The sociology of health and illness, alternatively the sociology of health and wellness (or simply health sociology), examines the interaction between society and health. The objective of this topic is to see how social life affects morbidity and mortality rate, and vice versa. This aspect of sociology differs from medical sociology in that this branch of sociology discusses health and illness in relation to social institutions such as family, employment, and school. The sociology of medicine limits its concern to the patient-practitioner relationship and the role of health professionals in society. The sociology of health and illness covers sociological pathology (causes of disease and illness), reasons for seeking particular types of medical aid, and patient compliance or noncompliance with medical regimes.
Health, or lack of health, was once merely attributed to
biological or natural conditions. Sociologists have demonstrated that
the spread of diseases is heavily influenced by the socioeconomic status
of individuals, ethnic traditions or beliefs, and other cultural
factors.
Where medical research might gather statistics on a disease, a
sociological perspective on an illness would provide insight on what
external factors caused the demographics who contracted the disease to
become ill.
This topic requires a global approach of analysis because the influence of societal factors varies throughout the world. This will be demonstrated through discussion of the major diseases of each continent. These diseases are sociologically examined and compared based on the traditional medicine, economics, religion, and culture that is specific to each region. HIV/AIDS serves as a common basis of comparison among regions. While it is extremely problematic in certain areas, in others it has affected a relatively small percentage of the population. Sociological factors can help to explain why these discrepancies exist.
There are obvious differences in patterns of health and illness across societies, over time, and within particular society types. There has historically been a long-term decline in mortality within industrialized societies, and on average, life-expectancies are considerably higher in developed, rather than developing or undeveloped, societies. Patterns of global change in health care systems make it more imperative than ever to research and comprehend the sociology of health and illness. Continuous changes in economy, therapy, technology and insurance can affect the way individual communities view and respond to the medical care available. These rapid fluctuations cause the issue of health and illness within social life to be very dynamic in definition. Advancing information is vital because as patterns evolve, the study of the sociology of health and illness constantly needs to be updated.
This topic requires a global approach of analysis because the influence of societal factors varies throughout the world. This will be demonstrated through discussion of the major diseases of each continent. These diseases are sociologically examined and compared based on the traditional medicine, economics, religion, and culture that is specific to each region. HIV/AIDS serves as a common basis of comparison among regions. While it is extremely problematic in certain areas, in others it has affected a relatively small percentage of the population. Sociological factors can help to explain why these discrepancies exist.
There are obvious differences in patterns of health and illness across societies, over time, and within particular society types. There has historically been a long-term decline in mortality within industrialized societies, and on average, life-expectancies are considerably higher in developed, rather than developing or undeveloped, societies. Patterns of global change in health care systems make it more imperative than ever to research and comprehend the sociology of health and illness. Continuous changes in economy, therapy, technology and insurance can affect the way individual communities view and respond to the medical care available. These rapid fluctuations cause the issue of health and illness within social life to be very dynamic in definition. Advancing information is vital because as patterns evolve, the study of the sociology of health and illness constantly needs to be updated.
Historical background
Wall painting found in the tomb of an Egyptian official known as the physicians tomb
Humans have long sought advice from those with knowledge or skill in healing. Paleopathology and other historical records, allow an examination of how ancient societies dealt with illness and outbreak. Rulers in Ancient Egypt sponsored physicians that were specialists in specific diseases. Imhotep
was the first medical doctor known by name. An Egyptian who lived
around 2650 B.C., he was an adviser to King Zoser at a time when
Egyptians were making progress in medicine. Among his contributions to
medicine was a textbook on the treatment of wounds, broken bones, and
even tumors.
Stopping the spread of infectious disease was of utmost importance for maintaining a healthy society. The outbreak of disease during the Peloponnesian War was recorded by Thucydides who survived the epidemic.
From his account it is shown how factors outside the disease itself can
affect society. The Athenians were under siege and concentrated within
the city. Major city centers were the hardest hit. This made the outbreak even more deadly and with probable food shortages the fate of Athens was inevitable. Approximately 25% of the population died of the disease. Thucydides stated that the epidemic "carried away all alike". The disease attacked people of different ages, sexes and nationalities.
