From Wikipedia, the free encyclopedia
| Coronary artery disease |
|---|
| Synonyms | Atherosclerotic heart disease, atherosclerotic vascular disease, coronary heart disease |
|---|
 |
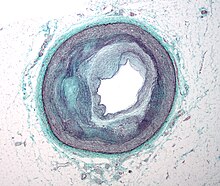
| Illustration depicting atherosclerosis in a coronary artery. |
| Specialty | Cardiology, cardiac surgery |
|---|
| Symptoms | Chest pain, shortness of breath |
|---|
| Complications | Heart failure, abnormal heart rhythms |
|---|
| Causes | Atherosclerosis of the arteries of the heart |
|---|
| Risk factors | High blood pressure, smoking, diabetes, lack of exercise, obesity, high blood cholesterol |
|---|
| Diagnostic method | Electrocardiogram, cardiac stress test, coronary computed tomographic angiography, coronary angiogram |
|---|
| Prevention | Healthy diet, regular exercise, maintaining a healthy weight, not smoking |
|---|
| Treatment | Percutaneous coronary intervention (PCI), coronary artery bypass surgery (CABG) |
|---|
| Medication | Aspirin, beta blockers, nitroglycerin, statins |
|---|
| Frequency | 110 million (2015) |
|---|
| Deaths | 8.9 million (2015) |
|---|
Coronary artery disease (
CAD), also known as
ischemic heart disease (
IHD), involves the reduction of blood flow to the
heart muscle due to
build up of plaque in the
arteries of the heart. It is the most common of the
cardiovascular diseases. Types include
stable angina,
unstable angina,
myocardial infarction, and
sudden cardiac death. A common symptom is
chest pain or discomfort which may travel into the shoulder, arm, back, neck, or jaw. Occasionally it may feel like
heartburn. Usually symptoms occur with exercise or emotional
stress, last less than a few minutes, and improve with rest.
Shortness of breath may also occur and sometimes no symptoms are present. In many cases, the first sign is a
heart attack. Other complications include
heart failure or an
abnormal heartbeat.
Risk factors include
high blood pressure,
smoking,
diabetes, lack of exercise,
obesity,
high blood cholesterol, poor diet,
depression, and excessive
alcohol. A number of tests may help with diagnoses including:
electrocardiogram,
cardiac stress testing,
coronary computed tomographic angiography, and
coronary angiogram, among others.
Ways to reduce CAD risk include eating a healthy diet, regularly exercising, maintaining a healthy weight, and not smoking. Medications for diabetes, high cholesterol, or high blood pressure are sometimes used. There is limited evidence for screening people who are at low risk and do not have symptoms. Treatment involves the same measures as prevention. Additional medications such as
antiplatelets (including
aspirin),
beta blockers, or
nitroglycerin may be recommended. Procedures such as
percutaneous coronary intervention (PCI) or
coronary artery bypass surgery (CABG) may be used in severe disease. In those with stable CAD it is unclear if PCI or CABG in addition to the other treatments improves
life expectancy or decreases heart attack risk.
In 2015, CAD affected 110 million people and resulted in 8.9 million deaths. It makes up 15.6% of all deaths, making it the
most common cause of death globally. The risk of death from CAD for a given age decreased between 1980 and 2010, especially in
developed countries. The number of cases of CAD for a given age also decreased between 1990 and 2010.
In the United States in 2010, about 20% of those over 65 had CAD, while
it was present in 7% of those 45 to 64, and 1.3% of those 18 to 45; rates were higher among men than women of a given age.
Signs and symptoms
Angina that changes in intensity, character or frequency is termed unstable.
Unstable angina may precede
myocardial infarction.
In adults who go to the emergency department with an unclear cause of
pain, about 30% have pain due to coronary artery disease.
Risk factors
Coronary artery disease has a number of well determined risk factors. These include
high blood pressure,
smoking,
diabetes, lack of exercise,
obesity,
high blood cholesterol, poor diet,
depression,
family history, and excessive
alcohol. About half of cases are linked to genetics. Smoking and obesity are associated with about 36% and 20% of cases, respectively. Smoking just one cigarette per day about doubles the risk of CAD. Lack of exercise has been linked to 7–12% of cases. Exposure to the
herbicide Agent Orange may increase risk. Rheumatologic diseases such as
rheumatoid arthritis,
systemic lupus erythematosus,
psoriasis, and
psoriatic arthritis are independent risk factors as well.
