Diseases of poverty (also known as poverty related diseases)
is the term used to describe diseases that are more prevalent in the
low-income population. It includes infectious diseases as well as
diseases related to malnutrition and poor health behaviors. Poverty is
one of the social determinants of health. The World Health Report, 2002
states that diseases of poverty account for 45% of the disease burden in
the countries with high poverty rate which are preventable or treatable
with exciting interventions. Diseases of poverty are often co-morbid and ubiquitous with malnutrition.
Poverty and diseases are a ramification of each other. Poverty
increases chances of having these diseases as the deprivation of safe
shelter, drinking water and food, poor sanitation, lack of knowledge and
access to health services contributes towards poor health behaviors
which often results into diseases of poverty. At the same time, these
diseases act as a barrier for economic growth to affected people and
families caring for them which in turn results into increased poverty in
the community.
These diseases triggered in part by poverty are in contrast to so-called "diseases of affluence", which are diseases thought to be a result of increasing wealth in a society.
Contributing factors
For many environmental and social factors, including poor housing conditions and poor working conditions, inadequate sanitation, and disproportionate occupation as sex workers, the poor are more likely to be exposed to infectious diseases.
Malnutrition, mental stress, overwork, inadequate knowledge, and
minimal health care can hinder recovery and exacerbate the disease. Malnutrition
is associated with 54% of childhood deaths from diseases of poverty,
and lack of skilled attendants during childbirth is primarily
responsible for the high maternal and infant death rates among the poor.
Contaminated water
Each year many children and adults die as a result of a lack of access to clean drinking water
and poor sanitation. Many poverty related diseases such as diarrhea
acquire and spread as a result of inadequate access to clean drinking
water. According to UNICEF, 3,000 children die every day, worldwide due
to contaminated drinking water and poor sanitation.
Although the Millennium Development Goal (MDG) of halving the
number of people who did not have access to clean water by 2015, was
reached five years ahead of schedule in 2010, there are still 783
million people who rely on unimproved water sources.
In 2010 the United Nations declared access to clean water a fundamental
human right, integral to the achievement of other rights. This made it
enforceable and justifiable to permit governments to ensure their
populations access to clean water.
Though access to water has improved for some, it continues to be
especially difficult for women and children. Women and girls bear most
of the burden for accessing water and supplying it to their households.
In India, Sub-Saharan Africa,
and parts of Latin America, women are required to travel long distances
in order to access a clean water source and then bring some water home.
This has a significant impact on girls’ educational attainment.
There have been further efforts to improve water quality using
new technology which allows water to be disinfected immediately upon
collection and during the storage process. Clean water is necessary for
cooking, cleaning, and laundry because many people come into contact
with disease causing pathogens through their food, or while bathing or
washing.
An ongoing issue of contaminated water in the United States has been taking place in Flint, Michigan.
On September 4, 2018, evidence of E Coli and other organisms that can
cause disease were found in the water. The issue of contaminated water
in Flint, Michigan started when the source for drinking water in Flint
was changed from the Lake Huron and the Detroit River to the very cheap
Flint River.
Inadequate sanitation
Contaminated water and inadequate sanitation are related to diseases of poverty such as malaria, parasitic diseases, and schistosomiasis. These infections act as cofactors that increase the risk of HIV transmission.
Standpipes and sanitation are provided in most developing areas,
but the death rates are not significantly reduced. One of the reasons
that water-related diseases are still occurring is because water
supplies can be contacted by contaminated surface water. To effectively
decrease the morbidity and mortality of diseases, the population should
get access to water from home instead from outside. Therefore, in
addition to the installation of standpipes, water supplies and
sanitation should be provided within houses.
Poor nutrition
Malnutrition
disproportionately affect those in sub-Saharan Africa. Over 35 percent
of children under the age of 5 in sub-Saharan Africa show physical signs
of malnutrition.
