FDA-Approved"
Clearance
requests are for medical devices that prove they are "substantially
equivalent" to the predicate devices already on the market. Approved
requests are for items that are new or substantially different and need
to demonstrate "safety and efficacy", for example it may be inspected
for safety in case of new toxic hazards. Both aspects need to be proved
or provided by the submitter to ensure proper procedures are followed.
Cosmetics
Cosmetics are regulated by the
Center for Food Safety and Applied Nutrition,
the same branch of the FDA that regulates food. Cosmetic products are
not, in general, subject to premarket approval by the FDA unless they
make "structure or function claims" that make them into drugs.
However, all color additives must be specifically FDA approved before
manufacturers can include them in cosmetic products sold in the U.S. The
FDA regulates cosmetics labeling, and cosmetics that have not been
safety tested must bear a warning to that effect.
Though the cosmetic industry is predominantly responsible in
ensuring the safety of its products, the FDA also has the power to
intervene when necessary to protect the public but in general does not
require pre-market approval or testing. Companies are required to place
a warning note on their products if they have not been tested. Experts
in cosmetic ingredient reviews also play a role in monitoring safety
through influence on the use of ingredients, but also lack legal
authority. Overall the organization has reviewed about 1,200
ingredients and has suggested that several hundred be restricted, but
there is no standard or systemic method for reviewing chemicals for
safety and a clear definition of what is meant by 'safety' so that all
chemicals are tested on the same basis.
Veterinary products
CVM's primary focus is on medications that are used in food
animals and ensuring that they do not affect the human food supply. The
FDA's requirements to prevent the spread of
bovine spongiform encephalopathy are also administered by CVM through inspections of feed manufacturers.
Tobacco products
In 2009, Congress passed a law requiring color warnings on
cigarette packages and on printed advertising, in addition to text
warnings from the U.S. Surgeon General.
The nine new graphic warning labels were announced by the FDA in
June 2011 and were scheduled to be required to appear on packaging by
September 2012. The implementation date is uncertain, due to ongoing
proceedings in the case of R.J. Reynolds Tobacco Co. v. U.S. Food and
Drug Administration.
R.J. Reynolds,
Lorillard,
Commonwealth Brands Inc., Liggett Group LLC and
Santa Fe Natural Tobacco Company
Inc. have filed suit in Washington, D.C. federal court claiming that
the graphic labels are an unconstitutional way of forcing tobacco
companies to engage in anti-smoking advocacy on the government's behalf.
A
First Amendment lawyer,
Floyd Abrams,
is representing the tobacco companies in the case, contending requiring
graphic warning labels on a lawful product cannot withstand
constitutional scrutiny.
The Association of National Advertisers and the American Advertising
Federation have also filed a brief in the suit, arguing that the labels
infringe on commercial free speech and could lead to further government
intrusion if left unchallenged.
In November 2011, Federal judge Richard Leon of the U.S. District Court
for the District of Columbia temporarily halted the new labels, likely
delaying the requirement that tobacco companies display the labels. The
U.S. Supreme Court ultimately could decide the matter.
In July 2017, the FDA announced a plan that would reduce the current levels of nicotine permitted in tobacco cigarettes.
Regulation of living organisms
With
acceptance of premarket notification 510(k) k033391 in January 2004,
the FDA granted Dr. Ronald Sherman permission to produce and market
medical maggots for use in humans or other animals as a prescription medical device.
Medical maggots
represent the first living organism allowed by the Food and Drug
Administration for production and marketing as a prescription medical
device.
In June 2004, the FDA cleared
Hirudo medicinalis (medicinal leeches) as the second living organism to be used as a medical device.
Science and research programs
FDA lab at Building 64 in Silver Spring, Maryland
In addition to its regulatory functions, the FDA
carries out research and development activities
to develop technology and standards that support its regulatory role,
with the objective of resolving scientific and technical challenges
before they become impediments. The FDA's research efforts include the
areas of biologics, medical devices, drugs, women's health, toxicology,
food safety and applied nutrition, and veterinary medicine.
