Bariatric surgery (or weight loss surgery) includes a variety of procedures performed on people who have obesity. Weight loss is achieved by reducing the size of the stomach with a gastric band
or through removal of a portion of the stomach (sleeve gastrectomy or
biliopancreatic diversion with duodenal switch) or by resecting and
re-routing the small intestine to a small stomach pouch (gastric bypass surgery).
Long-term studies show the procedures cause significant long-term loss of weight, recovery from diabetes, improvement in cardiovascular risk factors, and a mortality reduction from 40% to 23%. The U.S. National Institutes of Health recommends bariatric surgery for obese people with a body mass index (BMI) of at least 40, and for people with BMI of at least 35 and serious coexisting medical conditions such as diabetes. However, research is emerging that suggests bariatric surgery could be appropriate for those with a BMI of 35 to 40 with no comorbidities or a BMI of 30 to 35 with significant comorbidities. The most recent American Society for Metabolic & Bariatric Surgery guidelines suggest the position statement on consensus for BMI as an indication for bariatric surgery. The recent guidelines suggest that any patient with a BMI of more than 30 with comorbidities is a candidate for bariatric surgery.
A National Institute of Health symposium held in 2013 that summarized available evidence found a 29% mortality reduction, a 10-year remission rate of Type 2 Diabetes of 36%, fewer cardiovascular events, and a lower rate of diabetes-related complications in a long-term, non-randomized, matched intervention 15-20 year follow-up study, the Swedish Obese Subjects Study. The symposium also found similar results from a Utah study using more modern gastric bypass techniques, though the follow-up periods of the Utah studies are only up to 7 years. While randomized controlled trials of bariatric surgery exist, they are limited by short follow-up periods.
Long-term studies show the procedures cause significant long-term loss of weight, recovery from diabetes, improvement in cardiovascular risk factors, and a mortality reduction from 40% to 23%. The U.S. National Institutes of Health recommends bariatric surgery for obese people with a body mass index (BMI) of at least 40, and for people with BMI of at least 35 and serious coexisting medical conditions such as diabetes. However, research is emerging that suggests bariatric surgery could be appropriate for those with a BMI of 35 to 40 with no comorbidities or a BMI of 30 to 35 with significant comorbidities. The most recent American Society for Metabolic & Bariatric Surgery guidelines suggest the position statement on consensus for BMI as an indication for bariatric surgery. The recent guidelines suggest that any patient with a BMI of more than 30 with comorbidities is a candidate for bariatric surgery.
A National Institute of Health symposium held in 2013 that summarized available evidence found a 29% mortality reduction, a 10-year remission rate of Type 2 Diabetes of 36%, fewer cardiovascular events, and a lower rate of diabetes-related complications in a long-term, non-randomized, matched intervention 15-20 year follow-up study, the Swedish Obese Subjects Study. The symposium also found similar results from a Utah study using more modern gastric bypass techniques, though the follow-up periods of the Utah studies are only up to 7 years. While randomized controlled trials of bariatric surgery exist, they are limited by short follow-up periods.
Medical uses
Biliopancreatic Diversion.
A medical guideline by the American College of Physicians concluded:
- "Surgery should be considered as a treatment option for patients with a BMI of 40 kg/m2 or greater who instituted but failed an adequate exercise and diet program (with or without adjunctive drug therapy) and who present with obesity-related comorbid conditions, such as hypertension, impaired glucose tolerance, diabetes mellitus, hyperlipidemia, and obstructive sleep apnea. A doctor–patient discussion of surgical options should include the long-term side effects, such as a possible need for reoperation, gallbladder disease, and malabsorption."
- "Patients should be referred to high-volume centers with surgeons experienced in bariatric surgery."
The surgery is contraindicated in patients who have end stage disease
and also in patients not committed to make lifestyle changes considered
ideal for the surgery.
In 2011, the International Diabetes Federation issued a position statement suggesting "Under some
circumstances, people with a BMI 30–35 should be eligible for surgery."
When determining eligibility for bariatric surgery for extremely obese
patients, psychiatric screening is critical; it is also critical for
determining postoperative success. Patients with a body-mass index of
40 kg/m2 or greater have a 5-fold risk of depression, and half of bariatric surgery candidates are depressed.
