Psychological evaluation is a method to assess an individual's behavior, personality, cognitive abilities, and several other domains. A common reason for a psychological evaluation is to identify psychological factors that may be inhibiting a person's ability to think, behave, or regulate emotion functionally or constructively. It is the mental equivalent of physical examination.
Other psychological evaluations seek to better understand the
individual's unique characteristics or personality to predict things
like workplace performance or customer relationship management.
History
Modern psychological evaluation has been around for roughly 200 years, with roots that stem as far back as 2200 B.C. It started in China, and many psychologists throughout Europe worked to
develop methods of testing into the 1900s. The first tests focused on
aptitude. Eventually scientists tried to gauge mental processes in
patients with brain damage, then children with special needs.
Ancient psychological evaluation
Earliest
accounts of evaluation are seen as far back as 2200 B.C. when Chinese
emperors were assessed to determine their fitness for office. These
rudimentary tests were developed over time until 1370 A.D. when an
understanding of classical Confucianism
was introduced as a testing mechanism. As a preliminary evaluation for
anyone seeking public office, candidates were required to spend one day
and one night in a small space composing essays and writing poetry over
assigned topics. Only the top 1% to 7% were selected for higher
evaluations, which required three separate session of three days and
three nights performing the same tasks. This process continued for one
more round until a final group emerged, comprising less than 1% of the
original group, became eligible for public office. The Chinese failure
to validate their selection procedures, along with widespread discontent
over such grueling processes, resulted in the eventual abolishment of
the practice by royal decree.
Development of psychological evaluation in 1800-1900-s
In the 1800s, Hubert von Grashey
developed a battery to determine the abilities of brain-damaged
patients. This test was also not favorable, as it took over 100 hours to
administer. However, this influenced Wilhelm Wundt,
who had the first psychological laboratory in Germany. His tests were
shorter, but used similar techniques. Wundt also measured mental
processes and acknowledged the fact that there are individual
differences between people.
Francis Galton established the first tests in London for measuring IQ.
He tested thousands of people, examining their physical characteristics
as a basis for his results and many of the records remain today. James Cattell
studied with him, and eventually worked on his own with brass
instruments for evaluation. His studies led to his paper "Mental Tests
and Measurements", one of the most famous writings on psychological
evaluation. He also coined the term "mental test" in this paper.
As the 1900s began, Alfred Binet
was also studying evaluation. However, he was more interested in
distinguishing children with special needs from their peers after he
could not prove in his other research that magnets could cure hysteria. He did his research in France, with the help of Theodore Simon.
They created a list of questions that were used to determine if
children would receive regular instruction, or would participate in
special education programs. Their battery was continually revised and
developed, until 1911 when the Binet-Simon questionnaire was finalized for different age levels.
After Binet's death, intelligence testing was further studied by Charles Spearman.
He theorized that intelligence was made up of several different
subcategories, which were all interrelated. He combined all the factors
together to form a general intelligence, which he abbreviated as "g". This led to William Stern's
idea of an intelligence quotient. He believed that children of
different ages should be compared to their peers to determine their
mental age in relation to their chronological age. Lewis Terman
combined the Binet-Simon questionnaire with the intelligence quotient
and the result was the standard test we use today, with an average score
of 100.
The large influx of non-English speaking immigrants into the US
brought about a change in psychological testing that relied heavily on
verbal skills for subjects that were not literate in English, or had
speech/hearing difficulties. In 1913, R.H. Sylvester standardized the
first non-verbal psychological test. In this particular test,
participants fit different shaped blocks into their respective slots on a
Seguin form board. From this test, Knox developed a series of non-verbal psychological
tests that he used while working at the Ellis Island immigrant station
in 1914. In his tests, were a simple wooden puzzle as well as
digit-symbol substitution test where each participant saw digits paired
up with a particular symbol, they were then shown the digits and had to
write in the symbol that was associated with it.
When the United States moved into World War I, Robert M. Yerkes
convinced the government that they should be testing all of the
recruits they were receiving into the Army. The results of the tests
could be used to make sure that the "mentally incompetent" and "mentally exceptional" were assigned to appropriate jobs. Yerkes and his colleagues developed the Army Alpha and Army Beta tests to use on all new recruits. These tests set a precedent for the development of psychological testing for the next several decades.
