Universal health care, 2018
Universal health care (also called universal health coverage, universal coverage, universal care, or socialized health care) is a health care
system that provides health care and financial protection to all
citizens of a particular country. It is organized around providing a
specified package of benefits to all members of a society with the end
goal of providing financial risk protection, improved access to health
services, and improved health outcomes.
Universal health care does not imply coverage for all people for
everything. Universal health care can be determined by three critical
dimensions: who is covered, what services are covered, and how much of
the cost is covered. It is described by the World Health Organization as a situation where citizens can access health services without incurring financial hardship.
The Director General of WHO describes universal health coverage as the
“single most powerful concept that public health has to offer” since it
unifies “services and delivers them in a comprehensive and integrated
way”.
One of the goals with universal healthcare is to create a system of
protection which provides equality of opportunity for people to enjoy
the highest possible level of health.
As part of Sustainable Development Goals, United Nations member states have agreed to work toward worldwide universal health coverage by 2030.
History
The first move towards a national health insurance system was launched in Germany
in 1883, with the Sickness Insurance Law. Industrial employers were
mandated to provide injury and illness insurance for their low-wage
workers, and the system was funded and administered by employees and
employers through "sick funds", which were drawn from deductions in
workers' wages and from employers' contributions. Other countries soon
began to follow suit. In the United Kingdom, the National Insurance Act 1911
provided coverage for primary care (but not specialist or hospital
care) for wage earners, covering about one third of the population. The Russian Empire
established a similar system in 1912, and other industrialized
countries began following suit. By the 1930s, similar systems existed in
virtually all of Western and Central Europe. Japan introduced an employee health insurance law in 1927, expanding further upon it in 1935 and 1940. Following the Russian Revolution of 1917, the Soviet Union established a fully public and centralized health care system in 1920. However, it was not a truly universal system at that point, as rural residents were not covered.
In New Zealand, a universal health care system was created in a series of steps, from 1939 to 1941. In Australia, the state of Queensland introduced a free public hospital system in the 1940s.
Following World War II, universal health care systems began to be set up around the world. On July 5, 1948, the United Kingdom launched its universal National Health Service. Universal health care was next introduced in the Nordic countries of Sweden (1955), Iceland (1956), Norway (1956), Denmark (1961), and Finland (1964). Universal health insurance was then introduced in Japan (1961), and in Canada through stages, starting with the province of Saskatchewan in 1962, followed by the rest of Canada from 1968 to 1972. The Soviet Union extended universal health care to its rural residents in 1969. Italy introduced its Servizio Sanitario Nazionale (National Health Service) in 1978. Universal health insurance was implemented in Australia beginning with the Medibank system which led to universal coverage under the Medicare system.
From the 1970s to the 2000s, Southern and Western European
countries began introducing universal coverage, most of them building
upon previous health insurance programs to cover the whole population.
For example, France
built upon its 1928 national health insurance system, with subsequent
legislation covering a larger and larger percentage of the population,
until the remaining 1% of the population that was uninsured received
coverage in 2000. In addition, universal health coverage was introduced in some Asian countries, including South Korea (1989), Taiwan (1995), Israel (1995), and Thailand (2001).
Following the collapse of the Soviet Union, Russia retained and reformed its universal health care system, as did other former Soviet nations and Eastern bloc countries.
Beyond the 1990s, many countries in Latin America, the Caribbean, Africa, and the Asia-Pacific region, including developing countries, took steps to bring their populations under universal health coverage, including China which has the largest universal health care system in the world and Brazil's SUS which improved coverage up to 80% of the population. A 2012 study examined progress being made by these countries, focusing on nine in particular: Ghana, Rwanda, Nigeria, Mali, Kenya, India, Indonesia, the Philippines, and Vietnam.