Weight loss
In
general, the malabsorptive procedures lead to more weight loss than the
restrictive procedures; however, they have a higher risk profile. A meta-analysis from University of California, Los Angeles, reports the following weight loss at 36 months:
- Biliopancreatic diversion — 117 Lbs / 53 kg
- Roux-en-Y gastric bypass (RYGB) — 90 Lbs / 41 kg
- Open — 95 Lbs/ 43 kg
- Laparoscopic — 84 Lbs / 38 kg
- Vertical banded gastroplasty — 71 Lbs / 32 kg
A 2017 meta-analysis showed bariatric surgery to be effective for
weight loss in adolescents, as assessed 36 months after the
intervention. The same meta-analysis noted that additional data is
needed to determine whether it is also effective for long-term weight
loss in adolescents. According to the Canadian Agency for Drugs and Technologies in Health,
the comparative evidence base for bariatric surgery in adolescents and
young adults is "...limited to a few studies that were narrow in scope
and with relatively small sample sizes."
Another 2017 meta-analysis reported that it was effective at reducing weight among morbidly obese adults in China.
Reduced mortality and morbidity
In
the short term, weight loss from bariatric surgeries is associated with
reductions in some comorbidities of obesity, such as diabetes,
metabolic syndrome and sleep apnea, but the benefit for hypertension is
uncertain. It is uncertain whether any given bariatric procedure is
more effective than another in controlling comorbidities. There is no
high quality evidence concerning longer-term effects compared with
conventional treatment on comorbidities.
Bariatric surgery in older patients has also been a topic of
debate, centered on concerns for safety in this population; the relative
benefits and risks in this population is not known.
Given the remarkable rate of diabetes remission with bariatric
surgery, there is considerable interest in offering this intervention to
people with type 2 diabetes
who have a lower BMI than is generally required for bariatric surgery,
but high quality evidence is lacking and optimal timing of the procedure
is uncertain.
Laparoscopic
bariatric surgery requires a hospital stay of only one or two days.
Short-term complications from laparoscopic adjustable gastric banding
are reported to be lower than laparoscopic Roux-en-Y surgery, and
complications from laparoscopic Roux-en-Y surgery are lower than
conventional (open) Roux-en-Y surgery.
Fertility and pregnancy
The
position of the American Society for Metabolic and Bariatric Surgery
as of 2017 was that it was not clearly understood whether medical
weight-loss treatments or bariatric surgery had an effect responsiveness
to subsequent treatments for infertility in both men and women. Bariatric surgery reduces the risk of gestational diabetes and hypertensive disorders of pregnancy in women who later become pregnant but increases the risk of preterm birth.
Psychiatric/Psychological
Some studies have suggested that psychological health can improve after bariatric surgery.
Adverse effects
Weight
loss surgery in adults is associated with relatively large risks and
complications, compared to other treatments for obesity.
The likelihood of major complications from weight-loss surgery is 4%.
“Sleeve gastrectomy had the lowest complication and reoperation rates
of the three (main weight-loss surgery) procedures.....The percentage of
procedures requiring reoperations due to complications was 15.3 percent
for the gastric band, 7.7 percent for gastric bypass and 1.5 percent
for sleeve gastrectomy” - American Society for Metabolic and Bariatric
Surgery.
As the rate of complications appears to be reduced when the
procedure is performed by an experienced surgeon, guidelines recommend
that surgery be performed in dedicated or experienced units.
It has been observed that the rate of leaks was greater in low volume
centres whereas high volume centres showed a lesser leak rate. Leak
rates have now globally decreased to a mean of 1-5%.
Metabolic bone disease manifesting as osteopenia and secondary hyperparathyroidism
have been reported after Roux-en-Y gastric bypass surgery due to reduced
calcium
absorption. The highest concentration of calcium transporters is in the
duodenum. Since the ingested food will not pass through the duodenum
after a bypass procedure, calcium levels in the blood may decrease,
causing secondary hyperparathyroidism, increase in bone turnover, and a
decrease in bone mass. Increased risk of fracture has also been linked
to bariatric surgery.
Rapid weight loss after obesity surgery can contribute to the
development of gallstones as well by increasing the lithogenicity of
bile. Adverse effects on the kidneys have been studied. Hyperoxaluria
that can potentially lead to oxalate nephropathy and irreversible renal
failure is the most significant abnormality seen on urine chemistry
studies. Rhabdomyolysis leading to acute kidney injury, and impaired renal handling of acid and base has been reported after bypass surgery.
