From Wikipedia, the free encyclopedia
Anesthesia or anaesthesia is a state of controlled,
temporary loss of sensation or awareness that is induced for medical or
veterinary purposes. It may include some or all of analgesia (relief from or prevention of pain), paralysis (muscle relaxation), amnesia (loss of memory), and unconsciousness. An individual under the effects of anesthetic drugs is referred to as being anesthetized.
Anesthesia enables the painless performance of procedures that
would otherwise cause severe or intolerable pain in a non-anesthetized
individual, or would otherwise be technically unfeasible. Three broad
categories of anesthesia exist:
- General anesthesia suppresses central nervous system activity and results in unconsciousness and total lack of sensation, using either injected or inhaled drugs.
- Sedation suppresses the central nervous system to a lesser degree, inhibiting both anxiety and creation of long-term memories without resulting in unconsciousness.
- Regional and local anesthesia,
which blocks transmission of nerve impulses from a specific part of the
body. Depending on the situation, this may be used either on its own
(in which case the individual remains fully conscious), or in
combination with general anesthesia or sedation.
- Local anesthesia is simple infiltration by the clinician directly onto the region of interest (e.g. numbing a tooth for dental work).
- Peripheral nerve blocks use drugs targeted at peripheral nerves to anesthetize an isolated part of the body, such as an entire limb.
- Neuraxial blockade , mainly epidural and spinal
anesthesia, can be performed in the region of the central nervous
system itself, suppressing all incoming sensation from nerves supplying
the area of the block.
In preparing for a medical or veterinary procedure, the clinician
chooses one or more drugs to achieve the types and degree of anesthesia
characteristics appropriate for the type of procedure and the particular
patient. The types of drugs used include general anesthetics, local anesthetics, hypnotics, dissociatives, sedatives, adjuncts, neuromuscular-blocking drugs, narcotics, and analgesics.
The risks of complications during or after anesthesia are often
difficult to separate from those of the procedure for which anesthesia
is being given, but in the main they are related to three factors: the
health of the individual, the complexity and stress of the procedure
itself, and the anaesthetic technique. Of these factors, the
individual's health has the greatest impact. Major perioperative risks
can include death, heart attack, and pulmonary embolism whereas minor risks can include postoperative nausea and vomiting and hospital readmission. Some conditions, like local anesthetic toxicity, airway trauma or malignant hyperthermia, can be more directly attributed to specific anesthetic drugs and techniques.
Medical uses
The purpose of anesthesia can be distilled down to three basic goals or endpoints:
Different types of anesthesia affect the endpoints differently. Regional anesthesia, for instance, affects analgesia; benzodiazepine-type sedatives (used for sedation, or "twilight anesthesia") favor amnesia; and general anesthetics
can affect all of the endpoints. The goal of anesthesia is to achieve
the endpoints required for the given surgical procedure with the least
risk to the subject.
The anesthetic area of an operating room
To achieve the goals of anesthesia, drugs act on different but
interconnected parts of the nervous system. Hypnosis, for instance, is
generated through actions on the nuclei in the brain and is similar to the activation of sleep. The effect is to make people less aware and less reactive to noxious stimuli.
Loss of memory (amnesia) is created by action of drugs on multiple (but specific) regions of the brain. Memories are created as either declarative or non-declarative memories in several stages (short-term, long-term, long-lasting) the strength of which is determined by the strength of connections between neurons termed synaptic plasticity. Each anesthetic produces amnesia through unique effects on memory formation at variable doses. Inhalational anesthetics
will reliably produce amnesia through general suppression of the nuclei
at doses below those required for loss of consciousness. Drugs like midazolam produce amnesia through different pathways by blocking the formation of long-term memories.
Nevertheless, a person can have dreams
during anesthetic or have consciousness of the procedure despite having
no indication of it under anesthetic. It is estimated that 22% of
people dream during general anesthesia and 1–2 cases per 1000 have some consciousness termed "awareness during general anesthesia". It is unknown whether non-human animals have dreams during general anesthesia.
Techniques
Anesthesia
is unique in that it is not a direct means of treatment; rather, it
allows the clinician to do things that may treat, diagnose, or cure an
ailment which would otherwise be painful or complicated. The best
anesthetic, therefore, is the one with the lowest risk to the patient
that still achieves the endpoints required to complete the procedure.
The first stage in anesthesia is the pre-operative risk assessment
consisting of the medical history, physical examination and lab tests.
