Newspaper headlines from around the world about polio vaccine tests (13 April 1955)
Public health is "the science and art of preventing disease, prolonging life and promoting human health through organized efforts and informed choices of society, organizations, public and private, communities and individuals". Analyzing the health of a population and the threats is the basis for public health.
The "public" in question can be as small as a handful of people, an
entire village or it can be as large as several continents, in the case
of a pandemic.
"Health" takes into account physical, mental and social well-being. It
is not merely the absence of disease or infirmity, according to the World Health Organization. Public health is interdisciplinary. For example, epidemiology, biostatistics and health services are all relevant. Environmental health, community health, behavioral health, health economics, public policy, mental health and occupational safety, gender issues in health, sexual and reproductive health are other important subfields.
Public health aims to improve the quality of life through prevention and treatment of disease, including mental health. This is done through the surveillance of cases and health indicators, and through the promotion of healthy behaviors. Common public health initiatives include promoting handwashing and breastfeeding, delivery of vaccinations, suicide prevention and distribution of condoms to control the spread of sexually transmitted diseases.
Modern public health practice requires multidisciplinary teams of public health workers and professionals. Teams might include epidemiologists, biostatisticians, medical assistants, public health nurses, midwives, medical microbiologists, economists, sociologists, geneticists and data managers. Depending on the need environmental health officers or public health inspectors, bioethicists, and even veterinarians, gender experts, sexual and reproductive health specialists might be called on.
Access to health care and public health initiatives are difficult challenges in developing countries. Public health infrastructures are still forming in those countries.
Background
The focus of a public health intervention is to prevent and manage diseases, injuries and other health conditions through surveillance of cases and the promotion of healthy behaviors, communities and environments. Many diseases are preventable through simple, non-medical methods. For example, research has shown that the simple act of handwashing with soap can prevent the spread of many contagious diseases. In other cases, treating a disease or controlling a pathogen can be vital to preventing its spread to others, either during an outbreak of infectious disease or through contamination of food or water supplies. Public health communications programs, vaccination programs and distribution of condoms
are examples of common preventive public health measures. Measures such
as these have contributed greatly to the health of populations and
increases in life expectancy.
Public health plays an important role in disease prevention
efforts in both the developing world and in developed countries through
local health systems and non-governmental organizations. The World Health Organization (WHO) is the international agency that coordinates and acts on global public health
issues. Most countries have their own government public health
agencies, sometimes known as ministries of health, to respond to
domestic health issues. For example, in the United States, the front line of public health initiatives are state and local health departments. The United States Public Health Service (PHS), led by the Surgeon General of the United States, and the Centers for Disease Control and Prevention, headquartered in Atlanta, are involved with several international health activities, in addition to their national duties. In Canada, the Public Health Agency of Canada is the national agency responsible for public health, emergency preparedness and response, and infectious and chronic disease control and prevention. The Public health system in India is managed by the Ministry of Health & Family Welfare of the government of India with state-owned health care facilities.
Current practice
Public health programs
There's a push and pull, as you know, between cheap alternatives for industry and public health concerns...We're always looking at retrospectively what the data shows...Unfortunately, for example, take tobacco: It took 50, 60 years of research before policy catches up with what the science is showing— Laura Anderko, professor at Georgetown University and director of the Mid-Atlantic Center for Children's Health and the Environment commenting on public health practices in response to proposal to ban chlorpyrifos pesticide.
Most governments recognize the importance of public health programs
in reducing the incidence of disease, disability, and the effects of
aging and other physical and mental health conditions. However, public
health generally receives significantly less government funding compared
with medicine. Public health programs providing vaccinations have made strides in promoting health, including the eradication of smallpox, a disease that plagued humanity for thousands of years.
Three former directors of the Global Smallpox Eradication Programme read the news that smallpox had been globally eradicated, 1980
The World Health Organization (WHO) identifies core functions of public health programs including:
- providing leadership on matters critical to health and engaging in partnerships where joint action is needed;
- shaping a research agenda and stimulating the generation, translation and dissemination of valuable knowledge;
- setting norms and standards and promoting and monitoring their implementation;
- articulating ethical and evidence-based policy options;
- monitoring the health situation and assessing health trends.
In particular, public health surveillance programs can:
- serve as an early warning system for impending public health emergencies;
- document the impact of an intervention, or track progress towards specified goals; and
- monitor and clarify the epidemiology of health problems, allow priorities to be set, and inform health policy and strategies.
- diagnose, investigate, and monitor health problems and health hazards of the community
Public health surveillance has led to the identification and
prioritization of many public health issues facing the world today,
including HIV/AIDS, diabetes, waterborne diseases, zoonotic diseases, and antibiotic resistance leading to the reemergence of infectious diseases such as tuberculosis. Antibiotic resistance, also known as drug resistance, was the theme of World Health Day 2011.
Although the prioritization of pressing public health issues is
important, Laurie Garrett argues that there are following consequences.