Nutritional derangements due to deficiencies of micronutrients
like iron, vitamin B12, fat soluble vitamins, thiamine, and folate are
especially common after malabsorptive bariatric procedures. Seizures due
to hyperinsulinemic hypoglycemia
have been reported. Inappropriate insulin secretion secondary to islet
cell hyperplasia, called pancreatic nesidioblastosis, might explain this
syndrome.
Self-harm behaviors and suicide appear to be increased in people
with mental health issues in the five years after bariatric surgery had
been done.
Types
Diagram of a biliopancreatic diversion.
Procedures can be grouped in three main categories: blocking, restricting, and mixed.
Standard of care in the United States and most of the industrialized
world in 2009 is for laparoscopic as opposed to open procedures. Future
trends are attempting to achieve similar or better results via
endoscopic procedures.
Blocking procedures
Some procedures block absorption of food, although they also reduce stomach size.
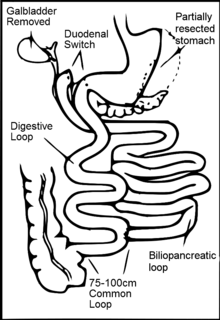
Biliopancreatic diversion
This operation is termed biliopancreatic diversion (BPD) or the Scopinaro procedure.
The original form of this procedure is now rarely performed because of
problems with. It has been replaced with a modification known as duodenal switch (BPD/DS). Part of the stomach is resected, creating a smaller stomach (however the patient can eat a free diet as there is no restrictive component). The distal part of the small intestine is then connected to the pouch, bypassing the duodenum and jejunum.
In around 2% of patients there is severe malabsorption
and nutritional deficiency that requires restoration of the normal
absorption. The malabsorptive effect of BPD is so potent that, as in
most restrictive procedures, those who undergo the procedure must take vitamin and dietary minerals
above and beyond that of the normal population. Without these
supplements, there is risk of serious deficiency diseases such as anemia and osteoporosis.
Because gallstones are a common complication of the rapid weight loss following any type of bariatric surgery, some surgeons remove the gallbladder as a preventive measure during BPD. Others prefer to prescribe medications to reduce the risk of post-operative gallstones.
Diagram of a vertical banded gastroplasty.
Far fewer surgeons perform BPD compared to other weight loss
surgeries, in part because of the need for long-term nutritional
follow-up and monitoring of BPD patients.
Jejunoileal bypass
This procedure is no longer performed. It was a surgical weight-loss procedure performed for the relief of morbid obesity from the 1950s through the 1970s in which all but 30 cm (12 in) to 45 cm (18 in) of the small bowel was detached and set to the side.
Endoluminal sleeve
A study on humans was done in Chile using the same technique
however the results were not conclusive and the device had issues with
migration and slipping. A study recently done in the Netherlands found a
decrease of 5.5 BMI points in 3 months with an endoluminal sleeve
Restrictive procedures
Procedures
that are restrictive shrink the size of the stomach or take up space
inside the stomach, making people feel more full when they eat less.
Diagram of an adjustable gastric banding.
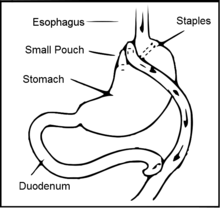
Vertical banded gastroplasty
In the vertical banded gastroplasty,
also called the Mason procedure or stomach stapling, a part of the
stomach is permanently stapled to create a smaller pre-stomach pouch,
which serves as the new stomach.
Adjustable gastric band
The restriction of the stomach also can be created using a silicone
band, which can be adjusted by addition or removal of saline through a
port placed just under the skin. This operation can be performed
laparoscopically, and is commonly referred to as a "lap band". Weight
loss is predominantly due to the restriction of nutrient intake that is
created by the small gastric pouch and the narrow outlet. It is considered one of the safest procedures performed today with a mortality rate of 0.05%.
Sleeve gastrectomy
Sleeve Gastrectomy.
Sleeve gastrectomy, or gastric sleeve, is a surgical weight-loss procedure in which the stomach is reduced to about 15% of its original size, by surgical removal of a large portion of the stomach, following the major curve. The open edges are then attached together (typically with surgical staples,
sutures, or both) to leave the stomach shaped more like a tube, or a
sleeve, with a banana shape. The procedure permanently reduces the size
of the stomach. The procedure is performed laparoscopically and is not reversible. It has been found to be comparable in effectiveness to Roux-en-Y gastric bypass.
