| Vitamin K | |
|---|---|
| Drug class | |

Vitamin K structures. MK-4 and MK-7 are both subtypes of K2.
| |
| Class identifiers | |
| Use | Vitamin K deficiency, Warfarin overdose |
| ATC code | B02BA |
| Biological target | Gamma-glutamyl carboxylase |
| Clinical data | |
| Drugs.com | Medical Encyclopedia |
| External links | |
| MeSH | D014812 |
Vitamin K is a group of structurally similar, fat-soluble vitamins found in foods and in dietary supplements. The human body requires vitamin K for complete synthesis of certain proteins that are needed for blood coagulation (K from koagulation, Danish for "coagulation") or for controlling binding of calcium in bones and other tissues. The vitamin K–related modification of the proteins allows them to bind calcium ions, which they cannot do otherwise. Without vitamin K, blood coagulation is seriously impaired, and uncontrolled bleeding occurs. Preliminary clinical research indicates that deficiency of vitamin K may weaken bones, potentially leading to osteoporosis, and may promote calcification of arteries and other soft tissues.
Chemically, the vitamin K family comprises 2-methyl-1,4-naphthoquinone (3-) derivatives. Vitamin K includes two natural vitamers: vitamin K1 and vitamin K2. Vitamin K2, in turn, consists of a number of related chemical subtypes, with differing lengths of carbon side chains made of isoprenoid groups of atoms.
Vitamin K1, also known as phylloquinone, is made by plants, and is found in highest amounts in green leafy vegetables because it is directly involved in photosynthesis. It may be thought of as the plant form of vitamin K. It is active as a vitamin in animals and performs the classic functions of vitamin K, including its activity in the production of blood-clotting proteins. Animals may also convert it to vitamin K2.
Bacteria in the gut flora can also convert K1 into vitamin K2 (menaquinone). In addition, bacteria typically lengthen the isoprenoid side chain of vitamin K2 to produce a range of vitamin K2 forms, most notably the MK-7 to MK-11 homologues of vitamin K2. All forms of K2 other than MK-4 can only be produced by bacteria, which use these during anaerobic respiration. The MK-7 and other bacterially derived forms of vitamin K2 exhibit vitamin K activity in animals, but MK-7's extra utility over MK-4, if any, is unclear and is a matter of investigation.
Because a synthetic form of vitamin K, vitamin K3 (menadione), may be toxic by interfering with the function of glutathione, it is no longer used to treat vitamin K deficiency.
Medical uses
Warfarin overdose and coumarin poisoning
Vitamin K is one of the treatments for bleeding events caused by overdose of the anticoagulant drug warfarin (Coumadin®). It can be administered by mouth, intravenously, or subcutaneously. Vitamin K is also used in situations when a patient's INR is greater than 10 and there is no active bleeding.
Vitamin K is also part of the suggested treatment regime for poisoning by rodenticide (coumarin poisoning).[6]
Vitamin K treatment may only be necessary in people who deliberately
have consumed large amounts of rodenticide or have consumed an unknown
amount of rodenticide. Patients are given oral vitamin K1 to
prevent the negative effects of rodenticide poisoning, and this dosing
must sometimes be continued for up to nine months in cases of poisoning
by "superwarfarin" rodenticides such as brodifacoum. Oral Vitamin K1 is preferred over other vitamin K1 routes of administration because it has less side effects.
Vitamin K deficiency bleeding in newborns
Vitamin K is given as an injection to newborns to prevent vitamin K deficiency bleeding.
The blood clotting factors of newborn babies are roughly 30–60% that of
adult values; this may be due to the reduced synthesis of precursor
proteins and the sterility of their guts. Human milk contains 1–4 μg/L of vitamin K1, while formula-derived milk can contain up to 100 μg/L in supplemented formulas. Vitamin K2 concentrations in human milk appear to be much lower than those of vitamin K1.
Occurrence of vitamin K deficiency bleeding in the first week of the
infant's life is estimated at 0.25–1.7%, with a prevalence of 2–10 cases
per 100,000 births. Premature babies have even lower levels of the vitamin, so they are at a higher risk from this deficiency.
Bleeding in infants due to vitamin K deficiency can be severe, leading to hospitalization, blood transfusions, brain damage,
and death. Supplementation can prevent most cases of vitamin K
deficiency bleeding in the newborn. Intramuscular injection, typically
given shortly after birth, is more effective in preventing late vitamin K
deficiency bleeding than oral administration.
