From Wikipedia, the free encyclopedia
| Pre-eclampsia |
|---|
| Other names | Preeclampsia toxaemia (PET) |
|---|
 |
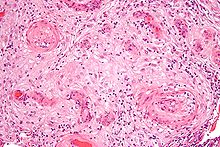
| A micrograph showing hypertrophic decidual vasculopathy, a finding seen in gestational hypertension and pre-eclampsia. H&E stain. |
| Specialty | Obstetrics |
|---|
| Symptoms | High blood pressure, protein in the urine |
|---|
| Complications | Red blood cell breakdown, low blood platelet count, impaired liver function, kidney problems, swelling, shortness of breath due to fluid in the lungs, eclampsia |
|---|
| Usual onset | After 20 weeks of pregnancy |
|---|
| Risk factors | Obesity, prior hypertension, older age, diabetes mellitus |
|---|
| Diagnostic method | BP > 140 mmHg systolic or 90 mmHg diastolic at two separate times |
|---|
| Prevention | Aspirin, calcium supplementation, treatment of prior hypertension |
|---|
| Treatment | Delivery, medications |
|---|
| Medication | Labetalol, methyldopa, magnesium sulfate |
|---|
| Frequency | 2–8% of pregnancies |
|---|
| Deaths | 46,900 hypertensive disorders in pregnancy (2015) |
|---|
Pre-eclampsia is a multi-system disorder specific to pregnancy, characterized by the onset of high blood pressure and often a significant amount of protein in the urine. When it arises, the condition begins after 20 weeks of pregnancy. In severe cases of the disease there may be red blood cell breakdown, a low blood platelet count, impaired liver function, kidney dysfunction, swelling, shortness of breath due to fluid in the lungs, or visual disturbances.
Pre-eclampsia increases the risk of undesirable as well as lethal
outcomes for both the mother and the fetus including preterm labor. If left untreated, it may result in seizures at which point it is known as eclampsia.
Risk factors for pre-eclampsia include obesity, prior hypertension, older age, and diabetes mellitus. It is also more frequent in a woman's first pregnancy and if she is carrying twins. The underlying mechanisms are complex and involve abnormal formation of blood vessels in the placenta amongst other factors. Most cases are diagnosed before delivery, and may be categorized depending on the gestational week at delivery. Commonly, pre-eclampsia continues into the period after delivery, then known as postpartum pre-eclampsia. Rarely, pre-eclampsia may begin in the period after delivery.
While historically both high blood pressure and protein in the urine
were required to make the diagnosis, some definitions also include those
with hypertension and any associated organ dysfunction. Blood pressure is defined as high when it is greater than 140 mmHg systolic or 90 mmHg diastolic at two separate times, more than four hours apart in a woman after twenty weeks of pregnancy. Pre-eclampsia is routinely screened during prenatal care.
Recommendations for prevention include: aspirin in those at high risk, calcium supplementation in areas with low intake, and treatment of prior hypertension with medications. In those with pre-eclampsia, delivery of the baby and placenta is an effective treatment but full recovery can take days or weeks. When delivery becomes recommended depends on how severe the pre-eclampsia and how far along in pregnancy a woman is. Blood pressure medication, such as labetalol and methyldopa, may be used to improve the mother's condition before delivery. Magnesium sulfate may be used to prevent eclampsia in those with severe disease. Bed rest and salt intake have not been found to be useful for either treatment or prevention.
Pre-eclampsia affects 2–8% of pregnancies worldwide. Hypertensive disorders of pregnancy (which include pre-eclampsia) are one of the most common causes of death due to pregnancy. They resulted in 46,900 deaths in 2015. Pre-eclampsia usually occurs after 32 weeks; however, if it occurs earlier it is associated with worse outcomes. Women who have had pre-eclampsia are at increased risk of high blood pressure, heart disease and stroke later in life. Further, those with pre-eclampsia may have a lower risk of breast cancer.
Etymology
The word "eclampsia" is from the Greek term for lightning. The first known description of the condition was by Hippocrates in the 5th century BC.
Signs and symptoms
Edema
(especially in the hands and face) was originally considered an
important sign for a diagnosis of pre-eclampsia. However, because edema
is a common occurrence in pregnancy, its utility as a distinguishing
factor in pre-eclampsia is not high. Pitting edema
(unusual swelling, particularly of the hands, feet, or face, notable by
leaving an indentation when pressed on) can be significant, and should
be reported to a health care provider.
