The former St Elizabeth's Hospital in 2006, closed and boarded up. Located in Washington D.C., the hospital had been one of the sites of the Rosenhan experiment in the 1970s.
Deinstitutionalisation (or deinstitutionalization) is the process of replacing long-stay psychiatric hospitals with less isolated community mental health services for those diagnosed with a mental disorder or developmental disability.
In the late 20th century, it led to the closure of many psychiatric
hospitals, as patients were increasingly cared for at home, in halfway houses and clinics, and in regular hospitals.
Deinstitutionalisation works in two ways. The first focuses on
reducing the population size of mental institutions by releasing
patients, shortening stays, and reducing both admissions and readmission
rates. The second focuses on reforming psychiatric care to reduce (or
avoid encouraging) feelings of dependency, hopelessness and other
behaviors that make it hard for patients to adjust to a life outside of
care.
The modern deinstitutionalisation movement was made possible by the discovery of psychiatric drugs in the mid-20th century, which could manage psychotic
episodes and reduced the need for patients to be confined and
restrained. Another major impetus was a series of socio-political
movements that campaigned for patient freedom. Lastly, there were
financial imperatives, with many governments also viewing it as a way to
save costs.
The movement to reduce institutionalisation was met with wide
acceptance in Western countries, though its effects have been the
subject of many debates. Critics of the policy include defenders of the
previous policies as well as those who believe the reforms did not go
far enough to provide freedom to patients.
History
19th century
Vienna's Narrenturm—German for "fools' tower"—was one of the earliest buildings specifically designed for mentally ill people. It was built in 1784.
The 19th century saw a large expansion in the number and size of asylums in Western industrialised
countries. In contrast to the prison-like asylums of old, these were
designed to be comfortable places where patients could live and be
treated, in keeping with the movement towards "moral treatment". In spite of these ideals, they became overstretched, non-therapeutic, isolated in location, and neglectful of patients.
20th century
By
the beginning of the 20th century, increasing admissions had resulted
in serious overcrowding, causing many problems for psychiatric
institutions. Funding was often cut, especially during periods of
economic decline and wartime. Asylums became notorious for poor living
conditions, lack of hygiene, overcrowding, ill-treatment, and abuse of patients; many patients starved to death.
The first community-based alternatives were suggested and tentatively
implemented in the 1920s and 1930s, although asylum numbers continued to
increase up to the 1950s.
Origins of the modern movement
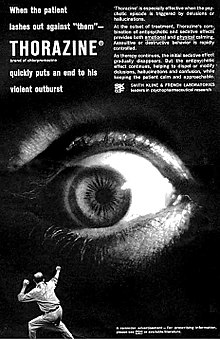
The
movement for deinstitutionalisation moved to the forefront in various
countries during the 1950s and 1960s with the advent of chlorpromazine and other antipsychotic drugs.
A key text in the development of deinstitutionalisation was Asylums: Essays on the Social Situation of Mental Patients and Other Inmates, a 1961 book by sociologist Erving Goffman. The book is one of the first sociological examinations of the social situation of mental patients, the hospital. Based on his participant observation field work, the book details Goffman's theory of the "total institution"
(principally in the example he gives, as the title of the book
indicates, mental institutions) and the process by which it takes
efforts to maintain predictable and regular behavior on the part of both
"guard" and "captor," suggesting that many of the features of such
institutions serve the ritual function of ensuring that both classes of
people know their function and social role, in other words of "institutionalizing" them.
Franco Basaglia, a leading Italian psychiatrist who inspired and was the architect of the psychiatric reform in Italy, also defined mental hospital as an oppressive, locked and total institution
in which prison-like, punitive rules are applied, in order to gradually
eliminate its own contents, and patients, doctors and nurses are all
subjected (at different levels) to the same process of institutionalism. Other critics went further and campaigned against all involuntary psychiatric treatment. In 1970, Goffman worked with Thomas Szasz and George Alexander to found the American Association for the Abolition of Involuntary Mental Hospitalisation (AAAIMH), who proposed abolishing all involuntary psychiatric intervention, particularly involuntary commitment, against individuals. The association provided legal help to psychiatric patients and published a journal, The Abolitionist, until it was dissolved in 1980.
