From Wikipedia, the free encyclopedia
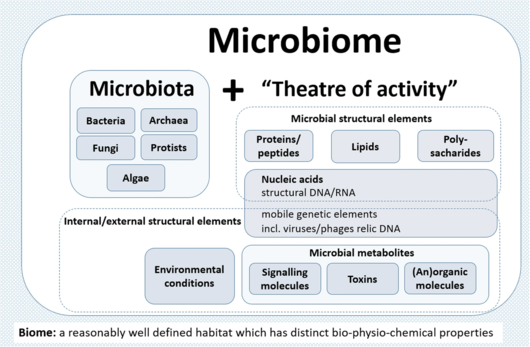
A microbiome (from Ancient Greek μικρός (mikrós) 'small', and βίος (bíos) 'life') is the community of microorganisms that can usually be found living together in any given habitat. It was defined more precisely in 1988 by Whipps et al.
as "a characteristic microbial community occupying a reasonably
well-defined habitat which has distinct physio-chemical properties. The
term thus not only refers to the microorganisms involved but also
encompasses their theatre of activity". In 2020, an international panel
of experts published the outcome of their discussions on the definition
of the microbiome. They proposed a definition of the microbiome based on
a revival of the "compact, clear, and comprehensive description of the
term" as originally provided by Whipps et al., but supplemented with two explanatory paragraphs. The first explanatory paragraph pronounces the dynamic character of the microbiome, and the second explanatory paragraph clearly separates the term microbiota from the term microbiome.
The microbiota consists of all living members forming the microbiome. Most microbiome researchers agree bacteria, archaea, fungi, algae, and small protists should be considered as members of the microbiome. The integration of phages, viruses, plasmids, and mobile genetic elements is more controversial. Whipps's "theatre of activity" includes the essential role secondary metabolites play in mediating complex interspecies interactions and ensuring survival in competitive environments. Quorum sensing induced by small molecules allows bacteria to control cooperative activities and adapts their phenotypes to the biotic environment, resulting, e.g., in cell-cell adhesion or biofilm formation.
All animals and plants form associations with microorganisms,
including protists, bacteria, archaea, fungi, and viruses. In the ocean,
animal–microbial relationships were historically explored in single
host–symbiont systems. However, new explorations into the diversity of
microorganisms associating with diverse marine animal hosts is moving
the field into studies that address interactions between the animal host
and the multi-member microbiome. The potential for microbiomes to
influence the health, physiology, behaviour, and ecology of marine
animals could alter current understandings of how marine animals adapt
to change. This applies to especially the growing climate-related and
anthropogenic-induced changes already impacting the ocean. The plant microbiome
plays key roles in plant health and food production and has received
significant attention in recent years. Plants live in association with
diverse microbial consortia, referred to as the plant microbiota, living both inside (the endosphere)
and outside (the episphere) of plant tissues. They play important roles
in the ecology and physiology of plants. The core plant microbiome is
thought to contain keystone microbial taxa essential for plant health
and for the fitness of the plant holobiont. Likewise, the mammalian gut microbiome
has emerged as a key regulator of host physiology, and coevolution
between host and microbial lineages has played a key role in the
adaptation of mammals to their diverse lifestyles.
Microbiome research originated in microbiology back in the
seventeenth century. The development of new techniques and equipment
boosted microbiological research and caused paradigm shifts in
understanding health and disease. The development of the first
microscopes allowed the discovery of a new, unknown world and led to the
identification of microorganisms. Infectious diseases became the
earliest focus of interest and research. However, only a small
proportion of microorganisms are associated with disease or
pathogenicity. The overwhelming majority of microbes are essential for
healthy ecosystem functioning and known for beneficial interactions with
other microbes and organisms. The concept that microorganisms exist as
single cells began to change as it became increasingly obvious that
microbes occur within complex assemblages in which species interactions and communication are critical. Discovery of DNA, the development of sequencing technologies, PCR, and cloning
techniques enabled the investigation of microbial communities using
cultivation-independent approaches. Further paradigm shifts occurred at
the beginning of this century and still continue, as new sequencing
technologies and accumulated sequence data have highlighted both the
ubiquity of microbial communities in association within higher organisms
and the critical roles of microbes in human, animal, and plant health.
These have revolutionised microbial ecology. The analysis of genomes and metagenomes in a high-throughput
manner now provide highly effective methods for researching the
functioning of both individual microorganisms as well as whole microbial
communities in natural habitats.
Background
History
Microbiome
research originated in microbiology and started back in the seventeenth
century. The development of new techniques and equipment has boosted
microbiological research and caused paradigm shifts in understanding
health and disease. Since infectious diseases have affected human
populations throughout most of history, medical microbiology was the earliest focus of research and public interest. Additionally, food microbiology is an old field of empirical applications. The development of the first microscopes allowed the discovery of a new, unknown world and led to the identification of microorganisms.
- Paradigm shift
Shift of paradigm from microbes as unsocial organisms causing
diseases to a holistic view of microorganisms as the centre of the One Health Concept interconnecting all areas of human lives.