Physician in Ancient Greece treating a patient 480–470 BC
Ancient medical systems stressed the importance of reducing illness through divination and ritual. Other codes of behavior and dietary protocols were widespread in the ancient world. During the Zhou Dynasty in China, doctors suggested exercise, meditation and temperance to preserve one's health. The Chinese closely link health with spiritual well-being. Health regimes in ancient India focused on oral health as the best method for a healthy life. The Talmudic code created rules for health which stressed ritual cleanliness, connected disease with certain animals and created diets. Other examples include the Mosaic Code and Roman baths and aqueducts.
Those that were most concerned with health, sanitation and illness in the ancient world were those in the elite class.
Good health was thought to reduce the risk of spiritual defilement and
therefore enhanced the social status of the ruling class who saw
themselves as the beacon of civilization. During the late Roman Period, sanitation for the lower classes was a concern for the leisured class. Those that had the means would donate to charities that focused on the health of non-elites. After the decline of the Roman Empire, physicians and concern with public health disappeared except in the largest cities. Health and public doctors remained in the Byzantine Empire. Focusing on preventing the spread of diseases such as small pox lead to a smaller mortality rate in much of the western world.
Other factors that allowed the modern rise in population include:
better nutrition and environmental reforms (such as getting clean water
supplies).
The present day sense of health being a public concern for the state began in the Middle Ages. A few state interventions include maintaining clean towns, enforcing quarantines during epidemics and supervising sewer systems.
Private corporations also played a role in public health. The funding
for research and the institutions for them to work were funded by
governments and private firms. Epidemics were the cause of most government interventions. The early goal of public health was reactionary whereas the modern goal is to prevent disease before it becomes a problem.
Despite the overall improvement of world health, there still has not
been any decrease in the health gap between the affluent and the
impoverished.
Today, society is more likely to blame health issues on the individual
rather than society as a whole. This was the prevailing view in the late
20th century. In the 1980s the Black Report, published in the United Kingdom, went against this view and argued that the true root of the problem was material deprivation. This report proposed a comprehensive anti-poverty strategy to address these issues. Since this did not parallel the views of the Conservative government, it did not go into action immediately.
The Conservative government was criticized by the Labour Party for not
implementing the suggestions that the Black Report listed.
This criticism gave the Black Report the exposure it needed and its
arguments were considered a valid explanation for health inequality. There is also a debate over whether poverty causes ill-health or if ill-health causes poverty. Arguments by the National Health Service gave considerable emphasis to poverty and lack of access to health care. It has also been found that heredity
has more of a bearing on health than social environment, but research
has also proved that there is indeed a positive correlation between
socioeconomic inequalities and illness.
Methodology
The
Sociology of Health and Illness looks at three areas: the
conceptualization, the study of measurement and social distribution, and
the justification of patterns in health and illness. By looking at
these things researchers can look at different diseases through a
sociological lens. The prevalence and response to different diseases
varies by culture.
By looking at bad health, researchers can see if health affects
different social regulations or controls. When measuring the
distribution of health and illness, it is useful to look at official statistics
and community surveys. Official statistics make it possible to look at
people who have been treated. It shows that they are both willing and
able to use health services. It also sheds light on the infected
person's view of their illness.
On the other hand, community surveys look at people's rating of their
health. Then looking at the relation of clinically defined illness and
self reports and find that there is often a discrepancy.
A great deal of the time, mortality statistics take the place of
the morbidity statistics because in many developed societies where
people typically die from degenerative conditions, the age in which they
die sheds more light on their life-time health. This produces many limitations
when looking at the pattern of sickness, but sociologists try to look
at various data to analyze the distribution better. Normally, developing
societies have lower life expectancies in comparison to developed
countries. They have also found correlations between mortality and sex
and age. Very young and old people are more susceptible to sickness and death. On average women typically live longer than men, although women are more likely to have bad health.
|
>80
77.5–80
75–77.5
72.5–75
70–72.5
|
67.5–70
65–67.5
60–65
55–60
50–55
|
Disparities in health were also found between people in different
social classes and ethnicities within the same society, even though in
the medical profession they put more importance in “health related
behaviors” such as alcohol consumption, smoking, diet, and exercise.