Further, a symptom such as epigastric pain may be misinterpreted
as heartburn. Common features of pre-eclampsia which are screened for
during pre-natal visits include elevated blood pressure and excess
protein in the urine. Additionally, some women may develop severe
headache as a sign of pre-eclampsia.
In general, none of the signs of pre-eclampsia are specific, and even
convulsions in pregnancy are more likely to have causes other than
eclampsia in modern practice.
Diagnosis depends on finding a coincidence of several pre-eclamptic
features, the final proof being their regression within the days and
weeks after delivery.
Causes
There is
no definitive known cause of pre-eclampsia, though it is likely related
to a number of factors. Some of these factors include:
- Abnormal placentation (formation and development of the placenta)
- Immunologic factors
- Prior or existing maternal pathology—pre-eclampsia is seen more at a higher incidence in individuals with pre-existing hypertension, obesity, or antiphospholipid antibody syndrome or those with a history of pre-eclampsia
- Dietary factors, e.g. calcium supplementation in areas where dietary
calcium intake is low has been shown to reduce the risk of
pre-eclampsia
- Environmental factors, e.g. air pollution
Those with long term high blood pressure have a risk 7 to 8 times higher than those without.
Physiologically, research has linked pre-eclampsia to the
following physiologic changes: alterations in the interaction between
the maternal immune response and the placenta, placental injury, endothelial cell injury, altered vascular reactivity, oxidative stress, imbalance among vasoactive substances, decreased intravascular volume, and disseminated intravascular coagulation.
While the exact cause of pre-eclampsia remains unclear, there is
strong evidence that a major cause predisposing a susceptible woman to
pre-eclampsia is an abnormally implanted placenta. This abnormally implanted placenta may result in poor uterine and placental perfusion, yielding a state of hypoxia and increased oxidative stress and the release of anti-angiogenic proteins along with inflammatory mediators into the maternal plasma. A major consequence of this sequence of events is generalized endothelial dysfunction. The abnormal implantation may stem from the maternal immune system's response to the placenta, specifically a lack of established immunological tolerance in pregnancy.
Endothelial dysfunction results in hypertension and many of the other
symptoms and complications associated with pre-eclampsia.
When pre-eclampsia develops in the last weeks of pregnancy or in a
multiple pregnancy, the causation may in some cases, partly be due to a
large placenta outgrowing the capacity of the uterus, eventually leading
to the symptoms of pre-eclampsia.
Abnormal chromosome 19 microRNA cluster (C19MC) impairs extravillus trophoblast cell invasion to the spiral arteries, causing high resistance, low blood flow, and low nutrient supply to the fetus.
Genetic factors
Despite
a lack of knowledge on specific causal mechanisms of pre-eclampsia,
there is strong evidence to suggest it results from both environmental
and heritable factors. A 2005 study showed that women with a
first-degree relative who had a pre-eclamptic birth are twice as likely
to develop it themselves. Furthermore, men related to someone with
affected birth have an increased risk of fathering a pre-eclamptic
pregnancy.
Fetuses affected by pre-eclampsia have a higher chance of later
pregnancy complications including growth restriction, prematurity, and
stillbirth.
The onset of pre-eclampsia is thought to be caused by several
complex interactions between genetics and environmental factors. Our
current understanding of the specifically heritable cause involves an
imbalance of angiogenic factors in the placenta. Angiogenesis
involves the growth of new blood vessels from existing vessels, and an
imbalance during pregnancy can affect the vascularization, growth, and
biological function of the fetus. The irregular expression of these
factors is thought to be controlled by multiple loci on different
chromosomes. Research on the topic has been limited because of the heterogeneous
nature of the disease. Maternal, paternal, and fetal genotypes all play
a role as well as complex epigenetic factors such as whether the
parents smoke, maternal age, sexual cohabitation, and obesity.
Currently, there is very little understanding behind the mechanisms of
these interactions. Due to the polygenic nature of pre-eclampsia, a
majority of the studies that have been conducted thus far on the topic
have utilized genome-wide association studies.
