From Wikipedia, the free encyclopedia
Sterilization refers to any process that removes, kills, or deactivates all forms of life (particularly microorganisms such as fungi, bacteria, spores, and unicellular eukaryotic organisms) and other biological agents such as prions present in or on a specific surface, object, or fluid. Sterilization can be achieved through various means, including heat, chemicals, irradiation, high pressure, and filtration. Sterilization is distinct from disinfection, sanitization, and pasteurization,
in that those methods reduce rather than eliminate all forms of life
and biological agents present. After sterilization, an object is
referred to as being sterile or aseptic.
Organisms growing on an
agar plate
Applications
Foods
One of the first steps toward modernized sterilization was made by Nicolas Appert,
who discovered that application of heat over a suitable period slowed
the decay of foods and various liquids, preserving them for safe
consumption for a longer time than was typical. Canning of foods is an extension of the same principle and has helped to reduce food borne illness ("food poisoning"). Other methods of sterilizing foods include food irradiation and high pressure (pascalization).
Medicine and surgery
Apparatus to sterilize surgical instruments (1914–1918)
In general, surgical instruments and medications that enter an already aseptic part of the body (such as the bloodstream, or penetrating the skin) must be sterile. Examples of such instruments include scalpels, hypodermic needles, and artificial pacemakers. This is also essential in the manufacture of parenteral pharmaceuticals.
Preparation of injectable medications and intravenous solutions for fluid replacement therapy requires not only sterility but also well-designed containers to prevent entry of adventitious agents after initial product sterilization.
Most medical and surgical devices used in healthcare facilities are made of materials that are able to go under steam sterilization.
However, since 1950, there has been an increase in medical devices and
instruments made of materials (e.g., plastics) that require
low-temperature sterilization. Ethylene oxide
gas has been used since the 1950s for heat- and moisture-sensitive
medical devices. Within the past 15 years, a number of new,
low-temperature sterilization systems (e.g., vaporized hydrogen peroxide, peracetic acid immersion, ozone) have been developed and are being used to sterilize medical devices.
Spacecraft
There are strict international rules to protect the contamination of Solar System bodies
from biological material from Earth. Standards vary depending on both
the type of mission and its destination; the more likely a planet is
considered to be habitable, the stricter the requirements are.
Many components of instruments used on spacecraft cannot
withstand very high temperatures, so techniques not requiring excessive
temperatures are used as tolerated, including heating to at least 120 °C
(248 °F), chemical sterilization, oxidization, ultraviolet, and
irradiation.
Quantification
The
aim of sterilization is the reduction of initially present
microorganisms or other potential pathogens. The degree of sterilization
is commonly expressed by multiples of the decimal reduction time, or D-value, denoting the time needed to reduce the initial number  to one tenth (
to one tenth ( ) of its original value. Then the number of microorganisms
) of its original value. Then the number of microorganisms  after sterilization time
after sterilization time  is given by:
is given by:
 .
.
The D-value is a function of sterilization conditions and varies with the type of microorganism, temperature, water activity, pH etc.. For steam sterilization (see below) typically the temperature, in degrees Celsius, is given as an index.
Theoretically, the likelihood of the survival of an individual
microorganism is never zero. To compensate for this, the overkill method
is often used. Using the overkill method, sterilization is performed by
sterilizing for longer than is required to kill the bioburden present on or in the item being sterilized. This provides a sterility assurance level (SAL) equal to the probability of a non-sterile unit.
For high-risk applications, such as medical devices and injections, a sterility assurance level of at least 10−6 is required by the United States Food and Drug Administration (FDA).
Heat
Steam
Steam sterilization, also known as moist heat sterilization, uses heated saturated steam under pressure to inactivate or kill microorganisms via denaturation of macromolecules, primarily proteins. This method is a faster process than dry heat sterilization. Steam sterilization is performed using an autoclave,
sometimes called a converter or steam sterilizer. The article is placed
in the autoclave chamber, which is then sealed and heated using
pressurized steam to a temperature set point for a defined period of
time. Steam sterilization cycles can be categorized as either pre-vacuum
or gravity displacement. Gravity displacement cycles rely on the lower
density of the injected steam to force cooler, denser air out of the
chamber drain.
