From Wikipedia, the free encyclopedia
Gut flora or, more appropriately, gut microbiota, consists of a complex community of microorganism species that live in the digestive tracts of animals and is the largest reservoir of microorganisms mutual to humans. In this context gut is synonymous with intestinal, and flora with microbiota and microflora. The gut microbiome refer to the genomes of the gut microbiota.
Gut microorganisms benefit the host by gleaning the energy from the fermentation of undigested carbohydrates and the subsequent absorption of short-chain fatty acids. The most important of these fatty acids are butyrates, metabolised by the colonic epithelium; propionates by the liver; and acetates by the muscle tissue. Intestinal bacteria also play a role in synthesizing vitamin B and vitamin K as well as metabolizing bile acids, sterols and xenobiotics.[1]
The human body carries about 100 trillion microorganisms in its intestines, a number ten times greater than the total number of human cells in the body.[2][3][4][5][6] The metabolic activities performed by these bacteria resemble those of an organ, leading some to liken gut bacteria to a "forgotten" organ.[7] It is estimated that these gut flora have around a hundred times as many genes in aggregate as there are in the human genome.[8]
Description
Bacteria make up most of the flora in the colon and up to 60% of the dry mass of feces.[9] Somewhere between 300[3] and 1000 different species live in the gut,[4] with most estimates at about 500.[5][7][10] However, it is probable that 99% of the bacteria come from about 30 or 40 species.[11] Fungi, protozoa, and archaea also make up a part of the gut flora, but little is known about their activities.Research suggests that the relationship between gut flora and humans is not merely commensal (a non-harmful coexistence), but rather a mutualistic relationship.[4] Though people can survive without gut flora,[5] the microorganisms perform a host of useful functions, such as fermenting unused energy substrates, training the immune system, preventing growth of harmful, pathogenic bacteria,[3] regulating the development of the gut, producing vitamins for the host, such as biotin[12] and vitamin K,[13] and producing hormones to direct the host to store fats. In return, these microorganisms procure within the host a protected, nutrient-rich environment in which they can thrive. However, in certain conditions, some species are thought to be capable of causing disease by producing infection or increasing cancer risk for the host.[3]
Over 99% of the bacteria in the gut are anaerobes,[3][4][11][14] but in the cecum, aerobic bacteria reach high densities.[3]
The compositions of microbiota rely on several factors like host diet, colonization history, and immune status.[15] Some microbes are better suited to complement specific metabolic enzymes over others. For example, Bacteroides change how they break down carbohydrates depending on if they received the right amount of certain substrates.[16]
Types
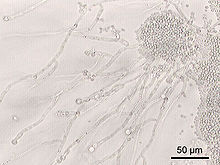
Not all the species in the gut have been identified[3][4] because most cannot be cultured,[4][11][17] and identification is difficult. Populations of species vary widely among different individuals but stay fairly constant within an individual over time, even though some alterations may occur with changes in lifestyle, diet and age.[3][7] An effort to better describe the microflora of the gut and other body locations has been initiated; see Human microbiome project. In 2009, scientists from INRA (France) highlighted the existence of a small number of species shared by all individuals constituting the human intestinal microbiota phylogenetic core.[18]
The four dominant phyla in the human gut are Firmicutes, Bacteroidetes, Actinobacteria, and Proteobacteria.[19] Most bacteria belong to the genera Bacteroides, Clostridium, Faecalibacterium,[3][11][14] Eubacterium, Ruminococcus, Peptococcus, Peptostreptococcus, and Bifidobacterium.[3][11] Other genera, such as Escherichia and Lactobacillus, are present to a lesser extent.[3] Species from the genus Bacteroides alone constitute about 30% of all bacteria in the gut, suggesting that this genus is especially important in the functioning of the host.[4]
The currently known genera of fungi of the gut flora include Candida, Saccharomyces, Aspergillus, and Penicillium.
Archaea constitute another large class of gut flora which are important in the metabolism of the bacterial products of fermentation.