Access to the previously invisible world opened the eyes and the minds of the researchers of the seventeenth century. Antonie van Leeuwenhoek investigated diverse bacteria of various shapes, fungi, and protozoa, which he called animalcules, mainly from water, mud, and dental plaque samples, and discovered biofilms as a first indication of microorganisms interacting within complex communities. Robert Koch's
explanation of the origin of human and animal diseases as a consequence
of microbial infection and development of the concept of pathogenicity
was an important milestone in microbiology. These findings shifted the
focus of the research community and the public on the role of
microorganisms as disease-forming agents that needed to be eliminated.
However, comprehensive research over the past century has shown
only a small proportion of microorganisms are associated with disease or
pathogenicity. The overwhelming majority of microbes are essential for ecosystem functioning
and known for beneficial interactions with other microbes as well as
macroorganisms. In fact, maintaining a healthy microbiome is essential
for human health and may be a target for new therapeutics. At the end of the nineteenth century, microbial ecology started with the pioneering work by Martinus W. Beijerinck and Sergei Winogradsky. The newly established science of environmental microbiology resulted in another paradigm shift: microorganisms are everywhere in natural environments, often associated with hosts and, for the first time, beneficial effects on their hosts were reported.
Subsequently, the concept that microorganisms exist as single
cells began to change as it became increasingly obvious that microbes
occur within complex assemblages in which species interactions and
communication are critical to population dynamics and functional
activities. Discovery of DNA, the development of sequencing technologies, PCR, and cloning techniques enabled the investigation of microbial communities using cultivation-independent, DNA and RNA-based approaches.
A further important step was the introduction of phylogenetic markers such as the 16S rRNA gene for microbial community analysis by Carl Woese and George E. Fox in 1977. Nowadays biologists can barcode bacteria, archaea, fungi, algae, and protists in their natural habitats, e.g., by targeting their 16S and 18S rRNA genes, internal transcribed spacer (ITS), or, alternatively, specific functional regions of genes coding for specific enzymes.
Another major paradigm shift was initiated at the beginning of
this century and continues through today, as new sequencing technologies
and accumulated sequence data have highlighted both the ubiquity of microbial communities in association within higher organisms and the critical roles of microbes in human, animal, and plant health. These new possibilities have revolutionized microbial ecology, because the analysis of genomes and metagenomes
in a high-throughput manner provides efficient methods for addressing
the functional potential of individual microorganisms as well as of
whole communities in their natural habitats. Multiomics technologies including metatranscriptome, metaproteome and metabolome
approaches now provide detailed information on microbial activities in
the environment. Based on the rich foundation of data, the cultivation
of microbes, which was often ignored or underestimated over the last
thirty years, has gained new importance, and high throughput culturomics
is now an important part of the toolbox to study microbiomes. The high
potential and power of combining multiple "omics" techniques to analyze
host-microbe interactions are highlighted in several reviews.
Etymology
The word microbiome (from the Greek micro meaning "small" and bíos meaning "life") was first used by J.L. Mohr in 1952 in The Scientific Monthly to mean the microorganisms found in a specific environment.
Definitions
Microbial
communities have commonly been defined as the collection of
microorganisms living together. More specifically, microbial communities
are defined as multi-species assemblages, in which (micro) organisms
interact with each other in a contiguous environment. In 1988, Whipps and colleagues working on the ecology of rhizosphere microorganisms provided the first definition of the term microbiome. They described the microbiome as a combination of the words micro and biome,
naming a "characteristic microbial community" in a "reasonably
well-defined habitat which has distinct physio-chemical properties" as
their "theatre of activity". This definition represents a substantial
advancement of the definition of a microbial community, as it defines a
microbial community with distinct properties and functions and its
interactions with its environment, resulting in the formation of
specific ecological niches.
However, many other microbiome definitions have been published in recent decades. By 2020 the most cited definition was by Lederberg, and described microbiomes within an ecological context as a community of commensal, symbiotic, and pathogenic microorganisms within a body space or other environment. Marchesi and Ravel focused in their definition on the genomes and microbial (and viral) gene expression patterns and proteomes in a given environment and its prevailing biotic and abiotic conditions.
All these definitions imply that general concepts of macro-ecology
could be easily applied to microbe-microbe as well as to microbe-host
interactions. However, the extent to which these concepts, developed for
macro-eukaryotes, can be applied to prokaryotes with their different lifestyles regarding dormancy, variation of phenotype, and horizontal gene transfer
as well as to micro-eukaryotes that is not quite clear. This raises the
challenge of considering an entirely novel body of conceptual ecology
models and theory for microbiome ecology, particularly in relation to
the diverse hierarchies of interactions of microbes with one another and
with the host biotic and abiotic environments. Many current definitions
fail to capture this complexity and describe the term microbiome as
encompassing the genomes of microorganisms only.
| Microbiome definitions
|
|---|
| Definition type
|
Examples
|
| Ecological
|
Definitions based on
ecology describe the microbiome following the concepts derived from the
ecology of multicellular organisms. The main issue here is that the
theories from the macro-ecology do not always fit the rules in the
microbial world.
|
- "A convenient ecological framework in which to examine
biocontrol systems is that of the microbiome. This may be defined as a
characteristic microbial community occupying a reasonably well-defined
habitat which has distinct physio-chemical properties. The term thus not
only refers to the microorganisms involved but also encompasses their
theatre of activity".