In comparison, pre-vacuum cycles draw a vacuum in the chamber to remove
cool dry air prior to injecting saturated steam, resulting in faster
heating and shorter cycle times. Typical steam sterilization cycles are
between 3 and 30 minutes at 121–134 °C (250–273 °F) at 100 kPa (15 psi),
but adjustments may be made depending on the bioburden of the article being sterilized, its resistance (D-value)
to steam sterilization, the article's heat tolerance, and the required
sterility assurance level. Following the completion of a cycle, liquids
in a pressurized autoclave must be cooled slowly to avoid boiling over
when the pressure is released. This may be achieved by gradually
depressurizing the sterilization chamber and allowing liquids to
evaporate under a negative pressure, while cooling the contents.
Proper autoclave treatment will inactivate all resistant bacterial spores in addition to fungi, bacteria, and viruses, but is not expected to eliminate all prions,
which vary in their resistance. For prion elimination, various
recommendations state 121–132 °C (250–270 °F) for 60 minutes or 134 °C
(273 °F) for at least 18 minutes. The 263K scrapie prion is inactivated relatively quickly by such sterilization procedures; however, other strains of scrapie, and strains of Creutzfeldt-Jakob disease (CKD) and bovine spongiform encephalopathy (BSE) are more resistant. Using mice as test animals, one experiment showed that heating BSE positive brain tissue at 134–138 °C (273–280 °F) for 18 minutes resulted in only a 2.5 log decrease in prion infectivity.
Most autoclaves have meters and charts that record or display
information, particularly temperature and pressure as a function of
time. The information is checked to ensure that the conditions required
for sterilization have been met. Indicator tape
is often placed on the packages of products prior to autoclaving, and
some packaging incorporates indicators. The indicator changes color when
exposed to steam, providing a visual confirmation.
Biological indicators
can also be used to independently confirm autoclave performance. Simple
biological indicator devices are commercially available, based on
microbial spores. Most contain spores of the heat-resistant microbe Geobacillus stearothermophilus (formerly Bacillus stearothermophilus),
which is extremely resistant to steam sterilization. Biological
indicators may take the form of glass vials of spores and liquid media,
or as spores on strips of paper inside glassine
envelopes. These indicators are placed in locations where it is
difficult for steam to reach to verify that steam is penetrating there.
For autoclaving, cleaning is critical. Extraneous biological
matter or grime may shield organisms from steam penetration. Proper
cleaning can be achieved through physical scrubbing, sonication, ultrasound, or pulsed air.
Pressure cooking and canning is analogous to autoclaving, and when performed correctly renders food sterile.
To sterilize waste materials that are chiefly composed of liquid, a purpose-built effluent decontamination system can be utilized. These devices can function using a variety of sterilants, although using heat via steam is most common.
Dry
Dry
heat was the first method of sterilization and is a longer process than
moist heat sterilization. The destruction of microorganisms through the
use of dry heat is a gradual phenomenon. With longer exposure to lethal
temperatures, the number of killed microorganisms increases. Forced
ventilation of hot air can be used to increase the rate at which heat is
transferred to an organism and reduce the temperature and amount of
time needed to achieve sterility. At higher temperatures, shorter
exposure times are required to kill organisms. This can reduce
heat-induced damage to food products.
The standard setting for a hot air oven is at least two hours at
160 °C (320 °F). A rapid method heats air to 190 °C (374 °F) for 6
minutes for unwrapped objects and 12 minutes for wrapped objects.
Dry heat has the advantage that it can be used on powders and other
heat-stable items that are adversely affected by steam (e.g. it does not
cause rusting of steel objects).
Flaming
Flaming is done to inoculation loops and straight-wires in microbiology labs for streaking. Leaving the loop in the flame of a Bunsen burner or alcohol burner
until it glows red ensures that any infectious agent is inactivated.
