| Selective serotonin reuptake inhibitor | |
|---|---|
| Drug class | |
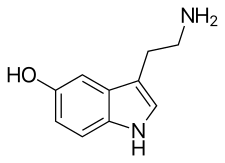
Serotonin, the neurotransmitter that is involved in the mechanism of action of SSRIs.
| |
| Class identifiers | |
| Synonyms | Serotonin-specific reuptake inhibitors, serotonergic antidepressants |
| Use | Major depressive disorder, anxiety disorders |
| ATC code | N06AB |
| Biological target | Serotonin transporter |
| Clinical data | |
| Drugs.com | Drug Classes |
| Consumer Reports | Best Buy Drugs |
| External links | |
| MeSH | D017367 |
| In Wikidata | |
Selective serotonin reuptake inhibitors (SSRIs) are a class of drugs that are typically used as antidepressants in the treatment of major depressive disorder and anxiety disorders.
The exact mechanism of action of SSRIs is unknown. They are believed to increase the extracellular level of the neurotransmitter serotonin by limiting its reabsorption (reuptake) into the presynaptic cell, increasing the level of serotonin in the synaptic cleft available to bind to the postsynaptic receptor. They have varying degrees of selectivity for the other monoamine transporters, with pure SSRIs having only weak affinity for the norepinephrine and dopamine transporters.
SSRIs are the most widely prescribed antidepressants in many countries. The efficacy of SSRIs in mild or moderate cases of depression has been disputed and may be outweighed by side effects.
Medical uses
The main indication for SSRIs is major depressive disorder; however, they are frequently prescribed for anxiety disorders, such as social anxiety disorder, panic disorder, obsessive–compulsive disorder (OCD), eating disorders, chronic pain, and, in some cases, for posttraumatic stress disorder (PTSD). They are also frequently used to treat depersonalization disorder, although generally with poor results.
Depression
Antidepressants are recommended by the National Institute for Health and Care Excellence
(NICE) as a first-line treatment of severe depression and for the
treatment of mild-to-moderate depression that persists after
conservative measures such as cognitive therapy. They recommend against their routine use in those who have chronic health problems and mild depression.
There has been controversy regarding the efficacy of
antidepressants in treating depression depending on its severity and
duration.
- Two meta-analyses published in 2008 (Kirsch) and 2010 (Fournier) found that in mild and moderate depression, the effect of SSRIs is small or none compared to placebo, while in very severe depression the effect of SSRIs is between "relatively small" and "substantial". The 2008 meta-analysis combined 35 clinical trials submitted to the Food and Drug Administration (FDA) before licensing of four newer antidepressants (including the SSRIs paroxetine and fluoxetine, the non-SSRI antidepressant nefazodone, and the serotonin and norepinephrine reuptake inhibitor (SNRI) venlafaxine). The authors attributed the relationship between severity and efficacy to a reduction of the placebo effect in severely depressed patients, rather than an increase in the effect of the medication. Some researchers have questioned the statistical basis of this study suggesting that it underestimates the effect size of antidepressants.
- A 2010 comprehensive review conducted by NICE concluded that antidepressants have no advantage over placebo in the treatment of short-term mild depression, but that the available evidence supported the use of antidepressants in the treatment of dysthymia and other forms of chronic mild depression.
- A 2012 meta-analysis of fluoxetine and venlafaxine concluded that statistically and clinically significant treatment effects were observed for each drug relative to placebo irrespective of baseline depression severity.
- In 2014 the U.S. FDA published a systematic review of all antidepressant maintenance trials submitted to the agency between 1985 and 2012. The authors concluded that maintenance treatment reduced the risk of relapse by 52% compared to placebo, and that this effect was primarily due to recurrent depression in the placebo group rather than a drug withdrawal effect.
- A 2017 systematic review stated that "SSRIs versus placebo seem to have statistically significant effects on depressive symptoms, but the clinical significance of these effects seems questionable and all trials were at high risk of bias. Furthermore, SSRIs versus placebo significantly increase the risk of both serious and non-serious adverse events. Our results show that the harmful effects of SSRIs versus placebo for major depressive disorder seem to outweigh any potentially small beneficial effects". The review was criticized for being inaccurate and misleading.