After seeing the success of the Army standardized tests, college
administration quickly picked up on the idea of group testing to decide
entrance into their institutions. The College Entrance Examination Board
was created to test applicants to colleges across the nation. In 1925,
they developed tests that were no longer essay tests that were very open
to interpretation, but now were objective tests that were also the
first to be scored by machine. These early tests evolved into modern day
College Board tests, like the Scholastic Assessment Test, Graduate Record Examination, and the Law School Admissions Test.
Formal
psychological evaluation consists of standardized batteries of tests
and highly structured clinician-run interviews, while informal
evaluation takes on a completely different tone. In informal evaluation,
assessments are based on unstructured, free-flowing interviews or observations
that allow both the patient and the clinician to guide the content.
Both of these methods have their pros and cons. A highly unstructured
interview and informal observations provide key findings about the
patient that are both efficient and effective. A potential issue with an
unstructured, informal approach is the clinician may overlook certain
areas of functioning or not notice them at all. Or they might focus too much on presenting complaints. The highly
structured interview, although very precise, can cause the clinician to
make the mistake of focusing a specific answer to a specific question
without considering the response in terms of a broader scope or life
context. They may fail to recognize how the patient's answers all fit together.
There are many ways that the issues associated with the interview
process can be mitigated. The benefits to more formal standardized
evaluation types such as batteries and tests are many. First, they
measure a large number of characteristics simultaneously. These include
personality, cognitive, or neuropsychological characteristics. Second,
these tests provide empirically quantified information. The obvious
benefit to this is that we can more precisely measure patient
characteristics as compared to any kind of structured or unstructured
interview. Third, all of these tests have a standardized way of being
scored and being administered. Each patient is presented a standardized stimulus that serves as a
benchmark that can be used to determine their characteristics. These
types of tests eliminate any possibility of bias and produce results
that could be harmful to the patient and cause legal and ethical issues.
Fourth, tests are normed. This means that patients can be
assessed not only based on their comparison to a "normal" individual,
but how they compare to the rest of their peers who may have the same
psychological issues that they face. Normed tests allow the clinician to
make a more individualized assessment of the patient. Fifth,
standardized tests that we commonly use today are both valid and
reliable. We know what specific scores mean, how reliable they are, and how the results will affect the patient.
Most clinicians agree that a balanced battery of tests is the
most effective way of helping patients. Clinicians should not become
victims of blind adherence to any one particular method. A balanced battery of tests allows there to be a mix of formal testing
processes that allow the clinician to start making their assessment,
while conducting more informal, unstructured interviews with the same
patient may help the clinician to make more individualized evaluations
and help piece together what could potentially be a very complex,
unique-to-the-individual kind of issue or problem .
Modern uses
Psychological assessment is most often used in the psychiatric, medical, legal, educational, or psychological clinic settings. The types of assessments and the purposes for them differ among these settings.
In the psychiatric
setting, the common needs for assessment are to determine risks,
whether a person should be admitted or discharged, the location the
patients should be held, as well as what therapy the patient should be
receiving. Within this setting, the psychologists need to be aware of the legal
responsibilities that what they can legally do in each situation.
Within a medical setting, psychological assessment is used to
find a possible underlying psychological disorder, emotional factors
that may be associated with medical complaints, assessment for
neuropsychological deficit, psychological treatment for chronic pain,
and the treatment of chemical dependency.
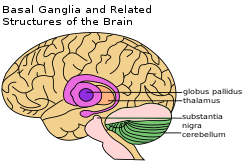
There has been greater importance placed on the patient's
neuropsychological status as neuropsychologists are becoming more
concerned with the functioning of the brain.
Psychological assessment also has a role in the legal setting.
Psychologists might be asked to assess the reliability of a witness, the
quality of the testimony a witness gives, the competency of an accused
person, or determine what might have happened during a crime. They also
may help support a plea of insanity or to discount a plea. Judges may
use the psychologist's report to change the sentence of a convicted
person, and parole officers work with psychologists to create a program
for the rehabilitation of a parolee. Problematic areas for psychologists
include predicting how dangerous a person will be. The predictive
accuracy of these assessments is debated; however, there is often a need for this prediction to prevent dangerous people from returning to society.
Psychologists may also be called on to assess a variety of things
within an education setting. They may be asked to assess strengths and
weaknesses of children who are having difficulty in the school systems,
assess behavioral difficulties, assess a child's responsiveness to an
intervention, or to help create an educational plan for a child. The
assessment of children also allows for the psychologists to determine if
the child will be willing to use the resources that may be provided.