Enterotype
An enterotype is a classification of living organisms based on its bacteriological ecosystem in the human gut microbiome not dictated by age, gender, body weight, or national divisions.[20] There are indications that long-term diet influences enterotype.[21] Three human enterotypes have been discovered.[20][22]Age
It has been demonstrated that there are common patterns of microbiome composition evolution during life.[23] Analysing bacterial V4 16S rRNA from 528 individuals of different ages and geographic origins,[24] demonstrated that the diversity of microbiota composition of the fecal samples is significantly higher in adults than in children, although interpersonal differences are higher in children than in adults. Interestingly, the maturation of microbiota into an adult-like configuration happens during the three first years of life. The metagenomic analysis of fecal samples combined with the analysis of V4 16S rRNA allowed a detailed study of phylotypes and showed that although there are not phylotypes being unique to adults or babies, phylotypes belonging to Bifidobacteria longum which dominate breast fed babies, decline in proportional representation with increasing age.[24]The study also showed a high prevalence of enzymes involved in fermentation, methanogenesis and in the metabolism of arginine, glutamate, aspartate and lysine in adult microbiomes whereas in infant microbiomes the dominant enzymes are involved in cysteine metabolism and fermentation pathways.[24]
Finally, analysing the effects of kinship on the microbiome across countries, it has been found that despite the large influence of cultural factors on which microbes are present in the population, sharing numerous common environmental exposures in a family is a strong determinant of individual microbiome composition. This effect has no genetic influence and it is consistently observed in culturally different populations.[24]
Gut flora and diet
Studies and statistical analyses have identified the different bacterial genera in gut microbiota and their associations with nutrient intake. Gut microflora is mainly composed of three enterotypes: Prevotella, Bacteroides and Ruminococcus. There is an association between the concentration of each microbial community and dietary components. For example, Prevotella is related to carbohydrates and simple sugars, indicating an association with a carbohydrate-based diet more typical of agrarian societies, while Bacteroides is associated with animal proteins, amino acids and saturated fats, components typical of a Western diet. That means that one enterotype will dominate over the other depending on the diet - those who eat plenty of protein and animal fats have predominantly Bacteroides bacteria, while for those who consume more carbohydrates the Prevotella species dominate.[21]Gut microbiome however can be changed by following a long-term diet. People whose microbiome is predominantly Bacteroides (diet based on high levels of protein and fat) and change their dietary patterns to a diet based on high levels of carbohydrates, will develop a Prevotella enterotype in the long-term. This relation may be interesting medically, as long-term dietary interventions may allow modulation of an individual's enterotype to improve health.[21]
Geography
Gut microbiome composition depends on the geographic origin of populations. Variations in trade off of Prevotella, the representation of the urease gene, and the representation of genes encoding glutamate synthase/degradation or other enzymes involved in amino acids degradation or vitamin biosynthesis show significant differences between populations from USA, Malawi or Amerindian origin.[24]The US population has a high representation of enzymes encoding the degradation of glutamine and enzymes involved in vitamin and lipoic acid biosynthesis; whereas Malawi and Amerindian populations have a high representation of enzymes encoding glutamate synthase and they also have an overrepresentation of α-amylase in their microbiomes. As the US population has a diet richer in fats than Amerindian or Malawian populations which have a corn-rich diet, the diet is probably a main determinant of gut bacterial composition.[24]
Further studies have indicated a large difference in the composition of microbiota between European and rural African children. The fecal bacteria of children from Florence were compared to that of children from the small rural village of Boulpon in Burkina Faso. The diet of a typical child living in this village is largely lacking in fats and animal proteins and rich in polysaccharides and plant proteins. The fecal bacteria of European children was dominated by Firmicutes and showed a marked reduction in biodiversity, while the fecal bacteria of the Boulpon children was dominated by Bacteroidetes. The increased biodiversity and different composition of gut flora in African populations may aid in the digestion of normally indigestible plant polysaccharides and also may result in a reduced incidence of non-infectious colonic diseases.[25]
Acquisition of gut flora in human infants