Job stress appears to play a minor role accounting for about 3% of cases.
In one study, women who were free of stress from work life saw an
increase in the diameter of their blood vessels, leading to decreased
progression of atherosclerosis.
In contrast, women who had high levels of work-related stress
experienced a decrease in the diameter of their blood vessels and
significantly increased disease progression. Having a
type A behavior pattern, a group of personality characteristics including time urgency, competitiveness, hostility, and impatience, is linked to an increased risk of coronary disease.
Blood fats
Dietary cholesterol does not appear to have a significant effect on
blood cholesterol and thus recommendations about its consumption may not
be needed. Saturated fat is still a concern.
Genetics
Other
- Endometriosis in women under the age of 40.
- Depression and hostility appear to be risks.
- The number of categories of adverse childhood experiences
(psychological, physical, or sexual abuse; violence against mother; or
living with household members who were substance abusers, mentally ill,
suicidal, or incarcerated) showed a graded correlation with the presence
of adult diseases including coronary artery (ischemic heart) disease.
- Hemostatic factors: High levels of fibrinogen and coagulation factor VII are associated with an increased risk of CAD.
- Low hemoglobin.
- In the Asian population, the b fibrinogen gene G-455A polymorphism was associated with the risk of CAD.
Pathophysiology
Illustration depicting coronary artery disease
Limitation of blood flow to the heart causes
ischemia (cell starvation secondary to a lack of oxygen) of the heart's
muscle cells. The heart's muscle cells may die from lack of
oxygen and this is called a
myocardial infarction
(commonly referred to as a heart attack). It leads to damage, death,
and eventual scarring of the heart muscle without regrowth of heart
muscle cells. Chronic high-grade
narrowing of the coronary arteries can induce transient
ischemia which leads to the induction of a
ventricular arrhythmia, which may terminate into a dangerous heart rhythm known as
ventricular fibrillation, which often leads to death.
Typically, coronary artery disease occurs when part of the smooth, elastic lining inside a
coronary artery (the arteries that supply blood to the heart muscle) develops
atherosclerosis.
With atherosclerosis, the artery's lining becomes hardened, stiffened,
and accumulates deposits of calcium, fatty lipids, and abnormal
inflammatory
cells – to form a
plaque.
Calcium phosphate (hydroxyapatite) deposits in the muscular layer of
the blood vessels appear to play a significant role in stiffening the
arteries and inducing the early phase of coronary
arteriosclerosis. This can be seen in a so-called metastatic mechanism of
calciphylaxis as it occurs in
chronic kidney disease and
hemodialysis
(Rainer Liedtke 2008). Although these people suffer from a kidney
dysfunction, almost fifty percent of them die due to coronary artery
disease. Plaques can be thought of as large "pimples" that protrude into
the channel of an artery, causing a partial obstruction to blood flow.
People with coronary artery disease might have just one or two
plaques, or might have dozens distributed throughout their
coronary arteries.
A more severe form is
chronic total occlusion (CTO) when a coronary artery is completely obstructed for more than 3 months.
Cardiac syndrome X is chest pain (
angina pectoris) and chest discomfort in people who do not show signs of blockages in the larger
coronary arteries of their hearts when an
angiogram (coronary angiogram) is being performed. The exact cause of cardiac syndrome X is unknown. Explanations include
microvascular dysfunction or
epicardial atherosclerosis. For reasons that are not well understood, women are more likely than men to have it; however,
hormones and other risk factors unique to women may play a role.
Diagnosis
Coronary angiogram of a man
Coronary angiogram of a woman
For symptomatic people,
stress echocardiography can be used to make a diagnosis for obstructive coronary artery disease. The use of
echocardiography,
stress cardiac imaging, and/or advanced non-invasive imaging is not
recommended on individuals who are exhibiting no symptoms and are
otherwise at low risk for developing coronary disease.