In a psychological clinic setting, psychological assessment can
be used to determine characteristics of the client that can be useful
for developing a treatment plan. Within this setting, psychologists
often are working with clients who may have medical or legal problems or
sometimes students who were referred to this setting from their school
psychologist.
Some psychological assessments have been validated for use when administered via computer or the Internet. However, caution must be applied to these test results, as it is possible to fake in electronically mediated assessment. Many electronic assessments do not truly measure what is claimed, such
as the Meyers-Briggs personality test. Although one of the most well
known personality assessments, it has been found both invalid and
unreliable by many psychological researches, and should be used with
caution.
Within clinical psychology,
the "clinical method" is an approach to understanding and treating
mental disorders that begins with a particular individual's personal
history and is designed around that individual's psychological needs.
It is sometimes posed as an alternative approach to the experimental
method which focuses on the importance of conducting experiments in
learning how to treat mental disorders, and the differential method
which sorts patients by class (gender, race, income, age, etc.) and
designs treatment plans based around broad social categories.
Taking a personal history along with clinical examination allow the health practitioners to fully establish a clinical diagnosis. A medical history
of a patient provides insights into diagnostic possibilities as well as
the patient's experiences with illnesses. The patients will be asked
about current illness and the history of it, past medical history and
family history, other drugs or dietary supplements being taken,
lifestyle, and allergies. The inquiry includes obtaining information about relevant diseases or conditions of other people in their family. Self-reporting methods may be used, including questionnaires, structured interviews and rating scales.
Personality Assessment
Personality traits
are an individual's enduring manner of perceiving, feeling, evaluating,
reacting, and interacting with other people specifically, and with
their environment more generally. Because reliable and valid personality inventories give a relatively
accurate representation of a person's characteristics, they are
beneficial in the clinical setting as supplementary material to standard
initial assessment procedures such as a clinical interview; review of
collateral information, e.g., reports from family members; and review of
psychological and medical treatment records.
MMPI
History
Developed by Starke R. Hathaway, PhD, and J. C. McKinley, MD, The Minnesota Multiphasic Personality Inventory (MMPI) is a personality inventory used to investigate not only personality, but also psychopathology. The MMPI was developed using an empirical, atheoretical approach. This
means that it was not developed using any of the frequently changing
theories about psychodynamics at the time. There are two variations of
the MMPI administered to adults, the MMPI-2 and the MMPI-2-RF, and two
variations administered to teenagers, the MMPI-A and MMPI-A-RF. This
inventory's validity has been confirmed by Hiller, Rosenthal, Bornstein,
and Berry in their 1999 meta-analysis. Throughout history the MMPI in
its various forms has been routinely administered in hospitals, clinical
settings, prisons, and military settings.
MMPI-2
The MMPI-2 consists of 567 true or false questions aimed at measuring the reporting person's psychological wellbeing. The MMPI-2 is commonly used in clinical settings and occupational
health settings. There is a revised version of the MMPI-2 called the
MMPI-2-RF (MMPI-2 Restructured Form). The MMPI-2-RF is not intended to be a replacement for the MMPI-2, but
is used to assess patients using the most current models of
psychopathology and personality.
MMPI-2 and MMPI-2-RF Scales
| MMPI-2
|
567
|
120
|
Validity Indicators, Superlative Self-Presentation Subscales,
Clinical Scales, Restructured Clinical (RC) Scales, Content Scales,
Content Component Scales, Supplementary Scales, Clinical Subscales
(Harris-Lingoes and Social Introversion Subscales)
|
| MMPI-2-RF
|
338
|
51
|
Validity, Higher-Order (H-O), Restructured Clinical (RC), Somatic,
Cognitive, Internalizing, Externalizing, Interpersonal, Interest,
Personality Psychopathology Five (PSY-5)
|
MMPI-A
The MMPI-A was published in 1992 and consists of 478 true or false questions. This version of the MMPI is similar to the MMPI-2 but used for
adolescents (age 14–18) rather than for adults. The restructured form of
the MMPI-A, the MMPI-A-RF, was published in 2016 and consists of 241
true or false questions that can understood with a sixth grade reading
level. Both the MMPI-A and MMPI-A-RF are used to assess adolescents for
personality and psychological disorders, as well as to evaluate
cognitive processes.