- In 2018 a systematic review of 21 different antidepressants found that all analysed antidepressants were more efficacious than placebo in adults with major depressive disorder. Effect sizes measured at 8-weeks after treatment onset however were modest.
There does not appear to be a big difference in the effectiveness
between medications in the second generation antidepressants (SSRIs and
SNRIs).
In children there are concerns around the quality of the evidence on the meaningfulness of benefits seen. If a medication is used, fluoxetine appears to be first line.
Generalized anxiety disorder
SSRIs are recommended by the National Institute for Health and Care Excellence (NICE) for the treatment of generalized anxiety disorder
(GAD) that has failed to respond to conservative measures such as
education and self-help activities. GAD is a common disorder of which
the central feature is excessive worry about a number of different
events. Key symptoms include excessive anxiety about multiple events and
issues, and difficulty controlling worrisome thoughts that persists for
at least 6 months.
Antidepressants provide a modest-to-moderate reduction in anxiety in GAD, and are superior to placebo in treating GAD. The efficacy of different antidepressants is similar.
Obsessive–compulsive disorder
SSRIs are a second line treatment of adult obsessive–compulsive disorder
(OCD) with mild functional impairment and as first line treatment for
those with moderate or severe impairment. In children, SSRIs can be
considered a second line therapy in those with moderate-to-severe
impairment, with close monitoring for psychiatric adverse effects.
SSRIs are efficacious in the treatment of OCD; patients treated with
SSRIs are about twice as likely to respond to treatment as those treated
with placebo.
Efficacy has been demonstrated both in short-term treatment trials of 6
to 24 weeks and in discontinuation trials of 28 to 52 weeks duration.
Eating disorders
Anti-depressants are recommended as an alternative or additional first step to self-help programs in the treatment of bulimia nervosa.
SSRIs (fluoxetine in particular) are preferred over other
anti-depressants due to their acceptability, tolerability, and superior
reduction of symptoms in short-term trials. Long-term efficacy remains
poorly characterized.
Similar recommendations apply to binge eating disorder. SSRIs provide short-term reductions in binge eating behavior, but have not been associated with significant weight loss.
Clinical trials have generated mostly negative results for the use of SSRIs in the treatment of anorexia nervosa. Treatment guidelines from the National Institute of Health and Clinical Excellence
recommend against the use of SSRIs in this disorder. Those from the
American Psychiatric Association note that SSRIs confer no advantage
regarding weight gain, but that they may be used for the treatment of
co-existing depressive, anxiety, or OCD.
Stroke recovery
SSRIs have been used in the treatment of stroke
patients, including those with and without symptoms of depression. A
recent meta-analysis of randomized, controlled clinical trials found a
statistically significant effect of SSRIs on dependence, neurological
deficit, depression, and anxiety. There was no statistically significant effect on death, motor deficits, or cognition.
Premature ejaculation
SSRIs are effective for the treatment of premature ejaculation. Chronic administration is more efficacious than on demand use.
Side effects
Side effects
vary among the individual drugs of this class. However, certain types
of adverse effects are found broadly among most if not all members of
this class:
- increased risk of bone fractures by 1.7 fold
- akathisia
- suicidal ideation (thoughts of suicide)
- photosensitivity
Sexual dysfunction
SSRIs can cause various types of sexual dysfunction such as anorgasmia, erectile dysfunction, diminished libido, genital numbness, and sexual anhedonia (pleasureless orgasm). Sexual problems are common with SSRIs. Poor sexual function is also one of the most common reasons people stop the medication.
In some cases, symptoms of sexual dysfunction may persist after discontinuation of SSRIs.
The mechanism by which SSRIs may cause sexual side effects is not
well understood as of 2015. The range of possible mechanisms includes
(1) nonspecific neurological effects (e.g., sedation) that globally
impair behavior including sexual function; (2) specific effects on brain
systems mediating sexual function; (3) specific effects on peripheral
tissues and organs, such as the penis, that mediate sexual function; and
(4) direct or indirect effects on hormones mediating sexual function. Management strategies include: for erectile dysfunction the addition of a PDE5 inhibitor such as sildenafil; for decreased libido, possibly adding or switching to bupropion; and for overall sexual dysfunction, switching to nefazodone.