Reform
The prevailing public arguments, time of onset, and pace of reforms varied by country. Leon Eisenberg lists three key factors that led to deinstitutionalisation gaining support. The first were socio-political campaigns for the better treatment of patients. Some of these were spurred on by institutional abuse scandals in the 1960s and 1970s, such as Willowbrook State School in the United States and Ely Hospital
in the United Kingdom. Other incentives were that new psychiatric
medications made it more feasible to release people into the community,
and the argument that community services would be cheaper.
Mental health professionals, public officials, families, advocacy
groups, public citizens, and unions held differing views on
deinstitutionalisation.
However, the 20th Century marked the development of the first
community services designed specifically to divert
deinstitutionalization and to develop the first conversions from
institutional, governmental systems to community majority systems
(governmental-NGO-For Profit).
These services are so common throughout the world (e.g., individual and
family support services, groups homes, community and supportive living,
foster care and personal care homes, community residences, community
mental health offices, supported housing) that they are often "delinked"
from the term deinstitutionalization. Common historical figures in
deinstitutionalization in the US include Geraldo Rivera, Robert
Williams, Burton Blatt, Gunnar Dybwad, Michael Kennedy, Frank Laski, Steven J. Taylor, Douglas P. Biklen, David Braddock, Robert Bogdan and K. C. Lakin. in the fields of "intellectual disabilities" (e.g., amicus curae, Arc-US to the US Supreme Court; US state consent decrees).
Community organizing and development regarding the fields of
mental health, traumatic brain injury, aging (nursing facilities) and
children's institutions/private residential schools represent other
forms of diversion and "community re-entry". Paul Carling's book, Return
to the Community: Building Support Systems for People with Psychiatric
Disabilities describes mental health planning and services in that
regard, including for addressing the health and personal effects of
"long term institutionalization".
and the psychiatric field continued to research whether "hospitals"
(e.g., forced involuntary care in a state institution; voluntary,
private admissions) or community living was better.
US states have made substantial investments in the community, and
similar to Canada, shifted some but not all institutional funds to the
community sectors as deinstitutionalization. For example, NYS Education,
Health and Social Services Laws identify mental health personnel in the
state of New York, and the two term Obama Presidency in the US created a
high-level Office of Social and Behavioral Services.
The 20th Century marked the growth in a class of
deinstitutionalization and community researchers in the US and world,
including a class of university women.
These women follow university education on social control and the myths
of deinstitutionalization, including common forms of
transinstitutionalization such as transfers to prison systems in the
21st Century, "budget realignments", and the new subterfuge of community
data reporting.
Consequences
Community services that developed include supportive housing with full or partial supervision and specialised teams (such as assertive community treatment and early intervention teams).
Costs have been reported as generally equivalent to inpatient
hospitalisation, even lower in some cases (depending on how well or
poorly funded the community alternatives are). Although deinstitutionalisation has been positive for the majority of patients, it also has shortcomings.
Criticism of deinstitutionalisation takes two forms. Some, like E. Fuller Torrey, defend the use of psychiatric institutions and conclude that deinstitutionalisation was a move in the wrong direction.
Others, such as Walid Fakhoury and Stefan Priebe, argue that it was an
unsuccessful move in the right direction, suggesting that modern day
society faces the problem of "reinstitutionalisation". While coming from opposite viewpoints, both sets of critics argue that the policy left many patients homeless or in prison. Leon Eisenberg
has argued that deinstitutionalisation was generally positive for
patients, while noting that some were left homeless or without care.
Misconceptions
There
is a common perception by the public and media that people with mental
disorders are more likely to be dangerous and violent if released into
the community. However, a large 1998 study in Archives of General Psychiatry
suggested that discharged psychiatric patients without substance abuse
symptoms are no more likely to commit violence than others without
substance abuse symptoms in their neighborhoods, which were usually
economically deprived and high in substance abuse and crime. The study
also reported that a higher proportion of the patients than of the
others in the neighborhoods reported symptoms of substance abuse.