- "This term refers to the entire habitat, including the
microorganisms (bacteria, archaea, lower and higher eurkaryotes, and
viruses), their genomes (i.e., genes), and the surrounding environmental
conditions. This definition is based on that of “biome,” the biotic and
abiotic factors of given environments. Others in the field limit the
definition of microbiome to the collection of genes and genomes of
members of a microbiota. It is argued that this is the definition of
metagenome, which combined with the environment constitutes the
microbiome. The microbiome is characterized by the application of one or
combinations of metagenomics, metabonomics, metatranscriptomics, and
metaproteomics combined with clinical or environmental metadata".
- "others use the term microbiome to mean all the microbes of a
community, and in particular, for the plant microbiome, those microbial
communities associated with the plant which can live, thrive, and
interact with different tissues such as roots, shoots, leaves, flowers,
and seeds".
- "Ecological community of commensal, symbiotic and pathogenic microorganisms within a body space or other environment".
|
| Organisms/host-dependent
|
The host-dependent
definitions are based on the microbial interactions with the host. The
main gaps here concern the question whether the microbial-host
interaction data gained from one host can be transferred to another. The
understanding of coevolution and selection in the host-dependent
definitions is also underrepresented.
|
- "A community of microorganisms (such as bacteria, fungi, and
viruses) that inhabit a particular environment and especially the
collection of microorganisms living in or on the human body".
- "Human Microbiome Project (HMP): [...] The Human Microbiome is the
collection of all the microorganisms living in association with the
human body. These communities consist of a variety of microorganisms
including eukaryotes, archaea, bacteria and viruses".
|
| Genomic/ method-driven
|
There is a variety of
microbiome definitions available that are driven by the methods applied.
Mostly, these definitions rely on DNA sequence-based analysis and
describe microbiome as a collective genome of microorganisms in a
specific environment. The main bottleneck here is that every new
available technology will result in a need for a new definition.
|
- "The collective genomes of microorganisms inhabiting a particular environment and especially the human body".
- "The microbiome comprises all of the genetic material within a
microbiota (the entire collection of microorganisms in a specific niche,
such as the human gut). This can also be referred to as the metagenome
of the microbiota".
- "Microbiome is a term that describes the genome of all the
microorganisms, symbiotic and pathogenic, living in and on all
vertebrates. The gut microbiome consists of the collective genome of
microbes inhabiting the gut including bacteria, archaea, viruses, and
fungi".
- "Different approaches to define the population provide different
information. a | Microbiota: 16S rRNA surveys are used to taxonomically
identify the microorganisms in the environment. b | Metagenome: the
genes and genomes of the microbiota, including plasmids, highlighting
the genetic potential of the population. c | Microbiome: the genes and
genomes of the microbiota, as well as the products of the microbiota and
the host environment".
- "Totality of genomes of a microbiota. Often used to describe the
entity of microbial traits (=functions) encoded by a microbiota."
|
| Combined
|
There are some microbiome definitions available that fit several categories with their advantages and disadvantages.
|
- "A microbiome is the ecological community of commensal,
symbiotic, and pathogenic microorganisms that literally share our body
space."
- "The microbiome is the sum of the microbes and their genomic elements in a particular environment".
- "The genes and genomes of the microbiota, as well as the products of the microbiota and the host environment".
|
In 2020, a panel of international experts, organised by the EU-funded MicrobiomeSupport project, published the results of their deliberations on the definition of the microbiome.
The panel was composed of about 40 leaders from diverse microbiome
areas, and about one hundred further experts from around the world
contributed through an online survey. They proposed a definition of the
microbiome based on a revival of what they characterised as the
"compact, clear, and comprehensive description of the term" as
originally provided by Whipps et al. in 1988,
amended with a set of recommendations considering subsequent
technological developments and research findings. They clearly separate
the terms microbiome and microbiota
and provide a comprehensive discussion considering the composition of
microbiota, the heterogeneity and dynamics of microbiomes in time and
space, the stability and resilience of microbial networks, the
definition of core microbiomes, and functionally relevant keystone
species as well as co-evolutionary principles of microbe-host and
inter-species interactions within the microbiome.
The term microbiome encompasses both the
microbiota (community of microorganisms) and their "theatre of activity" (structural elements,
metabolites/
signal molecules, and the surrounding environmental conditions.
The panel extended the Whipps et al. definition, which
contains all important points that are valid even 30 years after its
publication in 1988, by two explanatory paragraphs differentiating the
terms microbiome and microbiota and pronouncing its dynamic character,
as follows:
- The microbiome is defined as a characteristic microbial
community occupying a reasonable well-defined habitat which has distinct
physio-chemical properties. The microbiome not only refers to the
microorganisms involved but also encompass their theatre of activity,
which results in the formation of specific ecological niches. The
microbiome, which forms a dynamic and interactive micro-ecosystem prone
to change in time and scale, is integrated in macro-ecosystems including
eukaryotic hosts, and here crucial for their functioning and health.