A number of non-SSRI drugs are not associated with sexual side effects (such as bupropion, mirtazapine, tianeptine, agomelatine and moclobemide).
Several studies have suggested that SSRIs may adversely affect semen quality.
Priapism can also be caused sometimes.
Cardiac
SSRIs do not appear to affect the risk of coronary heart disease (CHD) in those without a previous diagnosis of CHD.
A large cohort study suggested no substantial increase in the risk of
cardiac malformations attributable to SSRI usage during the first
trimester of pregnancy. A number of large studies of people without known pre-existing heart disease have reported no EKG changes related to SSRI use. The recommended maximum daily dose of citalopram and escitalopram was reduced due to concerns with QT interval prolongation. In overdose, fluoxetine has been reported to cause sinus tachycardia, myocardial infarction, junctional rhythms and trigeminy. Some authors have suggested electrocardiographic monitoring in patients with severe pre-existing cardiovascular disease who are taking SSRIs.
Bleeding
SSRIs interact with anticoagulants, like warfarin, and antiplatelet drugs, like aspirin. This includes an increased risk of GI bleeding, and post operative bleeding. The relative risk of intracranial bleeding is increased, but the absolute risk is very low. SSRIs are known to cause platelet dysfunction.
This risk is greater in those who are also on anticoagulants,
antiplatelet agents and NSAIDs (nonsteroidal anti-inflammatory drugs),
as well as with the co-existence of underlying diseases such as
cirrhosis of the liver or liver failure.
Fracture risk
Evidence
from longitudinal, cross-sectional, and prospective cohort studies
suggests an association between SSRI usage at therapeutic doses and a
decrease in bone mineral density, as well as increased fracture risk, a relationship that appears to persist even with adjuvant bisphosphonate therapy.
However, because the relationship between SSRIs and fractures is based
on observational data as opposed to prospective trials, the phenomenon
is not definitively causal.
There also appears to be an increase in fracture-inducing falls with
SSRI use, suggesting the need for increased attention to fall risk in
elderly patients using the medication. The loss of bone density does not appear to occur in younger patients taking SSRIs.
Discontinuation syndrome
Serotonin reuptake inhibitors should not be abruptly discontinued
after extended therapy, and whenever possible, should be tapered over
several weeks to minimize discontinuation-related symptoms which may
include nausea, headache, dizziness, chills, body aches, paresthesias,
insomnia, and electric shock-like sensations. Paroxetine may produce
discontinuation-related symptoms at a greater rate than other SSRIs,
though qualitatively similar effects have been reported for all SSRIs. Discontinuation effects appear to be less for fluoxetine, perhaps owing
to its long half-life and the natural tapering effect associated with
its slow clearance from the body. One strategy for minimizing SSRI
discontinuation symptoms is to switch the patient to fluoxetine and then
taper and discontinue the fluoxetine.
Serotonin syndrome
Serotonin syndrome is typically caused by the use of two or more serotonergic drugs, including SSRIs. Serotonin syndrome is a short-lived condition that can range from mild (most common) to deadly. Mild symptoms may consist of increased heart rate, shivering, sweating, dilated pupils, myoclonus (intermittent jerking or twitching), as well as overresponsive reflexes. Concomitant use of an SSRI or selective norepinephrine reuptake inhibitor for depression with a triptan for migraine does not appear to heighten the risk of the serotonin syndrome.
Suicide risk
Children and adolescents
Meta
analyses of short duration randomized clinical trials have found that
SSRI use is related to a higher risk of suicidal behavior in children
and adolescents. For instance, a 2004 U.S. Food and Drug Administration (FDA) analysis of clinical trials on children with major depressive disorder found statistically significant increases of the risks of "possible suicidal ideation and suicidal behavior" by about 80%, and of agitation and hostility by about 130%. According to the FDA, the heightened risk of suicidality is within the first one to two months of treatment. The National Institute for Health and Care Excellence (NICE) places the excess risk in the "early stages of treatment".