Osteoporosis
There is no good evidence that vitamin K supplementation benefits the bone health of postmenopausal women.
Cardiovascular health
Adequate intake of vitamin K is associated with the inhibition of arterial calcification and stiffening,
but there have been few interventional studies and no good evidence
that vitamin K supplementation is of any benefit in the primary
prevention of cardiovascular disease.
One 10-year population study, the Rotterdam Study, did show a
clear and significant inverse relationship between the highest intake
levels of menaquinone (mainly MK-4 from eggs and meat, and MK-8 and MK-9
from cheese) and cardiovascular disease and all-cause mortality in
older men and women.
Cancer
Vitamin K has been promoted in supplement form with claims it can slow tumor growth; however, no good medical evidence supports such claims.
Side effects
Although allergic reaction from supplementation is possible, no known toxicity is associated with high doses of the phylloquinone (vitamin K1) or menaquinone (vitamin K2) forms of vitamin K, so no tolerable upper intake level (UL) has been set. Specifically vitamin K1
has been associated with severe adverse reactions such as bronchospasm
and cardiac arrest when given intravenously as opposed to orally.
Blood clotting (coagulation) studies in humans using 45 mg per day of vitamin K2 (as MK-4) and even up to 135 mg per day (45 mg three times daily) of K2 (as MK-4),
showed no increase in blood clot risk. Even doses in rats as high as
250 mg/kg body weight did not alter the tendency for blood-clot
formation to occur.
Unlike the safe natural forms of vitamin K1 and vitamin K2 and their various isomers, a synthetic form of vitamin K, vitamin K3 (menadione), is demonstrably toxic at high levels. The U.S. FDA has banned this form from over-the-counter sale in the United States because large doses have been shown to cause allergic reactions, hemolytic anemia, and cytotoxicity in liver cells.
Interactions
Phylloquinone (K1) or menaquinone (K2) are capable of reversing the anticoagulant activity of the anticoagulant warfarin
(tradename Coumadin). Warfarin works by blocking recycling of vitamin
K, so that the body and tissues have lower levels of active vitamin K,
and thus a deficiency of vitamin K.
Supplemental vitamin K (for which oral dosing is often more
active than injectable dosing in human adults) reverses the vitamin K
deficiency caused by warfarin, and therefore reduces the intended
anticoagulant action of warfarin and related drugs.
Sometimes small amounts of vitamin K are given orally to patients
taking warfarin so that the action of the drug is more predictable.
The proper anticoagulant action of the drug is a function of vitamin K
intake and drug dose, and due to differing absorption must be
individualized for each patient.
The action of warfarin and vitamin K both require two to five days
after dosing to have maximum effect, and neither warfarin nor vitamin K
shows much effect in the first 24 hours after they are given.
The newer anticoagulants apixaban, dabigatran and rivaroxaban have different mechanisms of action that do not interact with vitamin K, and may be taken with supplemental vitamin K.
Chemistry
Vitamin K2 (menaquinone). In menaquinone, the side chain is composed of a varying number of isoprenoid residues. The most common number of these residues is four, since animal enzymes normally produce menaquinone-4 from plant phylloquinone.
The structure of phylloquinone, Vitamin K1, is marked by the presence of a phytyl group.
The structures of menaquinones are marked by the polyisoprenyl side
chain present in the molecule that can contain four to 13 isoprenyl
units.
A sample of phytomenadione for injection, also called phylloquinone
The three synthetic forms of vitamin K are vitamins K3 (menadione), K4, and K5, which are used in many areas, including the pet food industry (vitamin K3) and to inhibit fungal growth (vitamin K5).
Conversion of vitamin K1 to vitamin K2
Vitamin K1 (phylloquinone) – both forms of the vitamin contain a functional naphthoquinone ring and an aliphatic side chain. Phylloquinone has a phytyl side chain.
The MK-4 form of vitamin K2 is produced by conversion of vitamin K1 in the testes, pancreas, and arterial walls. While major questions still surround the biochemical pathway for this transformation, the conversion is not dependent on gut bacteria, as it occurs in germ-free rats and in parenterally administered K1 in rats. In fact, tissues that accumulate high amounts of MK-4 have a remarkable capacity to convert up to 90% of the available K1 into MK-4. There is evidence that the conversion proceeds by removal of the phytyl tail of K1 to produce menadione as an intermediate, which is then condensed with an activated geranylgeranyl moiety (see also prenylation) to produce vitamin K2 in the MK-4 (menatetrenone) form.