- The microbiota consists of the assembly of microorganisms
belonging to different kingdoms (prokaryotes (bacteria, archaea),
eukaryotes (algae, protozoa, fungi etc), while "their theatre of
activity" includes microbial structures, metabolites, mobile genetic
elements (such as transposons, phages, and viruses), and relic DNA
embedded in the environmental conditions of the habitat.
Membership
Microbiota
The microbiota comprises all living members forming the microbiome.
Most microbiome researchers agree bacteria, archaea, fungi, algae, and
small protists should be considered as members of the microbiome. The integration of phages, viruses, plasmids,
and mobile genetic elements is a more controversial issue in the
definition of the microbiome. There is also no clear consensus as to
whether extracellular DNA derived from dead cells, so-called "relic
DNA", belongs to the microbiome. Relic DNA can be up to 40% of the sequenced DNA in soil,
and was up to 33% of the total bacterial DNA on average in a broader
analysis of habitats with the highest proportion of 80% in some samples. Despite its omnipresence and abundance, relic DNA had a minimal effect on estimates of taxonomic and phylogenetic diversity.
When it comes to the use of specific terms, a clear
differentiation between microbiome and microbiota helps to avoid the
controversy concerning the members of a microbiome. Microbiota is usually defined as the assemblage of living microorganisms present in a defined environment. As phages, viruses, plasmids, prions, viroids, and free DNA are usually not considered as living microorganisms, they do not belong to the microbiota.
The term microbiome, as it was originally postulated by Whipps and coworkers,
includes not only the community of the microorganisms but also their
"theatre of activity". The latter involves the whole spectrum of
molecules produced by the microorganisms, including their structural
elements (nucleic acids, proteins, lipids, polysaccharides), metabolites
(signalling molecules, toxins, organic, and inorganic molecules), and
molecules produced by coexisting hosts and structured by the surrounding
environmental conditions. Therefore, all mobile genetic elements, such
as phages, viruses, and "relic" and extracellular DNA, should be
included in the term microbiome, but are not a part of microbiota. The
term microbiome is also sometimes confused with the metagenome. Metagenome is, however, clearly defined as a collection of genomes and genes from the members of a microbiota.
Microbiome studies sometimes focus on the behaviour of a specific
group of microbiota, generally in relation to or justified by a clear
hypothesis. More and more terms like bacteriome, archaeome, mycobiome, or virome
have started appearing in the scientific literature, but these terms do
not refer to biomes (a regional ecosystem with a distinct assemblage of
(micro) organisms, and physical environment often reflecting a certain
climate and soil) as the microbiome itself.
Consequently, it would be better to use the original terms (bacterial,
archaeal, or fungal community). In contrast to the microbiota, which can
be studied separately, the microbiome is always composed by all
members, which interact with each other, live in the same habitat, and
form their ecological niche together. The well-established term virome is derived from virus and genome and is used to describe viral shotgun metagenomes consisting of a collection of nucleic acids associated with a particular ecosystem or holobiont. Viral metagenomes can be suggested as a semantically and scientifically better term.
Networks
Co-occurrence networks help visualising microbial interactions
Nodes usually represent taxa of microorganisms, and edges represent statistically significant associations between nodes.
–––––––––––––––––––––––––––
Testing of the hypotheses resulted from the network analyses is required for a comprehensive study of microbial interactions.
Microbes interact with one another, and these symbiotic interactions
have diverse consequences for microbial fitness, population dynamics,
and functional capacities within the microbiome.
The microbial interactions can either be between microorganisms of the
same species or between different species, genera, families, and domains
of life. The interactions can be separated into positive, negative, and
neutral types. Positive interactions include mutualism, synergism, and commensalism. Negative interactions include amensalism such as predation, parasitism, antagonism,
and competition. Neutral interactions are interactions where there is
no observed effect on the functional capacities or fitness of
interacting species microbial life strategy concepts.
Co-occurrence networks show difference in gut microbiota between herbivorous and carnivorous cichlids
Nodes
coloured according to phylum. The herbivore network has higher
complexity (156 nodes and 339 edges) compared to the carnivore network
(21 nodes and 70 edges).
Microbiomes exhibit different adaptive strategies. Oligotrophs are organisms that can live in an environment offering very low levels of nutrients, particularly carbon.
They are characterised by slow growth, low rates of metabolism, and
generally low population density. Oligotrophic environments include deep
oceanic sediments, caves, glacial and polar ice, deep subsurface soil,
aquifers, ocean waters, and leached soils. In contrast are the copiotrophs, which thrive in much higher carbon concentrations, and do well in high organic substrate conditions such as sewage lagoons.
In addition to oligotrophic and copiotrophic strategists, the competitor–stress tolerator–ruderals framework can influence the outcomes of interactions.
For example, microorganisms competing for the same source can also
benefit from each other when competing for the same compound at
different trophic levels.
Stability of a complex microbial ecosystem depends on trophic
interactions for the same substrate at different concentration levels.
As of 2020 microbial social adaptations in nature have been understudied. Here molecular markers can provide insight into social adaptations by supporting the theories, e.g., of altruists and cheaters in native microbiomes.