One known effector of pre-eclampsia is the fetal loci FLT1. Located on chromosome 13 in the q12 region, FLT1 codes for Fms-like tyrosine kinase 1, an angiogenic factor expressed in fetal trophoblasts. Angiogenic factors are crucial for vascular growth in the placenta. An FLT1 soluble isoform caused by a splice variant
is sFLT1, which works as an antiangiogenic factor, reducing vascular
growth in the placenta. A healthy, normotensive pregnancy is
characterized by a balance between these factors. However, upregulation
of this variant and overexpression of sFL1 can contribute to endothelial dysfunction. Reduced vascular growth and endothelial dysfunction manifest primarily in maternal symptoms such as renal failure, edema, and seizures. However, these factors can also lead to inadequate oxygen, nutrient, or blood supply to the fetus. Furthermore, in this loci region, several single-nucleotide polymorphisms
(SNPs) have been observed to impact the overexpression of sFL1.
Specifically, SNPs rs12050029 and rs4769613's risk alleles are linked
with low red blood cell counts and carry an increased risk of late-onset
pre-eclampsia.
Patau syndrome,
or Trisomy 13, is also associated with the upregulation of sFLT1 due to
the extra copy of the 13th chromosome. Because of this upregulation of
an antiangiogenic factor, women with trisomy 13 pregnancies often
experience reduced placental vascularization and are at higher risk for
developing pre-eclampsia.
Beyond fetal loci, there have been some maternal loci identified as effectors of pre-eclampsia. Alpha-ketoglutarate-dependent hydroxylase expression on chromosome 16
in the q12 region is also associated with pre-eclampsia. Specifically,
allele rs1421085 heightens the risk of not just pre-eclampsia but also
an increase in BMI and hypertension. This pleiotropy is one of the reasons why these traits are considered to be a risk factor. Furthermore, ZNF831
(zinc finger protein 831) and its loci on chromosome 20q13 were
identified as another significant factor in pre-eclampsia. The risk
allele rs259983 is also associated with both pre-eclampsia and
hypertension, further evidence that the two traits are possibly linked.
While the current understanding suggests that maternal alleles
are the main hereditary cause of pre-eclampsia, paternal loci have also
been implicated. In one study, paternal DLX5 (Distal-Less Homeobox 5) was identified as an imprinted gene. Located on chromosome 7 in the q21 region, DLX5 serves as a transcription factor often linked with the developmental growth of organs.
When paternally inherited, DLX5 and its SNP rs73708843 are shown to
play a role in trophoblast proliferation, affecting vascular growth and
nutrient delivery.
Besides specific loci, several important genetic regulatory
factors contribute to the development of pre-eclampsia. Micro RNAs, or miRNAs,
are noncoding mRNAs that down-regulate posttranscriptional gene
expression through RNA-induced silencing complexes. In the placenta,
miRNAs are crucial for regulating cell growth, angiogenesis, cell
proliferation, and metabolism. These placental-specific miRNAs are clustered in large groups, mainly on chromosomes 14 and 19,
and irregular expression of either is associated with an increased risk
of an affected pregnancy. For instance, miR-16 and miR-29 are vascular endothelial growth factors (VEGFs) and play a role in upregulating sFLT-1. In particular, the overexpression of miRNA miR-210 has been shown to induce hypoxia, which affects spiral artery remodeling, an important part of the pathogenesis of pre-eclampsia.
Risk factors
Known risk factors for pre-eclampsia include:
Pathogenesis
Although
much research into mechanism of pre-eclampsia has taken place, its
exact pathogenesis remains uncertain. Pre-eclampsia is thought to result
from an abnormal placenta, the removal of which ends the disease in
most cases.
During normal pregnancy, the placenta vascularizes to allow for the
exchange of water, gases, and solutes, including nutrients and wastes,
between maternal and fetal circulations.
Abnormal development of the placenta leads to poor placental perfusion.
The placenta of women with pre-eclampsia is abnormal and characterized
by poor trophoblastic invasion.
It is thought that this results in oxidative stress, hypoxia, and the
release of factors that promote endothelial dysfunction, inflammation,
and other possible reactions.
In normal early embryonic development, the outer epithelial layer
contains cytotrophoblast cells, a stem cell type found in the
trophoblast that later differentiates into the fetal placenta. These
cells differentiate into many placental cells types, including
extravillous trophoblast cells. Extravillous trophoblast cells are an
invasive cell type which remodel the maternal spiral arteries by
replacing the maternal epithelium and smooth muscle lining the spiral
arteries, thus causing and maintaining spiral artery dilation. This
prevents maternal vasoconstriction in the spiral arteries and allows for
continued blood and nutrient supply to the growing fetus with low
resistance and high blood flow.