MMPI-A and MMPI-A-RF Scales
| MMPI-A
|
478
|
105
|
Validity Indicators, Clinical Scales, Clinical Subscales
(Harris-Lingoes and Social Introversion Subscales), Content Scales,
Content Component Scales, Supplementary Scales
|
| MMPI-A-RF
|
241
|
48
|
Validity, Higher-Order (H-O), Restructured Clinical (RC),
Somatic/Cognitive, Internalizing, Externalizing, Interpersonal,
Personality Psychopathology Five (PSY-5)
|
NEO Personality Inventory
The NEO Personality Inventory was developed by Paul Costa Jr. and Robert R. McCrae
in 1978. When initially created, it only measured three of the Big Five
personality traits: Neuroticism, Openness to Experience, and
Extroversion. The inventory was then renamed as the
Neuroticism-Extroversion-Openness Inventory (NEO-I). It was not until
1985 that Agreeableness and Conscientiousness were added to the
personality assessment. With all Big Five personality traits being
assessed, it was then renamed as the NEO Personality Inventory. Research
for the NEO-PI continued over the next few years until a revised manual
with six facets for each Big Five trait was published in 1992. In the 1990s, now called the NEO PI-R, issues were found with the
personality inventory. The developers of the assessment found it to be
too difficult for younger people, and another revision was done to
create the NEO PI-3.
The NEO Personality Inventory is administered in two forms:
self-report and observer report. It consists of 240 personality items
and a validity item. It can be administered in roughly 35–45 minutes.
Every item is answered on a Likert scale, widely known as a scale from
Strongly Disagree to Strongly Agree. If more than 40 items are missing
or more than 150 responses or less than 50 responses are Strongly
Agree/Disagree, the assessment should be viewed with great caution and
has the potential to be invalid. In the NEO report, each trait's T score is recorded along with the
percentile they rank on compared to all data recorded for the
assessment. Then, each trait is broken up into their six facets along
with raw score, individual T-scores, and percentile. The next page goes
on to list what each score means in words as well as what each facet
entails. The exact responses to questions are given in a list as well as
the validity response and amount of missing responses.
When an individual is given their NEO report, it is important to
understand specifically what the facets are and what the corresponding
scores mean.
- Neuroticism
- Anxiety
- High scores suggest nervousness, tenseness, and fearfulness. Low scores suggest feeling relaxed and calm.
- Angry Hostility
- High scores suggest feeling anger and frustration often. Low scores suggest being easy-going.
- Depression
- High scores suggest feeling guilty, sad, hopeless, and lonely.
Low scores suggest less feeling of that of someone who scores highly,
but not necessarily being light-hearted and cheerful.
- Self-consciousness
- High scores suggest shame, embarrassment, and sensitivity. Low
scores suggest being less affected by others' opinions, but not
necessarily having good social skills or poise.
- Impulsiveness
- High scores suggest the inability to control cravings and urges. Low scores suggest easy resistance to such urges.
- Vulnerability
- High scores suggest inability to cope with stress, being
dependent, and feeling panicked in high stress situations. Low scores
suggest capability to handle stressful situations.
- Extraversion
- Warmth
- High scores suggest friendliness and affectionate behavior. Low
scores suggest being more formal, reserved, and distant. A low score
does not necessarily mean being hostile or lacking compassion.
- Gregariousness
- High scores suggest wanting the company of others. Low scores tend to be from those who avoid social stimulation.
- Assertiveness
- High scores suggest a forceful and dominant person who lacks
hesitation. Low scores suggest are more passive and try not to stand out
in a crowd.
- Activity
- High scores suggest a more energetic and upbeat personality and
lead a quicker paced lifestyle. Low scores suggest the person is more
leisurely, but does not imply being lazy or slow.
- Excitement-Seeking
- High scores suggest a person who seeks and craves excitement and
is similar to those with high sensation seeking. Low scores seek a less
exciting lifestyle and come off more boring.
- Positive Emotions
- High scores suggest the tendency to feel happier, laugh more,
and are optimistic. Low scorers are not necessarily unhappy, but more so
are less high-spirited and are more pessimistic.
- Openness to Experience
- Fantasy
- Those who score high in fantasy have a more creative imagination
and daydream frequently. Low scores suggest a person who lives more in
the moment.
- Aesthetics
- High scores suggest a love and appreciation for art and physical
beauty. These people are more emotionally attached to music, artwork,
and poetry. Low scorers have a lack of interest in the arts.
- Feelings
- High scorers have a deeper ability to experience emotion and see
their emotions as more important than those who score low on this
facet. Low scorers are less expressive.