Diagnosing an animal's pre-operative physical status allows the
clinician to minimize anesthetic risks. A well completed medical
history will arrive at the correct diagnosis 56% of the time which
increases to 73% with a physical examination. Lab tests
help in diagnosis but only in 3% of cases, underscoring the need for a
full history and physical examination prior to anesthetics. Incorrect
pre-operative assessments or preparations are the root cause of 11% of
all adverse anesthetic events.
Safe anesthesia care depends greatly on well-functioning teams of highly trained healthcare workers. The medical specialty centred around anesthesia is called anesthesiology, and doctors specialised in the field are termed anesthesiologists.
Additional healthcare professionals involved in anesthesia provision
have varying titles and roles depending on the jurisdiction, and include
anesthetic nurses, nurse anesthetists, anesthesiologist assistants, anaesthetic technicians, anaesthesia associates, operating department practitioners and anesthesia technologists. International standards for the safe practice of anesthesia, jointly endorsed by the World Health Organization and the World Federation of Societies of Anaesthesiologists,
highly recommend that anesthesia should be provided, overseen or led by
anesthesiologists, with the exception of minimal sedation or
superficial procedures performed under local anesthesia.
A trained, vigilant anesthesia provider should continually care for the
patient; where the provider is not an anesthesiologist, they should be
locally directed and supervised by an anesthesiologist, and in countries
or settings where this is not feasible, care should be led by the most
qualified local individual within a regional or national
anesthesiologist-led framework. The same minimum standards for patient safety
apply regardless of the provider, including continuous clinical and
biometric monitoring of tissue oxygenation, perfusion and blood
pressure; confirmation of correct placement of airway management devices by auscultation and carbon dioxide detection; use of the WHO Surgical Safety Checklist; and safe onward transfer of the patient's care following the procedure.
One part of the risk assessment
is based on the patient's health. The American Society of
Anesthesiologists has developed a six-tier scale that stratifies the
patient's pre-operative physical state. It is called the ASA physical status classification. The scale assesses risk as the patient's general health relates to an anesthetic.
The more detailed pre-operative medical history aims to discover genetic disorders (such as malignant hyperthermia or pseudocholinesterase deficiency), habits (tobacco, drug and alcohol use), physical attributes (such as obesity or a difficult airway) and any coexisting diseases (especially cardiac and respiratory diseases) that might impact the anesthetic. The physical examination helps quantify the impact of anything found in the medical history in addition to lab tests.
Aside from the generalities of the patient's health assessment,
an evaluation of specific factors as they relate to the surgery also
need to be considered for anesthesia. For instance, anesthesia during childbirth must consider not only the mother but the baby. Cancers and tumors that occupy the lungs or throat create special challenges to general anesthesia.
After determining the health of the patient undergoing anesthesia and
the endpoints that are required to complete the procedure, the type of
anesthetic can be selected. Choice of surgical method and anesthetic
technique aims to reduce risk of complications, shorten time needed for
recovery and minimize the surgical stress response.
General anesthesia
A
vaporizer holds a liquid anesthetic and converts it to gas for inhalation (in this case
sevoflurane)
A patient receiving anesthesia through inhalation
Anesthesia is a combination of the endpoints (discussed above) that
are reached by drugs acting on different but overlapping sites in the central nervous system. General anesthesia (as opposed to sedation or regional anesthesia) has three main goals: lack of movement (paralysis), unconsciousness, and blunting of the stress response.
In the early days of anesthesia, anesthetics could reliably achieve
the first two, allowing surgeons to perform necessary procedures, but
many patients died because the extremes of blood pressure and pulse
caused by the surgical insult were ultimately harmful. Eventually, the
need for blunting of the surgical stress response was identified by Harvey Cushing, who injected local anesthetic prior to hernia repairs. This led to the development of other drugs that could blunt the response leading to lower surgical mortality rates.
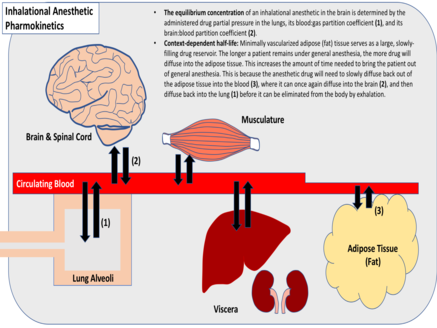
The most common approach to reach the endpoints of general anesthesia
is through the use of inhaled general anesthetics. Each anesthetic has
its own potency which is correlated to its solubility in oil. This
relationship exists because the drugs bind directly to cavities in
proteins of the central nervous system, although several theories of general anesthetic action
have been described. Inhalational anesthetics are thought to exact
their effects on different parts of the central nervous system. For
instance, the immobilizing effect of inhaled anesthetics results from an effect on the spinal cord whereas sedation, hypnosis and amnesia involve sites in the brain. The potency of an inhalational anesthetic is quantified by its minimum alveolar concentration
(MAC). The MAC is the percentage dose of anesthetic that will prevent a
response to painful stimulus in 50% of subjects. The higher the MAC,
generally, the less potent the anesthetic.