The European Psychiatric Association places the excess risk in the
first two weeks of treatment and, based on a combination of
epidemiological, prospective cohort, medical claims, and randomized
clinical trial data, concludes that a protective effect dominates after
this early period. A 2014 Cochrane review found that at six to nine
months, suicidal ideation remained higher in children treated with
antidepressants compared to those treated with psychological therapy.
A recent comparison of aggression and hostility occurring during
treatment with fluoxetine to placebo in children and adolescents found
that no significant difference between the fluoxetine group and a
placebo group.
There is also evidence that higher rates of SSRI prescriptions are
associated with lower rates of suicide in children, though since the
evidence is correlational, the true nature of the relationship is unclear.
In 2004, the Medicines and Healthcare products Regulatory Agency (MHRA) in the United Kingdom judged fluoxetine (Prozac) to be the only antidepressant that offered a favorable risk-benefit ratio
in children with depression, though it was also associated with a
slight increase in the risk of self-harm and suicidal ideation. Only two SSRIs are licensed for use with children in the UK, sertraline (Zoloft) and fluvoxamine (Luvox), and only for the treatment of obsessive–compulsive disorder. Fluoxetine is not licensed for this use.
Adults
It is unclear whether SSRIs affect the risk of suicidal behavior in adults.
- A 2005 meta-analysis of drug company data found no evidence that SSRIs increased the risk of suicide; however, important protective or hazardous effects could not be excluded.
- A 2005 review observed that suicide attempts are increased in those who use SSRIs as compared to placebo and compared to therapeutic interventions other than tricyclic antidepressants. No difference risk of suicide attempts was detected between SSRIs versus tricyclic antidepressants.
- On the other hand, a 2006 review suggests that the widespread use of antidepressants in the new "SSRI-era" appears to have led to a highly significant decline in suicide rates in most countries with traditionally high baseline suicide rates. The decline is particularly striking for women who, compared with men, seek more help for depression. Recent clinical data on large samples in the US too have revealed a protective effect of antidepressant against suicide.
- A 2006 meta-analysis of random controlled trials suggests that SSRIs increase suicide ideation compared with placebo. However, the observational studies suggest that SSRIs did not increase suicide risk more than older antidepressants. The researchers stated that if SSRIs increase suicide risk in some patients, the number of additional deaths is very small because ecological studies have generally found that suicide mortality has declined (or at least not increased) as SSRI use has increased.
- An additional meta-analysis by the FDA in 2006 found an age-related effect of SSRI's. Among adults younger than 25 years, results indicated that there was a higher risk for suicidal behavior. For adults between 25 and 64, the effect appears neutral on suicidal behavior but possibly protective for suicidal behavior for adults between the ages of 25 and 64. For adults older than 64, SSRI's seem to reduce the risk of both suicidal behavior.
- In 2016 a study criticized the effects of the FDA Black Box suicide warning inclusion in the prescription. The authors discussed the suicide rates might increase also as a consequence of the warning.
Pregnancy and breastfeeding
SSRI
use in pregnancy has been associated with a variety of risks with
varying degrees of proof of causation. As depression is independently
associated with negative pregnancy outcomes, determining the extent to
which observed associations between antidepressant use and specific
adverse outcomes reflects a causative relationship has been difficult in
some cases. In other cases, the attribution of adverse outcomes to antidepressant exposure seems fairly clear.
SSRI use in pregnancy is associated with an increased risk of spontaneous abortion of about 1.7-fold. Use is also associated preterm birth.
A systematic review of the risk of major birth defects in
antidepressant-exposed pregnancies found a small increase (3% to 24%) in
the risk of major malformations and a risk of cardiovascular birth
defects that did not differ from non-exposed pregnancies.
A study of fluoxetine-exposed pregnancies found a 12% increase in the
risk of major malformations that just missed statistical significance.
Other studies have found an increased risk of cardiovascular birth
defects among depressed mothers not undergoing SSRI treatment,
suggesting the possibility of ascertainment bias, e.g. that worried
mothers may pursue more aggressive testing of their infants.