When foreign aid is funnelled into disease-specific programs, the
importance of public health in general is disregarded. This public
health problem of stovepiping is thought to create a lack of funds to combat other existing diseases in a given country.
For example, the WHO reports that at least 220 million people
worldwide suffer from diabetes. Its incidence is increasing rapidly, and
it is projected that the number of diabetes deaths will double by the
year 2030. In a June 2010 editorial in the medical journal The Lancet, the authors opined that "The fact that type 2 diabetes, a largely preventable disorder, has reached epidemic proportion is a public health humiliation." The risk of type 2 diabetes is closely linked with the growing problem of obesity.
The WHO’s latest estimates as of June 2016 highlighted that globally
approximately 1.9 billion adults were overweight in 2014, and 41 million
children under the age of five were overweight in 2014.
The United States is the leading country with 30.6% of its population
being obese. Mexico follows behind with 24.2% and the United Kingdom
with 23%. Once considered a problem in high-income countries, it is now
on the rise in low-income countries, especially in urban settings. Many
public health programs are increasingly dedicating attention and
resources to the issue of obesity, with objectives to address the
underlying causes including healthy diet and physical exercise.
Some programs and policies associated with public health
promotion and prevention can be controversial. One such example is
programs focusing on the prevention of HIV transmission through safe sex campaigns and needle-exchange programs. Another is the control of tobacco smoking. Changing smoking behavior requires long-term strategies, unlike the fight against communicable diseases, which usually takes a shorter period for effects to be observed. Many nations have implemented major initiatives to cut smoking, such as increased taxation and bans on smoking in some or all public places. Proponents
argue by presenting evidence that smoking is one of the major killers,
and that therefore governments have a duty to reduce the death rate,
both through limiting passive (second-hand) smoking and by providing fewer opportunities for people to smoke. Opponents
say that this undermines individual freedom and personal
responsibility, and worry that the state may be emboldened to remove
more and more choice in the name of better population health overall.
Simultaneously, while communicable diseases have historically ranged uppermost as a global health priority, non-communicable diseases and the underlying behavior-related risk factors have been at the bottom. This is changing, however, as illustrated by the United Nations hosting its first General Assembly Special Summit on the issue of non-communicable diseases in September 2011.
Many health problems are due to maladaptive personal behaviors. From an evolutionary psychology perspective, over consumption of novel substances that are harmful is due to the activation of an evolved reward system
for substances such as drugs, tobacco, alcohol, refined salt, fat, and
carbohydrates. New technologies such as modern transportation also cause
reduced physical activity. Research has found that behavior is more
effectively changed by taking evolutionary motivations into
consideration instead of only presenting information about health
effects. The marketing industry has long known the importance of
associating products with high status and attractiveness to others.
Films are increasingly being recognized as a public health tool. In fact, film festivals and competitions have been established to specifically promote films about health.
Conversely, it has been argued that emphasizing the harmful and
undesirable effects of tobacco smoking on other persons and imposing
smoking bans in public places have been particularly effective in
reducing tobacco smoking.
Applications in health care
As
well as seeking to improve population health through the implementation
of specific population-level interventions, public health contributes
to medical care by identifying and assessing population needs for health care services, including:
- Assessing current services and evaluating whether they are meeting the objectives of the health care system
- Ascertaining requirements as expressed by health professionals, the public and other stakeholders
- Identifying the most appropriate interventions
- Considering the effect on resources for proposed interventions and assessing their cost-effectiveness
- Supporting decision making in health care and planning health services including any necessary changes.
- Informing, educating, and empowering people about health issues
Implementing effective improvement strategies
To
improve public health, one important strategy is to promote modern
medicine and scientific neutrality to drive the public health policy and
campaign, which is recommended by Armanda Solorzana, through a case
study of the Rockefeller Foundation's hookworm campaign in Mexico in the
1920s. Soloranza argues that public health policy can't concern only
politics or economics. Political concerns can lead government officials
to hide the real numbers of people affected by disease in their
regions, such as upcoming elections. Therefore, scientific neutrality in
making public health policy is critical; it can ensure treatment needs
are met regardless of political and economic conditions.
The history of public health care clearly shows the global effort to improve health care for all.
However, in modern-day medicine, real, measurable change has not been
clearly seen, and critics argue that this lack of improvement is due to
ineffective methods that are being implemented. As argued by Paul E.
Farmer, structural interventions could possibly have a large impact, and
yet there are numerous problems as to why this strategy has yet to be
incorporated into the health system. One of the main reasons that he
suggests could be the fact that physicians are not properly trained to
carry out structural interventions, meaning that the ground level health
care professionals cannot implement these improvements. While
structural interventions can not be the only area for improvement, the
lack of coordination between socioeconomic factors and health care for
the poor could be counterproductive, and end up causing greater inequity
between the health care services received by the rich and by the poor.
Unless health care is no longer treated as a commodity, global public
health will ultimately not be achieved.
This being the case, without changing the way in which health care is
delivered to those who have less access to it, the universal goal of
public health care cannot be achieved.