The ideal anesthetic drug would provide hypnosis, amnesia, analgesia,
and muscle relaxation without undesirable changes in blood pressure,
pulse or breathing. In the 1930s, physicians started to augment inhaled
general anesthetics with intravenous
general anesthetics. The drugs used in combination offered a better
risk profile to the subject under anesthesia and a quicker recovery. A
combination of drugs was later shown to result in lower odds of dying in
the first seven days after anesthetic. For instance, propofol (injection) might be used to start the anesthetic, fentanyl (injection) used to blunt the stress response, midazolam (injection) given to ensure amnesia and sevoflurane
(inhaled) during the procedure to maintain the effects. More recently,
several intravenous drugs have been developed which, if desired, allow
inhaled general anesthetics to be avoided completely.
Equipment
The core instrument in an inhalational anesthetic delivery system is an anesthetic machine. It has vaporizers, ventilators,
an anesthetic breathing circuit, waste gas scavenging system and
pressure gauges. The purpose of the anesthetic machine is to provide
anesthetic gas at a constant pressure, oxygen for breathing and to
remove carbon dioxide or other waste anesthetic gases. Since
inhalational anesthetics are flammable, various checklists have been
developed to confirm that the machine is ready for use, that the safety
features are active and the electrical hazards are removed. Intravenous anesthetic is delivered either by bolus doses or an infusion pump. There are also many smaller instruments used in airway management and monitoring the patient. The common thread to modern machinery in this field is the use of fail-safe systems that decrease the odds of catastrophic misuse of the machine.
Monitoring

Patients under general anesthesia must undergo continuous physiological monitoring to ensure safety. In the US, the American Society of Anesthesiologists
(ASA) has established minimum monitoring guidelines for patients
receiving general anesthesia, regional anesthesia, or sedation. These
include electrocardiography (ECG), heart rate, blood pressure, inspired
and expired gases, oxygen saturation of the blood (pulse oximetry), and
temperature.
In the UK the Association of Anaesthetists (AAGBI) have set minimum
monitoring guidelines for general and regional anesthesia. For minor
surgery, this generally includes monitoring of heart rate, oxygen saturation, blood pressure, and inspired and expired concentrations for oxygen, carbon dioxide,
and inhalational anesthetic agents. For more invasive surgery,
monitoring may also include temperature, urine output, blood pressure, central venous pressure, pulmonary artery pressure and pulmonary artery occlusion pressure, cardiac output, cerebral activity,
and neuromuscular function. In addition, the operating room environment
must be monitored for ambient temperature and humidity, as well as for
accumulation of exhaled inhalational anesthetic agents, which might be
deleterious to the health of operating room personnel.
Sedation
Sedation (also referred to as dissociative anesthesia or twilight anesthesia) creates hypnotic, sedative, anxiolytic, amnesic, anticonvulsant,
and centrally produced muscle-relaxing properties. From the
perspective of the person giving the sedation, the patient appears
sleepy, relaxed and forgetful, allowing unpleasant procedures to be more
easily completed. Sedatives such as benzodiazepines are usually given with pain relievers (such as narcotics, or local anesthetics or both) because they do not, by themselves, provide significant pain relief.
From the perspective of the subject receiving a sedative, the
effect is a feeling of general relaxation, amnesia (loss of memory) and
time passing quickly. Many drugs can produce a sedative effect
including benzodiazepines, propofol, thiopental, ketamine
and inhaled general anesthetics. The advantage of sedation over a
general anesthetic is that it generally does not require support of the
airway or breathing (no tracheal intubation or mechanical ventilation) and can have less of an effect on the cardiovascular system which may add to a greater margin of safety in some patients.
Regional anesthesia
Sonography guided femoral nerve block
When pain is blocked from a part of the body using local anesthetics,
it is generally referred to as regional anesthesia. There are many
types of regional anesthesia either by injecting into the tissue itself,
a vein that feeds the area or around a nerve trunk that supplies
sensation to the area. The latter are called nerve blocks and are
divided into peripheral or central nerve blocks.