Malnutrition, the immune system, and infectious diseases operate in a
cyclical manner: infectious diseases have deleterious effects on
nutritional status, and nutritional deficiencies can lower the strength
of the immune system which affects the body’s ability to resist
infections. Similarly, malnutrition of both macronutrients (such as protein and energy) and micronutrients (such as iron, zinc, and vitamins)
increase susceptibility to HIV infections by interfering with the
immune system and through other biological mechanisms. Depletion of
macro-nutrients and micro-nutrients promotes viral replication that contributes to greater risks of HIV transmission from mother-to-child as well as those through sexual transmission. Increased mother-to-child transmission is related to specific deficiencies in micro-nutrients such as vitamin A. Further, anemia, a decrease in the number of red blood cells, increases viral shedding in the birth canal, which also increases risk of mother-to-child transmission. Without these vital nutrients, the body lacks the defense mechanisms to resist infections.
At the same time, HIV lowers the body’s ability to intake essential
nutrients. HIV infection can affect the production of hormones that
interfere with the metabolism of carbohydrates, proteins, and fats.
In the United States, 11.1 percent of households struggle with food insecurity. Food insecurity refers to the lack of access to quality food for a healthy lifestyle.
The rate of hunger and malnutrition in female headed households was
three times the national average at 30.2 percent. According to the Food
and Agriculture Organization of the United Nations, 10 percent of the
population in Latin America and the Caribbean are affected by hunger and
malnutrition.
Poor housing conditions
Quality
and affordability of housing are one of the major concerns in public
health. Poor housing conditions can be described as leaks, molds, indoor
air pollutant, overcrowding, hazardous structures, affordability of
home heating, and poor ergonomics. Housing insecurities are very common
among the poor. It is often associated with infectious diseases, lead
exposure, injuries, and mental health.
Lack of access to health services
According
to WHO, medical strategies report, approximately 30% of the global
population does not have regular access to exciting medicines. In the
poorest parts of Africa and Asia, this percent goes up to 50%.
The population below the poverty line lacks access due to higher retail
price and unavailability of the medicines. The higher cost can be due
to the higher manufacturing price or due to local or regional tax and
Value Added Tax. There is a significant disparity in the research
conducted in the health sector. It is claimed that only 10% of the
health research conducted globally focuses on 90% disease burden.
However, diseases such as cancer, cardiovascular diseases etc that
traditionally were associated with the wealthier community are now
becoming more prevalent in the poor communities as well. Hence, the
research conducted now is relevant to poor population.
Political priority is also one of the contributing factors of
inaccessibility. The government of poor countries may allocate less
funding to public health due to the scarcity of resources.
Diseases
Together, diseases of poverty kill approximately 14 million people annually. Gastroenteritis with its associated diarrhea results in about 1.8 million deaths in children yearly with most of these in the world's poorest nations.
At the global level, the three primary PRDs are tuberculosis, AIDS/HIV and malaria. Developing countries account for 95% of the global AIDS prevalence and 98% of active tuberculosis infections. Furthermore, 90% of malaria deaths occur in sub-Saharan Africa. Together, these three diseases account for 10% of global mortality.
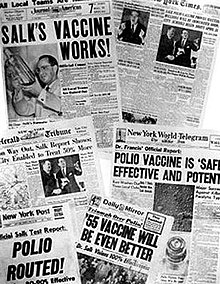
Treatable childhood diseases are another set which have
disproportionately higher rates in poor countries despite the
availability of cures for decades. These include measles, pertussis and polio. The largest three poverty-related diseases (PRDs) — AIDS, malaria, and tuberculosis — account for 18% of diseases in poor countries. The disease burden of treatable childhood diseases in high-mortality, poor countries is 5.2% in terms of disability-adjusted life years but just 0.2% in the case of advanced countries.
In addition, infant mortality and maternal mortality are far more prevalent among the poor. For example, 98% of the 11,600 daily maternal and neonatal deaths occur in developing countries.