Coevolution
- Shift in the understanding of the microbial-host coevolution
from "separation" theories to a holistic approach
In a holistic approach, the hosts and their associated microbiota are assumed to have coevolved with each other
According to the "separation" approach, the microorganisms can be
divided into pathogens, neutral, and symbionts, depending on their
interaction with their host. The coevolution between host and its
associated microbiota may be accordingly described as antagonistic
(based on negative interactions) or mutualistic (based on positive
interactions).
As of 2020, the emergence in publications about opportunistic pathogens and pathobionts
has produced a shift towards a holistic approach in the coevolutions
theory. The holistic approach sees the host and its associated
microbiota as one unit (the so-called holobiont), that coevolves as one entity. According to the holistic approach, holobiont's disease state is linked to dysbiosis, low diversity of the associated microbiota, and their variability: a so-called pathobiome state. The healthy state, on the other hand, is accompanied with eubiosis, high diversity, and uniformity of the respective microbiota.
Types
Marine
- Marine animal host-microbiome relationship
Relationships are generally thought to exist in a symbiotic state,
and are normally exposed to environmental and animal-specific factors
that may cause natural variations. Some events may change the
relationship into a functioning but altered symbiotic state, whereas
extreme stress events may cause dysbiosis or a breakdown of the relationship and interactions.
All animals on Earth form associations with microorganisms, including
protists, bacteria, archaea, fungi, and viruses. In the ocean,
animal–microbial relationships were historically explored in single
host–symbiont systems. However, new explorations into the diversity of
microorganisms associating with diverse marine animal hosts is moving
the field into studies that address interactions between the animal host
and a more multi-member microbiome. The potential for microbiomes to
influence the health, physiology, behavior, and ecology of marine
animals could alter current understandings of how marine animals adapt
to change, and especially the growing climate-related and
anthropogenic-induced changes already impacting the ocean environment.
The microbiomes of diverse marine animals are currently under study, from simplistic organisms including sponges and ctenophores to more complex organisms such as sea squirts and sharks.
The relationship between the Hawaiian bobtail squid and the bioluminescent bacterium Aliivibrio fischeri
is one of the best studied symbiotic relationships in the sea and is a
choice system for general symbiosis research. This relationship has
provided insight into fundamental processes in animal-microbial
symbioses, and especially biochemical interactions and signaling between
the host and bacterium.
The gutless marine oligochaete worm Olavius algarvensis
is another relatively well-studied marine host to microbes. These three
centimetre long worms reside within shallow marine sediments of the
Mediterranean Sea. The worms do not contain a mouth or a digestive or
excretory system, but are instead nourished with the help of a suite of
extracellular bacterial endosymbionts that reside upon coordinated use
of sulfur present in the environment. This system has benefited from some of the most sophisticated 'omics and visualization tools. For example, multi-labeled probing has improved visualization of the microbiome
and transcriptomics and proteomics have been applied to examine
host–microbiome interactions, including energy transfer between the host
and microbes and recognition of the consortia by the worm's innate immune system.
The major strength of this system is that it does offer the ability to
study host–microbiome interactions with a low diversity microbial
consortium, and it also offers a number of host and microbial genomic
resources
Stylophora pistillata coral colony and the bacteria
Endozoicomonas
(Ez) probed cells (yellow) within the tentacles of S. pistillata
residing in aggregates (Ez agg) as well as just outside the aggregate
(b).
Corals
are one of the more common examples of an animal host whose symbiosis
with microalgae can turn to dysbiosis, and is visibly detected as
bleaching. Coral microbiomes have been examined in a variety of studies,
which demonstrate how variations in the ocean environment, most notably
temperature, light, and inorganic nutrients, affect the abundance and
performance of the microalgal symbionts, as well as calcification and physiology of the host.
Studies have also suggested that resident bacteria, archaea, and fungi
additionally contribute to nutrient and organic matter cycling within
the coral, with viruses also possibly playing a role in structuring the
composition of these members, thus providing one of the first glimpses
at a multi-domain marine animal symbiosis. The gammaproteobacterium Endozoicomonas is emerging as a central member of the coral's microbiome, with flexibility in its lifestyle. Given the recent mass bleaching occurring on reefs, corals will likely continue to be a useful and popular system for symbiosis and dysbiosis research.
Sponges
are common members of the ocean's diverse benthic habitats and their
abundance and ability to filter large volumes of seawater have led to
the awareness that these organisms play critical roles in influencing
benthic and pelagic processes in the ocean.
They are one of the oldest lineages of animals, and have a relatively
simple body plan that commonly associates with bacteria, archaea, algal
protists, fungi, and viruses.
Sponge microbiomes are composed of specialists and generalists, and
complexity of their microbiome appears to be shaped by host phylogeny.
Studies have shown that the sponge microbiome contributes to nitrogen
cycling in the oceans, especially through the oxidation of ammonia by
archaea and bacteria. Most recently, microbial symbionts of tropical sponges were shown to produce and store polyphosphate granules, perhaps enabling the host to survive periods of phosphate depletion in oligotrophic marine environments.