The following are the types of regional anesthesia:
- Infiltrative anesthesia: a small amount of local anesthetic is injected in a small area to stop any sensation (such as during the closure of a laceration, as a continuous infusion or "freezing" a tooth). The effect is almost immediate.
- Peripheral nerve block:
local anesthetic is injected near a nerve that provides sensation to
particular portion of the body. There is significant variation in the
speed of onset and duration of anesthesia depending on the potency of
the drug (e.g. Mandibular block, Fascia Iliaca Compartment Block).
- Intravenous regional anesthesia (also called a Bier block): dilute local anesthetic is infused to a limb through a vein with a tourniquet placed to prevent the drug from diffusing out of the limb.
- Central nerve block: Local anesthetic is injected or infused
in or around a portion of the central nervous system (discussed in more
detail below in spinal, epidural and caudal anesthesia).
- Topical anesthesia:
local anesthetics that are specially formulated to diffuse through the
mucous membranes or skin to give a thin layer of analgesia to an area
(e.g. EMLA patches).
- Tumescent anesthesia: a large amount of very dilute local anesthetics are injected into the subcutaneous tissues during liposuction.
- Systemic local anesthetics: local anesthetics are given systemically (orally or intravenous) to relieve neuropathic pain.
A 2018 Cochrane review found moderate quality evidence that regional anesthesia may reduce the frequency of persistent postoperative pain (PPP) from 3 to 18 months following thoracotomy and 3 to 12 months following caesarean. Low quality evidence was found 3 to 12 months following breast cancer surgery.
This review acknowledges certain limitations that impact its
applicability beyond the surgeries and regional anesthesia techniques
reviewed.
Nerve blocks
When local anesthetic is injected around a larger diameter nerve that transmits sensation from an entire region it is referred to as a nerve block or regional nerve blockade. Nerve blocks are commonly used in dentistry, when the mandibular nerve is blocked for procedures on the lower teeth. With larger diameter nerves (such as the interscalene block for upper limbs or psoas compartment block for lower limbs) the nerve and position of the needle is localized with ultrasound
or electrical stimulation. Evidence supports the use of ultrasound
guidance alone, or in combination with peripheral nerve stimulation, as
superior for improved sensory and motor block, a reduction in the need
for supplementation and fewer complications.
Because of the large amount of local anesthetic required to affect the
nerve, the maximum dose of local anesthetic has to be considered.
Nerve blocks are also used as a continuous infusion, following major
surgery such as knee, hip and shoulder replacement surgery, and may be
associated with lower complications.
Nerve blocks are also associated with a lower risk of neurologic
complications compared to the more central epidural or spinal neuraxial
blocks.
Spinal, epidural and caudal anesthesia
Central neuraxial anesthesia is the injection of local anesthetic around the spinal cord to provide analgesia in the abdomen, pelvis or lower extremities. It is divided into either spinal (injection into the subarachnoid space), epidural (injection outside of the subarachnoid space into the epidural space) and caudal (injection into the cauda equina or tail end of the spinal cord). Spinal and epidural are the most commonly used forms of central neuraxial blockade.
Spinal anesthesia
is a "one-shot" injection that provides rapid onset and profound
sensory anesthesia with lower doses of anesthetic, and is usually
associated with neuromuscular blockade (loss of muscle control). Epidural anesthesia
uses larger doses of anesthetic infused through an indwelling catheter
which allows the anesthetic to be augmented should the effects begin to
dissipate. Epidural anesthesia does not typically affect muscle control.
Because central neuraxial blockade causes arterial and venous vasodilation, a drop in blood pressure is common. This drop is largely dictated by the venous side of the circulatory system which holds 75% of the circulating blood volume. The physiologic effects are much greater when the block is placed above the 5th thoracic vertebra. An ineffective block is most often due to inadequate anxiolysis or sedation rather than a failure of the block itself.
Acute pain management
Nociception
(pain sensation) is not hard-wired into the body. Instead, it is a
dynamic process wherein persistent painful stimuli can sensitize the
system and either make pain management difficult or promote the
development of chronic pain. For this reason, preemptive acute pain
management may reduce both acute and chronic pain and is tailored to the
surgery, the environment in which it is given (in-patient/out-patient)
and the individual.