Three other diseases, measles, pneumonia, and diarrheal diseases,
are also closely associated with poverty, and are often included with
AIDS, malaria, and tuberculosis in broader definitions and discussions
of diseases of poverty.
Neglected diseases
Based upon the spread of research in cures for diseases, certain diseases are identified and referred to as "neglected diseases". These include the following diseases:
- African trypanosomiasis
- Chagas disease
- Leishmaniasis
- Lymphatic filariasis
- Dracunculiasis (“Guinea worm disease”)
- Onchocerciasis
- Schistosomiasis
- Trichomoniasis
Tropical diseases such as these tend to be neglected in research and
development efforts. Of 1393 new drugs brought into use over a period of
25 years (1975–1999), only a total of thirteen, less than 1%, related
to these diseases. Of 20 MNC drug companies surveyed for research on
PRDs, only two had projects targeted towards these neglected PRDs.
However, the combined total number of deaths due to these diseases is
dwarfed by the enormous number of patients affected by PRDs such as
respiratory infections, HIV/AIDS, diarrhea and tuberculosis, besides
many others.
Similar to the spread of tropical neglected diseases in developing
nations, these neglected infections disproportionately affect poor and
minority populations in the United States. These diseases have been identified by the Centers for Disease Control and Prevention, as priorities for public health action based on the number of people infected, the severity of the illnesses, and the ability to prevent and treat them.
Trichomoniasis
Trichomoniasis
is the most common sexually transmitted infection affecting more than
200 million people worldwide. It is especially prevalent among young,
poor and African American women. This infection is also common in poor
communities in Sub-Saharan Africa and impoverished parts of Asia. This
neglected infection is one of special concern because it is associated
with a heightened risk for contracting HIV and pre-term deliveries.
In addition, availability of cures and recent advances in
medicine have led to only three diseases being considered neglected
diseases, namely, African trypanosomiasis, Chagas disease and
Leishmaniasis.
Malaria
Africa accounts for a majority of malaria
infections and deaths worldwide. Over 80 percent of the 300 to 500
million malaria infections occurring annually worldwide are in Africa. Each year, about one million children under the age of five die from malaria.
Children who are poor, have mothers with little to no education, and
live in rural areas are more susceptible to malaria and more likely to
die from it. Malaria is directly related to the spread of HIV in sub-Saharan Africa.
It increases viral load seven to ten times, which increases the chances
of transmission of HIV through sexual intercourse from a patient with
malaria to an uninfected partner. After the first pregnancy,
HIV can also decrease the immunity to malaria. This contributes to the
increase of the vulnerability to HIV and higher mortality from HIV,
especially for women and infants.
HIV and malaria interact in a cyclical manner—being infected with
malaria increases susceptibility to HIV infection, and HIV infections
increase malarial episodes. The co-existence of HIV and malaria
infections helps spread both diseases, particularly in Sub-Saharan
Africa. Malaria vaccines are an area of intensive research.
Intestinal parasites
Intestinal parasites are extremely prevalent in tropical areas. These include hookworms, roundworms, and other amoebas. They can aggravate malnutrition by depleting essential nutrients through intestinal blood loss and chronic diarrhea. Chronic worm infections can further burden the immune system.
At the same time, chronic worm infections can cause immune activation
that increases susceptibility of HIV infection and vulnerability to HIV
replication once infected.
Schistosomiasis
Schistosomiasis (bilharzia) is a parasitic disease caused by the parasitic flatworm trematodes. Moreover, more than 80 percent of the 200 million people worldwide who have schistosomiasis live in sub-Saharan Africa.
Infections often occur in contaminated water where freshwater snails
release larval forms of the parasite. After penetrating the skin and
eventually traveling to the intestines or the urinary tract, the
parasite lays eggs and infects those organs. It damages the intestines, bladder, and other organs and can lead to anemia and protein-energy deficiency.