Vitamin K2
Vitamin K2 (menaquinone) includes several subtypes. The two most studied ones are menaquinone-4 (menatetrenone, MK-4) and menaquinone-7 (MK-7).
Physiology
Vitamin K1 (phylloquinone), the precursor of most vitamin K in nature, is an important chemical in green plants, where it functions as an electron acceptor in photosystem I during photosynthesis. For this reason, vitamin K1 is found in large quantities in the photosynthetic tissues of plants (green leaves, and dark green leafy vegetables such as romaine lettuce, kale, and spinach), but it occurs in far smaller quantities in other plant tissues (roots, fruits, etc.). Iceberg lettuce
contains relatively little. The function of phylloquinone in plants
appears to have no resemblance to its later metabolic and biochemical
function (as "vitamin K") in animals, where it performs a completely
different biochemical reaction.
Vitamin K (in animals) is involved in the carboxylation of certain glutamate residues in proteins to form gamma-carboxyglutamate (Gla) residues. The modified residues are often (but not always) situated within specific protein domains called Gla domains. Gla residues are usually involved in binding calcium, and are essential for the biological activity of all known Gla proteins.
At this time, 17 human proteins with Gla domains have been
discovered, and they play key roles in the regulation of three
physiological processes:
- Blood coagulation: prothrombin (factor II), factors VII, IX, and X, and proteins C, S, and Z.
- Bone metabolism: osteocalcin, also called bone Gla protein (BGP), matrix Gla protein (MGP), periostin, and the recently discovered Gla-rich protein (GRP).
- Vascular biology: growth arrest-specific protein 6 (Gas6).
- Unknown function: proline-rich γ-carboxyglutamyl proteins (PRGPs) 1 and 2, and transmembrane γ-carboxy glutamyl proteins (TMGs) 3 and 4.
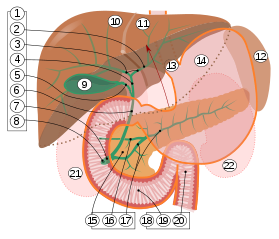
When Vitamin K1 enters the body through foods in a person's diet, it is absorbed through the jejunum and ileum in the small intestine, and like other lipid-soluble vitamins (A, D, and E), vitamin K is stored in the fatty tissue of the human body.
Absorption and dietary need
Previous theory held that dietary deficiency is extremely rare unless the small intestine was heavily damaged, resulting in malabsorption of the molecule. Another at-risk group for deficiency were those subject to decreased production of K2 by normal intestinal microbiota, as seen in broad-spectrum antibiotic use.
Taking broad-spectrum antibiotics can reduce vitamin K production in
the gut by nearly 74% in people compared with those not taking these
antibiotics. Diets low in vitamin K also decrease the body's vitamin K concentration. Those with chronic kidney disease are at risk for vitamin K deficiency, as well as vitamin D deficiency, and particularly those with the apoE4 genotype. Additionally, the elderly have a reduction in vitamin K2.
Dietary recommendations
The
U.S. Institute of Medicine (IOM) updated Estimated Average Requirements
(EARs) and Recommended Dietary Allowances (RDAs) for vitamin K in 1998.
The IOM does not distinguish between K1 and K2 –
both are counted as vitamin K. At that time, sufficient information was
not available to establish EARs and RDAs for vitamin K. In instances
such as these, the board sets Adequate Intakes (AIs), with the
understanding that at some later date, AIs will be replaced by more
exact information. The current AIs for adult women and men ages 19 and
up are 90 and 120 μg/day, respectively. AI for pregnancy is 90 μg/day.
AI for lactation is 90 μg/day. For infants up to 12 months, the AI is
2.0–2.5 μg/day; for children ages 1–18 years the AI increases with age
from 30 to 75 μg/day. As for safety, the IOM sets tolerable upper intake levels
(known as ULs) for vitamins and minerals when evidence is sufficient.
Vitamin K has no UL, as human data for adverse effects from high doses
are inadequate. Collectively, the EARs, RDAs, AIs and ULs are referred
to as Dietary Reference Intakes.
The European Food Safety Authority
(EFSA) refers to the collective set of information as Dietary Reference
Values, with Population Reference Intake (PRI) instead of RDA, and
Average Requirement instead of EAR. AI and UL are defined the same as in
United States. For women and men over age 18 the AI is set at 70
μg/day. AI for pregnancy is 70 μg/day, ad for lactation 70 μg/day. For
children ages 1–17 years, the AIs increase with age from 12 to 65
μg/day. These AIs are lower than the U.S. RDAs.