Pain management is classified into either pre-emptive or on-demand. On-demand pain medications typically include either opioid or non-steroidal anti-inflammatory drugs but can also make use of novel approaches such as inhaled nitrous oxide or ketamine. On demand drugs can be administered by a clinician ("as needed drug orders") or by the patient using patient-controlled analgesia
(PCA). PCA has been shown to provide slightly better pain control and
increased patient satisfaction when compared with conventional methods. Common preemptive approaches include epidural neuraxial blockade or nerve blocks. One review which looked at pain control after abdominal aortic surgery
found that epidural blockade provides better pain relief (especially
during movement) in the period up to three postoperative days. It
reduces the duration of postoperative tracheal intubation by roughly half. The occurrence of prolonged postoperative mechanical ventilation and myocardial infarction is also reduced by epidural analgesia.
Risks and complications
Risks and complications as they relate to anesthesia are classified
as either morbidity (a disease or disorder that results from anesthesia)
or mortality
(death that results from anesthesia). Quantifying how anesthesia
contributes to morbidity and mortality can be difficult because an
animal's health prior to surgery and the complexity of the surgical
procedure can also contribute to the risks.
Prior to the introduction of anesthesia in the early 19th century, the physiologic stress from surgery caused significant complications and many deaths from shock.
The faster the surgery was, the lower the rate of complications
(leading to reports of very quick amputations). The advent of
anesthesia allowed more complicated and life-saving surgery to be
completed, decreased the physiologic stress of the surgery, but added an
element of risk. It was two years after the introduction of ether
anesthetics that the first death directly related to the use of
anesthesia was reported.
Morbidity can be major (myocardial infarction, pneumonia, pulmonary embolism, kidney failure/chronic kidney disease, postoperative cognitive dysfunction and allergy) or minor (minor nausea,
vomiting, readmission). There is usually overlap in the contributing
factors that lead to morbidity and mortality between the health of the
animals, the type of surgery being performed and the anesthetic. To
understand the relative risk
of each contributing factor, consider that the rate of deaths totally
attributed to the patient's health is 1:870. Compare that to the rate
of deaths totally attributed to surgical factors (1:2860) or anesthesia
alone (1:185,056) illustrating that the single greatest factor in
anesthetic mortality is the health of the patient. These statistics can
also be compared to the first such study on mortality in anesthesia
from 1954, which reported a rate of death from all causes at 1:75 and a
rate attributed to anesthesia alone at 1:2680.
Direct comparisons between mortality statistics cannot reliably be
made over time and across countries because of differences in the
stratification of risk factors, however, there is evidence that
anesthetics have made a significant improvement in safety but to what degree is uncertain.
Rather than stating a flat rate of morbidity or mortality, many
factors are reported as contributing to the relative risk of the
procedure and anesthetic combined. For instance, an operation on a
person who is between the ages of 60–79 years old places the patient at
2.3 times greater risk than someone less than 60 years old. Having an
ASA score of 3, 4 or 5 places the person at 10.7 times greater risk than
someone with an ASA score of 1 or 2. Other variables include age
greater than 80 (3.3 times risk compared to those under 60), gender
(females have a lower risk of 0.8), urgency of the procedure
(emergencies have a 4.4 times greater risk), experience of the person
completing the procedure (less than 8 years experience and/or less than
600 cases have a 1.1 times greater risk) and the type of anesthetic
(regional anesthetics are lower risk than general anesthetics). Obstetrical, the very young and the very old are all at greater risk of complication so extra precautions may need to be taken.
On 14 December 2016, the Food and Drug Administration issued a
Public Safety Communication warning that "repeated or lengthy use of
general anesthetic and sedation drugs during surgeries or procedures in
children younger than 3 years or in pregnant women during their third
trimester may affect the development of children's brains."
The warning was criticized by the American College of Obstetricians and
Gynecologists, which pointed out the absence of direct evidence
regarding use in pregnant women and the possibility that "this warning
could inappropriately dissuade providers from providing medically
indicated care during pregnancy."
Patient advocates noted that a randomized clinical trial would be
unethical, that the mechanism of injury is well-established in animals,
and that studies had shown exposure to multiple uses of anesthetic
significantly increased the risk of developing learning disabilities in
young children, with a hazard ratio of 2.12 (95% confidence interval, 1.26–3.54).
Recovery
The immediate time after anesthesia is called emergence. Emergence from general anesthesia or sedation requires careful monitoring because there is still a risk of complication. Nausea and vomiting are reported at 9.8% but will vary with the type of anesthetic and procedure. There is a need for airway support in 6.8%, there can be urinary retention (more common in those over 50 years of age) and hypotension in 2.7%. Hypothermia,
shivering and confusion are also common in the immediate post-operative
period because of the lack of muscle movement (and subsequent lack of
heat production) during the procedure.