The gastrointestinal tract of a normal fetus has been considered to be sterile, however recently it has been acknowledged that microbial colonisation may occur in the fetus.[26] During birth and rapidly thereafter, bacteria from the mother and the surrounding environment colonize the infant's gut. Immediately after vaginal delivery, babies may have bacterial strains derived from the mothers' feces in the upper gastrointestinal tract.[27] Infants born by caesarean section may also be exposed to their mothers' microflora, but the initial exposure is most likely to be from the surrounding environment such as the air, other infants, and the nursing staff, which serve as vectors for transfer.[28] The initial inoculum of babies born by cesarian section is typically dominated by Staphyloccocus, Corynebacterium and Propionibacterium species.[29] The primary gut flora in infants born by caesarean delivery may be disturbed for up to six months after birth, whereas vaginally born infants take up to one month for their intestinal microflora to be well established.[30] After birth, environmental, oral and cutaneous bacteria are readily transferred from the mother to the infant through suckling, kissing, and caressing.All infants are initially colonized by large numbers of E. coli and streptococci. Within a few days, bacterial numbers reach 108 to 1010 per gram of feces.[28][31] During the first week of life, these bacteria create a reducing environment favorable for the subsequent bacterial succession of strict anaerobic species mainly belonging to the genera Bifidobacterium, Bacteroides, Clostridium, and Ruminococcus.[32] Breast-fed babies become dominated by bifidobacteria, possibly due to the contents of bifidobacterial growth factors in breast milk.[33][34] In contrast, the microbiota of formula-fed infants is more diverse, with high numbers of Enterobacteriaceae, enterococci, bifidobacteria, Bacteroides, and clostridia.[35][36]
The microbiomes of infants are enriched by enzymes involved in foraging of glycans represented in breast milk and the intestinal mucosa.[24]
Functions
Bacteria in the gut fulfill a host of useful functions for humans, including digestion of unutilized energy substrates,[37] stimulating cell growth, repressing the growth of harmful microorganisms, training the immune system to respond only to pathogens, and defending against some diseases.[3][4][38]Carbohydrate fermentation and absorption
Without gut flora, the human body would be unable to utilize some of the undigested carbohydrates it consumes, because some types of gut flora have enzymes that human cells lack for breaking down certain polysaccharides.[4] Rodents raised in a sterile environment and lacking in gut flora need to eat 30% more calories just to remain the same weight as their normal counterparts.[4] Carbohydrates that humans cannot digest without bacterial help include certain starches, fiber, oligosaccharides and sugars that the body failed to digest and absorb[3][10][11] like lactose in the case of lactose intolerance and sugar alcohols, mucus produced by the gut, and proteins.[10] A further result is flatulence, specifically due to the metabolism of oligosaccharides (notably from beans) by many different species.Bacteria turn carbohydrates they ferment into short-chain fatty acids (SCFAs)[10][11] by a form of fermentation called saccharolytic fermentation.[10] Products include acetic acid, propionic acid and butyric acid.[10][11] These materials can be used by host cells, providing a major source of useful energy and nutrients for humans,[10] as well as helping the body to absorb essential dietary minerals such as calcium, magnesium and iron.[3] Gases and organic acids, such as lactic acid, are also produced by saccharolytic fermentation.[11] Acetic acid is used by muscle, propionic acid helps the liver produce ATP, and butyric acid provides energy to gut cells and may prevent cancer.[10] Evidence also indicates that bacteria enhance the absorption and storage of lipids[4] and produce and then facilitate the body to absorb needed vitamins like vitamin K.
Another, less favorable type of fermentation, proteolytic fermentation, breaks down proteins like enzymes, dead host and bacterial cells, and collagen and elastin found in food, and can produce toxins and carcinogens in addition to SCFAs. Thus, a diet lower in protein reduces exposure to toxins.[3]
Beneficial flora increase the gut's absorption of water, reduce counts of damaging bacteria, increase growth of human gut cells,[citation needed] and stimulate growth of indigenous bacteria.[3]
Trophic effects
Another benefit of SCFAs is that they increase growth of intestinal epithelial cells and control their proliferation and differentiation.[3] They may also cause lymphoid tissue near the gut to grow. Bacterial cells also alter intestinal growth by changing the expression of cell surface proteins such as sodium/glucose transporters.[4] In addition, changes they make to cells may prevent injury to the gut mucosa from occurring.[38]Suppression of pathogenic microbial growth