This is commonly used for small metal or glass objects, but not for
large objects (see Incineration
below). However, during the initial heating, infectious material may be
sprayed from the wire surface before it is killed, contaminating nearby
surfaces and objects. Therefore, special heaters have been developed
that surround the inoculating loop with a heated cage, ensuring that
such sprayed material does not further contaminate the area. Another
problem is that gas flames may leave carbon or other residues on the
object if the object is not heated enough. A variation on flaming is to
dip the object in a 70% or more concentrated solution of ethanol, then briefly touch the object to a Bunsen burner flame. The ethanol will ignite and burn off rapidly, leaving less residue than a gas flame
Incineration
Incineration
is a waste treatment process that involves the combustion of organic
substances contained in waste materials. This method also burns any
organism to ash. It is used to sterilize medical and other biohazardous waste
before it is discarded with non-hazardous waste. Bacteria incinerators
are mini furnaces that incinerate and kill off any microorganisms that
may be on an inoculating loop or wire.
Tyndallization
Named after John Tyndall, Tyndallization
is an obsolete and lengthy process designed to reduce the level of
activity of sporulating bacteria that are left by a simple boiling water
method. The process involves boiling for a period (typically 20
minutes) at atmospheric pressure, cooling, incubating for a day, and
then repeating the process a total of three to four times. The
incubation periods are to allow heat-resistant spores surviving the
previous boiling period to germinate to form the heat-sensitive
vegetative (growing) stage, which can be killed by the next boiling
step. This is effective because many spores are stimulated to grow by
the heat shock. The procedure only works for media that can support
bacterial growth, and will not sterilize non-nutritive substrates like
water. Tyndallization is also ineffective against prions.
Glass bead sterilizers
Glass
bead sterilizers work by heating glass beads to 250 °C (482 °F).
Instruments are then quickly doused in these glass beads, which heat the
object while physically scraping contaminants off their surface. Glass
bead sterilizers were once a common sterilization method employed in dental offices as well as biological laboratories, but are not approved by the U.S. Food and Drug Administration (FDA) and Centers for Disease Control and Prevention (CDC) to be used as a sterilizers since 1997. They are still popular in European and Israeli dental practices, although there are no current evidence-based guidelines for using this sterilizer.
Chemical sterilization

Chemicals are also used for sterilization. Heating provides a
reliable way to rid objects of all transmissible agents, but it is not
always appropriate if it will damage heat-sensitive materials such as
biological materials, fiber optics, electronics, and many plastics.
In these situations chemicals, either in a gaseous or liquid form, can
be used as sterilants. While the use of gas and liquid chemical
sterilants avoids the problem of heat damage, users must ensure that the
article to be sterilized is chemically compatible with the sterilant
being used and that the sterilant is able to reach all surfaces that
must be sterilized (typically cannot penetrate packaging). In addition,
the use of chemical sterilants poses new challenges for workplace safety,
as the properties that make chemicals effective sterilants usually make
them harmful to humans. The procedure for removing sterilant residue
from the sterilized materials varies depending on the chemical and
process that is used.
Ethylene oxide
Ethylene oxide
(EO, EtO) gas treatment is one of the common methods used to sterilize,
pasteurize, or disinfect items because of its wide range of material
compatibility. It is also used to process items that are sensitive to
processing with other methods, such as radiation (gamma, electron beam,
X-ray), heat (moist or dry), or other chemicals. Ethylene oxide
treatment is the most common chemical sterilization method, used for
approximately 70% of total sterilizations, and for over 50% of all disposable medical devices.
Ethylene oxide treatment is generally carried out between 30 and 60 °C (86 and 140 °F) with relative humidity above 30% and a gas concentration between 200 and 800 mg/l. Typically, the process lasts for several hours. Ethylene oxide is highly effective, as it penetrates all porous materials,
and it can penetrate through some plastic materials and films. Ethylene
oxide kills all known microorganisms, such as bacteria (including
spores), viruses, and fungi (including yeasts and moulds), and is
compatible with almost all materials even when repeatedly applied. It is
flammable, toxic, and carcinogenic;
however, only with a reported potential for some adverse health effects
when not used in compliance with published requirements. Ethylene oxide
sterilizers and processes require biological validation after sterilizer installation, significant repairs or process changes.
The traditional process consists of a preconditioning phase (in a
separate room or cell), a processing phase (more commonly in a vacuum
vessel and sometimes in a pressure rated vessel), and an aeration phase
(in a separate room or cell) to remove EO residues and lower by-products
such as ethylene chlorohydrin (EC or ECH) and, of lesser importance, ethylene glycol
(EG). An alternative process, known as all-in-one processing, also
exists for some products whereby all three phases are performed in the
vacuum or pressure rated vessel. This latter option can facilitate
faster overall processing time and residue dissipation.