Intragastric balloon
Intragastric balloon involves placing a deflated balloon into the
stomach, and then filling it to decrease the amount of gastric space.
The balloon can be left in the stomach for a maximum of 6 months and
results in an average weight loss of 5–9 BMI over half a year.
The intragastric balloon is approved in Australia, Canada, Mexico,
India, United States (received FDA approval in 2015) and several
European and South American countries.
The intragastric balloon may be used prior to another bariatric
surgery in order to assist the patient to reach a weight which is
suitable for surgery, further it can also be used on several occasions
if necessary.
There are three cost categories for the intragastric balloon:
pre-operative (e.g. professional fees, lab work and testing), the
procedure itself (e.g. surgeon, surgical assistant, anesthesia and
hospital fees) and post-operative (e.g. follow-up physician office
visits, vitamins and supplements).
Quoted costs for the intragastric balloon are surgeon-specific
and vary by region. Average quoted costs by region are as follows
(provided in United States Dollars for comparison): Australia: $4,178
USD; Canada: $8,250 USD; Mexico: $5,800 USD; United Kingdom: $6,195 USD;
United States: $8,150 USD).
Stomach folding
Basically, the procedure can best be understood as a version of the more popular gastric sleeve or gastrectomy
surgery where a sleeve is created by suturing rather than removing
stomach tissue thus preserving its natural nutrient absorption
capabilities. Gastric plication significantly reduces the volume of the
patient's stomach, so smaller amounts of food provide a feeling of
satiety.[citation needed] The procedure is producing some significant results that were published in a recent study in Bariatric Times
and are based on post-operative outcomes for 66 patients (44 female)
who had the gastric sleeve plication procedure between January 2007 and
March 2010. Mean patient age was 34, with a mean BMI of 35. Follow-up
visits for the assessment of safety and weight loss were scheduled at
regular intervals in the postoperative period. No major complications
were reported among the 66 patients. Weight loss outcomes are comparable
to gastric bypass.
The study describes gastric sleeve plication (also referred to as gastric imbrication or laparoscopic greater curvature plication) as a restrictive technique that eliminates the complications associated with adjustable gastric banding and vertical sleeve gastrectomy—it does this by creating restriction without the use of implants and without gastric resection (cutting) and staples.
Mixed procedures
Roux-en-Y gastric bypass.
Gastric bypass surgery
A common form of gastric bypass surgery
is the Roux-en-Y gastric bypass, designed to reduce the amount of food a
person is able to eat by cutting away a part of the stomach. Gastric
bypass is a permanent procedure that helps patients by changing how the
stomach and small intestine handle the food that is eaten to achieve and
maintain weight loss goals. After the surgery, the stomach will be smaller. A patient will feel full with less food.
The gastric bypass had been the most commonly performed operation
for weight loss in the United States, and approximately 140,000 gastric
bypass procedures were performed in 2005. Its market share has
decreased since then and by 2011, the frequency of gastric bypass was
thought to be less than 50% of the weight loss surgery market.
A factor in the success of any bariatric surgery is strict post-surgical adherence to a healthy pattern of eating.
There are certain patients who cannot tolerate the malabsorption
and dumping syndrome associated with gastric bypass. In such patients,
although earlier considered to be an irreversible procedure, there are
instances where gastric bypass procedure can be partially reversed.
Diagram of a sleeve gastrectomy with duodenal switch.
Sleeve gastrectomy with duodenal switch
A variation of the biliopancreatic diversion includes a duodenal switch. The part of the stomach
along its greater curve is resected. The stomach is "tubulized" with a
residual volume of about 150 ml. This volume reduction provides the food
intake restriction component of this operation. This type of gastric
resection is anatomically and functionally irreversible. The stomach is
then disconnected from the duodenum and connected to the distal part of
the small intestine. The duodenum and the upper part of the small intestine are reattached to the rest at about 75–100 cm from the colon.
Implantable gastric stimulation
This
procedure where a device similar to a heart pacemaker that is implanted
by a surgeon, with the electrical leads stimulating the external
surface of the stomach, is being studied in the USA. Electrical
stimulation is thought to modify the activity of the enteric nervous system
of the stomach, which is interpreted by the brain to give a sense of
satiety, or fullness. Early evidence suggests that it is less effective
than other forms of bariatric surgery.