C. difficile colonies on a blood agar plate. The overgrowth of C. difficile in the gut can be harmful to the host.
Another important role of helpful gut flora is that they prevent species that would harm the host from colonizing the gut through competitive exclusion, an activity termed the "barrier effect". Harmful yeasts and bacterial species such as Clostridium difficile (the overgrowth of which can cause pseudomembranous colitis) are unable to grow excessively due to competition from helpful gut flora species adhering to the mucosal lining of the intestine, thus animals without gut flora are infected very easily. The barrier effect protects humans from both invading species and species normally present in the gut at low numbers, whose growth is usually inhibited by the gut flora.[3]
Helpful bacteria prevent the growth of pathogenic species by competing for nutrition and attachment sites to the epithelium of the colon. Symbiotic bacteria are more at home in this ecological niche and are thus more successful in the competition. Indigenous gut floras also produce bacteriocins, which are proteinaceous toxins that inhibit growth of similar bacterial strains, substances that kill harmful microbes and the levels of which can be regulated by enzymes produced by the host.[3]
The process of fermentation, since it produces lactic acid and different fatty acids, also serves to lower the pH in the colon, preventing the proliferation of harmful species of bacteria and facilitating that of helpful species. The pH may also enhance the excretion of carcinogens.[10]
Immunity
Gut flora have a continuous and dynamic effect on the host's gut and systemic immune systems. The bacteria are key in promoting the early development of the gut's mucosal immune system both in terms of its physical components and function and continue to play a role later in life in its operation. The bacteria stimulate the lymphoid tissue associated with the gut mucosa to produce antibodies to pathogens. The immune system recognizes and fights harmful bacteria, but leaves the helpful species alone, a tolerance developed in infancy.[3][5][17]As soon as an infant is born, bacteria begin colonizing its digestive tract. The first bacteria to settle in are able to affect the immune response, making it more favorable to their own survival and less so to competing species; thus the first bacteria to colonize the gut are important in determining the person's lifelong gut flora makeup. However, there is a shift at the time of weaning from predominantly facultative anaerobic species, such as Streptococci and Escherichia coli, to mostly obligate anaerobic species.[3][4]
Recent findings have shown that gut bacteria play a role in the expression of toll-like receptors (TLRs) in the intestines, molecules that help the host repair damage due to injury. TLRs cause parts of the immune system to repair injury caused, for example, by radiation.[4][38] TLRs are one of the two classes of pattern-recognition receptors (PRR) that provide the intestine the ability to discriminate between the pathogenic and commensal bacteria. These PRRs identify the pathogens that have crossed the mucosal barriers and trigger a set of responses that take action against the pathogen, which involve three main immunosensory cells: surface enterocytes, M cells and dendritic cells.[7]
The other class of PRRs are known as the nucleotide-binding oligomerization domain/caspase recruitment domain isoforms (NOD/CARD), which are cytoplasmic proteins that recognize endogenous or microbial molecules or stress responses and forms oligomers that activate inflammatory caspases. This would result in the cleavage and activation of important inflammatory cytokines and/or activate NF-κB signaling pathway to induce the production of inflammatory molecules.[7]
Bacteria can influence the phenomenon known as oral tolerance, in which the immune system is less sensitive to an antigen (including those produced by gut bacteria) once it has been ingested. This tolerance, mediated in part by the gastrointestinal immune system and in part by the liver, can reduce an overreactive immune response like those found in allergies and autoimmune disease.[39] Oral tolerance is dependent on the development of regulatory T cells (Treg), specific white blood cells that develop in response to signals delivered to naïve T cells by other cells of the immune system in response to the gut flora. Different species of gut flora can differentially influence the development of these and other key cells of the immune system to thereby increase or decrease the likelihood of developing oral tolerance.[40] The ability of the gut flora to exert these immunomodulatory effects on the host appears to be restricted to a ‘critical window’ during development when the flora population is first becoming established and the immune system is completing its development.[41] Support for this hypothesis has come from findings of associations between altered patterns of microbial colonization during this critical window and an increased likelihood of developing atopic diseases.[42]
Some species of gut flora, such as some of those in the Bacteroides genus, are able to change their surface receptors to mimic those of host cells in order to evade immune response. Bacteria with neutral and harmful effects on the host can also use these types of strategies. The host immune system has also adapted to this activity, preventing overgrowth of harmful species.[3][5]