The clinical manifestations of pre-eclampsia are associated with
general endothelial dysfunction, including vasoconstriction and
end-organ ischemia. Implicit in this generalized endothelial dysfunction may be an imbalance of angiogenic and anti-angiogenic factors. Both circulating and placental levels of soluble fms-like tyrosine kinase-1 (sFlt-1) are higher in women with pre-eclampsia than in women with normal pregnancy. sFlt-1 is an anti-angiogenic protein that antagonizes vascular endothelial growth factor (VEGF) and placental growth factor (PIGF), both of which are proangiogenic factors. Soluble endoglin
(sEng) has also been shown to be elevated in women with pre-eclampsia
and has anti-angiogenic properties, much like sFlt-1 does.
Both sFlt-1 and sEng are upregulated in all pregnant women to
some extent, supporting the idea that hypertensive disease in pregnancy
is a normal pregnancy adaptation gone awry. As natural killer cells are
intimately involved in placentation and placentation involves a degree
of maternal immune tolerance
for a foreign placenta, it is not surprising that the maternal immune
system might respond more negatively to the arrival of some placentae
under certain circumstances, such as a placenta which is more invasive
than normal. Initial maternal rejection of the placental cytotrophoblasts may be the cause of the inadequately remodeled spiral arteries
in those cases of pre-eclampsia associated with shallow implantation,
leading to downstream hypoxia and the appearance of maternal symptoms in
response to upregulated sFlt-1 and sEng.
Oxidative stress may also play an important part in the
pathogenesis of pre-eclampsia. The main source of reactive oxygen
species (ROS) is the enzyme xanthine oxidase
(XO) and this enzyme mainly occurs in the liver. One hypothesis is that
the increased purine catabolism from placental hypoxia results in
increased ROS production in the maternal liver and release into the
maternal circulation that causes endothelial cell damage.
Abnormalities in the maternal immune system and insufficiency of gestational immune tolerance seem to play major roles in pre-eclampsia. One of the main differences found in pre-eclampsia is a shift toward Th1 responses and the production of IFN-γ. The origin of IFN-γ is not clearly identified and could be the natural killer cells of the uterus, the placental dendritic cells modulating responses of T helper cells, alterations in synthesis of or response to regulatory molecules, or changes in the function of regulatory T cells in pregnancy.
Aberrant immune responses promoting pre-eclampsia may also be due to an
altered fetal allorecognition or to inflammatory triggers. It has been documented that fetal cells such as fetal erythroblasts as well as cell-free fetal DNA
are increased in the maternal circulation in women who develop
pre-eclampsia. These findings have given rise to the hypothesis that
pre-eclampsia is a disease process by which a placental lesion such as
hypoxia allows increased fetal material into the maternal circulation,
that in turn leads to an immune response and endothelial damage, and that ultimately results in pre-eclampsia and eclampsia.
One hypothesis for vulnerability to pre-eclampsia is the maternal-fetal conflict between the maternal organism and fetus.
After the first trimester trophoblasts enter the spiral arteries of the
mother to alter the spiral arteries and thereby gain more access to
maternal nutrients. Occasionally there is impaired trophoblast invasion that results in inadequate alterations to the uterine spiral arteries.
It is hypothesized that the developing embryo releases biochemical
signals that result in the woman developing hypertension and
pre-eclampsia so that the fetus can benefit from a greater amount of
maternal circulation of nutrients due to increased blood flow to the
impaired placenta.
This results in a conflict between maternal and fetal fitness and
survival because the fetus is invested in only its survival and fitness
while the mother is invested in this and subsequent pregnancies.
Another evolutionary hypothesis for vulnerability to
pre-eclampsia is the idea of ensuring pair-bonding between the mother
and father and paternal investment in the fetus.
Researchers posit that pre-eclampsia is an adaptation for the mother to
terminate investment in a fetus that might have an unavailable father,
as determined by repeated semen exposure of the father to the mother.
Various studies have shown that women who frequently had exposure to
partners' semen before conception had a reduced risk of pre-eclampsia.
Also, subsequent pregnancies by the same father had a reduced risk of
pre-eclampsia while subsequent pregnancies by a different father had a
higher risk of developing pre-eclampsia.
In pre-eclampsia, abnormal expression of chromosome 19 microRNA
cluster (C19MC) in placental cell lines reduces extravillus trophoblast
migration.
Specific microRNAs in this cluster which might cause abnormal spiral
artery invasion include miR-520h, miR-520b, and 520c-3p. This impairs
extravillus trophoblast cells invasion to the maternal spiral arteries,
causing high resistance and low blood flow and low nutrient supply to
the fetus. There is tentative evidence that vitamin supplementation can decrease the risk.