Another reason why measurable changes may not be noticed in
public health is because agencies themselves may not be measuring their
programs' efficacy. Perrault et al.
analyzed over 4,000 published objectives from Community Health
Improvement Plans (CHIPs) of 280 local accredited and non-accredited
public health agencies in the U.S., and found that the majority of
objectives - around two-thirds - were focused on achieving agency
outputs (e.g., developing communication plans, installing sidewalks,
disseminating data to the community). Only about one-third focused on
seeking measurable changes in the populations they serve (i.e., changing
people's knowledge, attitudes, behaviors). What this research showcases
is that if agencies are only focused on accomplishing tasks (i.e.,
outputs) and do not have a focus on measuring actual changes in their
populations with the activities they perform, it should not be
surprising when measurable changes are not reported. Perrault et al. advocate for public health agencies to work with those in the discipline of Health Communication
to craft objectives that are measurable outcomes, and to assist
agencies in developing tools and methods to be able to track more
proximal changes in their target populations (e.g., knowledge and
attitude shifts) that may be influenced by the activities the agencies
are performing.
Public Health 2.0
Public Health 2.0
is a movement within public health that aims to make the field more
accessible to the general public and more user-driven. The term is used
in three senses. In the first sense, "Public Health 2.0" is similar to "Health 2.0"
and describes the ways in which traditional public health practitioners
and institutions are reaching out (or could reach out) to the public
through social media and health blogs.
In the second sense, "Public Health 2.0" describes public health
research that uses data gathered from social networking sites, search
engine queries, cell phones, or other technologies.
A recent example is the proposal of statistical framework that utilizes
online user-generated content (from social media or search engine
queries) to estimate the impact of an influenza vaccination campaign in
the UK.
In the third sense, "Public Health 2.0" is used to describe public health activities that are completely user-driven. An example is the collection and sharing of information about environmental radiation levels after the March 2011 tsunami in Japan. In all cases, Public Health 2.0 draws on ideas from Web 2.0, such as crowdsourcing, information sharing, and user-centred design.
While many individual healthcare providers have started making their
own personal contributions to "Public Health 2.0" through personal
blogs, social profiles, and websites, other larger organizations, such
as the American Heart Association
(AHA) and United Medical Education (UME), have a larger team of
employees centered around online driven health education, research, and
training. These private organizations recognize the need for free and
easy to access health materials often building libraries of educational
articles.
Low- and middle-income countries
Emergency Response Team in Burma after Cyclone Nargis in 2008
There is a great disparity in access to health care and public health initiatives between developed nations and developing nations. In the developing world, public health infrastructures are still forming. There may not be enough trained health workers,
monetary resources or, in some cases, sufficient knowledge to provide
even a basic level of medical care and disease prevention.
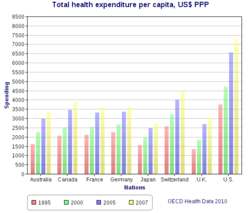
As a result, a large majority of disease and mortality in the
developing world results from and contributes to extreme poverty. For
example, many African governments spend less than US$10 per person per year on health care, while, in the United States, the federal government
spent approximately US$4,500 per capita in 2000. However, expenditures
on health care should not be confused with spending on public health.
Public health measures may not generally be considered "health care" in
the strictest sense. For example, mandating the use of seat belts in
cars can save countless lives and contribute to the health of a
population, but typically money spent enforcing this rule would not
count as money spent on health care.
Large parts of the world remained plagued by largely preventable
or treatable infectious diseases. In addition to this however, many low- and middle-income countries
are also experiencing an epidemiological shift and polarization in
which populations are now experiencing more of the effects of chronic
diseases as life expectancy increases with, the poorer communities being
heavily affected by both chronic and infectious diseases. Another major public health concern in the developing world is poor maternal and child health, exacerbated by malnutrition and poverty. The WHO reports that a lack of exclusive breastfeeding during the first six months of life contributes to over a million avoidable child deaths each year. Intermittent preventive therapy aimed at treating and preventing malaria episodes among pregnant women and young children is one public health measure in endemic countries.
Each day brings new front-page headlines about public health: emerging infectious diseases such as SARS, rapidly making its way from China (see Public health in China) to Canada, the United States and other geographically distant countries; reducing inequities in health care access through publicly funded health insurance programs; the HIV/AIDS pandemic and its spread from certain high-risk groups to the general population in many countries, such as in South Africa; the increase of childhood obesity and the concomitant increase in type II diabetes among children; the social, economic and health effects of adolescent pregnancy; and the public health challenges related to natural disasters such as the 2004 Indian Ocean tsunami, 2005's Hurricane Katrina in the United States and the 2010 Haiti earthquake.
Since the 1980s, the growing field of population health has broadened the focus of public health from individual behaviors and risk factors to population-level issues such as inequality,
poverty, and education. Modern public health is often concerned with
addressing determinants of health across a population. There is a
recognition that our health is affected by many factors including where
we live, genetics, our income, our educational status and our social
relationships; these are known as "social determinants of health".