Once the host immune system is developed, it regulates the bacterial composition in the gut. One of the regulation mechanisms—immune exclusion—is mediated through the neutralizing action of secretory immunoglobulin A (IgA).[43]
Far beyond immune exclusion, IgAs are also essential to maintain the symbiotic balance between gut microbiota communities and the host immune system. Thus, there is a cross-talk between gut microbiota and the immune system which is basic for the production of the appropriate repertoire of IgA plasma cells. Kawamoto et al.[44] have assessed the influence of the inhibitory co-receptor programmed cell death 1 (PD-1) in this process. They observed that PD-1 deficiency generates an excess of T follicular helper cells (TFH) with altered phenotypes, which results in deregulated selection of IgA precursor cells in the germinal center of Peyer’s patches. Consequently, the IgAs produced in PD-1-deficient mice have reduced bacteria-binding capacity, which causes alterations of microbial communities in the gut. Thus, PD-1 plays a critical role in the regulation of antibody diversification required for the maintenance of intact mucosal barrier.[44]
The right repertoire of gut IgAs depends on two selection processes. There is a first selection process of IgA presenting B lymphocytes in the germinal centers of Peyer’s patches. This selection process involves the activation of B lymphocyte differentiation into plasmablasts which migrate to the lamina propria. T follicular helper cells (TFH) play a pivotal role in the first selection step in Peyer’s patches, and PD1 is a key protein for the communication between B-cells and T-cells. In PD1 deficient mice the TFH cell counts are higher than in normal mice, while the turnover of B-cells increases. Once plasmablasts are within the lamina propria there is a second, commensal driven selection. Here, plasmablasts are reselected to fit the geographical distribution of bacterial dynamic bacterial communities along the intestine. The right clones continue the differentiation process into antibody producing plasma cells. Within the plasma cell, IgA dimer is assembled from the interaction of IgA monomers with the Joining region (JR) and secreted in to the lamina propria. In addition to assembling monomeric IgA, the Joining chain (JR) interacts with the Polymeric immunoglobulin receptor (pIgR), an antibody-transporting protein expressed on the surface of mucosal epithelial cells, which contains secretory IgA fragments. The polymeric immunoglobulin receptor transports IgA across epithelial cells.[citation needed]
Finally, both the secretory IgA complex and the dimeric IgA will develop the immune exclusion. The secretory IgA complex is translocated to the mucosal surface, where it will prevent commensal bacteria from breaching the mucosal surface and IgA polymer leaves the epithelial cells, and is secreted in to the blood, where it will develop inflammatory reactions as necessary.[citation needed]
According to VaccineNewsDaily, there were two studies conducted by the University of Maryland School of Medicine Institute for Genome Sciences and the Center for Vaccine Development on how gut-bacteria impacts the immune system in response to a vaccine. The results of the studies are preliminary and more research is needed. The researchers hope to help relieve people who suffer from various infections caused by Salmonella enterica species and from Shigella diseases.[45]
However, due to a widely accepted theory, new research is going into fecal transplant theory (poop pills), therapeutic worms, and probiotics to replace the missing gut bacteria our bodies originally had.[citation needed] Poop pills have two methods of transmission where they either use a plastic tube that runs through your nose or the anus to deliver the fecal transplant to a host. The fecal transplant is loaded with microorganisms, but strained of any color, smells, and harmful bacteria, to restore the balance. Additionally, therapeutic worms are needed to combat the idea of the Old Friend’s Hypothesis.[citation needed] The hypothesis talks about how modern medicine has reduced parasitic infections, but these worms were what kept our immune system in check. Eliminating worms eliminates our body’s way of down regulating the immune system meaning it becomes hyper-charged. A hyper-charged immune system resonates nothing, but trouble, the start to an autoimmune disease.[citation needed] Lastly, probiotics have become a highly discussed topic and a multi-billion dollar industry within a few years time. Probiotics are generically known as bacteria that can improve your health.[46]
They have a few methods of action when it comes to modifying the microbiota “reduction of luminal pH, competition for nutrients, secretion of anti-microbial compounds, prevention of bacterial adhesion and evasion of epithelial cells, and induction of the production of antimicrobial compounds (defensins) by the host.”[23] Probiotics are now marketed in most stores with a lot of products like yogurt, cheese, and other dairy goods. People above the age of forty generally take probiotics as a supplement to their daily intake of food to help digest, metabolism, and make efficient use of their food. While others, like athletes, take it to maintain a stronger immune system, a healthy gastrointestinal tract, and efficient abundant microbiota[citation needed].