The microbiomes of some sponge species do appear to change in community
structure in response to changing environmental conditions, including
temperature and ocean acidification, as well as synergistic impacts.
Collecting a sample of blow from a blue whale using a helicopter drone
Relative abundance of bacterial classes from whale blow, air and seawater samples.
Cetacean microbiomes
can be difficult to assess because of difficulties accessing microbial
samples. For example, many whale species are rare and are deep divers.
There are different techniques for sampling a cetacean's
gut microbiome. The most common is collecting fecal samples from the
environment and taking a probe from the center that is non-contaminated.
The skin
is a barrier protecting marine mammals from the outside world. The
epidermal microbiome on the skin is an indicator of how healthy the
animal is, and is also an ecological indicator of the state of the
surrounding environment. Knowing what the microbiome of the skin of
marine mammals looks like under typical conditions allows understanding
of how these communities different from free microbial communities found
in the sea. Cetaceans
are in danger because they are affected by multiple stress factors
which make them more vulnerable to various diseases. They have been high
susceptibility to airway infections, but little is known about their
respiratory microbiome. Sampling the exhaled breath or "blow" of
cetaceans can provide an assessment of their state of health. Blow is
composed of a mixture of microorganisms and organic material, including lipids, proteins
, and cellular debris derived from the linings of the airways which,
when released into the relatively cooler outdoor air, condense to form a
visible mass of vapor, which can be collected. There are various
methods for collecting exhaled breath samples, one of the most recent is
through the use of aerial drones. This method provides a safer,
quieter, and less invasive alternative and often a cost-effective option
for monitoring fauna and flora. Blow samples are taken to the
laboratory where the respiratory tract microbiota are amplified and
sequenced. The use of aerial drones has been more successful with large
cetaceans due to slow swim speeds and larger blow sizes.
Terrestrial
Plant
Microbiomes in the plant ecosystem
The plant microbiome plays roles in plant health and food production and has received significant attention in recent years. Plants live in association with diverse microbial consortia. These microbes, referred to as the plant's microbiota, live both inside (the endosphere) and outside (the episphere) of plant tissues, and play important roles in the ecology and physiology of plants.
"The core plant microbiome is thought to comprise keystone microbial
taxa that are important for plant fitness and established through
evolutionary mechanisms of selection and enrichment of microbial taxa
containing essential functions genes for the fitness of the plant
holobiont."
Plant microbiomes are shaped by both factors related to the plant
itself, such as genotype, organ, species and health status, as well as
factors related to the plant's environment, such as management, land use
and climate. The health status of a plant has been reported in some studies to be reflected by or linked to its microbiome.
Plant and plant-associated microbiota colonise different niches
on and inside the plant tissue. All the above-ground plant parts
together, called the phyllosphere, are a continuously evolving habitat due to ultraviolet
(UV) radiation and altering climatic conditions. It is primarily
composed of leaves. Below-ground plant parts, mainly roots, are
generally influenced by soil properties. Harmful interactions affect the
plant growth through pathogenic activities of some microbiota members.
On the other hand, beneficial microbial interactions promote plant
growth.
Animal
The mammalian gut microbiome has emerged as a key regulator of host physiology,
and coevolution between host and microbial lineages has played a key
role in the adaptation of mammals to their diverse lifestyles. Diet,
especially herbivory, is an important correlate of microbial diversity in mammals. Most mammalian microbiomes are also strongly correlated with host phylogeny, despite profound shifts in diet. This suggests host factors that themselves change across host
phylogeny, such as gut physiology, play an important role in structuring
the gut microbiomes across mammals. The vertebrate adaptive immune system is even speculated to have evolved as just such a factor for selective maintenance of symbiotic homeostasis.
The importance of phylogeny-correlated factors to the diversity
of vertebrate microbiomes more generally is still poorly understood. Phylosymbiosis, or the observation that more closely related host species have more similar microbiomes, has been described in a number of nonmammalian taxa. Other analyses have found substantial variation in phylosymbiotic signals among mammalian taxa, sometimes with conflicting results. The presence of a robust phylosymbiotic correlation implies that host factors control microbial assembly.
Even if the specific mechanisms are unknown, variation in the strength
or presence of a measurable phylosymbiotic signal across host phylogeny
could prove useful for identifying such mechanisms through comparative
studies. However, as of 2020 most studies have focused on just a few
taxa at a time, and variable methods for both surveying the microbiome
and measuring phylosymbiosis and host specificity (or the restriction of
microbes to specific host lineages) have made generalisations
difficult.
Without broader evolutionary context, it is unclear how
universally conserved patterns of host-microbe phylosymbiosis actually
are. Growing evidence indicates that the strong patterns identified in
mammals are the exception rather than the rule in vertebrates. Meta-analyses of fish and birds
have failed to detect the strength of correlations to diet and
phylogeny reported in mammals. A recent analysis of samples from more
than 100 vertebrate species also found the strength of phylogenetic
correlation to be much higher in mammals than in birds, reptiles,
amphibians, or fish.