The upstream drivers such as environment, education, employment,
income, food security, housing, social inclusion and many others effect
the distribution of health between and within populations and are often
shaped by policy.
A social gradient in health runs through society. The poorest generally
suffer the worst health, but even the middle classes will generally
have worse health outcomes than those of a higher social stratum. The new public health advocates for population-based policies that improve health in an equitable manner.
Health aid in less developed countries
Health aid to developing countries is an important source of public health funding for many low- and middle-income countries.
Health aid to developing countries has shown a significant increase
after World War II as concerns over the spread of disease as a result of
globalization increased and the HIV/AIDS epidemic in sub-Saharan Africa
surfaced.
From 1990 to 2010, total health aid from developed countries increased
from 5.5 billion to 26.87 billion with wealthy countries continuously
donating billions of dollars every year with the goal of improving
population health.
Some efforts, however, receive a significantly larger proportion of
funds such as HIV which received an increase in funds of over $6 billion
dollars between 2000 and 2010 which was more than twice the increase
seen in any other sector during those years. Health aid has seen an expansion through multiple channels including private philanthropy, non-governmental organizations, private foundations such as the Bill & Melinda Gates Foundation, bilateral donors, and multilateral donors such as the World Bank or UNICEF. In 2009 health aid from the OECD amounted to $12.47 billion which amounted to 11.4% of its total bilateral aid. In 2009, Multilateral donors were found to spend 15.3% of their total aid on bettering public healthcare. Recent data, however, shows that international health aid has plateaued and may begin to decrease.
International health aid debates
Debates
exist questioning the efficacy of international health aid. Proponents
of aid claim that health aid from wealthy countries is necessary in
order for developing countries to escape the poverty trap.
Opponents of health aid claim that international health aid actually
disrupts developing countries' course of development, causes dependence
on aid, and in many cases the aid fails to reach its recipients.
For example, recently, health aid was funneled towards initiatives such
as financing new technologies like antiretroviral medication,
insecticide-treated mosquito nets, and new vaccines. The positive
impacts of these initiatives can be seen in the eradication of smallpox
and polio; however, critics claim that misuse or misplacement of funds
may cause many of these efforts to never come into fruition.
Economic modeling based on the Institute for Health Metrics and Evaluation and the World Health Organization has shown a link between international health aid in developing countries and a reduction in adult mortality rates.
However, a 2014-2016 study suggests that a potential confounding
variable for this outcome is the possibility that aid was directed at
countries once they were already on track for improvement.
That same study, however, also suggests that 1 billion dollars in
health aid was associated with 364,000 fewer deaths occurring between
ages 0 and 5 in 2011.
Sustainable development goals 2030
To address current and future challenges in addressing health issues in the world, the United Nations have developed the Sustainable Development Goals building off of the Millennium Development Goals of 2000 to be completed by 2030.
These goals in their entirety encompass the entire spectrum of
development across nations, however Goals 1-6 directly address health
disparities, primarily in developing countries. These six goals address key issues in global public health: Poverty, Hunger and food security, Health, Education, Gender equality and women's empowerment, and water and sanitation.
Public health officials can use these goals to set their own agenda and
plan for smaller scale initiatives for their organizations. These goals
hope to lessen the burden of disease and inequality faced by developing
countries and lead to a healthier future.
The links between the various sustainable development goals and public health are numerous and well established:
- Living below the poverty line is attributed to poorer health outcomes and can be even worse for persons living in developing countries where extreme poverty is more common. A child born into poverty is twice as likely to die before the age of five compared to a child from a wealthier family.
- The detrimental effects of hunger and malnutrition that can arise from systemic challenges with food security are enormous. The World Health Organization estimates that 12.9 percent of the population in developing countries is undernourished.
- Health challenges in the developing world are enormous, with "only half of the women in developing nations receiving the recommended amount of healthcare they need.
- Educational equity has yet to be reached in the world. Public health efforts are impeded by this, as a lack of education can lead to poorer health outcomes. This is shown by children of mothers who have no education having a lower survival rate compared to children born to mothers with primary or greater levels of education. Cultural differences in the role of women vary by country, many gender inequalities are found in developing nations. Combating these inequalities has shown to also lead to better public health outcome.
- In studies done by the World Bank on populations in developing countries, it was found that when women had more control over household resources, the children benefit through better access to food, healthcare, and education.
- Basic sanitation resources and access to clean sources of water are a basic human right. However, 1.8 billion people globally use a source of drinking water that is fecally contaminated, and 2.4 billion people lack access to basic sanitation facilities like toilets or pit latrines. A lack of these resources is what causes approximately 1000 children a day to die from diarrheal diseases that could have been prevented from better water and sanitation infrastructure.
U.S. initiatives
The
U.S. Global Health Initiative was created in 2009 by President Obama in
an attempt to have a more holistic, comprehensive approach to improving
global health as opposed to previous, disease-specific interventions.