Metabolic function
The resident gut microflora positively control the intestinal epithelial cell differentiation and proliferation through the production of short-chain fatty acids. They also mediate other metabolic effects such as the syntheses of vitamins like biotin and folate, as well as absorption of ions including magnesium, calcium and iron.[7] Methanogenic archae such as Methanobrevibacter smithii are involved in the removal of end products of bacterial fermentation such as hydrogen.The gut flora play a major role in metabolizing dietary carcinogens,[7] the microcomponents and the macrocomponents. The microcomponents are genotoxic, and the major focus is on recent advances in heterocyclic amines (HCAs), which are produced by cooking at high temperatures proteinaceous food, such as meat and fish, which can then induce tumors in organs including the breast, colon and prostate. HCAs are naturally occurring; therefore, the complete avoidance of them is impractical, which is why the metabolic function of gut flora of such components is of great importance to the human, as this would help in prevention of such tumors that are difficult to avoid. The macrocomponents consists of the excessive intake of fat and sodium chloride (that is, plain table salt), which can later promote tumors, such as in breasts and colons, from fat and gastric carcinogenesis from sodium chloride.[47]
One striking effect you can see in[citation needed] is the control of our body fat content. Using mice as models, it has been demonstrated that alterations on microbiota composition due to the administration of subtherapeutic doses of different antibiotics increases the fat content without affecting body weight. First, antibiotics affects the gut microbiota because of their differential effect on different types of bacteria. In particular, the ratio of firmicutes increases, specially remarkable is the increase in members of the family Lachnospiraceae.[citation needed]
Concomitant with the changes in gut microbiota composition, they[specify] found increased concentrations of small chain fatty acids (SCFAs) in the caecum. Intestinal SCFAs directly provide energy to colonocytes and absorption into the portal circulation stimulates adipogenesis. Further investigations lead to the conclusion that the increase in the production of SCFAs alters the hepatic metabolism as the transcription pattern of many genes related with lipid metabolism change in mice administered with antibiotics. Finally, they did not observe any difference between the metabolism of the adipose tissue in antibiotic administered mice and control mice meaning that the increase in adiposity is a downstream phenomenon primarily mediated by changes in the gut and liver.[48][49][50]
Preventing allergy
Bacteria are implicated in preventing allergies,[2] which are overreactions of the immune system to harmless antigens. Studies on the gut flora of infants and young children have shown that those who have or later develop allergies have different compositions of gut flora from those without allergies, with higher chances of having the harmful species C. difficile and S. aureus and lower prevalence of Bacteroides and Bifidobacteria.[2] One explanation is that since helpful gut flora stimulate the immune system and "train" it to respond properly to antigens, a lack of these bacteria in early life leads to an inadequately trained immune system that overreacts to antigens.[2] On the other hand, the differences in flora could be a result, not a cause, of the allergies.[2]Preventing inflammatory bowel disease
Another indicator that bacteria help train the immune system is the epidemiology of Inflammatory Bowel Disease, or IBD, such as Crohn's Disease (CD). Some authors suggest that SCFAs prevent IBD. In addition, some forms of bacteria can prevent inflammation.[51] The incidence and prevalence of IBD is high in industrialized countries with a high standard of living and low in less economically developed countries, having increased in developed countries throughout the twentieth century. The disease is also linked to good hygiene in youth; lack of breastfeeding; and consumption of large amounts of sucrose and animal fat.[51] Its incidence is inversely linked with poor sanitation during the first years of life and consumption of fruits, vegetables, and unprocessed foods.[51] Also, the use of antibiotics, which kill native gut flora and harmful infectious pathogens alike, especially during childhood, is associated with inflammatory bowel disease.[37] On the other hand, using high concentrations of probiotics called "Amanlac" probiotics, helps to effectively maintain intestinal homeostasis, while also treating intestinal inflammation in IBD.[52]Alterations in flora balance
Inflammation
Many tests with colitis-susceptible mice (Il10−/−) show significantly increased levels of luminal Verrucomicrobia, Bacteroidetes and Proteobacteria. For example, inflammation promotes an E. coli proliferation.Effects of antibiotic use