The most common EO processing method is the gas chamber method. To benefit from economies of scale,
EO has traditionally been delivered by filling a large chamber with a
combination of gaseous EO either as pure EO, or with other gases used as
diluents; diluents include chlorofluorocarbons (CFCs), hydrochlorofluorocarbons (HCFCs), and carbon dioxide.
Ethylene oxide is still widely used by medical device manufacturers. Since EO is explosive at concentrations above 3%, EO was traditionally supplied with an inert carrier gas, such as a CFC or HCFC. The use of CFCs or HCFCs as the carrier gas was banned because of concerns of ozone depletion. These halogenated hydrocarbons
are being replaced by systems using 100% EO, because of regulations and
the high cost of the blends. In hospitals, most EO sterilizers use
single-use cartridges because of the convenience and ease of use
compared to the former plumbed gas cylinders of EO blends.
It is important to adhere to patient and healthcare personnel
government specified limits of EO residues in and/or on processed
products, operator exposure after processing, during storage and
handling of EO gas cylinders, and environmental emissions produced when
using EO.
The U.S. Occupational Safety and Health Administration (OSHA) has set the permissible exposure limit (PEL) at 1 ppm – calculated as an eight-hour time-weighted average (TWA) – and 5 ppm as a 15-minute excursion limit (EL). The National Institute for Occupational Safety and Health's (NIOSH) immediately dangerous to life and health limit (IDLH) for EO is 800 ppm. The odor threshold is around 500 ppm,
so EO is imperceptible until concentrations are well above the OSHA
PEL. Therefore, OSHA recommends that continuous gas monitoring systems
be used to protect workers using EO for processing.
Nitrogen dioxide
Nitrogen dioxide (NO2)
gas is a rapid and effective sterilant for use against a wide range of
microorganisms, including common bacteria, viruses, and spores. The
unique physical properties of NO2 gas allow for sterilant
dispersion in an enclosed environment at room temperature and
atmospheric pressure. The mechanism for lethality is the degradation of DNA in the spore core through nitration of the phosphate backbone, which kills the exposed organism as it absorbs NO2. This degradations occurs at even very low concentrations of the gas. NO2 has a boiling point of 21 °C (70 °F) at sea level, which results in a relatively highly saturated vapour pressure at ambient temperature. Because of this, liquid NO2 may be used as a convenient source for the sterilant gas. Liquid NO2 is often referred to by the name of its dimer, dinitrogen tetroxide (N2O4). Additionally, the low levels of concentration required, coupled with the high vapour pressure, assures that no condensation
occurs on the devices being sterilized. This means that no aeration of
the devices is required immediately following the sterilization cycle. NO2 is also less corrosive than other sterilant gases, and is compatible with most medical materials and adhesives.
The most-resistant organism (MRO) to sterilization with NO2 gas is the spore of Geobacillus stearothermophilus, which is the same MRO for both steam and hydrogen peroxide sterilization processes. The spore form of G. stearothermophilus has been well characterized over the years as a biological indicator in sterilization applications. Microbial inactivation of G. stearothermophilus with NO2 gas proceeds rapidly in a log-linear
fashion, as is typical of other sterilization processes. Noxilizer,
Inc. has commercialized this technology to offer contract sterilization
services for medical devices at its Baltimore, Maryland (U.S.) facility.
This has been demonstrated in Noxilizer’s lab in multiple studies and
is supported by published reports from other labs. These same properties
also allow for quicker removal of the sterilant and residual gases
through aeration of the enclosed environment. The combination of rapid
lethality and easy removal of the gas allows for shorter overall cycle
times during the sterilization (or decontamination) process and a lower
level of sterilant residuals than are found with other sterilization
methods.
Eniware, LLC has developed a portable, power-free sterilizer that uses no electricity, heat or water.
The 25 liter unit makes sterilization of surgical instruments possible
for austere forward surgical teams, in health centers throughout the
world with intermittent or no electricity and in disaster relief and
humanitarian crisis situations. The four hour cycle uses a single use
gas generation ampoule and a disposable scrubber to remove nitrogen
dioxide gas.
