|
| |||

| |||
| Names | |||
|---|---|---|---|
| Preferred IUPAC name
2-Hydroxybenzoic acid | |||
| Identifiers | |||
3D model (JSmol)
|
|||
| ChEBI | |||
| ChEMBL | |||
| ChemSpider | |||
| DrugBank | |||
| ECHA InfoCard | 100.000.648 | ||
| EC Number |
| ||
| KEGG | |||
PubChem CID
|
|||
| RTECS number |
| ||
| UNII | |||
CompTox Dashboard (EPA)
|
|||
| Properties | |
|---|---|
| C7H6O3 | |
| Molar mass | 138.122 g/mol |
| Appearance | Colorless to white crystals |
| Odor | Odorless |
| Density | 1.443 g/cm3 (20 °C) |
| Melting point | 158.6 °C (317.5 °F; 431.8 K) |
| Boiling point | 200 °C (392 °F; 473 K) decomposes 211 °C (412 °F; 484 K) at 20 mmHg |
| Sublimes at 76 °C | |
| |
| Solubility | Soluble in ether, CCl4, benzene, propanol, acetone, ethanol, oil of turpentine, toluene |
| Solubility in benzene |
|
| Solubility in chloroform |
|
| Solubility in methanol |
|
| Solubility in olive oil | 2.43 g/100 g (23 °C) |
| Solubility in acetone | 39.6 g/100 g (23 °C) |
| log P | 2.26 |
| Vapor pressure | 10.93 mPa |
| Acidity (pKa) |
|
| UV-vis (λmax) | 210 nm, 234 nm, 303 nm (4 mg/dL in ethanol) |
| −72.23·10−6 cm3/mol | |
Refractive index (nD)
|
1.565 (20 °C) |
| 2.65 D | |
| Thermochemistry | |
Std enthalpy of
formation (ΔfH⦵298) |
−589.9 kJ/mol |
Std enthalpy of
combustion (ΔcH⦵298) |
3.025 MJ/mol |
| Pharmacology | |
| A01AD05 (WHO) B01AC06 (WHO) D01AE12 (WHO) N02BA01 (WHO) S01BC08 (WHO) | |
| Hazards | |
| Safety data sheet | MSDS |
| GHS pictograms |  
|
| GHS Signal word | Danger |
| H302, H318 | |
| P280, P305+351+338 | |
| Eye hazard | Severe irritation |
| Skin hazard | Mild irritation |
| NFPA 704 (fire diamond) | |
| Flash point | 157 °C (315 °F; 430 K) closed cup |
| 540 °C (1,004 °F; 813 K) | |
| Lethal dose or concentration (LD, LC): | |
LD50 (median dose)
|
480 mg/kg (mice, oral) |
| Related compounds | |
Related compounds
|
Methyl salicylate, Benzoic acid, Phenol, Aspirin, 4-Hydroxybenzoic acid, Magnesium salicylate, Choline salicylate, Bismuth subsalicylate, Sulfosalicylic acid |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa). | |
| Infobox references | |
|
|
|
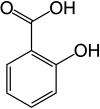
Salicylic acid is an organic compound with the formula HOC6H4CO2H. A colorless, bitter-tasting solid, it is a precursor to and a metabolite of aspirin (acetylsalicylic acid). It is a plant hormone. The name is from Latin salix for willow tree. It is an ingredient in some anti-acne products. Salts and esters of salicylic acid are known as salicylates.
Uses
Medicine
Salicylic acid as a medication is used commonly to remove the outer layer of the skin. As such, it is used to treat warts, psoriasis, acne vulgaris, ringworm, dandruff, and ichthyosis.
Similar to other hydroxy acids, salicylic acid is an ingredient in many skincare products for the treatment of seborrhoeic dermatitis, acne, psoriasis, calluses, corns, keratosis pilaris, acanthosis nigricans, ichthyosis, and warts.
Uses in manufacturing
Salicylic acid is used in the production of other pharmaceuticals, including 4-aminosalicylic acid, sandulpiride, and landetimide (via salethamide).
Salicylic acid has long been a key starting material for making acetylsalicylic acid (aspirin). Aspirin (acetylsalicylic acid or ASA) is prepared by the esterification of the phenolic hydroxyl group of salicylic acid with the acetyl group from acetic anhydride or acetyl chloride.
Bismuth subsalicylate, a salt of bismuth and salicylic acid, is the active ingredient in stomach-relief aids such as Pepto-Bismol, is the main ingredient of Kaopectate, and "displays anti-inflammatory action (due to salicylic acid) and also acts as an antacid and mild antibiotic".
Other derivatives include methyl salicylate used as a liniment to soothe joint and muscle pain and choline salicylate used topically to relieve the pain of mouth ulcers.
Other uses
Salicylic acid is used as a food preservative, a bactericide, and an antiseptic.
Sodium salicylate is a useful phosphor in the vacuum ultraviolet spectral range, with nearly flat quantum efficiency for wavelengths between 10 and 100 nm. It fluoresces in the blue at 420 nm. It is easily prepared on a clean surface by spraying a saturated solution of the salt in methanol followed by evaporation.
Mechanism of action
Salicylic acid modulates COX1 enzymatic activity to decrease the formation of pro-inflammatory prostaglandins. Salicylate may competitively inhibit prostaglandin formation. Salicylate's antirheumatic (nonsteroidal anti-inflammatory) actions are a result of its analgesic and anti-inflammatory mechanisms.