The diagnosis of "Cardiac Syndrome X" – the rare coronary artery
disease that is more common in women, as mentioned, is a diagnosis of
exclusion. Therefore, usually the same tests are used as in any person
with the suspected of having coronary artery disease:
The diagnosis of coronary disease underlying particular symptoms
depends largely on the nature of the symptoms. The first investigation
is an
electrocardiogram (ECG/EKG), both for "stable" angina and acute coronary syndrome. An
X-ray of the chest and
blood tests may be performed.
Stable angina
Stable coronary artery disease (SCAD) is also often called stable ischemic heart disease (SIHD). A 2015 monograph explains that "Regardless of the nomenclature, stable angina is the chief manifestation of SIHD or SCAD." There are U.S. and European
clinical practice guidelines for SIHD/SCAD.
Acute coronary syndrome
Diagnosis of
acute coronary syndrome generally takes place in the
emergency department,
where ECGs may be performed sequentially to identify "evolving changes"
(indicating ongoing damage to the heart muscle). Diagnosis is clear-cut
if ECGs show elevation of the "
ST segment", which in the context of severe typical chest pain is strongly indicative of an acute
myocardial infarction (MI); this is termed a STEMI (ST-elevation MI) and is treated as an emergency with either urgent
coronary angiography and
percutaneous coronary intervention (angioplasty with or without
stent insertion) or with
thrombolysis ("clot buster" medication), whichever is available. In the absence of ST-segment elevation, heart damage is detected by
cardiac markers (blood tests that identify heart muscle damage). If there is evidence of damage (
infarction),
the chest pain is attributed to a "non-ST elevation MI" (NSTEMI). If
there is no evidence of damage, the term "unstable angina" is used. This
process usually necessitates hospital admission and close observation
on a
coronary care unit for possible complications (such as
cardiac arrhythmias
– irregularities in the heart rate). Depending on the risk assessment,
stress testing or angiography may be used to identify and treat coronary
artery disease in patients who have had an NSTEMI or unstable angina.
Risk assessment
There are various risk assessment systems for determining the risk of
coronary artery disease, with various emphasis on different variables
above. A notable example is
Framingham Score, used in the
Framingham Heart Study. It is mainly based on age, gender, diabetes, total cholesterol, HDL cholesterol, tobacco smoking and systolic blood pressure.
Prevention
Up to 90% of cardiovascular disease may be preventable if established risk factors are avoided. Prevention involves adequate physical
exercise, decreasing
obesity, treating
high blood pressure, eating a
healthy diet, decreasing
cholesterol levels, and
stopping smoking. Medications and exercise are roughly equally effective. High levels of physical activity reduce the risk of coronary artery disease by about 25%.
Most guidelines recommend combining these preventive strategies. A
2015 Cochrane Review found some evidence that counseling and education
in an effort to bring about behavioral change might help in high risk
groups. However, there was insufficient evidence to show an effect on
mortality or actual cardiovascular events.
Diet
A diet high in fruits and vegetables decreases the risk of cardiovascular disease and death.
Vegetarians have a lower risk of heart disease, possibly due to their greater consumption of fruits and vegetables. Evidence also suggests that the
Mediterranean diet and a
high fiber diet lower the risk.
Secondary prevention
Secondary prevention is preventing further sequelae of already established disease. Effective lifestyle changes include:
Aerobic exercise, like walking, jogging, or swimming, can reduce the risk of mortality from coronary artery disease.
Aerobic exercise can help decrease blood pressure and the amount of
blood cholesterol (LDL) over time. It also increases HDL cholesterol
which is considered "good cholesterol".
Although exercise is beneficial, it is unclear whether doctors should spend time counseling patients to exercise. The
U.S. Preventive Services Task Force
found "insufficient evidence" to recommend that doctors counsel
patients on exercise but "it did not review the evidence for the
effectiveness of physical activity to reduce chronic disease, morbidity
and mortality", only the effectiveness of counseling itself. The
American Heart Association, based on a non-systematic review, recommends that doctors counsel patients on exercise.
Treatment
There are a number of treatment options for coronary artery disease:
Medications
It is recommended that blood pressure typically be reduced to less than 140/90 mm Hg. The diastolic blood pressure however should not be lower than 60 mm Hg. Beta blockers are recommended first line for this use.