Immune factors may also play a role.
Diagnosis
Testing for pre-eclampsia is recommended throughout pregnancy via measuring a woman's blood pressure.
Diagnostic criteria
Pre-eclampsia is diagnosed when a pregnant woman develops:
- Blood pressure ≥140 mmHg systolic or ≥90 mmHg diastolic on two
separate readings taken at least four to six hours apart after 20 weeks'
gestation in an individual with previously normal blood pressure.
- In a woman with essential hypertension beginning before 20 weeks'
gestational age, the diagnostic criteria are an increase in systolic
blood pressure (SBP) of ≥30 mmHg or an increase in diastolic blood
pressure (DBP) of ≥15 mmHg.
- Proteinuria
≥ 0.3 grams (300 mg) or more of protein in a 24-hour urine sample or a
SPOT urinary protein to creatinine ratio ≥0.3 or a urine dipstick
reading of 1+ or greater (dipstick reading should only be used if other
quantitative methods are not available).
Suspicion for pre-eclampsia should be maintained in any pregnancy
complicated by elevated blood pressure, even in the absence of
proteinuria. Ten percent of individuals with other signs and symptoms of
pre-eclampsia and 20% of individuals diagnosed with eclampsia show no
evidence of proteinuria. In the absence of proteinuria, the presence of new-onset hypertension (elevated blood pressure) and the new onset of one or more of the following is suggestive of the diagnosis of pre-eclampsia:
Pre-eclampsia is a progressive disorder and these signs of organ
dysfunction are indicative of severe pre-eclampsia. A systolic blood
pressure ≥160 or diastolic blood pressure ≥110 and/or proteinuria >5g
in a 24-hour period is also indicative of severe pre-eclampsia. Clinically, individuals with severe pre-eclampsia may also present epigastric/right upper quadrant abdominal pain, headaches, and vomiting. Severe pre-eclampsia is a significant risk factor for intrauterine fetal death.
A rise in baseline blood pressure (BP) of 30 mmHg
systolic or 15 mmHg diastolic, while not meeting the absolute criteria
of 140/90, is important to note but is not considered diagnostic.
Predictive tests
There
have been many assessments of tests aimed at predicting pre-eclampsia,
though no single biomarker is likely to be sufficiently predictive of
the disorder.
Predictive tests that have been assessed include those related to
placental perfusion, vascular resistance, kidney dysfunction, endothelial dysfunction, and oxidative stress. Examples of notable tests include:
- Doppler ultrasonography
of the uterine arteries to investigate for signs of inadequate
placental perfusion. This test has a high negative predictive value
among those individuals with a history of prior pre-eclampsia.
- Elevations in serum uric acid (hyperuricemia) is used by some to "define" pre-eclampsia, though it has been found to be a poor predictor of the disorder. Elevated levels in the blood (hyperuricemia) are likely due to reduced uric acid clearance secondary to impaired kidney function.
- Angiogenic proteins such as vascular endothelial growth factor (VEGF) and placental growth factor (PIGF) and anti-angiogenic proteins such as soluble fms-like tyrosine kinase-1
(sFlt-1) have shown promise for potential clinical use in diagnosing
pre-eclampsia, though evidence is insufficient to recommend a clinical
use for these markers.
A recent study, ASPRE, known to be the largest multi-country
prospective trial, has reported a significant performance in identifying
pregnant women at high risk of pre-eclampsia yet during the first
trimester of pregnancy. Utilizing a combination of maternal history,
mean arterial blood pressure, intrauterine Doppler and PlGF measurement,
the study has shown a capacity to identify more than 75% of the women
that will develop pre-eclampsia, allowing early intervention to prevent
development of later symptoms. This approach is now officially recommended by the International Federation of Gynecologists & Obstetricians (FIGO),
However this model particularly predict pre-eclampsia with onset before
34 weeks' of gestation, while prediction of pre-eclampsia with later
onset remains challenging.
- Recent studies have shown that looking for podocytes
(specialized cells of the kidney) in the urine has the potential to aid
in the prediction of pre-eclampsia. Studies have demonstrated that
finding podocytes in the urine may serve as an early marker of and
diagnostic test for pre-eclampsia.