There is a great deal of data supporting the conclusion that these
behaviors affect health more significantly than other factors. Sociologists think that it is more helpful to look at health and illness through a broad lens. Sociologists agree that alcohol
consumption, smoking, diet, and exercise are important issues, but they
also see the importance of analyzing the cultural factors that affect
these patterns. Sociologists also look at the effects that the
productive process has on health and illness. While also looking at
things such as industrial pollution, environmental pollution, accidents at work, and stress-related diseases.
Social factors play a significant role in developing health and illness. Studies of epidemiology
show that autonomy and control in the workplace are vital factors in
the etiology of heart disease. One cause is an effort-reward imbalance.
Decreasing career advancement opportunities and major imbalances in
control over work have been coupled with various negative health costs.
Various studies have shown that pension rights may shed light on
mortality differences between retired men and women of different
socioeconomic statuses. These studies show that there are outside
factors that influence health and illness.
International perspective
Africa
Estimation
of the number of adults in Africa who are infected with HIV or AIDS.
Note that levels of infection are much higher in sub-Saharan Africa.
HIV/AIDS is the leading epidemic that affects the social welfare of Africa.
Human Immunodeficiency virus (HIV) can cause AIDS which is an acronym
for Acquired Immunodeficiency Syndrome (AIDS), a condition in humans in
which the immune system
begins to fail, leading to life-threatening infections. Two-thirds of
the worlds HIV population is located in Sub-Saharan Africa. Since the
epidemic started more than 15 million Africans have died by
complications with HIV/AIDS.
People apart of religious sub-groups of Sub-Saharan Africa
and those who actively and frequently participate in religious
activities are more likely to be at a lower risk of contracting
HIV/AIDS. On the opposite end, there are many beliefs that an infected
male can be cured of the infection by having sex with a virgin. These beliefs increase the number of people with the virus and also increase the number of rapes against women.
Herbal treatment is one of the primary medicines used to treat
HIV in Africa. It is used more than standard treatment because it is
more affordable.
Herbal treatment is more affordable but is not researched and is poorly
regulated . This lack of research on whether the herbal medicines work
and what the medicines consist of is a major flaw in the healing cycle
of HIV in Africa.
Economically, HIV has a significant negative effect. The labor
force in Africa is slowly diminishing, due to HIV-related deaths and
illness. In response, government income declines and so does tax
revenue. The government has to spend more money than it is making, in
order to care for those affected with HIV/AIDS.
AIDS orphans in Malawi
A major social problem in Africa in regards to HIV is the orphan
epidemic. The orphan epidemic in Africa is a regional problem. In most
cases, both of the parents are affected with HIV. Due to this, the
children are usually raised by their grandmothers and in extreme cases
they are raised by themselves. In order to care for the sick parents,
the children have to take on more responsibility by working to produce
an income. Not only do the children lose their parents but they also
lose their childhood as well. Having to provide care for their parents,
the children also miss out on an education which increases the risk of
teen pregnancy and people affected with HIV. The most efficient way to
diminish the orphan epidemic is prevention: preventing children from
acquiring HIV from their mothers at birth, as well as educating them on
the disease as they grow older. Also, educating adults about HIV and
caring for the infected people adequately will lower the orphan
population.
The HIV/AIDS epidemic is reducing the average life expectancy
of people in Africa by twenty years. The age range with the highest
death rates, due to HIV, are those between the ages of 20 and 49 years.
The fact that this age range is when adults acquire most of their income
they cannot afford to send their children to school, due to the high
medication costs. It also removes the people who could help aid in
responding to the epidemic.
Asia
Asian
countries have wide variations of population, wealth, technology and
health care, causing attitudes towards health and illness to differ. Japan, for example, has the third highest life expectancy (82 years old), while Afghanistan has the 11th worst (44 years old).