Along with malaria, schistosomiasis is one of the most important
parasitic co-factors aiding in HIV transmission. Epidemiological data
shows schistosome-endemic areas coincide with areas of high HIV
prevalence, suggesting that parasitic infections such as schistosomiasis
increase risk of HIV transmission.
Tuberculosis
Tuberculosis is the leading cause of death around the world for an infectious disease.
This disease is especially prevalent in sub-Saharan Africa, and the
Latin American and Caribbean region. While the tuberculosis rate is
decreasing in the rest of the world, it is increasing by rate of 6
percent per year in Sub-Saharan Africa. It is the leading cause of
death for people with HIV in Africa. Tuberculosis (TB) is closely
related to lifestyles of poverty, overcrowded conditions, alcoholism,
stress, drug addiction and malnutrition. This disease spreads quickly
among people who are undernourished.
According to the Center for Disease Control and Prevention, in the
United States, tuberculosis is more prevalent among foreign born
persons, and ethnic minorities. The rates are especially high among
Hispanics, Blacks and Asians.
HIV infection and TB are also closely tied. Being infected with HIV
increases the rate of activation of latent TB infections, and having TB,
increases the rate of HIV replication, therefore accelerating the
progression of AIDS.
AIDS
AIDS is a disease of the human immune system caused by the human immunodeficiency virus (HIV). Primary modes of HIV transmission in sub-Saharan Africa are sexual intercourse, mother-to-child transmission (vertical transmission), and through HIV-infected blood.
Since rate of HIV transmission via heterosexual intercourse is so low,
it is insufficient to cause AIDS disparities between countries. Critics of AIDS policies promoting safe sexual behaviors believe that these policies miss the biological mechanisms and social risk factors that contribute to the high HIV rates in poorer countries.
In these developing countries, especially those in sub-Saharan Africa,
certain health factors predispose the population to HIV infections.
Many of the countries in Sub-Saharan Africa are ravaged with
poverty and many people live on less than one United States dollar a
day.
The poverty in these countries gives rise to many other factors that
explain the high prevalence of AIDS. The poorest people in most African
countries suffer from malnutrition, lack of access to clean water, and
have improper sanitation. Because of a lack of clean water many people
are plagued by intestinal parasites that significantly increase their
chances of contracting HIV due to compromised immune system. Malaria, a
disease still rampant in Africa also increases the risk of contracting
HIV. These parasitic diseases, affect the body’s immune response to
HIV, making people more susceptible to contracting the disease once
exposed. Genital schistosomiasis, also prevalent in the topical areas
of Sub-Saharan Africa and many countries worldwide, produces genital
lesions and attract CD4 cells to the genital region which promotes HIV
infection. All these factors contribute to the high rate of HIV in
Sub-Saharan Africa. Many of the factors seen in Africa are also present
in Latin America and the Caribbean and contribute to the high rates of
infections seen in those regions. In the United States, poverty is a
contributing factor to HIV infections. There is also a large racial disparity, with African Americans having a significantly higher rate of infection than their white counterparts.
Asthma
More than 300 million people worldwide have asthma.
The rate of asthma increases as countries become more urbanized and in
many parts of the world those who develop asthma do not have access to
medication and medical care.
Within the United States, African Americans and Latinos are four times
more likely to suffer from severe asthma than whites. The disease is
closely tied to poverty and poor living conditions.
Asthma is also prevalent in children in low income countries. Homes
with roaches and mice, as well as mold and mildew put children at risk
for developing asthma as well as exposure to cigarette smoke.
Unlike many other Western countries, the mortality rate for
asthma has steadily risen in the United States over the last two
decades. Mortality rates for African American children due to asthma are also far higher than that of other racial groups.
For African Americans, the rate of visits to the emergency room is 330
percent higher than their white counterparts. The hospitalization rate
is 220 percent higher and the death rate is 190 percent higher.
Among Hispanics, Puerto Ricans are disproportionately affected by asthma
with a disease rate that is 113 percent higher than non-Hispanic Whites
and 50 percent higher than non-Hispanic Blacks.