Differential diagnosis
Pre-eclampsia
can mimic and be confused with many other diseases, including chronic
hypertension, chronic renal disease, primary seizure disorders,
gallbladder and pancreatic disease, immune or thrombotic thrombocytopenic purpura, antiphospholipid syndrome and hemolytic-uremic syndrome.
It must be considered a possibility in any pregnant woman beyond 20
weeks of gestation. It is particularly difficult to diagnose when
pre-existing conditions such as hypertension are present. Women with acute fatty liver of pregnancy
may also present with elevated blood pressure and protein in the urine,
but differ by the extent of liver damage. Other disorders that can
cause high blood pressure include thyrotoxicosis, pheochromocytoma, and drug misuse.
Prevention
Preventive
measures against pre-eclampsia have been heavily studied. Because the
pathogenesis of pre-eclampsia is not completely understood, prevention
remains a complex issue. Some currently accepted recommendations are:
Diet
Supplementation with a balanced protein and energy diet does not appear to reduce the risk of pre-eclampsia. Further, there is no evidence that changing salt intake has an effect.
Supplementation with antioxidants such as vitamin C, D and E has no effect on pre-eclampsia incidence; therefore, supplementation with vitamins C, E, and D is not recommended for reducing the risk of pre-eclampsia.
Calcium
supplementation of at least 1 gram per day is recommended during
pregnancy as it prevents pre-eclampsia where dietary calcium intake is
low, especially for those at high risk. Higher selenium level is associated with lower incidence of pre-eclampsia. Higher cadmium level is associated with higher incidence of pre-eclampsia.
Aspirin
Taking aspirin is associated with a 1 to 5% reduction in pre-eclampsia and a 1 to 5% reduction in premature births in women at high risk. The World Health Organization
recommends low-dose aspirin for the prevention of pre-eclampsia in
women at high risk and recommends it be started before 20 weeks of
pregnancy. The United States Preventive Services Task Force recommends a low-dose regimen for women at high risk beginning in the 12th week. Benefits are less if started after 16 weeks. Since 2018 the American College of Obstetricians and Gynecologists has recommended low-dose aspirin therapy as standard preventive treatment for pre-eclampsia. There is a reported problem of its efficacy when combined with paracetamol. Supplementation of aspirin with L-Arginine has shown favourable results.
The study ASPRE, besides its efficacy in identifying women
suspected to develop pre-eclampsia, has also been able to demonstrate a
strong drop in the rate of early pre-eclampsia (-82%) and preterm
pre-eclampsia (-62%). The efficacy of aspirin is due to screening to
identify high risk women, adjusted prophylaxis dosage (150 mg/day),
timing of the intake (bedtime) and must start before week 16 of
pregnancy.
Physical activity
There is insufficient evidence to recommend either exercise or strict bedrest as preventive measures of pre-eclampsia.
Smoking cessation
In low-risk pregnancies, the association between cigarette smoking
and a reduced risk of pre-eclampsia has been consistent and
reproducible across epidemiologic studies. High-risk pregnancies (those
with pregestational diabetes, chronic hypertension, history of
pre-eclampsia in a previous pregnancy, or multifetal gestation) showed
no significant protective effect. The reason for this discrepancy is not
definitively known; research supports speculation that the underlying
pathology increases the risk of pre-eclampsia to such a degree that any
measurable reduction of risk due to smoking is masked.
However, the damaging effects of smoking on overall health and
pregnancy outcomes outweighs the benefits in decreasing the incidence of
pre-eclampsia. It is recommended that smoking be stopped prior to, during and after pregnancy.
Immune modulation
Some studies have suggested the importance of a woman's gestational immunological tolerance
to her baby's father, as the baby and father share genetics. There is
tentative evidence that ongoing exposure either by vaginal or oral sex
to the same semen that resulted in the pregnancy decreases the risk of
pre-eclampsia.
As one early study described, "although pre-eclampsia is a disease of
first pregnancies, the protective effect of multiparity is lost with
change of partner".
The study also concluded that although women with changing partners are
strongly advised to use condoms to prevent sexually transmitted
diseases, "a certain period of sperm exposure within a stable relation,
when pregnancy is aimed for, is associated with protection against
pre-eclampsia".
Several other studies have since investigated the decreased
incidence of pre-eclampsia in women who had received blood transfusions
from their partner, those with long preceding histories of sex without
barrier contraceptives, and in women who had been regularly performing oral sex.
