| Behaviour therapy | |
|---|---|
| ICD-9-CM | 94.33 |
| MeSH | D001521 |
Behavior therapy or behavioral psychotherapy is a broad term referring to clinical psychotherapy that uses techniques derived from behaviorism. Those who practice behavior therapy tend to look at specific, learned behaviors and how the environment influences those behaviors. Those who practice behavior therapy are called behaviourists, or behavior analysts. They tend to look for treatment outcomes that are objectively measurable. Behavior therapy does not involve one specific method but it has a wide range of techniques that can be used to treat a person's psychological problems. Traditional behavior therapy draws from respondent conditioning and operant conditioning to solve patients problems.
Behavioral psychotherapy is sometimes juxtaposed with cognitive psychotherapy, while cognitive behavioral therapy integrates aspects of both approaches.
Applied behavior analysis (ABA) is the application of behavior analysis that focuses on assessing how environmental variables influence learning principles, particularly respondent and operant conditioning, to identify potential behavior-change procedures, which are frequently used throughout clinical therapy. Cognitive-behavior therapy views cognition and emotions as preceding overt behavior with treatment plans in psychotherapy to lessen the issue. Hallmark techniques of behaviour therapies are overlapping components of cognitive psychology, in addition to behaviour analytic principles of counterconditioning, punishment, habituation, and functional analysis (FA).
History
Precursors of certain fundamental aspects of behaviour therapy have
been identified in various ancient philosophical traditions,
particularly Stoicism. For example, Wolpe and Lazarus wrote,
While the modern behavior therapist deliberately applies principles of learning to this therapeutic operations, empirical behavior therapy is probably as old as civilization – if we consider civilization as having started when man first did things to further the well-being of other men. From the time that this became a feature of human life there must have been occasions when a man complained of his ills to another who advised or persuaded him of a course of action. In a broad sense, this could be called behavior therapy whenever the behavior itself was conceived as the therapeutic agent. Ancient writings contain innumerable behavioral prescriptions that accord with this broad conception of behavior therapy.
The first use of the term behaviour modification appears to have been by Edward Thorndike in 1911. His article Provisional Laws of Acquired Behavior or Learning makes frequent use of the term "modifying behavior". Through early research in the 1940s and the 1950s the term was used by Joseph Wolpe's research group. The experimental tradition in clinical psychology
used it to refer to psycho-therapeutic techniques derived from
empirical research. It has since come to refer mainly to techniques for
increasing adaptive behaviour through reinforcement and decreasing
maladaptive behaviour through extinction or punishment (with emphasis on
the former). Two related terms are behaviour therapy and applied behaviour analysis.
Since techniques derived from behavioural psychology tend to be the
most effective in altering behaviour, most practitioners consider
behaviour modification along with behaviour therapy and applied
behaviour analysis to be founded in behaviourism.
While behaviour modification and applied behaviour analysis typically
uses interventions based on the same behavioural principles, many
behaviour modifiers who are not applied behaviour analysts tend to use
packages of interventions and do not conduct functional assessments
before intervening.
Possibly the first occurrence of the term "behavior therapy" was in a 1953 research project by B.F. Skinner, Ogden Lindsley, Nathan H. Azrin and Harry C. Solomon.
The paper talked about operant conditioning and how it could be used to
help improve the functioning of people who were diagnosed with chronic
schizophrenia. Early pioneers in behaviour therapy include Joseph Wolpe and Hans Eysenck.
In general, behaviour therapy is seen as having three distinct
points of origin: South Africa (Wolpe's group), The United States
(Skinner), and the United Kingdom (Rachman and Eysenck). Each had its
own distinct approach to viewing behaviour problems. Eysenck in
particular viewed behaviour problems as an interplay between personality
characteristics, environment, and behaviour. Skinner's group in the United States took more of an operant conditioning focus. The operant focus created a functional approach to assessment and interventions focused on contingency management such as the token economy and behavioural activation. Skinner's student Ogden Lindsley is credited with forming a movement called precision teaching,
which developed a particular type of graphing program called the
standard celeration chart to monitor the progress of clients. Skinner
became interested in the individualising of programs for improved
learning in those with or without disabilities and worked with Fred S. Keller to develop programmed instruction. Programmed instruction had some clinical success in aphasia rehabilitation. Gerald Patterson used programme instruction to develop his parenting text for children with conduct problems. With age, respondent conditioning appears to slow but operant conditioning remains relatively stable.