Altering the numbers of gut bacteria, for example by taking broad-spectrum antibiotics, may affect the host's health and ability to digest food.[53] Antibiotics can cause antibiotic-associated diarrhea (AAD) by irritating the bowel directly, changing the levels of gut flora, or allowing pathogenic bacteria to grow.[11] Another harmful effect of antibiotics is the increase in numbers of antibiotic-resistant bacteria found after their use, which, when they invade the host, cause illnesses that are difficult to treat with antibiotics.[53]Changing the numbers and species of gut flora can reduce the body's ability to ferment carbohydrates and metabolize bile acids and may cause diarrhea. Carbohydrates that are not broken down may absorb too much water and cause runny stools, or lack of SCFAs produced by gut flora could cause the diarrhea.[11]
A reduction in levels of native bacterial species also disrupts their ability to inhibit the growth of harmful species such as C. difficile and Salmonella kedougou, and these species can get out of hand, though their overgrowth may be incidental and not be the true cause of diarrhea.[3][11][53] Emerging treatment protocols for C. difficile infections involve fecal microbiota transplantation of donor feces. (see Fecal transplant). Initial reports of treatment describe success rates of 90%, with few side effects. Efficacy is speculated to result from restoring bacterial balances of bacteroides and firmicutes classes of bacteria.[54]
Gut flora composition also changes in severe illnesses, due not only to antibiotic use but also to such factors as ischemia of the gut, failure to eat, and immune compromise. Negative effects from this have led to interest in selective digestive tract decontamination (SDD), a treatment to kill only pathogenic bacteria and allow the re-establishment of healthy ones.[55]
For more than 50 years we have known that the administration of low doses of antibacterial agents promotes the growth of farm animals to increase weight gain.[56]
Antibiotics alter the population of the gastrointestinal (GI) tract microbiota, may change the intra-community metabolic interactions, modify caloric intake by using carbohydrates, and globally affects host metabolic, hormonal and immune homeostasis.[56]
In a study performed on mice by Ilseung Cho,[56] the ratio of Firmicutes and Lachnospiraceae was significantly elevated in animals treated with subtherapeutic doses of different antibiotics. By analyzing the caloric content of faeces and the concentration of small chain fatty acids (SCFAs) in the GI tract, they concluded that the changes in the composition of microbiota lead to an increased capacity to extract calories from otherwise indigestible constituents, and to an increased production of SCFAs. These findings provide evidence that antibiotics perturb not only the composition of the GI microbiome but also its metabolic capabilities, specifically with respect to SCFAs.[56]
Pharmabiotics
Pharmabiotics is a generic term to encompass any form of therapeutic exploitation of the commensal flora, including the use of live probiotic bacteria, probiotic-derived biologically active metabolites, prebiotics, synbiotics or genetically modified commensal bacteria.[7] Since the lack of gut flora can have such harmful health effects, the use of probiotics has anti-inflammatory effects in the gut and may be useful for improving health. Prebiotics are dietary components that can help foster the growth of micro-organisms in the gut, which may lead to better health.[51] There is evidence supporting a therapeutic role for probiotic strategies for treating mucosal inflammatory disorders such as IBD, atopy, infection, diarrhoea, cancer and arthritis.[7]Pregnancy
Women's gut microbiota change as pregnancy advances, with the changes similar to those seen in metabolic syndromes such as diabetes. The change in gut flora causes no ill effects. The newborn's gut biota resemble the mother's first-trimester samples. The diversity of the flora decreases from the first to third trimester, as the numbers of certain species go up.[57]Weight loss
Weight loss initiates a shift in the bacteria phyla that compose gut flora. Specifically, Bacteroidetes increase nearly linearly as weight loss progresses.[58] While there is a high level of variation in bacteria species found among individual people, this trend is prominent and distinct in humans.[59]Role in disease
Bacteria in the digestive tract have pathogenic properties in addition to their health-inducing ones: they can produce toxins and carcinogens[citation needed] and have been implicated in such conditions as multisystem organ failure, sepsis, colon cancer, and inflammatory bowel disease (IBD).[3] A major factor in health is the balance of bacterial numbers; if the numbers grow too high or low, it will result in harm to the host. The host has enzymes to regulate this balance.[citation needed]Cancer
Some genera of bacteria, such as Bacteroides and Clostridium, have been associated with an increase in tumor growth rate, while other genera, such as Lactobacillus and Bifidobacteria, are known to prevent tumor formation.[3]Translocation