Having already noted the importance of a woman's immunological
tolerance to her baby's paternal genes, several Dutch reproductive
biologists decided to take their research a step further. Consistent
with the fact that human immune systems tolerate things better when they
enter the body via the mouth, the Dutch researchers conducted a series
of studies that confirmed a surprisingly strong correlation between a
diminished incidence of pre-eclampsia and a woman's practice of oral
sex, and noted that the protective effects were strongest if she
swallowed her partner's semen. A team from the University of Adelaide has also investigated to see if men who have fathered pregnancies which have ended in miscarriage or pre-eclampsia had low seminal levels of critical immune modulating factors such as TGF-beta.
The team has found that certain men, dubbed "dangerous males", are
several times more likely to father pregnancies that would end in either
pre-eclampsia or miscarriage.
Among other things, most of the "dangerous males" seemed to lack
sufficient levels of the seminal immune factors necessary to induce immunological tolerance in their partners.
As the theory of immune intolerance as a cause of pre-eclampsia
has become accepted, women with repeated pre-eclampsia, miscarriages, or
in vitro fertilization
failures could potentially be administered key immune factors such as
TGF-beta along with the father's foreign proteins, possibly either
orally, as a sublingual spray, or as a vaginal gel to be applied onto
the vaginal wall before intercourse.
Treatment
The
definitive treatment for pre-eclampsia is the delivery of the baby and
placenta, but danger to the mother persists after delivery, and full
recovery can take days or weeks. The timing of delivery should balance the desire for optimal outcomes for the baby while reducing risks for the mother. The severity of disease and the maturity of the baby are primary considerations.
These considerations are situation-specific and management will vary
with situation, location, and institution. Treatment can range from
expectant management to expedited delivery by induction of labor or Caesarean section,
in addition to medications. Important in management is the assessment
of the mother's organ systems, management of severe hypertension, and
prevention and treatment of eclamptic seizures.
Separate interventions directed at the baby may also be necessary. Bed
rest has not been found to be useful and is thus not routinely
recommended.
Blood pressure
The World Health Organization recommends that women with severe hypertension during pregnancy should receive treatment with anti-hypertensive agents. Severe hypertension is generally considered systolic BP of at least 160 or diastolic BP of at least 110. Evidence does not support the use of one anti-hypertensive over another.
The choice of which agent to use should be based on the prescribing
clinician's experience with a particular agent, its cost, and its
availability. Diuretics are not recommended for prevention of pre-eclampsia and its complications. Labetalol, hydralazine and nifedipine are commonly used antihypertensive agents for hypertension in pregnancy. ACE inhibitors and angiotensin receptor blockers are contraindicated as they affect fetal development.
The goal of treatment of severe hypertension in pregnancy is to
prevent cardiovascular, kidney, and cerebrovascular complications.
The target blood pressure has been proposed to be 140–160 mmHg systolic
and 90–105 mmHg diastolic, although values are variable.
Prevention of eclampsia
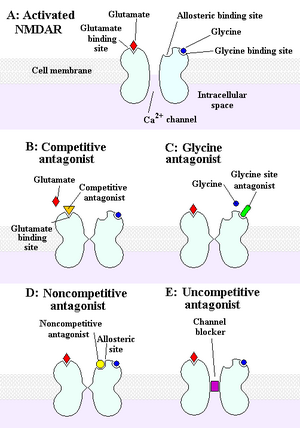
The intrapartum and postpartum administration of magnesium sulfate is recommended in severe pre-eclampsia for the prevention of eclampsia. Further, magnesium sulfate is recommended for the treatment of eclampsia over other anticonvulsants. Magnesium sulfate acts by interacting with NMDA receptors.
Epidemiology
Pre-eclampsia affects approximately 2–8% of all pregnancies worldwide.
The incidence of pre-eclampsia has risen in the U.S. since the 1990s,
possibly as a result of increased prevalence of predisposing disorders,
such as chronic hypertension, diabetes, and obesity.
Pre-eclampsia is one of the leading causes of maternal and perinatal morbidity and mortality worldwide.
Nearly one-tenth of all maternal deaths in Africa and Asia and
one-quarter in Latin America are associated with hypertensive diseases
in pregnancy, a category that encompasses pre-eclampsia.
Pre-eclampsia is much more common in women who are pregnant for the first time.