While the concept had its share of advocates and critics in the west,
its introduction in the Asian setting, particularly in India in the
early 1970s and its grand success were testament to the famous Indian psychologist H. Narayan Murthy's enduring commitment to the principles of behavioural therapy and biofeedback.
While many behaviour therapists remain staunchly committed to the basic operant and respondent paradigm, in the second half of the 20th century, many therapists coupled behaviour therapy with the cognitive therapy, of Aaron Beck, Albert Ellis, and [Donald Meichenbaum (psychologist)]]to form cognitive behaviour therapy.
In some areas the cognitive component had an additive effect (for
example, evidence suggests that cognitive interventions improve the
result of social phobia treatment.)
but in other areas it did not enhance the treatment, which led to the
pursuit of third generation behaviour therapies. Third generation
behaviour therapy uses basic principles of operant and respondent
psychology but couples them with functional analysis and a clinical formulation/case
conceptualisation of verbal behaviour more inline with view of the
behaviour analysts. Some research supports these therapies as being more
effective in some cases than cognitive therapy, but overall the question is still in need of answers.
Theoretical basis
The behavioural approach to therapy assumes that behaviour that
is associated with psychological problems develops through the same
processes of learning that affects the development of other behaviours.
Therefore, behaviourists see personality problems in the way that
personality was developed. They do not look at behaviour disorders as
something a person has but that it reflects how learning has influenced
certain people to behave in a certain way in certain situations.
Behaviour therapy is based upon the principles of classical conditioning developed by Ivan Pavlov and operant conditioning developed by B.F. Skinner.
Classical conditioning happens when a neutral stimulus comes right
before another stimulus that triggers a reflexive response. The idea is
that if the neutral stimulus and whatever other stimulus that triggers a
response is paired together often enough that the neutral stimulus will
produce the reflexive response. Operant conditioning has to do with rewards and punishments and how they can either strengthen or weaken certain behaviours.
Contingency management programs are a direct product of research from operant conditioning. These programs have been highly successful with those suffering from panic disorders, anxiety disorders, and phobias.
Systematic desensitisation and exposure and response prevention both evolved from respondent conditioning and have also received considerable research.
Behavior avoidance test (BAT) is a behavioural procedure in which
the therapist measures how long the client can tolerate an
anxiety-inducing stimulus.
The BAT falls under the exposure-based methods of behaviour therapy.
Exposure-based methods of behavioural therapy are well suited to the
treatment of phobias, which include intense and unreasonable fears
(e.g., of spiders, blood, public speaking).
The therapist needs some type of behavioural assessment to record the
continuing progress of a client undergoing an exposure-based treatment
for phobia. One simple assessment approach for this is the BAT. The BAT
approach is predicted on the assumption that the client's fear is the
main determinant of behaviour in the testing situation. BAT can be
conducted visual, virtually, or physically, depending on the clients'
maladaptive behaviour. Its application is not limited to phobias, it is
applied to various disorders such as post-traumatic stress disorder (PTSD) and obsessive-compulsive disorder (OCD).
Current forms
Behavioral therapy based on operant and respondent principles has considerable evidence base to support its usage. This approach remains a vital area of clinical psychology and is often termed clinical behavior analysis. Behavioral psychotherapy has become increasingly contextual in recent years. Behavioral psychotherapy has developed greater interest in recent years in personality disorders as well as a greater focus on acceptance and complex case conceptualizations.
Functional analytic psychotherapy
One current form of behavioral psychotherapy is functional analytic psychotherapy. Functional analytic psychotherapy is a longer duration behavior therapy. Functional analytic therapy focuses on in-session use of reinforcement and is primarily a relationally-based therapy. As with most of the behavioral psychotherapies, functional analytic psychotherapy is contextual in its origins and nature. and draws heavily on radical behaviorism and functional contextualism.
Functional analytic psychotherapy holds to a process model of research, which makes it unique compared to traditional behavior therapy and cognitive behavioral therapy.
Functional analytic psychotherapy has a strong research support.
Recent functional analytic psychotherapy research efforts are focusing
on management of aggressive inpatients.
Assessment
Behaviour
therapists complete a functional analysis or a functional assessment
that looks at four important areas: stimulus, organism, response and
consequences. The stimulus is the condition or environmental trigger that causes behaviour. An organism involves the internal responses of a person, like physiological responses, emotions and cognition.