Helpful bacteria can be very harmful to the host if they get outside of the intestinal tract.[4][14] Translocation, which occurs when bacteria leave the gut through its mucosal lining, the border between the lumen of the gut and the inside of the body,[5][60] can occur in a number of different diseases.[14][51] It can be caused by too much growth of bacteria in the small intestine, reduced immunity of the host, or increased gut lining permeability.[51] The gut can become more permeable in diseases like cirrhosis, which is damaging due in part to the activity of gut flora.[61]If the gut is perforated, bacteria can invade the body, causing a potentially fatal infection. Aerobic bacteria can make an infection worse by using up all available oxygen and creating an environment favorable to anaerobes.[14]
Likewise, just recently it was discovered that stomach ulcers could be caused by Helicobacter pylori sneaking underneath the epithelial lining of the stomach. Here the body produces an immune response. During this response parietal cells are stimulated and release extra hydrochloric acid (HCl+) into the stomach. However, the response does not stimulate the mucus-secreting cells that protect and line the epithelium of the stomach. The extra acid translates to searing holes into the epithelial lining of the stomach, resulting in stomach ulcers. Moreover, negatively affected microbiota compositions have a detrimental affect on individuals. Research experiments show that one of the probable causes for Inflammatory Bowel Disorder (chronic inflammatory disorders – Crohn’s disease), Likewise, an off balance in microbiota levels can cause widespread diseases like Irritable Bowel Syndrome (functional bowel disorder) and obesity.[23]
Inflammatory bowel disease
Some suspect that IBD is due to a reduction in immune tolerance and subsequent overreaction of the host's immune system to harmful or non-harmful bacteria. IBD may be caused by the entire gut flora together or some specific types.[37][62]It has been noted that though Ulcerative Colitis and Crohn's disease (two types of IBD) probably have genetic components, they are not inherited in a Mendelian fashion and are thus probably due to a complex set of factors rather than solely to a gene.[62] Though neither bacterial colonization nor genetics is sufficient to cause the disease, bacteria probably play a role in these disorders.[62]
Some suspect that inflammation in IBD is due to increased permeability of the inner lining of the colon, which may allow bacteria to invade the tissues and cause an immune reaction that leads to prolonged inflammation.[5][60] Tissue damage in IBD results from the immunological misperception of danger within the naturally occurring flora or due to failure of normal tolerance to pathogenic bacteria. It is still unclear whether the inflammation that occurs is due to a specific subset of intestinal microbes or due to a problem with the tolerance of commensal gut flora.[7] Abnormal tight junctions, which are supposed to prevent permeability, have been found in cells of patients with IBD.[60] Because of the potentially harmful role of these bacteria, antibiotics are frequently prescribed to treat Crohn's disease.[38] However, inflammation could occur first and cause the increased intestinal permeability found in diseases such as Crohn's, so the causative role of bacteria is not clear.[60] Conventional therapies for IBD primarily target the mucosal inflammatory responses by using pharmabiotics.[7]
Colitis
It has been suggested that commensal bacteria are responsible for the development of colitis, since mice raised in a sterile environment do not get the disease.[63] However, while some bacterial strains such as C. difficile[51] and even normal gut bacteria cause colitis,[63] others prevent the disease in mice.[51]Obesity
Obese mice lacking leptin, a lipid metabolism regulator (ob/ob mice), have a distinct gut flora compared to (normal) lean mice, reflected in a change in the ratio between bacteria from the divisions Bacteroidetes and Firmicutes, which is shifted towards fewer Bacteroidetes and more Firmicutes in obese mice.The microbes occupying the human gut are also in direct relation to obesity. A shift in the ratio between bacterial divisions Firmicutes and Bacteroidetes can be observed in lean and obese individuals—in the latter, a shift towards Firmicutes can be observed. The ratio between Firmicutes and Bacteroidetes dynamically reflects the overall weight condition of an individual, shifting towards Bacteroidetes if an obese individual loses weight.
The mutual influence of gut flora composition and weight condition is connected to differences in the energy-reabsorbing potential of different ratios of Firmicutes and Bacteroidetes, especially in the digestion of fatty acids and dietary polysaccharides, as shown by experiments[64] wherein the (caecum) gut flora of obese mice were transplanted into germ-free recipient mice, leading to an increase in weight despite a decrease in food consumption. The experimentation and results suggest bacteria specific to lean and obese genes can be a weapon in the fight against the obesity epidemic.[58][65][66][67][68]