- Actions
- High scores suggest a more open-mindedness to traveling and
experiencing new things. These people prefer novelty over a routine
life. Low scorers prefer a scheduled life and dislike change.
- Ideas
- Active pursuit of knowledge, high curiosity, and the enjoyment
of brain teasers and philosophical are common of those who score high on
this facet. Those who score lower are not necessarily less intelligent,
nor does a high score imply high intelligence. However, those who score
lower are more narrow in their interests and have low curiosity.
- Values
- High scorers are more investigative of political, social, and
religious values. Those who score lower and more accepting of authority
and honor more traditional values. High scorers are more typically
liberal while lower scorers are more typically conservative.
- Agreeableness
- Trust
- High scores are more trusting of others and believe others are
honest and have good intentions. Low scorers are more skeptical,
cynical, and assumes others are dishonest and/or dangerous.
- Straightforwardness
- Those who score high in this facet are more sincere and frank.
Low scorers are more deceitful and more willing to manipulate others,
but this does not mean they should be labeled as a dishonest or
manipulative person.
- Altruism
- High scores suggest a person concerned with the well-being of
others and show it through generosity, willingness to help others, and
volunteering for those less fortunate. Low scores suggest a more
self-centered person who is less willing to go out of their way to help
others.
- Compliance
- High scorers are more inclined to avoid conflict and tend to
forgive easily. Low scores suggest a more aggressive personality and a
love for competition.
- Modesty
- High scorers are more humble, but not necessarily lacking in
self-esteem or confidence. Low scorers believe they're more superior
than others and may come off as more conceited.
- Tender-Mindedness
- This facet scales one's concern for others and their ability to
empathize. High scorers are more moved by others' emotions, while low
scorers are more hardheaded and typically consider themselves realists.
- Conscientiousness
- Competence
- High scores suggest one is capable, sensible, prudent,
effective, and are well-prepared to deal with whatever happens in life.
Low scores suggest a potential lower self-esteem and are often
unprepared.
- Order
- High scorers are more neat and tidy, while low scorers lack organization and are unmethodical.
- Dutifulness
- Those who score highly in this facet are more strict about their
ethical principles and are more dependable. Low scorers are less
reliable and are more casual about their morals.
- Achievement Striving
- Those who score highly in this facet have higher aspirations and
work harder to achieve their goals. However, they may be too invested
in their work and become a workaholic. Low scorers are much less
ambitious and perhaps even lazy. They are often content with their lack
of goal-seeking.
- Self-Discipline
- High scorers complete whatever task is assigned to them and are
self-motivated. Low scorers often procrastinate and are easily
discouraged.
- Deliberation
- High scorers tend to think more than low scorers before acting.
High scorers are more cautious and deliberate while low scorers are more
hasty and act without considering the consequences.
HEXACO-PI
The HEXACO-PI,
developed by Lee and Ashton in the early 2000s, is a personality
inventory used to measure six different dimensions of personality which
have been found in lexical studies across various cultures. There are
two versions of the HEXACO: the HEXACO-PI and the HEXACO-PI-R which are
examined with either self reports or observer reports. The HEXACO-PI-R
has forms of three lengths: 200 items, 100 items, and 60 items. Items
from each form are grouped to measure scales of more narrow personality
traits, which are them grouped into broad scales of the six dimensions:
honesty & humility (H), emotionality (E), Extraversion (X),
agreeableness (A), conscientiousness (C), and openness to experience
(O).The HEXACO-PI-R includes various traits associated with neuroticism
and can be used to help identify trait tendencies. One table which give
examples of typically high loaded adjectives on the six factors of
HEXACO can be found in Ashton's book "Individual Differences and
Personality"
Adjective relating to the six factors within the HEXACO structure
| Personality Factor
|
Narrow Personality Traits
|
Related Adjectives
|
| Honesty-Humility
|
Sincerity, fairness, greed-avoidance, modesty
|
Sincere, honest, faithful/loyal, modest/unassuming, fair-minded
versus sly, deceitful, greedy, pretentious, hypocritical, boastful,
pompous
|
| Emotionality
|
Fearfulness, anxiety, depenence, sentimentality
|
Emotional, oversensitive, sentimental, fearful, anxious, vulnerable versus brave, tough, independent, self-assured, stable
|
| Extraversion
|
Social self-esteem, social boldness, sociability, liveliness
|
Outgoing, lively, extraverted, sociable, talkative, cheerful, active
versus shy, passive, withdrawn, introverted, quiet, reserved
|
| Agreeableness
|
Forgivingness, gentleness, flexibility, patience
|
Patient, tolerant, peaceful, mild, agreeable, lenient, gentle versus ill-tempered, quarrelsome, stubborn, choleric
|
| Conscientiousness
|
Organization, diligence, perfectionism, prudence
|
Organized, disciplined, diligent, careful, thorough, precise verus
sloppy, negligent, reckless, lazy, irresponsible, absent-minded
|
| Openness to Experience
|
Aesthetic appreciation, inquisitiveness, creativity, unconventionality
|
Intellectual, creative, unconventional, innovative, ironic versus shallow, unimaginative, conventional
|
One benefit of using the HEXACO is that of the facet of neuroticism
within the factor of emotionality: trait neuroticism has been shown to
have a moderate positive correlation with people with anxiety and
depression. The identification of trait neuroticism on a scale, paired
with anxiety, and/or depression is beneficial in a clinical setting for
introductory screenings some personality disorders. Because the HEXACO
has facets which help identify traits of neuroticism, it is also a
helpful indicator of the dark triad.