Salicylic acid works by causing the cells of the epidermis to slough off more readily, preventing pores from clogging up, and allowing room for new cell growth. Salicylic acid inhibits the oxidation of uridine-5-diphosphoglucose (UDPG) competitively with nicotinamide adenosine dinucleotide and noncompetitively with UDPG. It also competitively inhibits the transferring of glucuronyl group of uridine-5-phosphoglucuronic acid to the phenolic acceptor.
The wound-healing retardation action of salicylates is probably due mainly to its inhibitory action on mucopolysaccharide synthesis.
Safety
If high concentrations of salicylic ointment are applied to a large percentage of body surface, high levels of salicylic acid can enter the blood, requiring hemodialysis to avoid further complications.
Production and chemical reactions
Biosynthesis
Salicylic acid is biosynthesized from the amino acid phenylalanine. In Arabidopsis thaliana, it can be synthesized via a phenylalanine-independent pathway.
Industrial synthesis
Sodium salicylate is commercially prepared by treating sodium phenolate (the sodium salt of phenol) with carbon dioxide at high pressure (100 atm) and high temperature (115 °C) – a method known as the Kolbe-Schmitt reaction. Acidification of the product with sulfuric acid gives salicylic acid:
It can also be prepared by the hydrolysis of aspirin (acetylsalicylic acid) or methyl salicylate (oil of wintergreen) with a strong acid or base.
Reactions
Upon heating, salicylic acid converts to phenyl salicylate:
- 2 HOC6H4CO2H → C6H5O2C6H4OH + CO2 + H2O
Further heating gives xanthone.
Salicylic acid as its conjugate base is a chelating agent, with an affinity for iron(III).
Salicylic acid slowly degrades to phenol and carbon dioxide at 200–230 °C:
- C6H4OH(CO2H) → C6H5OH + CO2
History
Hippocrates, Galen, Pliny the Elder, and others knew that willow bark could ease pain and reduce fevers. It was used in Europe and China to treat these conditions. This remedy is mentioned in texts from Ancient Egypt, Sumer, and Assyria. The Cherokee and other Native Americans use an infusion of the bark for fever and other medicinal purposes.
In 2014, archaeologists identified traces of salicylic acid on seventh-century pottery fragments found in east-central Colorado. The Reverend Edward Stone, a vicar from Chipping Norton, Oxfordshire, England, noted in 1763 that the bark of the willow was effective in reducing a fever.
The active extract of the bark, called salicin, after the Latin name for the white willow (Salix alba), was isolated and named by German chemist Johann Andreas Buchner in 1828. A larger amount of the substance was isolated in 1829 by Henri Leroux, a French pharmacist. Raffaele Piria, an Italian chemist, was able to convert the substance into a sugar and a second component, which on oxidation becomes salicylic acid.
Salicylic acid was also isolated from the herb meadowsweet (Filipendula ulmaria, formerly classified as Spiraea ulmaria) by German researchers in 1839. While their extract was somewhat effective, it also caused digestive problems such as gastric irritation, bleeding, diarrhea, and even death when consumed in high doses.
Dietary sources
Salicylic acid occurs in plants as free salicylic acid and its carboxylated esters and phenolic glycosides. Several studies suggest that humans metabolize salicylic acid in measurable quantities from these plants. High-salicylate beverages and foods include beer, coffee, tea, numerous fruits and vegetables, sweet potato, nuts, and olive oil. Meat, poultry, fish, eggs, dairy products, sugar, and breads and cereals have low salicylate content.
Some people with sensitivity to dietary salicylates may have symptoms of allergic reaction, such as bronchial asthma, rhinitis, gastrointestinal disorders, or diarrhea, so may need to adopt a low-salicylate diet.
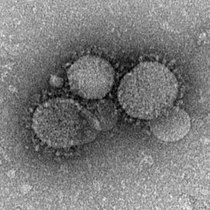
Plant hormone
Salicylic acid is a phenolic phytohormone, and is found in plants with roles in plant growth and development, photosynthesis, transpiration, and ion uptake and transport. Salicylic acid is involved in endogenous signaling, mediating plant defense against pathogens. It plays a role in the resistance to pathogens (i.e. systemic acquired resistance) by inducing the production of pathogenesis-related proteins and other defensive metabolites. Exogenously, salicylic acid can aid plant development via enhanced seed germination, bud flowering, and fruit ripening, though too high of a concentration of salicylic acid can negatively regulate these developmental processes.
The volatile methyl ester of salicylic acid, methyl salicylate, can also diffuse through the air, facilitating plant-plant communication. Methyl salicylate is taken up by the stomata of the nearby plant, where it can induce an immune response after being converted back to salicylic acid.
Signal transduction
A number of proteins have been identified that interact with SA in plants, especially salicylic acid binding proteins (SABPs) and the NPR genes (Nonexpressor of pathogenesis related genes), which are putative receptors.
History
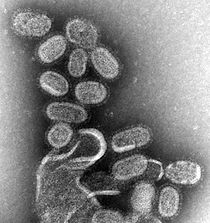
In 1979, salicylates were found to be involved in induced defenses of tobacco against tobacco mosaic virus. In 1987, salicylic acid was identified as the long-sought signal that causes thermogenic plants such as the voodoo lily, Sauromatum guttatum, to heat up.