Ozone
Ozone
is used in industrial settings to sterilize water and air, as well as a
disinfectant for surfaces. It has the benefit of being able to oxidize
most organic matter. On the other hand, it is a toxic and unstable gas
that must be produced on-site, so it is not practical to use in many
settings.
Ozone offers many advantages as a sterilant gas; ozone is a very
efficient sterilant because of its strong oxidizing properties (E=2.076 vs SHE)
capable of destroying a wide range of pathogens, including prions,
without the need for handling hazardous chemicals since the ozone is
generated within the sterilizer from medical-grade oxygen. The high reactivity of ozone means that waste ozone can be destroyed by passing over a simple catalyst
that reverts it to oxygen and ensures that the cycle time is relatively
short. The disadvantage of using ozone is that the gas is very reactive
and very hazardous. The NIOSH's immediately dangerous to life and
health limit (IDLH) for ozone is 5 ppm, 160 times smaller than the 800 ppm IDLH for ethylene oxide. NIOSH and OSHA has set the PEL for ozone at 0.1 ppm, calculated as an eight-hour
time-weighted average. The sterilant gas manufacturers include many
safety features in their products but prudent practice is to provide
continuous monitoring of exposure to ozone, in order to provide a rapid
warning in the event of a leak. Monitors for determining workplace
exposure to ozone are commercially available.
Glutaraldehyde and formaldehyde
Glutaraldehyde and formaldehyde solutions (also used as fixatives)
are accepted liquid sterilizing agents, provided that the immersion
time is sufficiently long. To kill all spores in a clear liquid can take
up to 22 hours with glutaraldehyde and even longer with formaldehyde.
The presence of solid particles may lengthen the required period or
render the treatment ineffective. Sterilization of blocks of tissue can
take much longer, due to the time required for the fixative to
penetrate. Glutaraldehyde and formaldehyde are volatile,
and toxic by both skin contact and inhalation. Glutaraldehyde has a
short shelf-life (<2 weeks), and is expensive. Formaldehyde is less
expensive and has a much longer shelf-life if some methanol is added to inhibit polymerization to paraformaldehyde,
but is much more volatile. Formaldehyde is also used as a gaseous
sterilizing agent; in this case, it is prepared on-site by
depolymerization of solid paraformaldehyde. Many vaccines, such as the
original Salk polio vaccine, are sterilized with formaldehyde.
Hydrogen peroxide
Hydrogen peroxide, in both liquid and as vaporized hydrogen peroxide (VHP), is another chemical sterilizing agent. Hydrogen peroxide is a strong oxidant,
which allows it to destroy a wide range of pathogens. Hydrogen peroxide
is used to sterilize heat- or temperature-sensitive articles, such as
rigid endoscopes.
In medical sterilization, hydrogen peroxide is used at higher
concentrations, ranging from around 35% up to 90%. The biggest advantage
of hydrogen peroxide as a sterilant is the short cycle time. Whereas
the cycle time for ethylene oxide may be 10 to 15 hours, some modern
hydrogen peroxide sterilizers have a cycle time as short as 28 minutes.
Drawbacks of hydrogen peroxide include material compatibility, a
lower capability for penetration and operator health risks. Products
containing cellulose, such as paper, cannot be sterilized using VHP and
products containing nylon may become brittle. The penetrating ability of hydrogen peroxide is not as good as ethylene oxide
and so there are limitations on the length and diameter of the lumen of
objects that can be effectively sterilized. Hydrogen peroxide is a
primary irritant and the contact of the liquid solution with skin will
cause bleaching or ulceration
depending on the concentration and contact time. It is relatively
non-toxic when diluted to low concentrations, but is a dangerous
oxidizer at high concentrations (> 10% w/w). The vapour is also
hazardous, primarily affecting the eyes and respiratory system. Even
short term exposures can be hazardous and NIOSH has set the IDLH at 75
ppm,
less than one tenth the IDLH for ethylene oxide (800 ppm). Prolonged
exposure to lower concentrations can cause permanent lung damage and
consequently, OSHA has set the permissible exposure limit to 1.0 ppm,
calculated as an eight-hour time-weighted average.