The Global Health Initiative is a six-year plan, "to develop a
comprehensive U.S. government strategy for global health, building on
the President's Emergency Plan for AIDS Relief
(PEPFAR) to combat HIV as well as U.S. efforts to address tuberculosis
(TB) and malaria, and augmenting the focus on other global health
priorities, including neglected tropical diseases (NTDs), maternal,
newborn and child health (MNCH), family planning and reproductive health
(FP/RH), nutrition, and health systems strengthening (HSS)". The GHI programs are being implemented in more than 80 countries around the world and works closely with the United States Agency for International Development, the Centers for Disease Control and Prevention, the United States Deputy Secretary of State.
There are seven core principles:
- Women, girls, and gender equality
- Strategic coordination and integration
- Strengthen and leverage key multilaterals and other partners
- Country-ownership
- Sustainability through Health Systems
- Improve metrics, monitoring, and evaluation
- Promote research and innovation
The aid effectiveness agenda is a useful tool for measuring the impact of these large scale programs such as The Global Fund to Fight AIDS, Tuberculosis and Malaria and the Global Alliance for Vaccines and Immunization (GAVI) which have been successful in achieving rapid and visible results. The Global Fund claims that its efforts have provided antiretroviral treatment for over three million people worldwide. GAVI claims that its vaccination programs have prevented over 5 million deaths since it began in 2000.
Education and training
Education
and training of public health professionals is available throughout the
world in Schools of Public Health, Medical Schools, Veterinary Schools,
Schools of Nursing, and Schools of Public Affairs. The training
typically requires a university degree with a focus on core disciplines of biostatistics, epidemiology, health services administration, health policy, health education, behavioral science, gender issues, sexual and reproductive health, public health nutrition and environmental and occupational health.
In the global context, the field of public health education has evolved
enormously in recent decades, supported by institutions such as the World Health Organization and the World Bank,
among others. Operational structures are formulated by strategic
principles, with educational and career pathways guided by competency
frameworks, all requiring modulation according to local, national and
global realities. It is critically important for the health of
populations that nations assess their public health human resource needs
and develop their ability to deliver this capacity, and not depend on
other countries to supply it.
Schools of public health: a US perspective
In the United States, the Welch-Rose Report of 1915
has been viewed as the basis for the critical movement in the history
of the institutional schism between public health and medicine because
it led to the establishment of schools of public health supported by the
Rockefeller Foundation. The report was authored by William Welch, founding dean of the Johns Hopkins Bloomberg School of Public Health, and Wickliffe Rose of the Rockefeller Foundation. The report focused more on research than practical education.
Some have blamed the Rockefeller Foundation's 1916 decision to support
the establishment of schools of public health for creating the schism
between public health and medicine and legitimizing the rift between
medicine's laboratory investigation of the mechanisms of disease and
public health's nonclinical concern with environmental and social
influences on health and wellness.
Even though schools of public health had already been established in Canada, Europe and North Africa,
the United States had still maintained the traditional system of
housing faculties of public health within their medical institutions. A
$25,000 donation from businessman Samuel Zemurray instituted the School of Public Health and Tropical Medicine at Tulane University in 1912 conferring its first doctor of public health degree in 1914. The Yale School of Public Health was founded by Charles-Edward Avory Winslow in 1915. The Johns Hopkins School of Hygiene and Public Health
became an independent, degree-granting institution for research and
training in public health, and the largest public health training
facility in the United States, when it was founded in 1916. By 1922, schools of public health were established at Columbia and Harvard
on the Hopkins model. By 1999 there were twenty nine schools of public
health in the US, enrolling around fifteen thousand students.
Over the years, the types of students and training provided have
also changed. In the beginning, students who enrolled in public health
schools typically had already obtained a medical degree; public health
school training was largely a second degree for medical professionals. However, in 1978, 69% of American students enrolled in public health schools had only a bachelor's degree.
Degrees in public health
Schools of public health offer a variety of degrees which generally fall into two categories: professional or academic. The two major postgraduate degrees are the Master of Public Health (MPH) or the Master of Science in Public Health (MSPH). Doctoral studies in this field include Doctor of Public Health (DrPH) and Doctor of Philosophy
(PhD) in a subspeciality of greater Public Health disciplines. DrPH is
regarded as a professional degree and PhD as more of an academic degree.
Professional degrees are oriented towards practice in public health settings. The Master of Public Health, Doctor of Public Health, Doctor of Health Science (DHSc) and the Master of Health Care Administration
are examples of degrees which are geared towards people who want
careers as practitioners of public health in health departments, managed
care and community-based organizations, hospitals and consulting firms,
among others. Master of Public Health
degrees broadly fall into two categories, those that put more emphasis
on an understanding of epidemiology and statistics as the scientific
basis of public health practice and those that include a more eclectic
range of methodologies. A Master of Science of Public Health is similar
to an MPH but is considered an academic degree (as opposed to a
professional degree) and places more emphasis on scientific methods and
research. The same distinction can be made between the DrPH and the
DHSc. The DrPH is considered a professional degree and the DHSc is an
academic degree.