It is increasingly appreciated in nonvertebrate animals that
fundamental aspects of the host’s relationship to its symbiotic
community can change drastically between taxa: many insects depend
entirely on microbes for key metabolites, while others seem to be devoid of resident gut microbes.
Human
The human microbiome is the aggregate of all microbiota that reside on or within human tissues and biofluids along with the corresponding anatomical sites in which they reside, including the skin, mammary glands, seminal fluid, uterus, ovarian follicles, lung, saliva, oral mucosa, conjunctiva, biliary tract, and gastrointestinal tract. Types of human microbiota include bacteria, archaea, fungi, protists and viruses. Though micro-animals can also live on the human body, they are typically excluded from this definition. In the context of genomics, the term human microbiome is sometimes used to refer to the collective genomes of resident microorganisms; the term human metagenome has the same meaning.
Humans are colonised by many microorganisms, with approximately the same order of magnitude of non-human cells as human cells. Some microorganisms that colonize humans are commensal, meaning they co-exist without harming or benefiting humans; others have a mutualistic relationship with their human hosts. Conversely, some non-pathogenic microorganisms can harm human hosts via the metabolites they produce, like trimethylamine, which the human body converts to trimethylamine N-oxide via FMO3-mediated oxidation.
Certain microorganisms perform tasks that are known to be useful to the
human host, but the role of most of them is not well understood. Those
that are expected to be present, and that under normal circumstances do
not cause disease, are sometimes deemed normal flora or normal microbiota.
The Human Microbiome Project
(HMP) took on the project of sequencing the genome of the human
microbiota, focusing particularly on the microbiota that normally
inhabit the skin, mouth, nose, digestive tract, and vagina. It reached a milestone in 2012 when it published its initial results.
In 2016, Bashan el al. found that, although different people have
different microbial species and abundance, the dynamics of human
microbial communities is not unique and everyone's microbiota follow the
same rules. The finding has relevance to health and disease, and helps
to understand the way microbial communities behave.
Assessment
Currently available methods for studying microbiomes, so-called multi-omics, range from high throughput isolation (culturomics) and visualization (microscopy), to targeting the taxonomic composition (metabarcoding), or addressing the metabolic potential (metabarcoding of functional genes, metagenomics) to analyze microbial activity (metatranscriptomics, metaproteomics, metabolomics). Based on metagenome data, microbial genomes can be reconstructed. While first metagenome-assembled genomes were reconstructed from environmental samples,
in recent years, several thousands of bacterial genomes were binned
without culturing the organisms behind. For example, 154,723 microbial
genomes of the global human microbiome were reconstructed in 2019 from 9,428 metagenomes.
- Methods for assessing microbial functioning
Methods for assessing microbial functioning
Complex microbiome studies cover various areas, starting from the level of complete microbial cells (
microscopy,
culturomics), followed by the DNA (
single cell genomics,
metabarcoding,
metagenomics), RNA (
metatranscriptomics), protein (
metaproteomics), and metabolites (
metabolomics).
In that order, the focus of the studies shifts from the microbial
potential (learning about available microbiota in the given habitat)
over the metabolic potential (deciphering available genetic material)
towards microbial functioning (e.g., the discovery of the active
metabolic pathways).
Computational modeling of microbiomes has been used to complement experimental methods for investigating microbial function by utilizing multi-omic data to predict complex inter-species and host-species dynamics. A popular in silico method is to combine metabolic network models of microbial taxa present in a community and use a mathematical modeling strategy such as flux balance analysis to predict the metabolic function of the microbial community at a taxon and community-level.
As of 2020, understanding remains limited due to missing links between the massive availability of microbiome DNA sequence data on the one hand and limited availability of microbial isolates needed to confirm metagenomic predictions of gene function on the other hand.
Metagenome data provides a playground for new predictions, yet much
more data is needed to strengthen the links between sequence and
rigorous functional predictions. This becomes obvious when considering
that the replacement of one single amino acid residue by another may lead to a radical functional change, resulting in an incorrect functional assignment to a given gene sequence.
Additionally, cultivation of new strains is needed to help identify the
large fraction of unknown sequences obtained from metagenomics
analyses, which for poorly studied ecosystems can be more than 70%.
Depending on the applied method, even in well-studied microbiomes,
40–70% of the annotated genes in fully sequenced microbial genomes have
no known or predicted function.
As of 2019, 85 of the then established 118 phyla had not had a single
species described, presenting a challenge to understanding prokaryotic functional diversity .
The number of prokaryotic phyla may reach hundreds, and archaeal ones are among the least studied. The growing gap between the diversity of Bacteria and Archaea held in pure culture and those detected by molecular methods has led to the proposal to establish a formal nomenclature for not-yet cultured taxa, primarily based on sequence information. According to this proposal, the concept of Candidatus species
would be extended to the groups of closely related genome sequences,
and their names would be published following established rules of bacterial nomenclature.
Each microbiome system is suited to address different types of
questions based on the culturability of microbes, genetic tractability
of microbes and host (where relevant), ability to maintain system in
laboratory setting, and ability to make host/environment germfree.
- Underlying complexity
Tradeoffs between experimental questions and complexity of microbiome systems
(A) Pairwise interactions between the soil bacteria Bacillus subtilis and Streptomyces spp. are well-suited for characterizing the functions of secondary metabolites in microbial interactions.