Subsequent procedures
After
a person successfully loses weight following bariatric surgery, they
are usually left with excess skin. These are addressed in a series of
plastic surgery procedures sometimes called body contouring in which the skin flaps are removed. Targeted areas include the arms, buttocks and thighs, abdomen, and breasts. These procedures are taken slowly, step by step, and from beginning to end often takes three years. A single body lifting operation can require seven to 10 hours under general anesthesia, blood transfusions and often, another surgeon to assist. Possible risks include infections and reactions and complications due to being under anesthesia for longer than six hours. The person may also experience seroma, a buildup of fluid; dehiscence (wound separation) and deep vein thrombosis (blood clots forming in the legs.) Rare complications include lymphatic
injury and major wound dehiscence. The hospital stay for the procedure
can require from one to four days while recovery can require about a
month.
Eating after bariatric surgery
Immediately
after bariatric surgery, the patient is restricted to a clear liquid
diet, which includes foods such as clear broth, diluted fruit juices or
sugar-free drinks and gelatin desserts. This diet is continued until
the gastrointestinal tract has recovered somewhat from the surgery. The
next stage provides a blended or pureed sugar-free diet for at least
two weeks. This may consist of high protein, liquid or soft foods such
as protein shakes, soft meats, and dairy products. Foods high in
carbohydrates are usually avoided when possible during the initial
weight loss period.
Post-surgery, overeating is curbed because exceeding the capacity of the stomach causes nausea and vomiting. Diet restrictions after recovery from surgery depend in part on the type of surgery. Many patients will need to take a daily multivitamin pill for life to compensate for reduced absorption of essential nutrients.
Because patients cannot eat a large quantity of food, physicians
typically recommend a diet that is relatively high in protein and low in
fats and alcohol.
Fluid recommendations
It
is very common, within the first month post-surgery, for a patient to
undergo volume depletion and dehydration. Patients have difficulty
drinking the appropriate amount of fluids as they adapt to their new
gastric volume. Limitations on oral fluid intake, reduced calorie
intake, and a higher incidence of vomiting and diarrhea are all factors
that have a significant contribution to dehydration. In order to prevent
fluid volume depletion and dehydration, a minimum of 48–64 fl oz
(1.4-1.9 L) should be consumed by repetitive small sips all day.
Costs
The costs
of bariatric surgery depend on the type of procedure performed and
method of payment along with location-specific factors including
geographical region, surgical practice and the hospital in which the
surgery is performed.
The four established procedure types (Roux-en-Y gastric bypass,
gastric banding, vertical sleeve gastrectomy (gastric sleeve) and
duodenal switch) carry an average cost in the United States of $24,000,
$15,000, $19,000 and $27,000 respectively. However, costs can vary
significantly by location. Quoted costs generally include fees for the
hospital, surgeon, surgical assistant, anesthesia and implanted devices
(if applicable). Depending on the surgical practice, costs may include
or omit pre-op, post-op or longer-term follow-up office visits.
Youth
As childhood obesity has more than doubled over recent years and more than tripled in adolescents (according to the CDC), bariatric surgery for youth has become increasingly common. Some worry that a decline in life expectancy might occur from the increasing levels of obesity,
so providing youth with proper care may help prevent the serious
medical complications caused by obesity and its related diseases.
Difficulties and ethical issues arise when making decisions related to
obesity treatments for those that are too young or otherwise unable to
give consent without adult guidance.
Children and adolescents are still developing, both physically
and mentally. This makes it difficult for them to make an informed
decision and give consent to move forward with a treatment.
These patients may also be experiencing severe depression or other
psychological disorders related to their obesity that make understanding
the information very difficult.
History
Open weight loss surgery began slowly in the 1950s with the intestinal bypass. It involved anastomosis
of the upper and lower intestine, which bypasses a large amount of the
absorptive circuit, which caused weight loss purely by the malabsorption
of food. Later Drs. J. Howard Payne, Lorent T. DeWind and Robert R.
Commons developed in 1963 the Jejuno-colic Shunt, which connected the
upper small intestine to the colon. The laboratory research leading to
gastric bypass did not begin until 1965 when Dr. Edward E. Mason
(b.1920) and Dr. Chikashi Ito (1930–2013) at the University of Iowa
developed the original gastric bypass for weight reduction which led to
fewer complications than the intestinal bypass and for this reason
Mason is known as the "father of obesity surgery".