Women who have previously been diagnosed with pre-eclampsia are also
more likely to experience pre-eclampsia in subsequent pregnancies. Pre-eclampsia is also more common in women who have pre-existing hypertension, obesity, diabetes, autoimmune diseases such as lupus, various inherited thrombophilias such as Factor V Leiden, renal disease, multiple gestation (twins or multiple birth), and advanced maternal age. Women who live at high altitude are also more likely to experience pre-eclampsia. Pre-eclampsia is also more common in some ethnic groups (e.g.
African-Americans, Sub-Saharan Africans, Latin Americans, African
Caribbeans, and Filipinos).
Change of paternity in a subsequent pregnancy has been implicated as
affecting risk, except in those with a family history of hypertensive
pregnancy.
Eclampsia
is a major complication of pre-eclampsia. Eclampsia affects 0.56 per
1,000 pregnant women in developed countries and almost 10 to 30 times as
many women in low-income countries as in developed countries.
Complications
Complications of pre-eclampsia can affect both the mother and the fetus. Acutely, pre-eclampsia can be complicated by eclampsia, the development of HELLP syndrome, hemorrhagic or ischemic stroke, liver damage and dysfunction, acute kidney injury, and acute respiratory distress syndrome (ARDS).
Pre-eclampsia is also associated with increased frequency of Caesarean section, preterm delivery, and placental abruption.
Furthermore, an elevation in blood pressure can occur in some
individuals in the first week postpartum attributable to volume
expansion and fluid mobilization. Fetal complications include fetal growth restriction and potential fetal or perinatal death.
Long-term, an individual with pre-eclampsia is at increased risk for recurrence of pre-eclampsia in subsequent pregnancies.
Eclampsia
Eclampsia is the development of new convulsions
in a pre-eclamptic patient that may not be attributed to other causes.
It is a sign that the underlying pre-eclamptic condition is severe and
is associated with high rates of perinatal and maternal morbidity and
mortality.
Warning symptoms for eclampsia in an individual with current
pre-eclampsia may include headaches, visual disturbances, and right
upper quadrant or epigastric abdominal pain, with a headache being the
most consistent symptom. During pregnancy brisk or hyperactive reflexes are common, however ankle clonus is a sign of neuromuscular irritability that usually reflects severe pre-eclampsia and also can precede eclampsia. Magnesium sulfate is used to prevent convulsions in cases of severe pre-eclampsia.
HELLP Syndrome
HELLP syndrome is defined as hemolysis (microangiopathic), elevated liver enzymes (liver dysfunction), and low platelets (thrombocytopenia). This condition may occur in 10–20% of patients with severe pre-eclampsia and eclampsia
and is associated with increased maternal and fetal morbidity and
mortality. In 50% of instances, HELLP syndrome develops preterm, while
20% of cases develop in late gestation and 30% during the post-partum
period.
Long term
Preeclampsia
predisposes for future cardiovascular disease and a history of
preeclampsia/eclampsia doubles the risk for cardiovascular mortality
later in life.
Other risks include stroke, chronic hypertension, kidney disease and venous thromboembolism. Preeclampsia and cardiovascular disease share many risk factors such
as age, elevated BMI, family history and certain chronic diseases.
It seems that pre-eclampsia does not increase the risk of cancer.
Lowered blood supply to the fetus in pre-eclampsia causes lowered nutrient supply, which could result in intrauterine growth restriction (IUGR) and low birth weight.
The fetal origins hypothesis states that fetal undernutrition is linked
with coronary heart disease later in adult life due to disproportionate
growth.
Because pre-eclampsia leads to a mismatch between the maternal
energy supply and fetal energy demands, pre-eclampsia can lead to IUGR
in the developing fetus.
Infants with IUGR are prone to have poor neuronal development and in
increased risk for adult disease according to the Barker hypothesis.
Associated adult diseases of the fetus due to IUGR include, but are not
limited to, coronary artery disease (CAD), type 2 diabetes mellitus (T2DM), cancer, osteoporosis, and various psychiatric illnesses.
The risk of pre-eclampsia and development of placental
dysfunction has also been shown to be recurrent cross-generationally on
the maternal side and most likely on the paternal side. Fetuses born to
mothers who were born small for gestational age
(SGA) were 50% more likely to develop pre-eclampsia while fetuses born
to both SGA parents were three-fold more likely to develop pre-eclampsia
in future pregnancies.
History
The word "eclampsia" is from the Greek term for lightning. The first known description of the condition was by Hippocrates in the 5th century BC.
An outdated medical term for pre-eclampsia is toxemia of pregnancy, a term that originated in the mistaken belief that the condition was caused by toxins.