Academic degrees are more oriented towards those with interests in the scientific basis of public health and preventive medicine
who wish to pursue careers in research, university teaching in graduate
programs, policy analysis and development, and other high-level public
health positions. Examples of academic degrees are the Master of Science, Doctor of Philosophy, Doctor of Science (ScD), and Doctor of Health Science
(DHSc). The doctoral programs are distinct from the MPH and other
professional programs by the addition of advanced coursework and the
nature and scope of a dissertation research project.
In the United States, the Association of Schools of Public Health represents Council on Education for Public Health (CEPH) accredited schools of public health. Delta Omega is the honor society for graduate studies in public health. The society was founded in 1924 at the Johns Hopkins School of Hygiene and Public Health. Currently, there are approximately 68 chapters throughout the United States and Puerto Rico.
History
Early history
The primitive nature of medieval medicine rendered Europe helpless to the onslaught of the Black Death
in the 14th century. Miniature from "The Chronicles of Gilles Li
Muisis" (1272-1352). Bibliothèque royale de Belgique, MS 13076-77, f.
24v.
Public health has early roots in antiquity. From the beginnings of human civilization, it was recognized that polluted water and lack of proper waste disposal spread communicable diseases (theory of miasma). Early religions attempted to regulate behavior that specifically related to health, from types of food eaten, to regulating certain indulgent behaviors, such as drinking alcohol or sexual relations. Leaders were responsible for the health of their subjects to ensure social stability, prosperity, and maintain order.
By Roman times, it was well understood that proper diversion of human waste was a necessary tenet of public health in urban areas. The ancient Chinese medical doctors developed the practice of variolation following a smallpox
epidemic around 1000 BC. An individual without the disease could gain
some measure of immunity against it by inhaling the dried crusts that
formed around lesions of infected individuals. Also, children were
protected by inoculating a scratch on their forearms with the pus from a lesion.
In 1485 the Republic of Venice established a permanent Venetian Magistrate for Health
comprising supervisors of health with special attention to the
prevention of the spread of epidemics in the territory from abroad. The
three supervisors were initially appointed by the Venetian Senate. In
1537 it was assumed by the Grand Council, and in 1556 added two judges,
with the task of control, on behalf of the Republic, the efforts of the
supervisors.
However, according to Michel Foucault, the plague model of governmentality was later controverted by the cholera
model. A Cholera pandemic devastated Europe between 1829 and 1851, and
was first fought by the use of what Foucault called "social medicine",
which focused on flux, circulation of air, location of cemeteries, etc. All those concerns, born of the miasma theory of disease, were mixed with urbanistic concerns for the management of populations, which Foucault designated as the concept of "biopower". The German conceptualized this in the Polizeiwissenschaft ("Police science").
Modern public health
The 18th century saw rapid growth in voluntary hospitals in England.
The latter part of the century brought the establishment of the basic
pattern of improvements in public health over the next two centuries: a
social evil was identified, private philanthropists brought attention to
it, and changing public opinion led to government action.
1802 caricature of Edward Jenner vaccinating patients who feared it would make them sprout cowlike appendages.
The practice of vaccination became prevalent in the 1800s, following the pioneering work of Edward Jenner in treating smallpox. James Lind's discovery of the causes of scurvy amongst sailors and its mitigation via the introduction of fruit on lengthy voyages was published in 1754 and led to the adoption of this idea by the Royal Navy. Efforts were also made to promulgate health matters to the broader public; in 1752 the British physician Sir John Pringle published Observations on the Diseases of the Army in Camp and Garrison, in which he advocated for the importance of adequate ventilation in the military barracks and the provision of latrines for the soldiers.
With the onset of the Industrial Revolution,
living standards amongst the working population began to worsen, with
cramped and unsanitary urban conditions. In the first four decades of
the 19th century alone, London's population doubled and even greater growth rates were recorded in the new industrial towns, such as Leeds and Manchester. This rapid urbanization exacerbated the spread of disease in the large conurbations that built up around the workhouses and factories. These settlements were cramped and primitive with no organized sanitation.
Disease was inevitable and its incubation in these areas was encouraged
by the poor lifestyle of the inhabitants. Unavailable housing led to
the rapid growth of slums and the per capita death rate began to rise alarmingly, almost doubling in Birmingham and Liverpool. Thomas Malthus warned of the dangers of overpopulation in 1798. His ideas, as well as those of Jeremy Bentham, became very influential in government circles in the early years of the 19th century.
Public health legislation
Sir Edwin Chadwick was a pivotal influence on the early public health campaign.
The first attempts at sanitary reform and the establishment of public health institutions were made in the 1840s. Thomas Southwood Smith, physician at the London Fever Hospital,
began to write papers on the importance of public health, and was one
of the first physicians brought in to give evidence before the Poor Law Commission in the 1830s, along with Neil Arnott and James Phillips Kay. Smith advised the government on the importance of quarantine and sanitary improvement for limiting the spread of infectious diseases such as cholera and yellow fever.