A response is the behaviour that a person exhibits and the consequences
are the result of the behaviour. These four things are incorporated
into an assessment done by the behaviour therapist.
Most behaviour therapists use objective assessment methods like
structured interviews, objective psychological tests or different
behavioural rating forms. These types of assessments are used so that
the behaviour therapist can determine exactly what a client's problem
may be and establish a baseline for any maladaptive responses that the
client may have. By having this baseline, as therapy continues this same
measure can be used to check a client's progress, which can help
determine if the therapy is working. Behaviour therapists do not
typically ask the why questions but tend to be more focused on the how,
when, where and what questions. Tests such as the Rorschach inkblot test
or personality tests like the MMPI (Minnesota Multiphasic Personality Inventory)
are not commonly used for behavioural assessment because they are based
on personality trait theory assuming that a person's answer to these
methods can predict behaviour. Behaviour assessment is more focused on
the observations of a persons behaviour in their natural environment.
Behavioural assessment specifically attempts to find out what the
environmental and self-imposed variables are. These variables are the
things that are allowing a person to maintain their maladaptive
feelings, thoughts and behaviours. In a behavioural assessment "person
variables" are also considered. These "person variables" come from a
person's social learning history and they effect the way in which the
environment affects that person's behaviour. An example of a person
variable would be behavioural competence. Behavioural competence looks
at whether a person has the appropriate skills and behaviours that are
necessary when performing a specific response to a certain situation or
stimuli.
When making a behavioural assessment the behaviour therapist
wants to answer two questions: (1) what are the different factors
(environmental or psychological) that are maintaining the maladaptive
behaviour and (2) what type of behaviour therapy or technique that can
help the individual improve most effectively. The first question
involves looking at all aspects of a person, which can be summed up by
the acronym BASIC ID. This acronym stands for behaviour, affective
responses, sensory reactions, imagery, cognitive processes,
interpersonal relationships and drug use.
Clinical applications
Behaviour
therapy based its core interventions on functional analysis. Just a few
of the many problems that behaviour therapy have functionally analysed
include intimacy in couples relationships, forgiveness in couples, chronic pain, stress-related behaviour problems of being an adult child of an alcoholic, anorexia, chronic distress, substance abuse, depression, anxiety, insomnia, and obesity.
Functional analysis has even been applied to problems that
therapists commonly encounter like client resistance, partially engaged
clients and involuntary clients.
Applications to these problems have left clinicians with considerable
tools for enhancing therapeutic effectiveness. One way to enhance
therapeutic effectiveness is to use positive reinforcement or operant
conditioning. Although behaviour therapy is based on the general
learning model, it can be applied in a lot of different treatment
packages that can be specifically developed to deal with problematic
behaviours. Some of the more well known types of treatments are:
Relaxation training, systematic desensitization, virtual reality
exposure, exposure and response prevention techniques, social skills
training, modeling, behavioural rehearsal and homework, and aversion therapy and punishment.
Relaxation training involves clients learning to lower arousal to
reduce their stress by tensing and releasing certain muscle groups
throughout their body.
Systematic desensitization is a treatment in which the client slowly
substitutes a new learned response for a maladaptive response by moving
up a hierarchy of situations involving fear.
Systematic desensitization is based in part on counter conditioning.
Counter conditioning is learning new ways to change one response for
another and in the case of desensitization it is substituting that
maladaptive behaviour for a more relaxing behaviour. Exposure and response prevention techniques (also known as flooding and response prevention)
is the general technique in which a therapist exposes an individual to
anxiety-provoking stimuli while keeping them from having any avoidance
responses.
Virtual reality therapy provides realistic, computer-based
simulations of troublesome situations. The modeling process involves a
person being subjected to watching other individuals who demonstrate
behaviour that is considered adaptive and that should be adopted by the
client. This exposure involves not only the cues of the "model person"
as well as the situations of a certain behaviour that way the
relationship can be seen between the appropriateness of a certain
behaviour and situation in which that behaviour occurs is demonstrated.
With the behavioural rehearsal and homework treatment a client gets a
desired behaviour during a therapy session and then they practice and
record that behaviour between their sessions. Aversion therapy
and punishment is a technique in which an aversive (painful or
unpleasant) stimulus is used to decrease unwanted behaviours from
occurring. It is concerned with two procedures: 1) the procedures are
used to decrease the likelihood of the frequency of a certain behaviour
and 2) procedures that will reduce the attractiveness of certain
behaviours and the stimuli that elicit them.