Studies have shown that asthma morbidity and mortality are concentrated
in inner city neighborhoods characterized by poverty and large minority
populations and this affects both genders at all ages.
Asthma continues to have an adverse effects on the health of the poor
and school attendance rates among poor children. 10.5 million days of
school are missed each year due to asthma.
Cardiovascular disease
Though heart disease
is not exclusive to the poor, there are aspects of a life of poverty
that contribute to its development. This category includes coronary heart disease, stroke and heart attack.
Heart disease is the leading cause of death worldwide and there are
disparities of morbidity between the rich and poor. Studies from around
the world link heart disease to poverty. Low neighborhood income and
education were associated with higher risk factors. Poor diet, lack of
exercise and limited (or no) access to a specialist were all factors
related to poverty, though to contribute to heart disease.
Both low income and low education were predictors of coronary heart
disease, a subset of cardiovascular disease. Of those admitted to
hospital in the United States for heart failure, women and African
Americans were more likely to reside in lower income neighborhoods. In
the developing world, there is a 10 fold increase in cardiac events in
the black and urban populations.
Obstetrical fistula
Obstetric fistula or vaginal fistula is a medical condition in which a fistula (hole) develops between either the rectum and vagina or between the bladder and vagina after severe or failed childbirth, when adequate medical care is not available.
It is considered a disease of poverty because of its tendency to occur
women in poor countries who do not have health resources comparable to
developed nations.
Dental decay
Dental decay or dental caries is the gradual destruction of tooth enamel. Poverty is a significant determinant for oral health.
Dental caries is one of the most common chronic diseases worldwide. In
the United States it is the most common chronic disease of childhood.
Risk factors for dental caries includes living in poverty, poor
education, low socioeconomic status, being part of an ethnic minority
group, having a developmental disability, recent immigrants and people
infected with HIV/AIDS. In Peru, poverty was found to be positively correlated with dental caries among children.
According to a report by U.S health surveillance, tooth decay peaks
earlier in life and is more severe in children with families living
below the poverty line.
Tooth decay is also strongly linked to dietary behaviors, and in poor
rural areas where nutrient dense foods, fruits and vegetables are
unavailable, the consumption of sugary and fatty food increases the
risk of dental decay.
Because the mouth is a gateway to the respiratory and digestive
tracts, oral health has a significant impact on other health outcomes.
Gum disease has been linked to diseases such as cardiovascular disease.
Consequences
Diseases
of poverty reflect the dynamic relationship between poverty and poor
health; while such diseases result directly from poverty, they also
perpetuate and deepen impoverishment by sapping personal and national
health and financial resources. For example, malaria decreases GDP
growth by up to 1.3% in some developing nations, and by killing tens of
millions in sub-Saharan Africa, AIDS alone threatens “the economies,
social structures, and political stability of entire societies”.
For women
Women
and children are often put at a high risk of being infected by
schistosomiasis, which in turn puts them at a higher risk of acquiring
HIV.
Since the mode of schistosomiasis transmission is usually through
contaminated water in streams and lakes, women and children who do their
household chores by the water are more likely to acquire the disease.
Activities that women and children often do around waterfront include
washing clothes, collecting water, bathing, and swimming. Women who have schistosomiasis lesions are three times more likely to be infected with HIV.
Women also have a higher risk of HIV transmission through the use of medical equipment such as needles.
Because more women than men use health services, especially during
pregnancy, they are more likely to come across unsterilized needles for
injections.
Although statistics estimate that unsterilized needles only account for
5 to 10 percent of primary HIV infections, studies show this mode of
HIV transmission may be higher than reported.
This increased risk of contracting HIV through non-sexual means has
social consequences for women as well. Over half of the husbands of
HIV-positive women in Africa tested HIV-negative. When HIV-positive women reveal their HIV status to their HIV-negative husbands, they are often accused of infidelity and face violence and abandonment from their family and community.