Data management
The FDA has collected a large amount of data through decades. In March 2013,
OpenFDA was created to enable easy access of the data for the public.
History
Up until the 20th century, there were few federal laws regulating the
contents and sale of domestically produced food and pharmaceuticals,
with one exception being the short-lived
Vaccine Act of 1813. The history of the FDA can be traced to the latter part of the 19th century and the
U.S. Department of Agriculture's
Division of Chemistry, later its
Bureau of Chemistry. Under
Harvey Washington Wiley,
appointed chief chemist in 1883, the Division began conducting research
into the adulteration and misbranding of food and drugs on the American
market. Wiley's advocacy came at a time when the public had become
aroused to hazards in the marketplace by
muckraking journalists like
Upton Sinclair, and became part of a general trend for increased federal regulations in matters pertinent to public safety during the
Progressive Era. The 1902
Biologics Control Act was put in place after a
diphtheria
antitoxin—derived from tetanus-contaminated serum—was used to produce a
vaccine that caused the deaths of thirteen children in St. Louis,
Missouri. The serum was originally collected from a
horse named Jim, who had contracted tetanus.
In June 1906, President
Theodore Roosevelt signed into law the
Pure Food and Drug Act, also known as the "Wiley Act" after its chief advocate.
The Act prohibited, under penalty of seizure of goods, the interstate
transport of food that had been "adulterated". The act applied similar
penalties to the interstate marketing of "adulterated" drugs, in which
the "standard of strength, quality, or purity" of the active ingredient
was not either stated clearly on the label or listed in the
United States Pharmacopoeia or the
National Formulary.
The responsibility for examining food and drugs for such
"adulteration" or "misbranding" was given to Wiley's USDA Bureau of
Chemistry.
Wiley used these new regulatory powers to pursue an aggressive campaign
against the manufacturers of foods with chemical additives, but the
Chemistry Bureau's authority was soon checked by judicial decisions,
which narrowly defined the bureau's powers and set high standards for
proof of fraudulent intent.
In 1927, the Bureau of Chemistry's regulatory powers were reorganized
under a new USDA body, the Food, Drug, and Insecticide organization.
This name was shortened to the Food and Drug Administration (FDA) three
years later.
By the 1930s, muckraking journalists, consumer protection
organizations, and federal regulators began mounting a campaign for
stronger regulatory authority by publicizing a list of injurious
products that had been ruled permissible under the 1906 law, including
radioactive beverages, the
mascara Lash lure, which caused blindness, and worthless "cures" for
diabetes and
tuberculosis. The resulting proposed law was unable to get through the
Congress of the United States for five years, but was rapidly enacted into law following the public outcry over the 1937
Elixir Sulfanilamide tragedy, in which over 100 people died after using a drug formulated with a toxic, untested solvent.
President
Franklin Delano Roosevelt signed the new
Food, Drug, and Cosmetic Act
(FD&C Act) into law on June 24, 1938. The new law significantly
increased federal regulatory authority over drugs by mandating a
pre-market review of the safety of all new drugs, as well as banning
false therapeutic claims in drug labeling without requiring that the FDA
prove fraudulent intent. Soon after passage of the 1938 Act, the FDA
began to designate certain drugs as safe for use only under the
supervision of a medical professional, and the category of "
prescription-only" drugs was securely codified into law by the 1951
Durham-Humphrey Amendment. These developments confirmed extensive powers for the FDA to enforce post-marketing recalls of ineffective drugs.
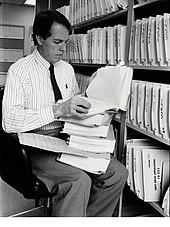
Medical
Officer Alexander Fleming, M. D., examines a portion of a 240-volume
new drug application around the late 1980s. Applications grew
considerably after the efficacy mandate under the 1962 Drug Amendments.