Another study found no increase in cardiovascular birth defects and a
27% increased risk of major malformations in SSRI exposed pregnancies.
The FDA issued a statement on July 19, 2006 stating nursing
mothers on SSRIs must discuss treatment with their physicians. However,
the medical literature on the safety of SSRIs has determined that some
SSRIs like Sertraline and Paroxetine are considered safe for
breastfeeding.
Neonatal abstinence syndrome
Several studies have documented neonatal abstinence syndrome,
a syndrome of neurological, gastrointestinal, autonomic, endocrine
and/or respiratory symptoms among a large minority of infants with
intrauterine exposure. These syndromes are short-lived, but insufficient
long-term data is available to determine whether there are long-term
effects.
Persistent pulmonary hypertension
Persistent pulmonary hypertension (PPHN) is a serious and life-threatening, but very rare, lung condition that occurs soon after birth of the newborn. Newborn babies with PPHN have high pressure in their lung blood vessels
and are not able to get enough oxygen into their bloodstream. About 1
to 2 babies per 1000 babies born in the U.S. develop PPHN shortly after
birth, and often they need intensive medical care. It is associated with about a 25% risk of significant long-term neurological deficits.
A 2014 meta analysis found no increased risk of persistent pulmonary
hypertension associated with exposure to SSRI's in early pregnancy and a
slight increase in risk associates with exposure late in pregnancy; "an
estimated 286 to 351 women would need to be treated with an SSRI in
late pregnancy to result in an average of one additional case of
persistent pulmonary hypertension of the newborn.". A review published in 2012 reached conclusions very similar to those of the 2014 study.
Neuropsychiatric effects in offspring
According to a 2015 review available data found that "some signal exists suggesting that antenatal exposure to SSRIs may increase the risk of ASDs (autism spectrum disorders)" even though a large cohort study published in 2013
and a cohort study using data from Finland's national register between
the years 1996 and 2010 and published in 2016 found no significant
association between SSRI use and autism in offspring. The 2016 Finland study also found no association with ADHD, but did find an association with increased rates of depression diagnoses in early adolescence.
Overdose
SSRIs appear safer in overdose
when compared with traditional antidepressants, such as the tricyclic
antidepressants. This relative safety is supported both by case series
and studies of deaths per numbers of prescriptions. However, case reports of SSRI poisoning have indicated that severe toxicity can occur and deaths have been reported following massive single ingestions, although this is exceedingly uncommon when compared to the tricyclic antidepressants.
Because of the wide therapeutic index
of the SSRIs, most patients will have mild or no symptoms following
moderate overdoses. The most commonly reported severe effect following
SSRI overdose is serotonin syndrome; serotonin toxicity is usually associated with very high overdoses or multiple drug ingestion. Other reported significant effects include coma, seizures, and cardiac toxicity.
Interactions
The following drugs may precipitate serotonin syndrome in people on SSRIs:
- Linezolid
- Monoamine oxidase inhibitors (MAOIs) including moclobemide, phenelzine, tranylcypromine, selegiline and methylene blue
- Lithium
- Sibutramine
- MDMA (ecstasy)
- Dextromethorphan
- Tramadol
- Pethidine/meperidine
- St. John's wort
- Yohimbe
- Tricyclic antidepressants (TCAs)
- Serotonin-norepinephrine reuptake inhibitors (SNRIs)
- Buspirone
- Triptan
- Mirtazapine
Painkillers of the NSAIDs drug family may interfere and reduce
efficiency of SSRIs and may compound the increased risk of
gastrointestinal bleeds caused by SSRI use. NSAIDs include:
There are a number of potential pharmacokinetic interactions between
the various individual SSRIs and other medications. Most of these arise
from the fact that every SSRI has the ability to inhibit certain P450 cytochromes.