Key issues in Asian health include childbirth and maternal health, HIV
and AIDS, mental health, and aging and the elderly. These problems are
influenced by the sociological factors of religion or belief systems,
attempts to reconcile traditional medicinal practices with modern
professionalism, and the economic status of the inhabitants of Asia.
People living with HIV/AIDS
Like the rest of the world, Asia is threatened by a possible pandemic of HIV and AIDS. Vietnam
is a good example of how society is shaping Asian HIV/AIDS awareness
and attitudes towards this disease. Vietnam is a country with feudal,
traditional roots, which, due to invasion, wars, technology and travel
is becoming increasingly globalized. Globalization
has altered traditional viewpoints and values. It is also responsible
for the spread of HIV and AIDS in Vietnam. Even early globalization has
added to this problem – Chinese influence made Vietnam a Confucian society,
in which women are of less importance than men. Men in their
superiority have no need to be sexually responsible, and women,
generally not well educated, are often unaware of the risk, perpetuating
the spread of HIV and AIDS as well as other STIs.
Confucianism has had a strong influence on the belief system in
Asia for centuries, particularly in China, Japan, and Korea, and its
influence can be seen in the way people chose to seek, or not seek,
medical care.
An important issue in Asia is societal effect on the ability of
disabled individuals to adjust to a disability. Cultural beliefs shape
attitudes towards physical and mental disabilities. China exemplifies
this problem. According to Chinese Confucian tradition (which is also
applicable in other countries where Confucianism
has been spread), people should always pursue good health in their
lives, with an emphasis on health promotion and disease prevention.
To the Chinese, having a disability signifies that one has not led a
proper lifestyle and therefore there is a lack of opportunities for
disabled individuals to explore better ways to accept or adapt to their
disability.
Indigenous healing practices are extremely diverse throughout
Asia but often follow certain patterns and are still prevalent today.
Many traditional healing practices include shamanism and herbal medicines, and may have been passed down orally in small groups or even institutionalized and professionalized.
In many developing countries the only health care available until a few
decades ago were those based on traditional medicine and spiritual
healing. Now governments must be careful to create health policies that
strike a balance between modernity and tradition. Organizations, like
the World Health Organization,
try to create policies that respect tradition without trying to replace
it with modern science, instead regulating it to ensure safety but
keeping it accessible.
India in particular tries to make traditional medicines safe but still
available to as many people as possible, adapting tradition to match
modernization while still considering the economic positions and culture
of its citizens.
Flag of World Health Organization
Mental health issues are gaining an increasing amount of attention in the Asian countries.
Many of these countries have a preoccupation with modernizing and
developing their economies, resulting in cultural changes. In order to
reconcile modern techniques with traditional practices, social psychologists in India are in the process of “indigenizing
psychology”. Indigenous psychology is that which is derived from the
laws, theories, principals, and ideas of a culture and unique to each
society.
In many Asian countries, childbirth is still treated by
traditional means and is thought of with regional attitudes. For
example, in Pakistan, decisions concerning pregnancy and antenatal care
(ANC) are usually made by older women, often the pregnant woman's
mother-in-law, while the mother and father to be are distanced from the
process. They may or may not receive professional ANC depending on their
education, class, and financial situation.
Generally in Asia, childbirth is still a woman's area and male
obstetricians are rare. Female midwives and healers are still the norm
in most places. Western methods are overtaking the traditional in an
attempt to improve maternal health and increase the number of live
births.
Asian countries, which are mostly developing nations, are aging rapidly even as they are attempting to build their economies. Even wealthy Asian nations, such as Japan, Singapore, and Taiwan,
also have very elderly populations and thus have to try to sustain
their economies and society with small younger generations while caring
for their elderly citizens.
The elderly have been traditionally well respected and well cared for
in most Asian cultures; experts predict that younger generations in the
future are less likely to be concerned and involved in the health care
of their older relatives due to various factors such as women joining
the workforce more, the separation of families because of urbanization
or migration, and the proliferation of Western ideals such as individualism.
Australia
The health patterns found on the continent of Australia which includes the Pacific Islands, have been very much influenced by European colonization.