The Poor Law Commission
reported in 1838 that "the expenditures necessary to the adoption and
maintenance of measures of prevention would ultimately amount to less
than the cost of the disease now constantly engendered". It recommended
the implementation of large scale government engineering projects to alleviate the conditions that allowed for the propagation of disease. The Health of Towns Association was formed in Exeter on 11 December 1844, and vigorously campaigned for the development of public health in the United Kingdom. Its formation followed the 1843 establishment of the Health of Towns Commission, chaired by Sir Edwin Chadwick, which produced a series of reports on poor and insanitary conditions in British cities.
These national and local movements led to the Public Health Act,
finally passed in 1848. It aimed to improve the sanitary condition of
towns and populous places in England and Wales by placing the supply of
water, sewerage, drainage, cleansing and paving under a single local
body with the General Board of Health as a central authority. The Act
was passed by the Liberal government of Lord John Russell, in response to the urging of Edwin Chadwick. Chadwick's seminal report on The Sanitary Condition of the Labouring Population was published in 1842 and was followed up with a supplementary report a year later.
Vaccination for various diseases was made compulsory in the United Kingdom in 1851, and by 1871 legislation required a comprehensive system of registration run by appointed vaccination officers.
Further interventions were made by a series of subsequent Public Health Acts, notably the 1875 Act. Reforms included latrinization, the building of sewers, the regular collection of garbage followed by incineration or disposal in a landfill, the provision of clean water and the draining of standing water to prevent the breeding of mosquitoes.
The Infectious Disease (Notification) Act 1889
mandated the reporting of infectious diseases to the local sanitary
authority, which could then pursue measures such as the removal of the
patient to hospital and the disinfection of homes and properties.
In the United States, the first public health organization based
on a state health department and local boards of health was founded in New York City in 1866.
Epidemiology
The science of epidemiology was founded by John Snow's identification of a polluted public water well as the source of an 1854 cholera outbreak in London. Dr. Snow believed in the germ theory of disease as opposed to the prevailing miasma theory. He first publicized his theory in an essay, On the Mode of Communication of Cholera,
in 1849, followed by a more detailed treatise in 1855 incorporating the
results of his investigation of the role of the water supply in the Soho epidemic of 1854.
By talking to local residents (with the help of Reverend Henry Whitehead), he identified the source of the outbreak as the public water pump on Broad Street (now Broadwick Street). Although Snow's chemical and microscope examination of a water sample from the Broad Street pump
did not conclusively prove its danger, his studies of the pattern of
the disease were convincing enough to persuade the local council to
disable the well pump by removing its handle.
Snow later used a dot map
to illustrate the cluster of cholera cases around the pump. He also
used statistics to illustrate the connection between the quality of the
water source and cholera cases. He showed that the Southwark and Vauxhall Waterworks Company was taking water from sewage-polluted sections of the Thames
and delivering the water to homes, leading to an increased incidence of
cholera. Snow's study was a major event in the history of public health
and geography. It is regarded as the founding event of the science of epidemiology.
Disease control
Paul-Louis Simond injecting a plague vaccine in Karachi, 1898.
With the pioneering work in bacteriology of French chemist Louis Pasteur and German scientist Robert Koch, methods for isolating the bacteria responsible for a given disease and vaccines for remedy were developed at the turn of the 20th century. British physician Ronald Ross identified the mosquito as the carrier of malaria and laid the foundations for combating the disease. Joseph Lister revolutionized surgery by the introduction of antiseptic surgery to eliminate infection. French epidemiologist Paul-Louis Simond proved that plague was carried by fleas on the back of rats, and Cuban scientist Carlos J. Finlay and U.S. Americans Walter Reed and James Carroll demonstrated that mosquitoes carry the virus responsible for yellow fever. Brazilian scientist Carlos Chagas identified a tropical disease and its vector.
With onset of the epidemiological transition and as the prevalence of infectious diseases decreased through the 20th century, public health began to put more focus on chronic diseases such as cancer and heart disease. Previous efforts in many developed countries had already led to dramatic reductions in the infant mortality rate using preventative methods. In Britain, the infant mortality rate fell from over 15% in 1870 to 7% by 1930.
Country examples
France
France 1871-1914
followed well behind Bismarckian Germany, as well as Great Britain, in
developing the welfare state including public health. Tuberculosis was
the most dreaded disease of the day, especially striking young people
in their 20s. Germany set up vigorous measures of public hygiene and
public sanatoria, but France let private physicians handle the problem,
which left it with a much higher death rate.