| Drug name | CYP1A2 | CYP2C9 | CYP2C19 | CYP2D6 | CYP3A4 | CYP2B6 |
|---|---|---|---|---|---|---|
| Citalopram | + | 0 | 0 | + | 0 | 0 |
| Escitalopram | 0 | 0 | 0 | + | 0 | 0 |
| Fluoxetine | + | ++ | +/++ | +++ | + | + |
| Fluvoxamine | +++ | ++ | +++ | + | + | + |
| Paroxetine | + | + | + | +++ | + | +++ |
| Sertraline | + | + | +/++ | + | + | + |
Legend:
0 — no inhibition
+ — mild inhibition
++ — moderate inhibition
+++ — strong inhibition
0 — no inhibition
+ — mild inhibition
++ — moderate inhibition
+++ — strong inhibition
The CYP2D6 enzyme is entirely responsible for the metabolism of hydrocodone, codeine and dihydrocodeine to their active metabolites (hydromorphone, morphine, and dihydromorphine, respectively), which in turn undergo phase 2 glucuronidation. These opioids (and to a lesser extent oxycodone, tramadol, and methadone) have interaction potential with selective serotonin reuptake inhibitors. The concomitant use of some SSRIs (paroxetine and fluoxetine) with codeine may decrease the plasma concentration of active metabolite morphine, which may result in reduced analgesic efficacy.
Another important interaction of certain SSRIs involves
paroxetine, a potent inhibitor of CYP2D6, and tamoxifen, an agent used
commonly in the treatment and prevention of breast cancer. Tamoxifen is a
prodrug that is metabolised by the hepatic cytochrome P450 enzyme
system, especially CYP2D6, to its active metabolites. Concomitant use of
paroxetine and tamoxifen in women with breast cancer is associated with
a higher risk of death, as much as a 91 percent in women who used it
the longest.
List of SSRIs
Marketed
Antidepressants
- Citalopram (Celexa)
- Escitalopram (Lexapro)
- Fluoxetine (Prozac)
- Fluvoxamine (Luvox)
- Paroxetine (Paxil)
- Sertraline (Zoloft)
Others
- Dapoxetine (Priligy)
Discontinued
Antidepressants
- Indalpine (Upstène)
- Zimelidine (Zelmid)
Never marketed
Antidepressants
- Alaproclate (GEA-654)
- Centpropazine
- Cericlamine (JO-1017)
- Femoxetine (Malexil; FG-4963)
- Ifoxetine (CGP-15210)
- Omiloxetine
- Panuramine (WY-26002)
- Pirandamine (AY-23713)
- Seproxetine ((S)-norfluoxetine)
Related drugs
Although described as SNRIs, duloxetine (Cymbalta), venlafaxine (Effexor), and desvenlafaxine (Pristiq) are in fact relatively selective as serotonin reuptake inhibitors (SRIs). They are about at least 10-fold selective for inhibition of serotonin reuptake over norepinephrine reuptake. The selectivity ratios are approximately 1:30 for venlafaxine, 1:9 for duloxetine, and 1:14 for desvenlafaxine. At low doses, these SNRIs act mostly as SSRIs; only at higher doses do they also prominently inhibit norepinephrine reuptake. Milnacipran (Ixel, Savella) and its stereoisomer levomilnacipran
(Fetzima) are the only widely marketed SNRIs that inhibit serotonin and
norepinephrine to similar degrees, both with ratios close to 1:1.
Vilazodone (Viibryd) and vortioxetine (Trintellix) are SRIs that also act as modulators of serotonin receptors and are described as serotonin modulators and stimulators (SMS).[134] Vilazodone is a 5-HT1A receptor partial agonist while vortioxetine is a 5-HT1A receptor agonist and 5-HT3 and 5-HT7 receptor antagonist. Litoxetine (SL 81-0385) and lubazodone (YM-992, YM-35995) are similar drugs that were never marketed. They are SRIs and litoxetine is also a 5-HT3 receptor antagonist while lubazodone is also a 5-HT2A receptor antagonist.
Mechanism of action
Serotonin reuptake inhibition
In the brain, messages are passed from a nerve cell to another via a chemical synapse, a small gap between the cells. The presynaptic cell
that sends the information releases neurotransmitters including
serotonin into that gap. The neurotransmitters are then recognized by receptors
on the surface of the recipient postsynaptic cell, which upon this
stimulation, in turn, relays the signal. About 10% of the
neurotransmitters are lost in this process; the other 90% are released
from the receptors and taken up again by monoamine transporters into the sending presynaptic cell, a process called reuptake.