Furthermore, the rare manifestation in the post-anesthetic period may
be the occurrence of functional neurological symptom disorder (FNSD).
Postoperative cognitive dysfunction (also known as POCD and post-anesthetic confusion) is a disturbance in cognition after surgery. It may also be variably used to describe emergence delirium
(immediate post-operative confusion) and early cognitive dysfunction
(diminished cognitive function in the first post-operative week).
Although the three entities (delirium, early POCD and long-term POCD)
are separate, the presence of delirium post-operatively predicts the
presence of early POCD. There does not appear to be an association
between delirium or early POCD and long-term POCD. According to a recent study conducted at the David Geffen School of Medicine at UCLA,
the brain navigates its way through a series of activity clusters, or
"hubs" on its way back to consciousness. Dr. Andrew Hudson, an assistant
professor in anesthesiology states, "Recovery from anesthesia is not
simply the result of the anesthetic 'wearing off,' but also of the brain
finding its way back through a maze of possible activity states to
those that allow conscious experience. Put simply, the brain reboots
itself."
Long-term POCD is a subtle deterioration in cognitive function,
that can last for weeks, months, or longer. Most commonly, relatives of
the person report a lack of attention, memory and loss of interest in
activities previously dear to the person (such as crosswords). In a
similar way, people in the workforce may report an inability to complete
tasks at the same speed they could previously. There is good evidence that POCD occurs after cardiac surgery and the major reason for its occurrence is the formation of microemboli.
POCD also appears to occur in non-cardiac surgery. Its causes in
non-cardiac surgery are less clear but older age is a risk factor for
its occurrence.
History
The first attempts at general anesthesia were probably herbal remedies administered in prehistory. Alcohol is one of the oldest known sedatives and it was used in ancient Mesopotamia thousands of years ago. The Sumerians are said to have cultivated and harvested the opium poppy (Papaver somniferum) in lower Mesopotamia as early as 3400 BCE. The ancient Egyptians had some surgical instruments, as well as crude analgesics and sedatives, including possibly an extract prepared from the mandrake fruit.
In China, Bian Que (Chinese: 扁鹊, Wade–Giles: Pien Ch'iao, c. 300 BCE) was a legendary Chinese internist and surgeon who reportedly used general anesthesia for surgical procedures.Despite this, it was the Chinese physician Hua Tuo
whom historians considered the first verifiable historical figure to
develop a type of mixture of anesthesia, though his recipe has yet to be
fully discovered.
Throughout Europe, Asia, and the Americas, a variety of Solanum species containing potent tropane alkaloids was used for anesthesia. In 13th-century Italy, Theodoric Borgognoni
used similar mixtures along with opiates to induce unconsciousness, and
treatment with the combined alkaloids proved a mainstay of anesthesia
until the 19th century. Local anesthetics were used in Inca civilization where shamans chewed coca leaves and performed operations on the skull while spitting into the wounds they had inflicted to anesthetize. Cocaine was later isolated and became the first effective local anesthetic. It was first used in 1859 by Karl Koller, at the suggestion of Sigmund Freud, in eye surgery in 1884. German surgeon August Bier (1861–1949) was the first to use cocaine for intrathecal anesthesia in 1898. Romanian surgeon Nicolae Racoviceanu-Piteşti (1860–1942) was the first to use opioids for intrathecal analgesia; he presented his experience in Paris in 1901.
The "soporific sponge" ("sleep sponge") used by Arabic physicians was introduced to Europe by the Salerno school of medicine in the late 12th century and by Ugo Borgognoni (1180–1258) in the 13th century. The sponge was promoted and described by Ugo's son and fellow surgeon, Theodoric Borgognoni (1205–1298). In this anesthetic method, a sponge was soaked in a dissolved solution of opium, mandragora,
hemlock juice, and other substances. The sponge was then dried and
stored; just before surgery the sponge was moistened and then held under
the patient's nose. When all went well, the fumes rendered the
individual unconscious.
Sir
Humphry Davy's
Researches chemical and philosophical: chiefly concerning nitrous oxide (1800), pp. 556 and 557 (right), outlining potential anesthetic properties of
nitrous oxide in relieving pain during surgery.
The most famous anesthetic, ether, may have been synthesized as early as the 8th century,
but it took many centuries for its anesthetic importance to be
appreciated, even though the 16th century physician and polymath Paracelsus
noted that chickens made to breathe it not only fell asleep but also
felt no pain. By the early 19th century, ether was being used by humans,
but only as a recreational drug.