The punishment side of aversion therapy is when an aversive stimulus is
presented at the same time that a negative stimulus and then they are
stopped at the same time when a positive stimulus or response is
presented. Examples of the type of negative stimulus or punishment that can be used is shock therapy treatments, aversive drug treatments as well as response cost contingent punishment which involves taking away a reward.
Applied behaviour analysis is using behavioural methods to modify
certain behaviours that are seen as being important socially or
personally. There are four main characteristics of applied behaviour
analysis. First behaviour analysis is focused mainly on overt behaviours
in an applied setting. Treatments are developed as a way to alter the
relationship between those overt behaviours and their consequences.
Another characteristic of applied behaviour analysis is how
it(behaviour analysis) goes about evaluating treatment effects. The
individual subject is where the focus of study is on, the investigation
is centered on the one individual being treated. A third characteristic
is that it focuses on what the environment does to cause significant
behaviour changes. Finally the last characteristic of applied behaviour
analysis is the use of those techniques that stem from operant and
classical conditioning such as providing reinforcement, punishment,
stimulus control and any other learning principles that may apply.
Social skills training teaches clients skills to access reinforcers and lessen life punishment. Operant conditioning procedures in meta-analysis had the largest effect size for training social skills, followed by modelling, coaching, and social cognitive techniques in that order. Social skills training has some empirical support particularly for schizophrenia. However, with schizophrenia, behavioural programs have generally lost favor.
Some other techniques that have been used in behaviour therapy
are contingency contracting, response costs, token economies,
biofeedback, and using shaping and grading task assignments.
Shaping and graded task assignments are used when behaviour that
needs to be learned is complex. The complex behaviours that need to be
learned are broken down into simpler steps where the person can achieve
small things gradually building up to the more complex behaviour. Each
step approximates the eventual goal and helps the person to expand their
activities in a gradual way. This behaviour is used when a person feels
that something in their lives can not be changed and life's tasks
appear to be overwhelming.
Another technique of behaviour therapy involves holding a client
or patient accountable of their behaviours in an effort to change them.
This is called a contingency contract, which is a formal written
contract between two or more people that defines the specific expected
behaviours that you wish to change and the rewards and punishments that
go along with that behaviour.
In order for a contingency contract to be official it needs to have
five elements. First it must state what each person will get if they
successfully complete the desired behaviour. Secondly those people
involved have to monitor the behaviours. Third, if the desired behaviour
is not being performed in the way that was agreed upon in the contract
the punishments that were defined in the contract must be done. Fourth
if the persons involved are complying with the contract they must
receive bonuses. The last element involves documenting the compliance
and noncompliance while using this treatment in order to give the
persons involved consistent feedback about the target behaviour and the
provision of reinforcers.
Token economies is a behaviour therapy technique where clients
are reinforced with tokens that are considered a type of currency that
can be used to purchase desired rewards, like being able to watch
television or getting a snack that they want when they perform
designated behaviours.
Token economies are mainly used in institutional and therapeutic
settings. In order for a token economy to be effective their must be
consistency in administering the program by the entire staff. Procedures
must be clearly defined so that there is no confusion among the
clients. Instead of looking for ways to punish the patients or to deny
them of rewards, the staff has to reinforce the positive behaviours so
that the clients will increase the occurrence of the desired behaviour.
Over time the tokens need to be replaced with less tangible rewards such
as compliments so that the client will be prepared when they leave the
institution and won't expect to get something every time they perform a
desired behaviour.
Closely related to token economies is a technique called response
costs. This technique can either be used with or without token
economies. Response costs is the punishment side of token economies
where there is a loss of a reward or privilege after someone performs an
undesirable behaviour. Like token economies this technique is used mainly in institutional and therapeutic settings.
Considerable policy implications have been inspired by
behavioural views of various forms of psychopathology. One form of
behaviour therapy, habit reversal training, has been found to be highly effective for treating tics.
In rehabilitation
Currently, there is a greater call for behavioral psychologists to be involved in rehabilitation efforts.
Treatment of mental disorders
Two large studies done by the Faculty of Health Sciences at Simon
Fraser University
indicates that both behaviour therapy and cognitive-behavioural therapy
(CBT) are equally effective for OCD. CBT has been shown to perform
slightly better at treating co-occurring depression.
Considerable policy implications have been inspired by
behavioural views of various forms of psychopathology. One form of
behaviour therapy (habit reversal training) has been found to be highly effective for treating tics.