SSRIs inhibit the reuptake of serotonin. As a result, the
serotonin stays in the synaptic gap longer than it normally would, and
may repeatedly stimulate the receptors of the recipient cell. In the
short run, this leads to an increase in signaling across synapses in
which serotonin serves as the primary neurotransmitter. On chronic
dosing, the increased occupancy of post-synaptic serotonin receptors
signals the pre-synaptic neuron to synthesize and release less
serotonin. Serotonin levels within the synapse drop, then rise again,
ultimately leading to downregulation of post-synaptic serotonin receptors.
Other, indirect effects may include increased norepinephrine output,
increased neuronal cyclic AMP levels, and increased levels of regulatory
factors such as BDNF and CREB.
Owing to the lack of a widely accepted comprehensive theory of the
biology of mood disorders, there is no widely accepted theory of how
these changes lead to the mood-elevating and anti-anxiety effects of
SSRIs.
Sigma receptor ligands
| Medication | SERT | σ1 | σ2 | σ1 / SERT | |
|---|---|---|---|---|---|
| Citalopram | 1.16 | 292–404 | Agonist | 5,410 | 252–348 |
| Escitalopram | 2.5 | 288 | Agonist | ND | ND |
| Fluoxetine | 0.81 | 191–240 | Agonist | 16,100 | 296–365 |
| Fluvoxamine | 2.2 | 17–36 | Agonist | 8,439 | 7.7–16.4 |
| Paroxetine | 0.13 | ≥1,893 | ND | 22,870 | ≥14,562 |
| Sertraline | 0.29 | 32–57 | Antagonist | 5,297 | 110–197 |
| Values are Ki (nM). The smaller the value, the more strongly the drug binds to the site. | |||||
In addition to their actions as reuptake inhibitors of serotonin, some SSRIs are also, coincidentally, ligands of the sigma receptors. Fluvoxamine is an agonist of the σ1 receptor, while sertraline is an antagonist of the σ1 receptor, and paroxetine does not significantly interact with the σ1 receptor. None of the SSRIs have significant affinity for the σ2 receptor, and the SNRIs, unlike the SSRIs, do not interact with either of the sigma receptors. Fluvoxamine has by far the strongest activity of the SSRIs at the σ1 receptor. High occupancy of the σ1 receptor by clinical dosages of fluvoxamine has been observed in the human brain in positron emission tomography (PET) research. It is thought that agonism of the σ1 receptor by fluvoxamine may have beneficial effects on cognition. In contrast to fluvoxamine, the relevance of the σ1
receptor in the actions of the other SSRIs is uncertain and
questionable due to their very low affinity for the receptor relative to
the SERT.
Anti-inflammatory effects
The
role of inflammation and the immune system in depression has been
extensively studied. The evidence supporting this link has been shown in
numerous studies over the past ten years. Nationwide studies and
meta-analyses of smaller cohort studies have uncovered a correlation
between pre-existing inflammatory conditions such as type 1 diabetes, rheumatoid arthritis (RA), or hepatitis, and an increased risk of depression. Data also shows that using pro-inflammatory agents in the treatment of diseases like melanoma can lead to depression. Several meta-analytical studies have found increased levels of proinflammatory cytokines and chemokines in depressed patients. This link has led scientists to investigate the effects of antidepressants on the immune system.
SSRIs were originally invented with the goal of increasing levels
of available serotonin in the extracellular spaces. However, the
delayed response between when patients first begin SSRI treatment to
when they see effects has led scientists to believe that other molecules
are involved in the efficacy of these drugs.
To investigate the apparent anti-inflammatory effects of SSRIs, both
Kohler et al. and Więdłocha et al. conducted meta-analyses which have
shown that after antidepressant treatment the levels of cytokines
associated with inflammation are decreased.
A large cohort study conducted by researchers in the Netherlands
investigated the association between depressive disorders, symptoms, and
antidepressants with inflammation. The study showed decreased levels of
interleukin (IL)-6, a cytokine that has proinflammatory effects, in patients taking SSRIs compared to non-medicated patients.