Meanwhile, in 1772, English scientist Joseph Priestley discovered the gas nitrous oxide. Initially, people thought this gas to be lethal, even in small doses, like some other nitrogen oxides. However, in 1799, British chemist and inventor Humphry Davy
decided to find out by experimenting on himself. To his astonishment he
found that nitrous oxide made him laugh, so he nicknamed it "laughing
gas".
In 1800 Davy wrote about the potential anesthetic properties of nitrous
oxide in relieving pain during surgery, but nobody at that time pursued
the matter any further.
On 14 November 1804, Hanaoka Seishū, a Japanese doctor, became the first person to successfully perform surgery using general anesthesia. Hanaoka learned traditional Japanese medicine as well as Dutch-imported
European surgery and Chinese medicine. After years of research and
experimentation, he finally developed a formula which he named tsūsensan
(also known as mafutsu-san), which combined Korean morning glory and other herbs.
Hanaoka's success in performing this painless operation soon
became widely known, and patients began to arrive from all parts of
Japan. Hanaoka went on to perform many operations using tsūsensan,
including resection of malignant tumors, extraction of bladder stones, and extremity amputations.
Before his death in 1835, Hanaoka performed more than 150 operations
for breast cancer. However, this finding did not benefit the rest of the
world until 1854 as the national isolation policy of the Tokugawa shogunate prevented Hanaoka's achievements from being publicized until after the isolation ended. Nearly forty years would pass before Crawford Long, who is titled as the inventor of modern anesthetics in the West, used general anesthesia in Jefferson, Georgia.
Long noticed that his friends felt no pain when they injured
themselves while staggering around under the influence of diethyl ether.
He immediately thought of its potential in surgery. Conveniently, a
participant in one of those "ether frolics", a student named James
Venable, had two small tumors he wanted excised. But fearing the pain of
surgery, Venable kept putting the operation off. Hence, Long suggested
that he have his operation while under the influence of ether. Venable
agreed, and on 30 March 1842 he underwent a painless operation. However,
Long did not announce his discovery until 1849.
Horace Wells conducted the first public demonstration of the inhalational anesthetic at the Massachusetts General Hospital in Boston in 1845. However, the nitrous oxide was improperly administered and the person cried out in pain. On 16 October 1846, Boston dentist William Thomas Green Morton gave a successful demonstration using diethyl ether to medical students at the same venue. Morton, who was unaware of Long's previous work, was invited to the Massachusetts General Hospital to demonstrate his new technique for painless surgery. After Morton had induced anesthesia, surgeon John Collins Warren removed a tumor from the neck of Edward Gilbert Abbott. This occurred in the surgical amphitheater now called the Ether Dome.
The previously skeptical Warren was impressed and stated, "Gentlemen,
this is no humbug." In a letter to Morton shortly thereafter, physician
and writer Oliver Wendell Holmes, Sr. proposed naming the state produced "anesthesia", and the procedure an "anesthetic".
Morton at first attempted to hide the actual nature of his anesthetic substance, referring to it as Letheon. He received a US patent for his substance, but news of the successful anesthetic spread quickly by late 1846. Respected surgeons in Europe including Liston, Dieffenbach, Pirogov, and Syme quickly undertook numerous operations with ether. An American-born physician, Boott, encouraged London dentist James Robinson
to perform a dental procedure on a Miss Lonsdale. This was the first
case of an operator-anesthetist. On the same day, 19 December 1846, in
Dumfries Royal Infirmary, Scotland, a Dr. Scott used ether for a
surgical procedure. The first use of anesthesia in the Southern Hemisphere took place in Launceston, Tasmania, that same year. Drawbacks with ether such as excessive vomiting and its explosive flammability led to its replacement in England with chloroform.
Discovered in 1831 by an American physician Samuel Guthrie
(1782–1848), and independently a few months later by Frenchman Eugène
Soubeiran (1797–1859) and Justus von Liebig (1803–1873) in Germany,
chloroform was named and chemically characterized in 1834 by
Jean-Baptiste Dumas (1800–1884). In 1842, Dr Robert Mortimer Glover in London discovered the anaesthetic qualities of chloroform on laboratory animals.