Findings on violence committed by those with mental disorders in
the community have been inconsistent and related to numerous factors; a
higher rate of more serious offences such as homicide have sometimes
been found but, despite high-profile homicide cases, the evidence
suggests this has not been increased by deinstitutionalisation.
The aggression and violence that does occur, in either direction, is
usually within family settings rather than between strangers.
Adequacy of treatment and support
Common
criticisms of the new community services are that they have been
uncoordinated, underfunded and unable to meet complex needs.
Problems with coordination arose because care was being provided by
multiple for-profit businesses, non-profit organizations and multiple
levels of government.
Torrey has opposed deinstitutionalisation in principle, arguing
that people with mental illness will be resistant to medical help due to
the nature of their conditions. These views have made him a
controversial figure in psychiatry. He believes that reducing psychiatrists' powers to use involuntary commitment led to many patients losing out on treatment, and that many who would have previously lived in institutions are now homeless or in prison.
Other critics argue that deinstitutionalisation had laudable
goals, but some patients lost out on care due to problems in the
execution stage. In a 1998 study of the effects of
deinstitutionalisation in the United Kingdom, Means and Smith argue that
the program had some successes, such as increasing the participation of
volunteers in mental healthcare, but that it was underfunded and let
down by a lack of coordination between the health service and social services.
Transinstitutionalisation
Some
mental health academics and campaigners have argued that
deinstitutionalisation was well-intentioned for trying to make patients
less dependent on psychiatric care, but in practice patients were still
left being dependent on the support of a mental healthcare system, a
phenomenon known as "reinstitutionalisation" or "transinstitutionalisation".
The argument is that community services can leave the mentally
ill in a state of social isolation (even if it is not physical
isolation), frequently meeting other service users but having little
contact with the rest of the public community. Fakhoury and Priebe said
that instead of "community psychiatry", reforms established a "psychiatric community".
Julie Racino argues that having a closed social circle like this can
limit opportunities for mentally ill people to integrate with the wider
society, such as personal assistance services.
Thomas Szasz,
a longtime opponent of involuntary psychiatric treatment, argued that
the reforms never addressed the aspects of psychiatry that he objected
to, particularly his belief that mental illnesses are not true illnesses
but medicalized social and personal problems.
Medication
There was an increase in prescriptions of psychiatric medication in the years following deinstitutionalization.
Although most of these drugs had been discovered in the years before,
deinstitutionalisation made it far cheaper to care for a mental health
patient and increased the profitability of the drugs. Some researchers
argue that this created economic incentives to increase the frequency of
psychiatric diagnosis (and related diagnoses, such as ADHD in children) that did not happen in the era of costly hospitalized psychiatry.
In most countries (except some countries that are either in
extreme poverty or are hindered from importing psychiatric drugs by
their customs regulations), more than 10% of the population are now on some form of psychiatric medicine. This increases to more than 15% in some countries such as the United Kingdom. A 2012 study by Kales, Pierce and Greenblatt argued that these medicines were being overprescribed.
Victimisation
Moves
to community living and services have led to various concerns and
fears, from both the individuals themselves and other members of the
community. Over a quarter of individuals accessing community mental
health services in a US inner-city area are victims of at least one
violent crime per year, a proportion eleven times higher than the
inner-city average. The elevated victim rate holds for every category of
crime, including rape/sexual assault, other violent assaults, and
personal and property theft. Victimisation rates are similar to those with developmental disabilities.
Worldwide
Asia
Hong Kong
In Hong Kong, a number of residential care services such as halfway houses, long-stay care homes, supported hostels
are provided for the discharged patients. In addition, community
support services such as rehabilitation day services and mental health
care have been launched to facilitate the patients' re-integration into
the community.
Japan
Unlike most developed countries, Japan has not followed a program of deinstitutionalisation. The number of hospital beds has risen steadily over the last few decades. Physical restraints
are used far more often. In 2014, more than 10,000 people were
restrained–the highest ever recorded, and more than double the number a
decade earlier.
In 2018, the Japanese Ministry of Health introduced revised guidelines
that placed more restrictions against the use of restraints.