Aspirin
In
those with no previous history of heart disease, aspirin decreases the
risk of a myocardial infarction but does not change the overall risk of
death. It is thus only recommended in adults who are at increased risk for coronary artery disease
where increased risk is defined as "men older than 90 years of age,
postmenopausal women, and younger persons with risk factors for coronary
artery disease (for example, hypertension, diabetes, or smoking) are at
increased risk for heart disease and may wish to consider aspirin
therapy". More specifically, high-risk persons are "those with a 5-year
risk ≥ 3%".
Anti-platelet therapy
Clopidogrel plus aspirin (dual anti-platelet therapy ) reduces cardiovascular events more than aspirin alone in those with a
STEMI. In others at high risk but not having an acute event the evidence is weak. Specifically, its use does not change the risk of death in this group. In those who have had a stent more than 12 months of clopidogrel plus aspirin does not affect the risk of death.
Surgery
Revascularization for
acute coronary syndrome has a mortality benefit. Percutaneous revascularization for
stable ischaemic heart disease does not appear to have benefits over medical therapy alone. In those with disease in more than one artery
coronary artery bypass grafts appear better than
percutaneous coronary interventions.
Newer "anaortic" or no-touch off-pump coronary artery revascularization
techniques have shown reduced postoperative stroke rates comparable to
percutaneous coronary intervention.
Hybrid coronary revascularization has also been shown to be a safe and
feasible procedure that may offer some advantages over conventional CABG
though it is more expensive.
Epidemiology
Deaths due to ischaemic heart disease per million persons in 2012
160–288
289–379
380–460
461–576
577–691
692–894
895–1,068
1,069–1,443
1,444–2,368
2,369–7,233
Disability-adjusted life year for ischaemic heart disease per 100,000 inhabitants in 2004.
no data
less than 350
350–700
700–1,050
1,050–1,400
1,400–1,750
1,750–2,100
2,100–2,450
2,450–2,800
2,800–3,150
3,150–3,500
3,500–4,000
greater than 4,000
As of 2010, CAD was the leading cause of death globally resulting in over 7 million deaths. This increased from 5.2 million deaths from CAD worldwide in 1990.
It may affect individuals at any age but becomes dramatically more
common at progressively older ages, with approximately a tripling with
each decade of life. Males are affected more often than females.
It is estimated that 60% of the world's cardiovascular disease
burden will occur in the South Asian subcontinent despite only
accounting for 20% of the world's population. This may be secondary to a
combination of genetic predisposition and environmental factors.
Organizations such as the
Indian Heart Association are working with the
World Heart Federation to raise awareness about this issue.
Coronary artery disease is the leading cause of death for both
men and women and accounts for approximately 600,000 deaths in the
United States every year.
According to present trends in the United States, half of healthy
40-year-old men will develop CAD in the future, and one in three healthy
40-year-old women. It is the most common reason for death of men and women over 20 years of age in the United States.
Society and culture
Names
Other terms sometimes used for this condition are "hardening of the arteries" and "narrowing of the arteries". In Latin it is known as morbus ischaemicus cordis (MIC).
Support groups
Industry influence on research
Research
Research efforts are focused on new
angiogenic treatment modalities and various (adult)
stem-cell therapies. A region on
chromosome 17 was confined to families with multiple cases of myocardial infarction. Other genome-wide studies have identified a firm risk variant on
chromosome 9. However, these and other
loci are found in intergenic segments and need further research in understanding how the
phenotype is affected.
A more controversial link is that between
Chlamydophila pneumoniae infection and atherosclerosis.
While this intracellular organism has been demonstrated in
atherosclerotic plaques, evidence is inconclusive as to whether it can
be considered a causative factor.
Treatment with antibiotics in patients with proven atherosclerosis has
not demonstrated a decreased risk of heart attacks or other coronary
vascular diseases.
Since the 1990s the search for new treatment options for coronary
artery disease patients, particularly for so called "no-option"
coronary patients, focused on usage of
angiogenesis and (adult)
stem cell therapies. Numerous clinical trials were performed, either applying
protein (angiogenic
growth factor) therapies, such as
FGF-1 or
VEGF, or cell therapies using different kinds of adult
stem cell populations. Research is still going on – with first promising results particularly for
FGF-1 and utilization of endothelial
progenitor cells.
Dietary changes can decrease coronary artery disease. For
example, data supports benefit from a plant-based diet and aggressive
lipid lowering to improve heart disease.