While indigenous medicinal beliefs are not significantly prevalent in
Australia, traditional ideas are still influential in the health care
problems in many of the islands of the Pacific. The rapid urbanization of Australia led to epidemics of typhoid fever and the Bubonic plague.
Because of this, public health was professionalized beginning in the
late 1870s in an effort to control these and other diseases. Since then
Australia's health system has evolved similarly to Western countries and
the main cultural influence affecting health care are the political
ideologies of the parties in control of the government.
Old heroin bottle
Australia has had treatment facilities for 'problem drinkers' since
the 1870s. In the 1960s and 1970s it was recognized that Australia had
several hundred thousand alcoholics and prevention became a priority
over cures, as there was a societal consensus that treatments are
generally ineffective. The government began passing laws attempting to curb alcohol consumption but consistently met opposition from the wine-making regions of southern Australia. The government has also waged a war on illegal drugs, particularly heroin, which in the 1950s became widely used as a pain reliever.
Experts believe that many of the health problems in the Pacific
Islands can be traced back to European colonization and the subsequent
globalization and modernization of island communities.
European colonization and late independence meant modernization but
also slow economic growth, which had an enormous effect on health care,
particularly on nutrition
in the Pacific Islands. The end of colonization meant a loss of medical
resources, and the fledgling independent governments could not afford
to continue the health policies put in place by the colonial
governments.
Nutrition was changed radically, contributing to various other health
problems. While more prosperous, urban areas could afford food, they
chose poor diets, causing 'overnourishment', and leading to extremely
high levels of obesity, type 2 diabetes, and cardiovascular diseases. Poorer rural communities, on the other hand, continue to suffer from malnutrition and malaria.
Traditional diets in the Pacific are very low in fat, but since World War II there has been a significant increase in fat and protein in Pacific diets. Native attitudes towards weight contribute to the obesity problem. Tongan
natives see obesity as a positive thing, especially in men. They also
believe that women should do as little physical work as possible while
the men provide for them, meaning they get very little exercise.
Europe
The largest endeavors to improve health across Europe is the World Health Organization European Region.
The goal is to improve the health of poor and disadvantaged populations
by promoting healthy lifestyles including environmental, economic,
social and providing health care. Overall health in Europe is very high compared to the rest of the world. The average life expectancy is around 78 in EU countries but there is a wide gap between Western and Eastern Europe. It is as low as 67 in Russia and 73 in the Balkan states. Europe is seeing an increase in the spread of HIV/AIDS in Eastern Europe because of a worsening socioeconomic situation. Cardiovascular disease, cancer and diabetes mellitus are more prevalent is Eastern Europe. The WHO claims that poverty is the most important factor bringing on ill health across Europe. Those at low socioeconomic status levels and many young people are also at risk because of their increased tobacco, alcohol and drug abuse.
Health and illness prevention in Europe is largely funded by the
governmental services including: regulating health care, insurance and
social programs. The role of religion and traditional medicine, however, is often left unexamined in such reports.
The study of hypertension within the United Kingdom
has turned to examining the role that beliefs play in its diagnosis and
treatment. Hypertension is an essential topic for study since it is
linked to increased risk of stroke and coronary heart disease. The most common treatment for hypertension is medication but compliance for this treatment plan is low.
A study conducted in the UK examined the differences between 'white'
patients and first generation immigrants from the West Indies. There
were differing reasons for non-compliance that involve the patients'
perception and beliefs about the diagnosis. Patients commonly believe that high levels of anxiety
when first diagnosed are the major cause and think that when stress
levels decline so too will their hypertension. Other respondents in this
UK based study had varying beliefs concerning the necessity of
medication while others still argued that it was the side effects of medication that made them end their prescribed regimen. West Indian respondents whose lay culture
teaches them to reject long-term drug therapy opted instead for folk
remedies in higher numbers than the 'white' respondents. What can be
seen here is that some people will choose to ignore a doctor's expert
advice and will employ 'lay consultation' instead.