Funding models
Universal health care in most countries has been achieved by a mixed
model of funding. General taxation revenue is the primary source of
funding, but in many countries it is supplemented by specific levies
(which may be charged to the individual and/or an employer) or with the
option of private payments (by direct or optional insurance) for
services beyond those covered by the public system. Almost all European
systems are financed through a mix of public and private contributions. Most universal health care systems are funded primarily by tax revenue (like in Portugal, Spain, Denmark, and Sweden). Some nations, such as Germany, France, and Japan,
employ a multipayer system in which health care is funded by private
and public contributions. However, much of the non-government funding is
by contributions by employers and employees to regulated non-profit
sickness funds. Contributions are compulsory and defined according to
law. A distinction is also made between municipal and national
healthcare funding. For example, one model is that the bulk of the
healthcare is funded by the municipality, speciality healthcare is
provided and possibly funded by a larger entity, such as a municipal
co-operation board or the state, and the medications are paid by a state
agency. A paper by Sherry A. Glied from Columbia University
found that universal health care systems are modestly redistributive,
and that the progressivity of health care financing has limited
implications for overall income inequality.
Compulsory insurance
This is usually enforced via legislation requiring residents to
purchase insurance, but sometimes the government provides the insurance.
Sometimes, there may be a choice of multiple public and private funds
providing a standard service (as in Germany) or sometimes just a single
public fund (as in Canada). Healthcare in Switzerland and the US Patient Protection and Affordable Care Act are based on compulsory insurance.
In some European countries, in which private insurance and
universal health care coexist, such as Germany, Belgium, and the
Netherlands, the problem of adverse selection
is overcome by using a risk compensation pool to equalize, as far as
possible, the risks between funds. Thus, a fund with a predominantly
healthy, younger population has to pay into a compensation pool and a
fund with an older and predominantly less healthy population would
receive funds from the pool. In this way, sickness funds compete on
price, and there is no advantage to eliminate people with higher risks
because they are compensated for by means of risk-adjusted capitation
payments. Funds are not allowed to pick and choose their policyholders
or deny coverage, but they compete mainly on price and service. In some
countries, the basic coverage level is set by the government and cannot
be modified.
The Republic of Ireland at one time had a "community rating" system by VHI,
effectively a single-payer or common risk pool. The government later
opened VHI to competition but without a compensation pool. That resulted
in foreign insurance companies entering the Irish market and offering
cheap health insurance to relatively healthy segments of the market,
which then made higher profits at VHI's expense. The government later
reintroduced community rating by a pooling arrangement and at least one
main major insurance company, BUPA, withdrew from the Irish market.
Among the potential solutions posited by economists are
single-payer systems as well as other methods of ensuring that health
insurance is universal, such as by requiring all citizens to purchase
insurance or limiting the ability of insurance companies to deny
insurance to individuals or vary price between individuals.
Single payer
Single-payer health care is a system in which the government, rather than private insurers, pays for all health care costs. Single-payer systems may contract for healthcare services from private organizations (as is the case in Canada) or own and employ healthcare resources and personnel (as was the case in England before the introduction of the Health and Social Care Act).
"Single-payer" thus describes only the funding mechanism and refers to
health care financed by a single public body from a single fund and does
not specify the type of delivery or for whom doctors work. Although the
fund holder is usually the state, some forms of single-payer use a
mixed public-private system.
Tax-based financing
In
tax-based financing, individuals contribute to the provision of health
services through various taxes. These are typically pooled across the
whole population, unless local governments raise and retain tax
revenues. Some countries (notably the United Kingdom, Canada, Ireland,
New Zealand, Italy, Spain, Portugal, and the Nordic countries)
choose to fund health care directly from taxation alone. Other
countries with insurance-based systems effectively meet the cost of
insuring those unable to insure themselves via social security
arrangements funded from taxation, either by directly paying their
medical bills or by paying for insurance premiums for those affected.
Social health insurance
In
a social health insurance system, contributions from workers, the
self-employed, enterprises, and governments are pooled into a single or
multiple funds on a compulsory basis. It is based on risk pooling. The social health insurance model is also referred to as the 'Bismarck Model,' after Prussian Chancellor Otto von Bismarck, who introduced the first universal health care system in Germany in the 19th century.