Relating to human capabilities
Malnutrition associated with HIV impacts people’s ability to provide for themselves and their dependents, thus limiting the human capabilities of both themselves and their dependents. HIV can negatively affect work output, which impacts the ability to generate income. This is crucial in parts of Africa where farming is the primary occupation and obtaining food is dependent on the agricultural outcome. Without adequate food production,
malnutrition becomes more prevalent. Children are often collateral
damage in the AIDS crisis. As dependents, they can be burdened by the
illness and eventual death of one or both parents due to HIV/AIDS.
Studies have shown that orphaned children are more likely to display
physical symptoms of malnutrition than children whose parents are both
alive.
Public policy proposals
There
are a number of proposals for reducing the diseases of poverty and
eliminating health disparities within and between countries. The World
Health Organization proposes closing the gaps by acting on social
determinants.
Their first recommendation is to improve daily living conditions. This
area involves improving the lives of women and girls so that their
children are born in healthy environments and placing an emphasis on
early childhood health.
Their second recommendation is to tackle the inequitable distribution of
money, power and resources. This would involve building stronger
public sectors and changing the way in which society is organized.
Their third recommendation is to measure and understand the problem and
assess the impact of action. This would involve training policy makers
and healthcare practitioners to recognize problems and form policy
solutions.
Health in All Policies
The 8th Global Conference on Health Promotion held in Helsinki in June 2013 has proposed an approach termed Health in All Policies. Health
inequalities are shaped by many powerful forces and social, political,
and economic determinants. Governments have a responsibility to ensure
that their people are able to live healthy lives and have equitable
access to achieving a reasonable state of good health. Policies that
governments craft and implement in all sectors have a significant and
ongoing impact on public health, health equity, and the lives of their
citizens. Increases in technology, medical innovation, and living
conditions have led to the disappearance of diseases and other factors
contributing to poor health. However, there are many diseases of poverty
that still persist in developed and developing countries. Tackling
these health inequalities and diseases of poverty requires a willingness
to engage the whole government in health. The Helskinki Statement lays
out a framework of action for countries and calls on governments to make
a commitment to building health equity within their country.
Health in All Policies (HiAP) is an approach to public policies
across all sectors of government that takes into account the health
implications of all government and policy decisions to improve health
equity across all populations residing within the borders of a country.
This concept is built upon principles in line with the Universal
Declaration of Human Rights, The United Nations Millennium Development
Declaration, and principles of good governance:
legitimacy given by national and international law, accountability of
government, transparency of policy making, participation of citizens,
sustainability ensuring policies meet the needs of both present and
future generations, and collaboration across sectors and levels of
government.
Finally the Framework lists and expands upon six steps for implementation that may be undertaken by a country in taking action towards Health in
All Policies. These are components of action and not a rigid checklist
of steps to adhere to. The most important aspect of this policy is that
governments should adapt the policy to suit the needs of their citizens,
their socioeconomic situation, and their governance system.
- Establish the need and priorities for HiAP
- Frame planned action
- Identify supportive structures and processes
- Facilitate assessment and engagement
- Ensure monitoring, evaluation, and reporting
- Build capacity.
HIV/AIDS policy
- Nutrition Supplements: Focusing on reversing the pattern of malnutrition in sub-Saharan African and other poor countries is a one possible way of decreasing susceptibility to HIV infections. Micro-nutrients such as iron and vitamin A can be delivered and provided at a very low cost. For example, vitamin A supplements cost $0.02 per capsule if provided twice a year. Iron supplements per child cost $0.02 if provided weekly or $0.08 if provided daily.
- Eliminating Co-factors: Tackling the very diseases that increase risk of HIV infections can help slow down the rates of HIV transmission. Co-factors such as malaria and parasitic infections can be combated in an effective and cost-efficient manner. For example, mosquito nets can be easily used to prevent malaria. Parasites can be eliminated with medication that is cost-effective and easy to administer. Twice-yearly treatments range from $0.02 to $0.25 depending on the type of worm.