Treatment with SSRIs has shown reduced production of inflammatory cytokines such as IL-1β, tumor necrosis factor (TNF)-α, IL-6, and interferon (IFN)-γ, which leads to a decrease in inflammation levels and subsequently a decrease in the activation level of the immune response. These inflammatory cytokines have been shown to activate microglia which are specialized macrophages that reside in the brain. Macrophages
are a subset of immune cells responsible for host defense in the innate
immune system. Macrophages can release cytokines and other chemicals to
cause an inflammatory response. Peripheral inflammation can induce an
inflammatory response in microglia and can cause neuroinflammation.
SSRIs inhibit proinflammatory cytokine production which leads to less
activation of microglia and peripheral macrophages. SSRIs not only
inhibit the production of these proinflammatory cytokines, they also
have been shown to upregulate anti-inflammatory cytokines such as IL-10.
Taken together, this reduces the overall inflammatory immune response.
In addition to affecting cytokine production, there is evidence
that treatment with SSRIs has effects on the proliferation and viability
of immune system cells involved in both innate and adaptive immunity.
Evidence shows that SSRIs can inhibit proliferation in T-cells, which are important cells for adaptive immunity and can induce inflammation. SSRIs can also induce apoptosis,
programmed cell death, in T-cells. The full mechanism of action for the
anti-inflammatory effects of SSRIs is not fully known. However, there
is evidence for various pathways to have a hand in the mechanism. One
such possible mechanism is the increased levels of cyclic adenosine monophosphate (cAMP) as a result of interference with activation of protein kinase A
(PKA), a cAMP dependent protein. Other possible pathways include
interference with calcium ion channels, or inducing cell death pathways
like MAPK and Notch signaling pathway.
The anti-inflammatory effects of SSRIs have prompted studies of
the efficacy of SSRIs in the treatment of autoimmune diseases such as multiple sclerosis, RA, inflammatory bowel diseases, and septic shock. These studies have been performed in animal models but have shown consistent immune regulatory effects. Fluoxetine, an SSRI, has also shown efficacy in animal models of graft vs. host disease.
SSRIs have also been used successfully as pain relievers in patients
undergoing oncology treatment. The effectiveness of this has been
hypothesized to be at least in part due to the anti-inflammatory effects
of SSRIs.
Pharmacogenetics
Large bodies of research are devoted to using genetic markers
to predict whether patients will respond to SSRIs or have side effects
that will cause their discontinuation, although these tests are not yet
ready for widespread clinical use.
Versus TCAs
SSRIs are described as 'selective'
because they affect only the reuptake pumps responsible for serotonin,
as opposed to earlier antidepressants, which affect other monoamine
neurotransmitters as well, and as a result, SSRIs have fewer side
effects.
There appears to be no significant difference in effectiveness between SSRIs and tricyclic antidepressants, which were the most commonly used class of antidepressants before the development of SSRIs. However, SSRIs have the important advantage that their toxic dose is high, and, therefore, they are much more difficult to use as a means to commit suicide. Further, they have fewer and milder side effects. Tricyclic antidepressants also have a higher risk of serious cardiovascular side effects, which SSRIs lack.
SSRIs act on signal pathways such as cAMP (Cyclic AMP) on the
postsynaptic neuronal cell, which leads to the release of Brain-Derived
Neurotrophic Factor (BDNF). BDNF enhances the growth and survival of
cortical neurons and synapses.
History
Fluoxetine was introduced in 1987 and was the first major SSRI to be marketed.
Society and culture
Controversy
A study examining publication of results from FDA-evaluated
antidepressants concluded that those with favorable results were much
more likely to be published than those with negative results.
Furthermore, an investigation of 185 meta-analyses on antidepressants
found that 79% of them had authors affiliated in some way to
pharmaceutical companies and that they were also reluctant to reporting
caveats for antidepressants.
David Healy
has argued that warning signs were available for many years prior to
regulatory authorities moving to put warnings on antidepressant labels
that they might cause suicidal thoughts. At the time these warnings were added, others argued that the evidence for harm remained unpersuasive and others continued to do so after the warnings were added.