Sterilizer manufacturers go to great lengths to make their products
safe through careful design and incorporation of many safety features,
though there are still workplace exposures of hydrogen peroxide from gas
sterilizers documented in the FDA MAUDE database.
When using any type of gas sterilizer, prudent work practices should
include good ventilation, a continuous gas monitor for hydrogen peroxide
and good work practices and training.
Vaporized hydrogen peroxide (VHP) is used to sterilize large enclosed and sealed areas, such as entire rooms and aircraft interiors.
Although toxic, VHP breaks down in a short time to water and oxygen.
Peracetic acid
Peracetic acid (0.2%) is a recognized sterilant by the FDA for use in sterilizing medical devices such as endoscopes.
Peracetic acid, which is also known as peroxyacetic acid, is a chemical
compound often used in disinfectants such as sanitizers. It is most
commonly produced by the reaction of acetic acid and hydrogen peroxide
with each other by using an acid catalyst. Peracetic acid is never sold
in unstabilized solutions which is why it is considered to be
environmentally friendly. Peracetic acid is a colorless liquid and the molecular formula of peracetic acid is C2H4O3 or CH3COOOH.
More recently, peracetic acid is being used throughout the world as
more people are using fumigation to decontaminate surfaces to reduce the
risk of Covid-19 and other diseases.
Potential for chemical sterilization of prions
Prions are highly resistant to chemical sterilization. Treatment with aldehydes,
such as formaldehyde, have actually been shown to increase prion
resistance. Hydrogen peroxide (3%) for one hour was shown to be
ineffective, providing less than 3 logs (10−3) reduction in contamination. Iodine, formaldehyde, glutaraldehyde, and peracetic acid also fail this test (one hour treatment). Only chlorine, phenolic compounds, guanidinium thiocyanate,
and sodium hydroxide reduce prion levels by more than 4 logs; chlorine
(too corrosive to use on certain objects) and sodium hydroxide are the
most consistent. Many studies have shown the effectiveness of sodium
hydroxide.
Radiation sterilization
Sterilization can be achieved using electromagnetic radiation, such as ultraviolet light, X-rays and gamma rays, or irradiation by subatomic particles such as by electron beams. Electromagnetic or particulate radiation can be energetic enough to ionize atoms or molecules (ionizing radiation), or less energetic (non-ionizing radiation).
Non-ionizing radiation sterilization
Ultraviolet light irradiation (UV, from a germicidal lamp) is useful for sterilization of surfaces and some transparent objects. Many objects that are transparent to visible light absorb UV. UV irradiation is routinely used to sterilize the interiors of biological safety cabinets
between uses, but is ineffective in shaded areas, including areas under
dirt (which may become polymerized after prolonged irradiation, so that
it is very difficult to remove). It also damages some plastics, such as polystyrene foam if exposed for prolonged periods of time.
Ionizing radiation sterilization
Efficiency illustration of the different radiation technologies (electron beam, X-ray, gamma rays)
The safety of irradiation facilities is regulated by the International Atomic Energy Agency of the United Nations and monitored by the different national Nuclear Regulatory Commissions
(NRC). The radiation exposure accidents that have occurred in the past
are documented by the agency and thoroughly analyzed to determine the
cause and improvement potential. Such improvements are then mandated to
retrofit existing facilities and future design.
Gamma radiation is very penetrating, and is commonly used for sterilization of disposable medical equipment, such as syringes, needles, cannulas and IV sets, and food. It is emitted by a radioisotope, usually cobalt-60 (60Co) or caesium-137 (137Cs), which have photon energies of up to 1.3 and 0.66 MeV, respectively.
Use of a radioisotope requires shielding for the safety of the
operators while in use and in storage. With most designs, the
radioisotope is lowered into a water-filled source storage pool, which
absorbs radiation and allows maintenance personnel to enter the
radiation shield. One variant keeps the radioisotope under water at all
times and lowers the product to be irradiated in the water in
hermetically-sealed bells; no further shielding is required for such
designs. Other uncommonly used designs use dry storage, providing
movable shields that reduce radiation levels in areas of the irradiation
chamber. An incident in Decatur, Georgia, US, where water-soluble caesium-137 leaked into the source storage pool, requiring NRC intervention
has led to use of this radioisotope being almost entirely discontinued
in favour of the more costly, non-water-soluble cobalt-60. Cobalt-60
gamma photons have about twice the energy, and hence greater penetrating range, of caesium-137-produced radiation.