The French medical profession jealously guarded its prerogatives, and
public health activists were not as well organized or as influential as
in Germany, Britain or the United States. For example, there was a long battle over a public health law
which began in the 1880s as a campaign to reorganize the nation's
health services, to require the registration of infectious diseases, to
mandate quarantines, and to improve the deficient health and housing
legislation of 1850. However the reformers met opposition from
bureaucrats, politicians, and physicians. Because it was so threatening
to so many interests, the proposal was debated and postponed for 20
years before becoming law in 1902. Success finally came when the
government realized that contagious diseases had a national security
impact in weakening military recruits, and keeping the population growth
rate well below Germany's.
United States
The seal of the United States Public Health Service.
Modern public health began developing in the 19th century, as a
response to advances in science that led to the understanding of, the
source and spread of disease. As the knowledge of contagious diseases
increased, means to control them and prevent infection were soon
developed. Once it became understood that these strategies would require
community-wide participation, disease control began being viewed as a
public responsibility. Various organizations and agencies were then
created to implement these disease preventing strategies.
Most of the Public health activity in the United States took
place at the municipal level before the mid-20th century. There was some
activity at the national and state level as well.
In the administration of the second president of the United States John Adams,
the Congress authorized the creation of hospitals for mariners. As the
U.S. expanded, the scope of the governmental health agency expanded.
In the United States, public health worker Sara Josephine Baker,
M.D. established many programs to help the poor in New York City keep
their infants healthy, leading teams of nurses into the crowded
neighborhoods of Hell's Kitchen and teaching mothers how to dress, feed, and bathe their babies.
Another key pioneer of public health in the U.S. was Lillian Wald, who founded the Henry Street Settlement house in New York. The Visiting Nurse Service of New York was a significant organization for bringing health care to the urban poor.
Dramatic increases in average life span in the late 19th century
and 20th century, is widely credited to public health achievements, such
as vaccination programs and control of many infectious diseases including polio, diphtheria, yellow fever and smallpox; effective health and safety policies such as road traffic safety and occupational safety; improved family planning; tobacco control measures; and programs designed to decrease non-communicable diseases by acting on known risk factors such as a person's background, lifestyle and environment.
Another major public health improvement was the decline in the "urban penalty" brought about by improvements in sanitation. These improvements included chlorination of drinking water, filtration and sewage treatment which led to the decline in deaths caused by infectious waterborne diseases such as cholera and intestinal diseases.
The federal Office of Indian Affairs (OIA) operated a large-scale field
nursing program. Field nurses targeted native women for health
education, emphasizing personal hygiene and infant care and nutrition.
Mexico
Logo for the Mexican Social Security Institute, a governmental agency dealing with public health.
Public health issues were important for the Spanish empire
during the colonial era. Epidemic disease was the main factor in the
decline of indigenous populations in the era immediately following the
sixteenth-century conquest era and was a problem during the colonial
era. The Spanish crown took steps in eighteenth-century Mexico to bring
in regulations to make populations healthier.
In the late nineteenth century, Mexico was in the process of
modernization, and public health issues were again tackled from a
scientific point of view. Even during the Mexican Revolution (1910–20), public health was an important concern, with a text on hygiene published in 1916.[105] During the Mexican Revolution, feminist and trained nurse Elena Arizmendi Mejia founded the Neutral White Cross, treating wounded soldiers no matter for what faction they fought.
In the post-revolutionary period after 1920, improved public health was a revolutionary goal of the Mexican government.
The Mexican state promoted the health of the Mexican population, with most resources going to cities.
Concern about disease conditions and social impediments to the
improvement of Mexicans' health were important in the formation of the Mexican Society for Eugenics. The movement flourished from the 1920s to the 1940s. Mexico was not alone in Latin America or the world in promoting eugenics. Government campaigns against disease and alcoholism were also seen as promoting public health.
The Mexican Social Security Institute was established in 1943, during the administration of President Manuel Avila Camacho to deal with public health, pensions, and social security.
Cuba
Since the 1959 Cuban Revolution the Cuban government has devoted extensive resources to the improvement of health conditions for its entire population via universal access to health care. Infant mortality has plummeted. Cuban medical internationalism
as a policy has seen the Cuban government sent doctors as a form of aid
and export to countries in need in Latin America, especially Venezuela, as well as Oceania and Africa countries.
Colombia and Bolivia
Public
health was important elsewhere in Latin America in consolidating state
power and integrating marginalized populations into the nation-state.
In Colombia, public health was a means for creating and implementing
ideas of citizenship. In Bolivia, a similar push came after their 1952 revolution.
Ghana
Though curable and preventative, malaria remains a huge public health problem and is the third leading cause of death in Ghana.
In the absence of a vaccine, mosquito control, or access to
anti-malaria medication, public health methods become the main strategy
for reducing the prevalence and severity of malaria.
These methods include reducing breeding sites, screening doors and
windows, insecticide sprays, prompt treatment following infection, and
usage of insecticide treated mosquito nets.
Distribution and sale of insecticide-treated mosquito nets is a common,
cost-effective anti-malaria public health intervention; however,
barriers to use exist including cost, hosehold and family organization,
access to resources, and social and behavioral determinants which have
not only been shown to affect malaria prevalence rates but also mosquito
net use.