In 1959, the
thalidomide
tragedy, in which thousands of European babies were born deformed after
their mothers took that drug – marketed for treatment of nausea –
during their pregnancies, Considering the US was largely spared that tragedy because Dr.
Frances Oldham Kelsey of the FDA refused to authorize the medication for market, the 1962
Kefauver-Harris Amendment to the FD&C Act was passed, which represented a "revolution" in FDA regulatory authority.
The most important change was the requirement that all new drug
applications demonstrate "substantial evidence" of the drug's efficacy
for a marketed indication, in addition to the existing requirement for
pre-marketing demonstration of safety. This marked the start of the FDA
approval process in its modern form.
These reforms had the effect of increasing the time, and the difficulty, required to bring a drug to market. One of the most important statutes in establishing the modern American pharmaceutical market was the 1984
Drug Price Competition and Patent Term Restoration Act,
more commonly known as the "Hatch-Waxman Act" after its chief sponsors.
The act extended the patent exclusivity terms of new drugs, and tied
those extensions, in part, to the length of the FDA approval process for
each individual drug. For generic manufacturers, the Act created a new
approval mechanism, the Abbreviated New Drug Application (ANDA), in
which the generic drug manufacturer need only demonstrate that their
generic formulation has the same active ingredient, route of
administration, dosage form, strength, and
pharmacokinetic
properties ("bioequivalence") as the corresponding brand-name drug.
This act has been credited with in essence creating the modern generic
drug industry.
Concerns about the length of the drug approval process were brought to the fore early in the
AIDS epidemic. In the mid- and late 1980s,
ACT-UP and other
HIV
activist organizations accused the FDA of unnecessarily delaying the
approval of medications to fight HIV and opportunistic infections.
Partly in response to these criticisms, the FDA issued new rules to
expedite approval of drugs for life-threatening diseases, and expanded
pre-approval access to drugs for patients with limited treatment
options. All of the initial drugs approved for the treatment of HIV/AIDS were approved through these accelerated approval mechanisms.
Frank Young, the commissioner of the FDA was behind the Action Plan
Phase II, established in August 1987 for quicker approval of AIDS
medication.
In two instances, state governments have sought to legalize drugs
that the FDA has not approved. Under the theory that federal law passed
pursuant to Constitutional authority overrules conflicting state laws,
federal authorities still claim the authority to seize, arrest, and
prosecute for possession and sales of these substances, even in states where they are legal under state law. The first wave was the legalization by 27 states of
laetrile
in the late 1970s. This drug was used as a treatment for cancer, but
scientific studies both before and after this legislative trend found it
to be ineffective. The second wave concerned
medical marijuana
in the 1990s and 2000s. Though Virginia passed a law with limited
effect in 1979, a more widespread trend began in California in 1996.
Historical first: FDA and Endo Pharmaceutical's Opana ER (2017)
21st century reforms
Critical Path Initiative
The Critical Path Initiative
is FDA's effort to stimulate and facilitate a national effort to
modernize the sciences through which FDA-regulated products are
developed, evaluated, and manufactured. The Initiative was launched in
March 2004, with the release of a report entitled Innovation/Stagnation:
Challenge and Opportunity on the Critical Path to New Medical Products.
Patients' rights to access unapproved drugs
A 2006 court case,
Abigail Alliance v. von Eschenbach,
would have forced radical changes in FDA regulation of unapproved
drugs. The Abigail Alliance argued that the FDA must license drugs for
use by terminally ill patients with "desperate diagnoses," after they
have completed Phase I testing. The case won an initial appeal in May 2006, but that decision was reversed by a March 2007 rehearing. The
US Supreme Court declined to hear the case, and the final decision denied the existence of a right to unapproved medications.
Critics
of the FDA's regulatory power argue that the FDA takes too long to
approve drugs that might ease pain and human suffering faster if brought
to market sooner. The AIDS crisis created some political efforts to
streamline the approval process. However, these limited reforms were
targeted for AIDS drugs, not for the broader market. This has led to
the call for more robust and enduring reforms that would allow patients,
under the care of their doctors, access to drugs that have passed the
first round of clinical trials.