In 1847, Scottish obstetrician James Young Simpson
was the first to demonstrate the anesthetic properties of chloroform on
humans and helped to popularize the drug for use in medicine. This first supply came from local pharmacists, James Duncan and William Flockhart, and its use spread quickly, with 750,000 doses weekly in Britain by 1895. Simpson arranged for Flockhart to supply Florence Nightingale. Chloroform gained royal approval in 1853 when John Snow administered it to Queen Victoria when she was in labor with Prince Leopold.
For the experience of child birth itself, chloroform met all the
Queen's expectations; she stated it was "delightful beyond measure".
Chloroform was not without fault though. The first fatality directly
attributed to chloroform administration was recorded on 28 January 1848
after the death of Hannah Greener.
This was the first of many deaths to follow from the untrained handling
of chloroform. Surgeons began to appreciate the need for a trained
anesthetist. The need, as Thatcher writes, was for an anesthetist to
"(1)Be satisfied with the subordinate role that the work would require,
(2) Make anesthesia their one absorbing interest, (3) not look at the
situation of anesthetist as one that put them in a position to watch and
learn from the surgeons technique (4) accept the comparatively low pay
and (5) have the natural aptitude and intelligence to develop a high
level of skill in providing the smooth anesthesia and relaxation that
the surgeon demanded" These qualities of an anesthetist were often found in submissive medical students and even members of the public. More often, surgeons sought out nurses to provide anesthesia. By the time of the Civil War, many nurses had been professionally trained with the support of surgeons.
John Snow of London published articles from May 1848 onwards "On
Narcotism by the Inhalation of Vapours" in the London Medical Gazette. Snow also involved himself in the production of equipment needed for the administration of inhalational anesthetics, the forerunner of today's anesthesia machines.
Alice Magaw, born in November 1860, is often referred to as "The
Mother of Anesthesia". Her renown as the personal anesthesia provider
for William and Charles Mayo was solidified by Mayo's own words in his
1905 article in which he described his satisfaction with and reliance on
nurse anesthetists: "The question of anaesthesia is a most important
one. We have regular anaesthetists [on] whom we can depend so that I can
devote my entire attention to the surgical work." Magaw kept thorough
records of her cases and recorded these anesthetics. In her publication
reviewing more than 14,000 surgical anesthetics, Magaw indicates she
successfully provided anesthesia without an anesthetic-related death.
Magaw describes
in another article, "We have administered an anesthetic 1,092 times;
ether alone 674 times; chloroform 245 times; ether and chloroform
combined 173 times. I can report that out of this number, 1,092 cases,
we have not had an accident". Magaw's records and outcomes created a
legacy defining that the delivery of anesthesia by nurses would serve
the surgical community without increasing the risks to patients. In
fact, Magaw's outcomes would eclipse those of practitioners today.
The first comprehensive medical textbook on the subject, Anesthesia, was authored in 1914 by anesthesiologist Dr. James Tayloe Gwathmey and the chemist Dr. Charles Baskerville.
This book served as the standard reference for the specialty for
decades and included details on the history of anesthesia as well as the
physiology and techniques of inhalation, rectal, intravenous, and
spinal anesthesia.
Of these first famous anesthetics, only nitrous oxide is still
widely used today, with chloroform and ether having been replaced by
safer but sometimes more expensive general anesthetics, and cocaine by more effective local anesthetics with less abuse potential.
Society and culture
Almost all healthcare providers use anesthetic drugs to some degree,
but most health professions have their own field of specialists in the
field including medicine, nursing and dentistry.
Doctors specializing in anaesthesiology, including perioperative care, development of an anesthetic plan, and the administration of anesthetics are known in the US as anesthesiologists and in the UK, Canada, Australia, and NZ as anaesthetists or anaesthesiologists. All anesthetics in the UK, Australia, New Zealand, Hong Kong and Japan are administered by doctors. Nurse anesthetists also administer anesthesia in 109 nations.
In the US, 35% of anesthetics are provided by physicians in solo
practice, about 55% are provided by anesthesia care teams (ACTs) with
anesthesiologists medically directing certified registered nurse
anesthetists (CRNAs) or anesthesiologist assistants, and about 10% are
provided by CRNAs in solo practice. There can also be anesthesiologist assistants (US) or physicians' assistants (anaesthesia) (UK) who assist with anesthesia.
Special populations
There are many circumstances when anesthesia needs to be altered for special circumstances due to the procedure (such as in
cardiac surgery,
cardiothoracic anesthesiology or
neurosurgery), the patient (such as in
pediatric anesthesia,
geriatric,
bariatric or
obstetrical anesthesia) or special circumstances (such as in
trauma,
prehospital care,
robotic surgery or extreme environments).