There has been a development towards combining techniques to
treat psychiatric disorders. Cognitive interventions are used to enhance
the effects of more established behavioural interventions based on
operant and classical conditioning. An increased effort has also been
placed to address the interpersonal context of behaviour.
Behaviour therapy can be applied to a number of mental disorders
and in many cases is more effective for specific disorders as compared
to others. Behaviour therapy techniques can be used to deal with any
phobias that a person may have. Desensitization has also been applied to
other issues such as dealing with anger, if a person has trouble
sleeping and certain speech disorders.
Desensitization does not occur over night, there is a process of
treatment. Desensitization is done on a hierarchy and happens over a
number of sessions. The hierarchy goes from situations that make a person less anxious or nervous up to things that are considered to be extreme for the patient.
Modeling has been used in dealing with fears and phobias.
Modeling has been used in the treatment of fear of snakes as well as a
fear of water.
Aversive therapy techniques have been used to treat sexual deviations as well as alcoholism.
Exposure and prevention procedure techniques can be used to treat
people who have anxiety problems as well as any fears or phobias.
These procedures have also been used to help people dealing with any
anger issues as well as pathological grievers (people who have
distressing thoughts about a deceased person).
Virtual reality therapy deals with fear of heights, fear of flying, and a variety of other anxiety disorders.
VRT has also been applied to help people with substance abuse problems
reduce their responsiveness to certain cues that trigger their need to
use drugs.
Shaping and graded task assignments has been used in dealing with
suicide and depressed or inhibited individuals. This is used when a
patient feel hopeless and they have no way of changing their lives. This
hopelessness involves how the person reacts and responds to someone
else and certain situations and their perceived powerlessness to change
that situation that adds to the hopelessness. For a person with suicidal
ideation, it is important to start with small steps. Because that
person may perceive everything as being a big step, the smaller you
start the easier it will be for the person to master each step.
This technique has also been applied to people dealing with
agoraphobia, or fear of being in public places or doing something
embarrassing.
Contingency contracting has been used to deal with behaviour
problems in delinquents and when dealing with on task behaviours in
students.
Token economies are used in controlled environments and are found
mostly in psychiatric hospitals. They can be used to help patients with
different mental illnesses but it doesn't focus on the treatment of the
mental illness but instead on the behavioural aspects of a patient.
The response cost technique has been used to address a variety of
behaviours such as smoking, overeating, stuttering, and psychotic talk.
Treatment outcomes
Systematic desensitization has been shown to successfully treat
phobias about heights, driving, insects as well as any anxiety that a
person may have. Anxiety can include social anxiety, anxiety about
public speaking as well as test anxiety. It has been shown that the use
of systematic desensitization is an effective technique that can be
applied to a number of problems that a person may have.
When using modeling procedures this technique is often compared
to another behavioural therapy technique. When compared to
desensitization, the modeling technique does appear to be less
effective.
However it is clear that the greater the interaction between the
patient and the subject he is modeling the greater the effectiveness of
the treatment.
While undergoing exposure therapy a person usually needs five
sessions to see if the treatment is working. After five sessions
exposure treatment is seen to benefit the patient and help with their
problems. However even after five sessions it is recommended that the
patient or client should still continue treatment.
Virtual Reality treatment has shown to be effective for a fear of heights. It has also been shown to help with the treatment of a variety of anxiety disorders.
Virtual reality therapy can be very costly so therapists are still
awaiting results of controlled trials for VR treatment to see which
applications show the best results.
For those with suicidal ideation treatment depends on how severe
the person's depression and feeling of hopelessness is. If these things
are severe the person's response to completing small steps will not be
of importance to them because they don't consider it to be a big deal.
Generally those who aren't severely depressed or fearful, this
technique has been successful because the completion of simpler
activities build up their confidences and allows them to continue on to
more complex situations.
Contingency contracts have been seen to be effective in changing
any undesired behaviours of individuals. It has been seen to be
effective in treating behaviour problems in delinquents regardless of
the specific characteristics of the contract.
Token economies have been shown to be effective when treating
patients in psychiatric wards who had chronic schizophrenia. The results
showed that the contingent tokens were controlling the behaviour of the
patients.
Response costs has been shown to work in suppressing a variety of
behaviours such as smoking, overeating or stuttering with a diverse
group of clinical populations ranging from sociopaths to school
children. These behaviours that have been suppressed using this
technique often do not recover when the punishment contingency is
withdrawn. Also undesirable side effects that are usually seen with
punishment are not typically found when using the response cost
technique.