Post-marketing drug safety monitoring
The widely publicized recall of
Vioxx, a
non-steroidal anti-inflammatory drug now estimated to have contributed to fatal
heart attacks
in thousands of Americans, played a strong role in driving a new wave
of safety reforms at both the FDA rulemaking and statutory levels. Vioxx
was approved by the FDA in 1999, and was initially hoped to be safer
than previous NSAIDs, due to its reduced risk of intestinal tract
bleeding. However, a number of pre- and post-marketing studies suggested
that Vioxx might increase the risk of myocardial infarction, and this
was conclusively demonstrated by results from the APPROVe trial in 2004.
Faced with numerous lawsuits, the manufacturer voluntarily
withdrew it from the market. The example of Vioxx has been prominent in
an ongoing debate over whether new drugs should be evaluated on the
basis of their absolute safety, or their safety relative to existing
treatments for a given condition. In the wake of the Vioxx recall, there
were widespread calls by major newspapers, medical journals, consumer
advocacy organizations, lawmakers, and FDA officials for reforms in the FDA's procedures for pre- and post- market drug safety regulation.
In 2006, a congressionally requested committee was appointed by the
Institute of Medicine
to review pharmaceutical safety regulation in the U.S. and to issue
recommendations for improvements. The committee was composed of 16
experts, including leaders in clinical medicinemedical research,
economics,
biostatistics, law, public policy, public health, and the allied health professions, as well as current and former executives from the
pharmaceutical, hospital, and
health insurance
industries. The authors found major deficiencies in the current FDA
system for ensuring the safety of drugs on the American market. Overall,
the authors called for an increase in the regulatory powers, funding,
and independence of the FDA.
Some of the committee's recommendations have been incorporated into
drafts of the PDUFA IV bill, which was signed into law in 2007.
As of 2011, Risk Minimization Action Plans (RiskMAPS) have been
created to ensure risks of a drug never outweigh the benefits of that
drug within the postmarketing period. This program requires that
manufacturers design and implement periodic assessments of their
programs' effectiveness. The Risk Minimization Action Plans are set in
place depending on the overall level of risk a prescription drug is
likely to pose to the public.
Pediatric drug testing
Prior
to the 1990s, only 20% of all drugs prescribed for children in the
United States were tested for safety or efficacy in a pediatric
population. This became a major concern of
pediatricians
as evidence accumulated that the physiological response of children to
many drugs differed significantly from those drugs' effects on adults.
Children react different to the drugs because of many reason, including
size, weight, etc. There were several reasons that not many medical
trials were done with children. For many drugs, children represented
such a small proportion of the potential market, that drug manufacturers
did not see such testing as cost-effective.
Also, because children were thought to be ethically restricted in their ability to give
informed consent,
there were increased governmental and institutional hurdles to approval
of these clinical trials, as well as greater concerns about
legal liability.
Thus, for decades, most medicines prescribed to children in the U.S.
were done so in a non-FDA-approved, "off-label" manner, with dosages
"extrapolated" from adult data through body weight and body-surface-area
calculations.
An initial attempt by the FDA to address this issue was the 1994
FDA Final Rule on Pediatric Labeling and Extrapolation, which allowed
manufacturers to add pediatric labeling information, but required drugs
that had not been tested for pediatric safety and efficacy to bear a
disclaimer to that effect. However, this rule failed to motivate many
drug companies to conduct additional pediatric drug trials. In 1997, the
FDA proposed a rule to require pediatric drug trials from the sponsors
of New Drug Applications. However, this new rule was successfully
preempted in federal court as exceeding the FDA's statutory authority.
While this debate was unfolding, Congress used the 1997
Food and Drug Administration Modernization Act
to pass incentives that gave pharmaceutical manufacturers a six-month
patent term extension on new drugs submitted with pediatric trial data.