Temperament Assessment
In
contrast to personality, i.e. the concept that relates to culturally-
and socially-influenced behaviour and cognition, the concept of
temperament' refers to biologically and neurochemically-based individual
differences in behaviour. Unlike personality, temperament is relatively
independent of learning, system of values, national, religious and
gender identity and attitudes. There are multiple tests for evaluation
of temperament traits (reviewed, for example, in, majority of which were developed arbitrarily from opinions of early
psychologists and psychiatrists but not from biological sciences.
There are only two temperament tests that were based on neurochemical
hypotheses: The Temperament and Character Inventory (TCI) and the Trofimova's Structure of Temperament Questionnaire-Compact (STQ-77). The STQ-77 is based on the neurochemical framework Functional Ensemble of Temperament
that summarizes the contribution of main neurochemical
(neurotransmitter, hormonal and opioid) systems to behavioural
regulation. The STQ-77 assesses 12 temperament traits linked to the neurochemical
components of the FET. The STQ-77 is freely available for non-commercial
use in 24 languages for testing in adults and several language versions
for testing children
Pseudopsychology (pop psychology) in assessment
Although
there have been many great advancements in the field of psychological
evaluation, some issues have also developed. One of the main problems
in the field is pseudopsychology, also called pop psychology.
Psychological evaluation is one of the biggest aspects in pop
psychology. In a clinical setting, patients are not aware that they are
not receiving correct psychological treatment, and that belief is one
of the main foundations of pseudopsychology. It is largely based upon
the testimonies of previous patients, the avoidance of peer review (a
critical aspect of any science), and poorly set up tests, which can
include confusing language or conditions that are left up to
interpretation.
Pseudopsychology can also occur when people claim to be psychologists, but lack qualifications. A prime example of this is found in quizzes that can lead to a variety
of false conclusions. These can be found in magazines, online, or just
about anywhere accessible to the public. They usually consist of a
small number of questions designed to tell the participant things about
themselves. These often have no research or evidence to back up any
claims made by the quizzes.
Ethics
Concerns
about privacy, cultural biases, tests that have not been validated, and
inappropriate contexts have led groups such as the American Educational Research Association (AERA) and the American Psychological Association (APA) to publish guidelines for examiners in regards to assessment. The American Psychological Association states that a client must give
permission to release any of the information that may come from a
psychologist. The only exceptions to this are in the case of minors, when the clients
are a danger to themselves or others, or if they are applying for a job
that requires this information. Also, the issue of privacy occurs
during the assessment itself. The client has the right to say as much or
little as they would like, however they may feel the need to say more
than they want or even may accidentally reveal information they would
like to keep private.
Guidelines have been put in place to ensure the psychologist
giving the assessments maintains a professional relationship with the
client since their relationship can impact the outcomes of the
assessment. The examiner's expectations may also influence the client's
performance in the assessments.
The validity and reliability of the tests being used also can
affect the outcomes of the assessments being used. When psychologists
are choosing which assessments they are going to use, they should pick
one that will be most effective for what they are looking at. Also, it
is important for the psychologists are aware of the possibility of the
client, either consciously or unconsciously, faking answers and consider
use of tests that have validity scales within them.