The EFSA also reviewed the safety question and reached the same
conclusion as in United States – that there was not sufficient evidence
to set a UL for vitamin K.
For U.S. food and dietary supplement labeling purposes, the
amount in a serving is expressed as a percentage of Daily Value (%DV).
For vitamin K labeling purposes, 100% of the Daily Value was 80 μg, but
as of May 27, 2016, it was revised upwards to 120 μg, to bring it into
agreement with the AI. A table of the old and new adult Daily Values is provided at Reference Daily Intake.
The original deadline to be in compliance was July 28, 2018, but on
September 29, 2017, the FDA released a proposed rule that extended the
deadline to January 1, 2020 for large companies and January 1, 2021 for
small companies.
Food sources
Vitamin K1
| Food | Serving size | Vitamin K1 (μg) |
|
Food | Serving size | Vitamin K1 (μg) |
|---|---|---|---|---|---|---|
| Kale, cooked | 1 cup | 531 | Parsley, raw | 1⁄4 cup | 246 | |
| Spinach, cooked | 1⁄2 cup, 77g | 444 | Spinach, raw | 1 cup | 145 | |
| Collards, cooked | 1⁄2 cup | 418 | Collards, raw | 1 cup | 184 | |
| Swiss chard, cooked | 1⁄2 cup | 287 | Swiss chard, raw | 1 cup | 299 | |
| Mustard greens, cooked | 1⁄2 cup | 210 | Mustard greens, raw | 1 cup | 279 | |
| Turnip greens, cooked | 1⁄2 cup | 265 | Turnip greens, raw | 1 cup | 138 | |
| Broccoli, cooked | 1 cup | 220 | Broccoli, raw | 1 cup | 89 | |
| Brussels sprouts, cooked | 1 cup | 219 | Endive, raw | 1 cup | 116 | |
| Cabbage, cooked | 1⁄2 cup | 82 | Green leaf lettuce | 1 cup | 71 | |
| Dandelion, green leaves | 100 gram | 778.4 μg or 741% of daily dose. | ||||
| Asparagus | 4 spears | 48 | ||||
| Romaine lettuce, raw | 1 cup | 57 | ||||
| Table from "Important information to know when you are taking: Warfarin (Coumadin) and Vitamin K", Clinical Center, National Institutes of Health Drug Nutrient Interaction Task Force. | ||||||
Vitamin K1 is found chiefly in leafy green vegetables such as spinach, swiss chard, lettuce and Brassica vegetables (such as cabbage, kale, cauliflower, broccoli, and brussels sprouts) and often the absorption is greater when accompanied by fats such as butter or oils. Some fruits, such as avocados, kiwifruit and grapes, also contain vitamin K. Some vegetable oils, notably soybean oil, contain vitamin K, but at levels that would require relatively large calorie consumption to meet the recommended amounts.
The tight binding of vitamin K1 to thylakoid membranes in chloroplasts makes it less bioavailable.
For example, cooked spinach has a 5% bioavailability of phylloquinone,
however, fat added to it increases bioavailability to 13% due to the
increased solubility of vitamin K in fat.
Vitamin K2
Vitamin K2 can be found in eggs, dairy, and meat, as well as fermented foods such as cheese and yogurt.
Deficiency
Average diets are usually not lacking in vitamin K, and primary
deficiency is rare in healthy adults. Newborn infants are at an
increased risk of deficiency. Other populations with an increased
prevalence of vitamin K deficiency include those who suffer from liver damage or disease (e.g. alcoholics), cystic fibrosis, or inflammatory bowel diseases, or have recently had abdominal surgeries. Secondary vitamin K deficiency can occur in people with bulimia, those on stringent diets, and those taking anticoagulants. Other drugs associated with vitamin K deficiency include salicylates, barbiturates, and cefamandole,
although the mechanisms are still unknown. Vitamin K deficiency has
been defined as a vitamin K-responsive hypoprothrombinemia which
increase prothrombin time and thus can result in coagulopathy, a bleeding disorder. Symptoms of K1 deficiency include anemia, bruising, nosebleeds and bleeding of the gums in both sexes, and heavy menstrual bleeding in women.
Osteoporosis and coronary heart disease are strongly associated with lower levels of K2 (menaquinone). Vitamin K2 (as menaquinones MK-4 through MK-10) intake level is inversely related to severe aortic calcification and all-cause mortality.