Third generation
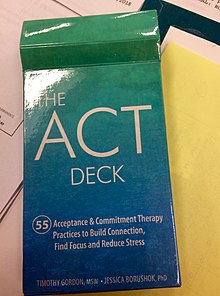
The third-generation behaviour therapy movement has been called clinical behavior analysis because it represents a movement away from cognitivism and back toward radical behaviourism and other forms of behaviourism, in particular functional analysis and behavioural models of verbal behaviour. This area includes acceptance and commitment therapy (ACT), cognitive behavioral analysis system of psychotherapy (CBASP) (McCullough, 2000), behavioural activation (BA), functional analytic psychotherapy (FAP), integrative behavioural couples therapy and dialectical behavioural therapy. These approaches are squarely within the applied behaviour analysis tradition of behaviour therapy.
ACT may be the most well-researched of all the third-generation behaviour therapy models. It is based on relational frame theory.
Other authors object to the term "third generation" or "third wave" and
incorporate many of the "third wave" therapeutic techniques under the
general umbrella term of modern cognitive behavioral therapies.
Functional analytic psychotherapy is based on a functional analysis of the therapeutic relationship. It places a greater emphasis on the therapeutic context and returns to the use of in-session reinforcement. In general, 40 years of research supports the idea that in-session reinforcement of behaviour can lead to behavioural change.
Behavioural activation
emerged from a component analysis of cognitive behaviour therapy. This
research found no additive effect for the cognitive component. Behavioural activation is based on a matching model of reinforcement.
A recent review of the research, supports the notion that the use of
behavioural activation is clinically important for the treatment of
depression.
Integrative behavioural couples therapy
developed from dissatisfaction with traditional behavioural couples
therapy. Integrative behavioural couples therapy looks to Skinner (1966)
for the difference between contingency-shaped and rule-governed
behaviour.
It couples this analysis with a thorough functional assessment of the
couple's relationship. Recent efforts have used radical behavioural
concepts to interpret a number of clinical phenomena including
forgiveness.
Organizations
Many organisations exist for behaviour therapists around the world. The Association for Behavior Analysis International (ABAI) provides accreditation for training programs in behaviour therapy. The ABAI has a special interest group for practitioner issues, behavioral counseling, and clinical behavior analysis ABA:I. ABAI has larger special interest groups for autism and its peculiar and narrow interpretation of behavioral medicine. ABAI serves as the core intellectual home for behavior analysts. ABAI sponsors two conferences/year – one in the U.S. and one international.
In the United States, the American Psychological Association's Division 25 is the division for behaviour analysis.
The Association for Contextual Behavior Therapy is another professional
organisation. ACBS is home to many clinicians with specific interest in
third generation behaviour therapy. Doctoral-level behavior analysts
who are psychologists belong to American Psychological Association's division 25 – Behavior analysis. APA offers a diplomate in behavioral psychology.
The Association for Behavioral and Cognitive Therapies
(formerly the Association for the Advancement of Behavior Therapy) is
for those with a more cognitive orientation. The ABCT also has an
interest group in behavior analysis,
which focuses on clinical behavior analysis. In addition, the
Association for Behavioral an Cognitive Therapies has a special interest
group on addictions.
The World Association for Behavior Analysis offers a certification in behavior therapy.
Characteristics
By
nature, behavioural therapies are empirical (data-driven), contextual
(focused on the environment and context), functional (interested in the
effect or consequence a behaviour ultimately has), probabilistic
(viewing behaviour as statistically predictable), monistic (rejecting mind–body dualism and treating the person as a unit), and relational (analysing bidirectional interactions).
Behavioural therapy develops, adds and provides behavioural
intervention strategies and programs for clients, and training to people
who care to facilitate successful lives in the communities.
Training
Recent efforts in behavioral psychotherapy have focused on the supervision process. A key point of behavioral models of supervision is that the supervisory process parallels the behavioral psychotherapy.
Methods
- Behaviour management
- Behaviour modification
- Clinical behavior analysis
- Contingency management
- Covert conditioning
- Exposure and response prevention
- Flooding
- Habit reversal training
- Matching law
- Modeling
- Observational learning
- Operant conditioning
- Professional practice of behavior analysis
- Respondent conditioning
- Systematic desensitisation