Electron beam processing is also commonly used for sterilization. Electron beams
use an on-off technology and provide a much higher dosing rate than
gamma or X-rays. Due to the higher dose rate, less exposure time is
needed and thereby any potential degradation to polymers is reduced.
Because electrons
carry a charge, electron beams are less penetrating than both gamma and
X-rays. Facilities rely on substantial concrete shields to protect
workers and the environment from radiation exposure.
High-energy X-rays (produced by bremsstrahlung) allow irradiation of large packages and pallet
loads of medical devices. They are sufficiently penetrating to treat
multiple pallet loads of low-density packages with very good dose
uniformity ratios. X-ray sterilization does not require chemical or
radioactive material: high-energy X-rays are generated at high intensity
by an X-ray generator that does not require shielding when not in use. X-rays are generated by bombarding a dense material (target) such as tantalum or tungsten with high-energy electrons, in a process known as bremsstrahlung conversion. These systems are energy-inefficient, requiring much more electrical energy than other systems for the same result.
Irradiation with X-rays, gamma rays, or electrons does not make materials radioactive, because the energy used is too low. Generally an energy of at least 10 MeV is needed to induce radioactivity in a material. Neutrons
and very high-energy particles can make materials radioactive, but have
good penetration, whereas lower energy particles (other than neutrons)
cannot make materials radioactive, but have poorer penetration.
Sterilization by irradiation with gamma rays may however affect material properties.
Irradiation is used by the United States Postal Service to sterilize mail in the Washington, D.C. area. Some foods (e.g. spices and ground meats) are sterilized by irradiation.
Subatomic particles may be more or less penetrating and may be
generated by a radioisotope or a device, depending upon the type of
particle.
Sterile filtration
Fluids that would be damaged by heat, irradiation or chemical sterilization, such as drug solution, can be sterilized by microfiltration using membrane filters. This method is commonly used for heat labile pharmaceuticals and protein solutions in medicinal drug processing. A microfilter with pore size of usually 0.22 µm will effectively remove microorganisms. Some staphylococcal species have, however, been shown to be flexible enough to pass through 0.22 µm filters. In the processing of biologics, viruses must be removed or inactivated, requiring the use of nanofilters with a smaller pore size (20–50 nm).
Smaller pore sizes lower the flow rate, so in order to achieve higher
total throughput or to avoid premature blockage, pre-filters might be
used to protect small pore membrane filters. Tangential flow filtration (TFF) and alternating tangential flow (ATF) systems also reduce particulate accumulation and blockage.
Membrane filters used in production processes are commonly made from materials such as mixed cellulose ester or polyethersulfone
(PES). The filtration equipment and the filters themselves may be
purchased as pre-sterilized disposable units in sealed packaging or must
be sterilized by the user, generally by autoclaving at a temperature
that does not damage the fragile filter membranes. To ensure proper
functioning of the filter, the membrane filters are integrity tested
post-use and sometimes before use. The nondestructive integrity test
assures the filter is undamaged and is a regulatory requirement. Typically, terminal pharmaceutical sterile filtration is performed inside of a cleanroom to prevent contamination.
Preservation of sterility
Instruments that have undergone sterilization can be maintained in such condition by containment in sealed packaging until use.
Aseptic technique is the act of maintaining sterility during procedures.
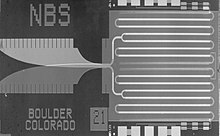
































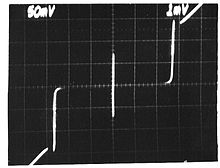
![{\displaystyle {\frac {\partial \varphi }{\partial t}}=2\pi [K_{J}V(t)]={\frac {2\pi }{\Phi _{0}}}V(t)\,.}](https://wikimedia.org/api/rest_v1/media/math/render/svg/c6a4d19b714169b822a4cda059cb835a84303f25)