Biochemistry
Function in animals
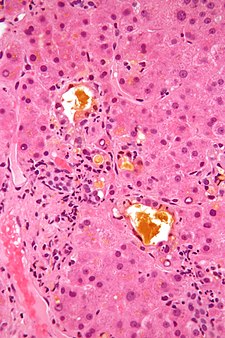
Mechanism of action of vitamin K1.
Vitamin K epoxide
In both cases R represents the isoprenoid side chain
The function of vitamin K2 in the animal cell is to add a carboxylic acid functional group to a glutamate (Glu) amino acid residue in a protein, to form a gamma-carboxyglutamate (Gla) residue. This is a somewhat uncommon posttranslational modification
of the protein, which is then known as a "Gla protein". The presence of
two −COOH (carboxylic acid) groups on the same carbon in the
gamma-carboxyglutamate residue allows it to chelate calcium ions.
The binding of calcium ions in this way very often triggers the
function or binding of Gla-protein enzymes, such as the so-called
vitamin K-dependent clotting factors discussed below.
Within the cell, vitamin K undergoes electron reduction to a reduced form called vitamin K hydroquinone, catalyzed by the enzyme vitamin K epoxide reductase (VKOR). Another enzyme then oxidizes vitamin K hydroquinone to allow carboxylation of Glu to Gla; this enzyme is called gamma-glutamyl carboxylase
or the vitamin K-dependent carboxylase. The carboxylation reaction only
proceeds if the carboxylase enzyme is able to oxidize vitamin K
hydroquinone to vitamin K epoxide at the same time. The carboxylation
and epoxidation reactions are said to be coupled. Vitamin K epoxide is
then reconverted to vitamin K by VKOR. The reduction and subsequent
reoxidation of vitamin K coupled with carboxylation of Glu is called the
vitamin K cycle. Humans are rarely deficient in vitamin K1 because, in part, vitamin K1 is continuously recycled in cells.
Warfarin and other 4-hydroxycoumarins block the action of VKOR.
This results in decreased concentrations of vitamin K and vitamin K
hydroquinone in tissues, such that the carboxylation reaction catalyzed
by the glutamyl carboxylase is inefficient. This results in the
production of clotting factors with inadequate Gla. Without Gla on the amino termini of these factors, they no longer bind stably to the blood vessel endothelium and cannot activate clotting
to allow formation of a clot during tissue injury. As it is impossible
to predict what dose of warfarin will give the desired degree of
clotting suppression, warfarin treatment must be carefully monitored to
avoid overdose.
Gamma-carboxyglutamate proteins
The following human Gla-containing proteins ("Gla proteins") have
been characterized to the level of primary structure: blood coagulation
factors II (prothrombin), VII, IX, and X, anticoagulant protein C and protein S, and the factor X-targeting protein Z. The bone Gla protein osteocalcin, the calcification-inhibiting matrix Gla protein (MGP), the cell growth
regulating growth arrest specific gene 6 protein (Gas6), and the four
transmembrane Gla proteins (TMGPs), the function of which is at present
unknown. Gas6 can function as a growth factor to activate the Axl receptor tyrosine kinase and stimulate cell proliferation or prevent apoptosis
in some cells. In all cases in which their function was known, the
presence of the Gla residues in these proteins turned out to be
essential for functional activity.
Gla proteins are known to occur in a wide variety of vertebrates: mammals, birds, reptiles, and fish. The venom
of a number of Australian snakes acts by activating the human
blood-clotting system. In some cases, activation is accomplished by
snake Gla-containing enzymes that bind to the endothelium
of human blood vessels and catalyze the conversion of procoagulant
clotting factors into activated ones, leading to unwanted and
potentially deadly clotting.
Another interesting class of invertebrate Gla-containing proteins is synthesized by the fish-hunting snail Conus geographus. These snails produce a venom containing hundreds of neuroactive peptides, or conotoxins, which is sufficiently toxic to kill an adult human. Several of the conotoxins contain two to five Gla residues.
Methods of assessment
Vitamin K status can be assessed by:
- The prothrombin time (PT) test measures the time required for blood to clot. A blood sample is mixed with citric acid and put in a fibrometer; delayed clot formation indicates a deficiency. This test is insensitive to mild deficiency, as the values do not change until the concentration of prothrombin in the blood has declined by at least 50%.
- Undercarboxylated prothrombin (PIVKA-II); in a study of 53 newborns, found "PT (prothrombin time) is a less sensitive marker than PIVKA II", and as indicated above, PT is unable to detect subclinical deficiencies that can be detected with PIVKA-II testing.