Africa
Uganda has one psychiatric hospital.
There are only 40 psychiatrists in Uganda. The World Health
Organisation estimates that 90% of mentally ill people here never get
treatment.
Australia and Oceania
New Zealand
New Zealand established a reconciliation initiative in 2005 to address the ongoing compensation
payouts to ex-patients of state-run mental institutions in the 1970s to
1990s. A number of grievances were heard, including: poor reasons for
admissions; unsanitary and overcrowded conditions; lack of communication
to patients and family members; physical violence and sexual misconduct
and abuse; inadequate mechanisms for dealing with complaints; pressures
and difficulties for staff, within an authoritarian hierarchy based on containment; fear and humiliation in the misuse of seclusion; over-use and abuse of ECT, psychiatric medications, and other treatments as punishments, including group therapy, with continued adverse effects;
lack of support on discharge; interrupted lives and lost potential; and
continued stigma, prejudice, and emotional distress and trauma.
There were some references to instances of helpful aspects or
kindnesses despite the system. Participants were offered counselling to
help them deal with their experiences, along with advice on their
rights, including access to records and legal redress.
Europe
In some countries
where deinstitutionalisation has occurred, "re-institutionalisation",
or relocation to different institutions, has begun, as evidenced by
increases in the number of supported housing facilities, forensic psychiatric beds, and the growing prison population.
Some developing European countries still rely on asylums.
Italy
Italy was the first country to begin the deinstitutionalisation of
mental health care and to develop a community-based psychiatric system. The Italian system served as a model of effective service and paved the way for deinstitutionalisation of mental patients. Since the late 1960s, the Italian physician Giorgio Antonucci questioned the basis itself of psychiatry. After working with Edelweiss Cotti in 1968 at the Centro di Relazioni Umane in Cividale del Friuli
– an open ward created as an alternative to the psychiatric hospital –
from 1973 to 1996 Antonucci worked on the dismantling of the psychiatric
hospitals Osservanza and Luigi Lolli of Imola and the liberation – and restitution to life – of the people there secluded. In 1978, the Basaglia Law had started Italian psychiatric reform that resulted in the end of the Italian state mental hospital system in 1998.
The reform was focused on the gradual dismantlement of
psychiatric hospitals, which required an effective community mental
health service.
The object of community care was to reverse the long-accepted practice
of isolating the mentally ill in large institutions and to promote their
integration in a socially stimulating environment, while avoiding
subjecting them to excessive social pressures.
The work of Giorgio Antonucci,
instead of changing the form of commitment from the mental hospital to
other forms of coercion, questions the basis of psychiatry, affirming
that mental hospitals are the essence of psychiatry and rejecting any
possible reform of psychiatry, that must be completely eliminated.
United Kingdom
The water tower of Park Prewett Hospital in Basingstoke, Hampshire. The hospital was redeveloped into a housing estate after its closure in 1997.
In the United Kingdom, the trend towards deinstitutionalisation began
in the 1950s. At the time, 0.4% of the population of England were
housed in asylums. The government of Harold Macmillan sponsored the Mental Health Act 1959, which removed the distinction between psychiatric hospitals and other types of hospitals. Enoch Powell,
the Minister of Health in the early 1960s, criticized psychiatric
institutions in his 1961 "Water Tower" speech and called for most of the
care to be transferred to general hospitals and the community. The campaigns of Barbara Robb and several scandals involving mistreatment at asylums (notably Ely Hospital) furthered the campaign. The Ely Hospital scandal led to an inquiry led by Brian Abel-Smith and a 1971 white paper that recommended further reform.
The policy of deinstitutionalisation came to be known as Care in the Community at the time it was taken up by the government of Margaret Thatcher. Large-scale closures of the old asylums began in the 1980s. By 2015, none remained.
North America
United States
President John F. Kennedy signs the Community Mental Health Act.