(B) The symbiosis between bobtail squid and the marine bacterium Aliivibrio fischeri is fundamental to understanding host and microbial factors that influence colonization.
(C) The use of gnotobiotic mice is crucial for making links between host diet and the effects on specific microbial taxa in a community.





![Shift of paradigm from microbes as unsocial organisms causing diseases to a holistic view of microorganisms as the centre of the One Health Concept interconnecting all areas of human lives.[1]](https://upload.wikimedia.org/wikipedia/commons/3/33/Microbiome_paradigm_shifts.png)
![Co-occurrence networks help visualising microbial interactions Nodes usually represent taxa of microorganisms, and edges represent statistically significant associations between nodes.[1] ––––––––––––––––––––––––––– Testing of the hypotheses resulted from the network analyses is required for a comprehensive study of microbial interactions.[1]](https://upload.wikimedia.org/wikipedia/commons/thumb/2/21/Microbial_interactions_visualized_through_microbial_co-occurrence_networks.webp/615px-Microbial_interactions_visualized_through_microbial_co-occurrence_networks.webp.png)
![Co-occurrence networks show difference in gut microbiota between herbivorous and carnivorous cichlids Nodes coloured according to phylum. The herbivore network has higher complexity (156 nodes and 339 edges) compared to the carnivore network (21 nodes and 70 edges).[82]](https://upload.wikimedia.org/wikipedia/commons/thumb/d/d0/Co-occurrence_networks_showing_difference_in_gut_microbiota_between_herbivorous_and_carnivorous_cichlids.webp/562px-Co-occurrence_networks_showing_difference_in_gut_microbiota_between_herbivorous_and_carnivorous_cichlids.webp.png)
![from "separation" theories to a holistic approach In a holistic approach, the hosts and their associated microbiota are assumed to have coevolved with each other [1]](https://upload.wikimedia.org/wikipedia/commons/thumb/0/05/Shift_of_microbial-host_coevolution_from_separation_theories_to_a_holistic_approach.webp/666px-Shift_of_microbial-host_coevolution_from_separation_theories_to_a_holistic_approach.webp.png)
![Relationships are generally thought to exist in a symbiotic state, and are normally exposed to environmental and animal-specific factors that may cause natural variations. Some events may change the relationship into a functioning but altered symbiotic state, whereas extreme stress events may cause dysbiosis or a breakdown of the relationship and interactions.[88]](https://upload.wikimedia.org/wikipedia/commons/b/be/Marine_animal_host-microbiome_relationships.jpg)

![Collecting a sample of blow from a blue whale using a helicopter drone [118]](https://upload.wikimedia.org/wikipedia/commons/thumb/f/f6/Whale_blow_sampling_with_drone.png/354px-Whale_blow_sampling_with_drone.png)
![Relative abundance of bacterial classes from whale blow, air and seawater samples.[119]](https://upload.wikimedia.org/wikipedia/commons/thumb/b/b5/Cetacean_blow%27s_bacteria.png/426px-Cetacean_blow%27s_bacteria.png)
![Microbiomes in the plant ecosystem [125]](https://upload.wikimedia.org/wikipedia/commons/0/02/Microbiome_in_plant_ecosystem.jpg)
![Principal coordinate analysis of animal gut microbiome data [133]](https://upload.wikimedia.org/wikipedia/commons/thumb/4/48/Principal-coordinate_analysis_of_animal_microbiome_data_sets.jpg/700px-Principal-coordinate_analysis_of_animal_microbiome_data_sets.jpg)
![Methods for assessing microbial functioning Complex microbiome studies cover various areas, starting from the level of complete microbial cells (microscopy, culturomics), followed by the DNA (single cell genomics, metabarcoding, metagenomics), RNA (metatranscriptomics), protein (metaproteomics), and metabolites (metabolomics). In that order, the focus of the studies shifts from the microbial potential (learning about available microbiota in the given habitat) over the metabolic potential (deciphering available genetic material) towards microbial functioning (e.g., the discovery of the active metabolic pathways).[1]](https://upload.wikimedia.org/wikipedia/commons/thumb/1/13/Methods_for_assessing_microbial_functioning.webp/972px-Methods_for_assessing_microbial_functioning.webp.png)
![Tradeoffs between experimental questions and complexity of microbiome systems [171] (A) Pairwise interactions between the soil bacteria Bacillus subtilis and Streptomyces spp. are well-suited for characterizing the functions of secondary metabolites in microbial interactions. (B) The symbiosis between bobtail squid and the marine bacterium Aliivibrio fischeri is fundamental to understanding host and microbial factors that influence colonization. (C) The use of gnotobiotic mice is crucial for making links between host diet and the effects on specific microbial taxa in a community.[171]](https://upload.wikimedia.org/wikipedia/commons/thumb/0/03/Tradeoffs_between_experimental_questions_and_complexity_of_microbiome_systems.jpg/1096px-Tradeoffs_between_experimental_questions_and_complexity_of_microbiome_systems.jpg)