- Plasma phylloquinone was found to be positively correlated with phylloquinone intake in elderly British women, but not men, but an article by Schurgers et al. reported no correlation between responses in a food frequency questionnaire and plasma phylloquinone.
- Urinary γ-carboxyglutamic acid responds to changes in dietary vitamin K intake. Several days are required before any change can be observed. In a study by Booth et al., increases of phylloquinone intakes from 100 μg to between 377 and 417 μg for five days did not induce a significant change. Response may be age-specific.
- Undercarboxylated osteocalcin (UcOc) levels have been inversely correlated with stores of vitamin K and bone strength in developing rat tibiae. Another study following 78 post-menopausal Korean women found a supplement regimen of vitamins K and D, and calcium, but not a regimen of vitamin D and calcium, was inversely correlated with reduced UcOc levels.
Function in bacteria
Many bacteria, such as Escherichia coli found in the large intestine, can synthesize vitamin K2 (menaquinone-7 or MK-7, up to MK-11), but not vitamin K1 (phylloquinone). In these bacteria, menaquinone transfers two electrons between two different small molecules, during oxygen-independent metabolic energy production processes (anaerobic respiration). For example, a small molecule with an excess of electrons (also called an electron donor) such as lactate, formate, or NADH,
with the help of an enzyme, passes two electrons to menaquinone. The
menaquinone, with the help of another enzyme, then transfers these two
electrons to a suitable oxidant, such fumarate or nitrate (also called an electron acceptor). Adding two electrons to fumarate or nitrate converts the molecule to succinate or nitrite plus water, respectively.
Some of these reactions generate a cellular energy source, ATP, in a manner similar to eukaryotic cell aerobic respiration, except the final electron acceptor is not molecular oxygen, but fumarate or nitrate. In aerobic respiration, the final oxidant is molecular oxygen (O2), which accepts four electrons from an electron donor such as NADH to be converted to water. E. coli, as facultative anaerobes, can carry out both aerobic respiration and menaquinone-mediated anaerobic respiration.
History
In 1929, Danish scientist Henrik Dam investigated the role of cholesterol by feeding chickens a cholesterol-depleted diet. He initially replicated experiments reported by scientists at the Ontario Agricultural College (OAC). McFarlane, Graham and Richardson, working on the chick feed program at OAC, had used chloroform
to remove all fat from chick chow. They noticed that chicks fed only
fat-depleted chow developed hemorrhages and started bleeding from tag
sites.
Dam found that these defects could not be restored by adding purified
cholesterol to the diet. It appeared that – together with the
cholesterol – a second compound had been extracted from the food, and
this compound was called the coagulation vitamin. The new vitamin
received the letter K because the initial discoveries were reported in a
German journal, in which it was designated as Koagulationsvitamin. Edward Adelbert Doisy of Saint Louis University did much of the research that led to the discovery of the structure and chemical nature of vitamin K. Dam and Doisy shared the 1943 Nobel Prize for medicine for their work on vitamin K (K1 and K2) published in 1939. Several laboratories synthesized the compound(s) in 1939.
For several decades, the vitamin K-deficient chick model was the
only method of quantifying vitamin K in various foods: the chicks were
made vitamin K-deficient and subsequently fed with known amounts of
vitamin K-containing food. The extent to which blood coagulation was
restored by the diet was taken as a measure for its vitamin K content.
Three groups of physicians independently found this: Biochemical
Institute, University of Copenhagen (Dam and Johannes Glavind), University of Iowa Department of Pathology (Emory Warner, Kenneth Brinkhous, and Harry Pratt Smith), and the Mayo Clinic (Hugh Butt, Albert Snell, and Arnold Osterberg).
The first published report of successful treatment with vitamin K
of life-threatening hemorrhage in a jaundiced patient with prothrombin
deficiency was made in 1938 by Smith, Warner, and Brinkhous.
The precise function of vitamin K was not discovered until 1974, when three laboratories (Stenflo et al., Nelsestuen et al., and Magnusson et. al.) isolated the vitamin K-dependent coagulation factor prothrombin (factor II) from cows that received a high dose of a vitamin K antagonist, warfarin. It was shown that, while warfarin-treated cows had a form of prothrombin that contained 10 glutamate (Glu) amino acid
residues near the amino terminus of this protein, the normal
(untreated) cows contained 10 unusual residues that were chemically
identified as γ-carboxyglutamate (Gla). The extra carboxyl group in Gla
made clear that vitamin K plays a role in a carboxylation reaction
during which Glu is converted into Gla.