The funds typically contract with a mix of public and private providers
for the provision of a specified benefit package. Preventive and public
health care may be provided by these funds or responsibility kept
solely by the Ministry of Health. Within social health insurance, a
number of functions may be executed by parastatal or non-governmental
sickness funds or in a few cases, by private health insurance companies.
Social health insurance is used in a number of Western European
countries and increasingly in Eastern Europe as well as in Israel and
Japan.
Private insurance
In
private health insurance, premiums are paid directly from employers,
associations, individuals, and families to insurance companies, which
pool risks across their membership base. Private insurance includes
policies sold by commercial for profit firms, non-profit companies, and
community health insurers. Generally, private insurance is voluntary in
contrast to social insurance programs, which tend to be compulsory.
In some countries with universal coverage, private insurance
often excludes many health conditions that are expensive and the state
health care system can provide. For example, in the United Kingdom, one
of the largest private health care providers is BUPA, which has a long list of general exclusions even in its highest coverage policy, most of which are routinely provided by the National Health Service. In the United States, dialysis treatment for end stage renal failure is generally paid for by government, not by the insurance industry. Those with privatized Medicare (Medicare Advantage) are the exception and must get their dialysis paid through their insurance company, but with end stage renal failure generally cannot buy Medicare Advantage plans.
In the Netherlands, which has regulated competition for its main
insurance system (but subject to a budget cap), insurers must cover a
basic package for all enrollees, but may choose which additional
services they cover in other, supplementary plans (which most people
possess - citation needed).
The Planning Commission of India has also suggested that the country should embrace insurance to achieve universal health coverage. General tax revenue is currently used to meet the essential health requirements of all people.
Community-based health insurance
A
particular form of private health insurance that has often emerged if
financial risk protection mechanisms have only a limited impact is
community-based health insurance. Individual members of a specific
community pay to a collective health fund, which they can draw from when
they need of medical care. Contributions are not risk-related, and
there is generally a high level of community involvement in the running
of these plans.
Implementation and comparisons
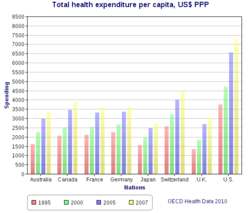
Health spending per capita, in US$ purchasing power parity-adjusted, among various OECD countries
Universal health care systems vary according to the degree of
government involvement in providing care and/or health insurance. In
some countries, such as the UK, Spain, Italy, Australia, and the Nordic
countries, the government has a high degree of involvement in the
commissioning or delivery of health care services and access is based on
residence rights, not on the purchase of insurance. Others have a much
more pluralistic delivery system, based on obligatory health with
contributory insurance rates related to salaries or income and usually
funded by employers and beneficiaries jointly.
Sometimes, the health funds are derived from a mixture of
insurance premiums, salary related mandatory contributions by employees
and/or employers to regulated sickness funds, and by government taxes.
These insurance based systems tend to reimburse private or public
medical providers, often at heavily regulated rates, through mutual or
publicly owned medical insurers. A few countries, such as the
Netherlands and Switzerland, operate via privately owned but heavily
regulated private insurers, which are not allowed to make a profit from
the mandatory element of insurance but can profit by selling
supplemental insurance.
Universal health care is a broad concept that has been
implemented in several ways. The common denominator for all such
programs is some form of government action aimed at extending access to
health care as widely as possible and setting minimum standards. Most
implement universal health care through legislation, regulation, and
taxation. Legislation and regulation direct what care must be provided,
to whom, and on what basis. Usually, some costs are borne by the patient
at the time of consumption, but the bulk of costs come from a
combination of compulsory insurance and tax revenues. Some programs are
paid for entirely out of tax revenues. In others, tax revenues are used
either to fund insurance for the very poor or for those needing
long-term chronic care.
The United Kingdom National Audit Office
in 2003 published an international comparison of ten different health
care systems in ten developed countries, nine universal systems against
one non-universal system (the United States), and their relative costs
and key health outcomes. A wider international comparison of 16 countries, each with universal health care, was published by the World Health Organization in 2004. In some cases, government involvement also includes directly managing the health care system, but many countries use mixed public-private systems to deliver universal health care.