Regions of the WHO
Before people seek medical help they try to interpret the symptoms
themselves and often consult people in their lives or use 'self-help'
measures. A study of 'everyday illness' in Finland including: influenza, infections and musculo-skeletal
problems focused on reasons for consulting medical experts and
explanations of illness. These common illness were examined not because
of their seriousness but because of their frequency. The researchers
explain five possible triggers that people seek medical aid: 1- the
occurrence of an interpersonal crisis 2- perceived interference with
social and personal relations 3- perceived interference with vocational
& physical activity
4- sanctioning by other people 5- sufferers ideas about how long
certain complaints should last. These kind of explanatory models are
part of the process that people use to construct medical culture.
They give meaning to illness and health, answer questions about
personal responsibility about health and most importantly are part of
the dialogue between patients' and professionals' illness explanations.
It can help explore why some patients will follow a doctors instructions
to the letter and others ignore them completely. A patient's
explanation or understanding of their illness can be much broader than a
physician's and this dynamic has become a major criticism of modern
medical practice since it normally excludes the "social, psychological
and experiential dimensions of illness."
The Finnish study examined 127 patients and the results have been
different from findings in other countries where there is more 'lay
consultation'. Half of the respondents did not have any lay consultation
before coming to the doctors office. One-third did not try any
self-treatment and three-quarters of the sample consulted the doctor
within three days of symptoms developing. Possible explanations are that in Finland there is an aspect "over-protectiveness" within their health care system. Many
might conclude that the Finnish people are dependent and helpless but
the researchers of this study found that people chose to consult
professionals because they trusted them over some lay explanation. These
results echo similar studies in Ireland that explain this phenomenon as
being based in a strong work ethic. Illness in these countries will
affect their work and Finnish people will quickly get treatment so they
can return to work. This research out of Finland also describes that
this relationship between patient and doctor is based on:
- National and municipal administrative bureaucracies that demand more output and more satisfied patients;
- The public demanding better care;
- Nurses criticizing physicians for not taking a holistic view of patients;
- Hospital specialists wanting better/earlier screening for serious illnesses (e.g. cancer).
The conflict between medical and lay worlds is prominent. On one hand
many patients believe they are the expert of their own body and view
the Doctor-patient relationship as authoritarian.
These people will often use knowledge outside the medical field to deal
with health and illness. Others see the doctor as the expert and are
shy about describing their symptoms and therefore rely on the doctor for
diagnosis and treatment.
North America
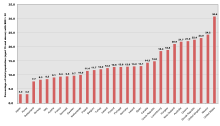
Compares figures in the population of OECD countries and the percentage of total population (aged 15 and above) with a body mass index greater than 30. Data was collected between 1996 and 2003.
North America is a fairly recent settled continent, made up of the
United States, Canada, Mexico, Central America, and the Caribbean. It
was built by an amalgamation of wealth, ideas, culture, and practices.
North America is highly advanced intellectually, technologically, and
traditionally. This advantageous character of North American nations has
caused a high average life expectancy
of 75 years for males and 80 years for females. This leads to the
conclusion that North America has cultivated a comparatively healthy
society. As North America contains several core nations, the growing
economies in those nations are able to maintain and develop medical
institutions. This subsequently provides more access to health care for
American citizens but health care is not universal. North America is
known for being a leading nation in regards to industrialization
and modernization, but the United States lacks federal laws regarding
health care as a basic human right. This lag of health care security
causes subsequent issues with pharmaceutical competition, lack of care
for the elderly, and little attention to alternative medicine. Health care and education are plentiful at a price and illness still persists for many reasons.
A main reason is that a lower- and middle-class population still exists
in plentiful numbers, maintaining a group that is highly vulnerable to
physical ailment.
World map showing alcohol consumption around the world
North America's primary risk factors for illness are currently alcohol abuse, malnutrition, obesity, tobacco use, and water sanitation. Obesity is a recent epidemic in North America. The 1990s brought a rise in the average Body Mass Index, or BMI. From the beginning and to the end of the decade, the median percent of adults who were obese rose from 12% to 20%. Alcoholism
is the addiction of over-consumption of alcohol and is highly prevalent
in the US. There are high incidence rates in many other world regions.
Roughly 61% of American adults drank in 2007, and 21% of current
drinkers consumed five or more drinks at one point in the last year.