The act reauthorizing these provisions, the 2002
Best Pharmaceuticals for Children Act,
allowed the FDA to request NIH-sponsored testing for pediatric drug
testing, although these requests are subject to NIH funding constraints.
In the Pediatric Research Equity Act of 2003, Congress codified the
FDA's authority to mandate manufacturer-sponsored pediatric drug trials
for certain drugs as a "last resort" if incentives and publicly funded
mechanisms proved inadequate.
Priority review voucher (PRV)
The
priority review voucher is a provision of the Food and Drug Administration Amendments Act (HR 3580) signed by President
George W. Bush
signed the bill in September 2007 which awards a transferable "priority
review voucher" to any company that obtains approval for a treatment
for a
neglected tropical diseases. The system was first proposed by
Duke University faculty David Ridley, Henry Grabowski, and Jeffrey Moe in their 2006
Health Affairs paper: "Developing Drugs for Developing Countries".
In 2012, President Obama signed into law the FDA Safety and Innovation
Act which includes Section 908 the "Rare Pediatric Disease Priority
Review Voucher Incentive Program".
Rules for generic biologics
Biotechnology drugs do not have the simple, readily verifiable
chemical structures of conventional drugs, and are produced through
complex, often proprietary techniques, such as transgenic mammalian cell
cultures. Because of these complexities, the 1984
Hatch-Waxman Act did not include biologics in the
Abbreviated New Drug Application
(ANDA) process, in essence precluding the possibility of generic drug
competition for biotechnology drugs. In February 2007, identical bills
were introduced into the House to create an ANDA process for the
approval of generic biologics, but were not passed.
Mobile medical applications
In 2013, a guidance was issued to regulate
mobile medical applications
and protect users from their unintended use. This guidance
distinguishes the apps subjected to regulation based on the marketing
claims of the apps.
Incorporation of the guidelines during the development phase of such
app has been proposed for expedite market entry and clearance.
Criticisms
The FDA has regulatory oversight over a large array of products that affect the health and life of American citizens.
As a result, the FDA's powers and decisions are carefully monitored by
several governmental and non-governmental organizations. A $1.8 million
2006
Institute of Medicine
report on pharmaceutical regulation in the U.S. found major
deficiencies in the current FDA system for ensuring the safety of drugs
on the American market. Overall, the authors called for an increase in
the
regulatory powers, funding, and independence of the FDA.
Nine FDA scientists appealed to then president-elect
Barack Obama over pressures from management, experienced during the
George W. Bush
presidency, to manipulate data, including in relation to the review
process for medical devices. Characterized as "corrupted and distorted
by current FDA managers, thereby placing the American people at risk,"
these concerns were also highlighted in the 2006 report on the agency as well.
The FDA has also been criticized from the opposite viewpoint, as
being too tough on industry. According to an analysis published on the
website of the
libertarian Mercatus Center
as well as published statements by economists, medical practitioners,
and concerned consumers, many feel the FDA oversteps its regulatory
powers and undermines small business and small farms in favor of large
corporations. Three of the FDA restrictions under analysis are the
permitting of new drugs and devices, the control of manufacturer speech,
and the imposition of prescription requirements. The authors argue that
in the increasingly complex and diverse food marketplace, the FDA is
not equipped to adequately regulate or inspect food. In addition, excessive regulation is blamed for the rising costs of health care and the creation of
monopolies, as potential competitors are unable to get FDA approval to enter the market to compete and keep
health care costs down.
However, in an indicator that the FDA may be too lax in their
approval process, in particular for medical devices, a 2011 study by Dr.
Diana Zuckerman and Paul Brown of the
National Research Center for Women and Families, and Dr. Steven Nissen of the
Cleveland Clinic,
published in the Archives of Internal Medicine, showed that most
medical devices recalled in the last five years for "serious health
problems or death" had been previously approved by the FDA using the
less stringent, and cheaper, 510(k) process. In a few cases the devices
had been deemed so low-risk that they did not need FDA regulation. Of
the 113 devices recalled, 35 were for cardiovascular health purposes.