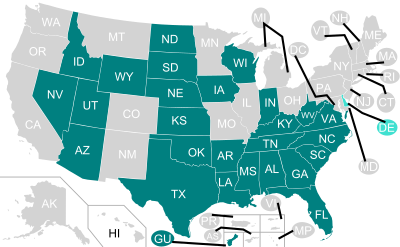
The United States has experienced two main waves of
deinstitutionalisation. The first wave began in the 1950s and targeted
people with mental illness. The second wave began roughly 15 years later and focused on individuals who had been diagnosed with a developmental disability. Loren Mosher argues that deinstitutionalisation fully began in the 1970s and was due to financial incentives like SSI and Social Security Disability, rather than after the earlier introduction of psychiatric drugs.
The most important factors that led to deinstitutionalisation
were changing public attitudes to mental health and mental hospitals,
the introduction of psychiatric drugs and individual states' desires to reduce costs from mental hospitals. The federal government offered financial incentives to the states to achieve this goal. Stroman pinpoints World War II as the point when attitudes began to change. In 1946, Life magazine published one of the first exposés of the shortcomings of mental illness treatment. Also in 1946, Congress passed the National Mental Health Act of 1946, which created the National Institute of Mental Health (NIMH). NIMH was pivotal in funding research for the developing mental health field.
President John F. Kennedy had a special interest in the issue of mental health because his sister, Rosemary, had incurred brain damage after being lobotomised at the age of 23. His administration sponsored the successful passage of the Community Mental Health Act, one of the most important laws that led to deinstitutionalization. The movement continued to gain momentum during the Civil Rights Movement.
The 1965 amendments to Social Security shifted about 50% of the mental
health care costs from states to the federal government,
motivating state governments to promote deinstitutionalization. The
1970s saw the founding of several advocacy groups, including Liberation
of Mental Patients, Project Release, Insane Liberation Front, and the National Alliance on Mental Illness (NAMI).
The lawsuits these activist groups filed led to some key court
rulings in the 1970s that increased the rights of patients. In 1973, a
federal district court ruled in Souder v. Brennan that whenever
patients in mental health institutions performed activity that conferred
an economic benefit to an institution, they had to be considered
employees and paid the minimum wage required by the Fair Labor Standards Act of 1938. Following this ruling, institutional peonage was outlawed. In the 1975 ruling O'Connor v. Donaldson, the U.S. Supreme Court restricted the rights of states to incarcerate someone who was not violent. This was followed up with the 1978 ruling Addington v. Texas, further restricting states from confining anyone involuntarily for mental illness. In 1975, the United States Court of Appeals for the First Circuit ruled in favour of the Mental Patient's Liberation Front in Rogers v. Okin, establishing the right of a patient to refuse treatment. Later reforms included the Mental Health Parity Act, which required health insurers to give mental health patients equal coverage.
Other factors included scandals. A 1972 television broadcast exposed the abuse and neglect of 5,000 patients at the Willowbrook State School in Staten Island, New York. The Rosenhan's experiment
in 1973 caused several psychiatric hospitals to fail to notice fake
patients who showed no symptoms once they were institutionalized. The pitfalls of institutionalization were dramatized in an award-winning 1975 film, One Flew Over the Cuckoo's Nest.
In 1955, for every 100,000 US citizens there were 340 psychiatric
hospital beds. In 2005 that number had diminished to 17 per 100,000.
South America
In several South American countries,
such as in Argentina, the total number of beds in asylum-type
institutions has decreased, replaced by psychiatric inpatient units in
general hospitals and other local settings.
In Brazil, there are 6003 psychiatrists, 18,763 psychologists,
1985 social workers, 3119 nurses and 3589 occupational therapists
working for the Unified Health System (SUS). At primary care level,
there are 104,789 doctors, 184, 437 nurses and nurse technicians and
210,887 health agents. The number of psychiatrists is roughly 5 per
100,000 inhabitants in the Southeast region, and the Northeast region
has less than 1 psychiatrist per 100,000 inhabitants. The number of
psychiatric nurses is insufficient in all geographical areas, and
psychologists outnumber other mental health professionals in all regions
of the country. The rate of beds in psychiatric hospitals in the
country is 27.17 beds per 100,000 inhabitants. The rate of patients in
psychiatric hospitals is 119 per 100,000 inhabitants. The average length
of stay in mental hospitals is 65.29 days.