There have also been 22,073 alcohol induced deaths in the United States
in the past year, about 13,000 of which were related to liver disease.
Alcoholism has many risk factors ingrained in North American culture,
such as heredity, stress from competition or availability.
The Swine Flu
(also known as (H1N1) epidemic is a recent disease emerging in the
early 21st century. In April 2009, during the early days of the
outbreak, a molecular biologist named Dr. Henry Miller wrote in the Wall Street Journal about New York City high-school students. These students apparently brought the virus back from Mexico and infected their classmates. All six cases so far reported in Canada
were connected directly or indirectly with travel to Mexico as well.
Flu viruses can be directly transmitted (via droplets from sneezing or
coughing) from pigs to people, and vice versa. These cross-species
infections occur most commonly when people are close to large numbers of
pigs, such as in barns, livestock exhibits at fairs, and
slaughterhouses. The flu is transmissible from human to human, either
directly or via contaminated surfaces."
South America
There are many diseases that affect South America, but two major conditions are malaria and Hepatitis D.
Malaria affects every country in South America except Uruguay, Chile, and The Falkland Islands. Elevation is a major factor in the areas where malaria is found. The disease is spread from person to person via mosquito bites. People are typically bitten by mosquitoes at dusk and dawn. Symptoms of this disorder are: high fever, chills, sweating, headaches, body aches, weakness, vomiting and diarrhea. If left untreated, new symptoms can occur; people that are infected may experience seizures, delirium and coma. Severe cases may end in death.
Malaria can be cured, but the symptoms may not become noticeable until
months later. There are three forms of medication that can cure Malaria.
An infected person's accessibility to these drugs is dependent upon
their access to medical care and their financial situation. Literature
about Malaria treatment typically is focused toward people who are
tourists. Most sources are not written with the native in mind.
Malaria
The first sign of Hepatitis D was detected in 1978 when a strange and unrecognizable internuclear antigen was discovered during a liver biopsy
of several Italians who suffered HBV infection. Scientists initially
thought that it was an antigenic specificity of HBV, but they soon found
that it was a protein
from another disease altogether. They called it "Hepatitis Delta Virus"
(HDV). This new virus was found to be defective. HDV needed HBV to act
as a helper function in order for it to be detected. Normally Hepatitis B
is transmitted through blood or any type of blood product. In South America Hepatitis D was found to be fatal. Scientists
are still unsure in what way this disease was being transmitted
throughout certain South American countries. Sexual contact and drug use
are the most common means of transmission. HDV is still considered an
unusual form of hepatitis. Agents of this virus resemble that of plant
viroids. It is still hard to tell how many stereotypes exist because HDV
is under the umbrella of HBV. HDV causes very high titers in the blood
of people who are infected. Incubation of Hepatitis D typically lasts
for thirty five days. Most often Hepatitis D is a co-infection with
Hepatitis B or a super-infection with chronic hepatitis. In terms of
super infections there are high mortality rates, ranging seventy to
eighty percent; in contrast with co-infections which have a one to three
percent mortality rate. There is little information with the ecology of
Hepatitis D. Epidemics have been found in Venezuela, Peru, Columbia,
and Brazil. People who are treated for Hepatitis B have been able to
control Hepatitis D. People who have chronic HDB will continue to get
HDV.
Another disease that affects South America is HIV and AIDS. In
2008 roughly two million people had HIV and AIDS. By the end of 2008 one
hundred and seventy thousand people were infected with AIDS and HIV.
Seventy seven thousand people died from this disease by the end of that
year. Brazil has the most people that are affected with AIDS and HIV in
South America. Forty-three percent of people in Brazil have HIV.
In Brazil sixty percent of the inhabitants use drugs, are HIV positive,
and are HIV positive because of their drug use. Usually this disease is
transmitted by either drug use involving needles or unprotected sex.
Sharing needles and being infected with HIV and AIDS is most common in
Paraguay and Uruguay. South America is trying to get treatment to the
thousands of people infected by this disease. Brazil is offering generic
AIDS prescriptions that are much less expensive than the name brand
drugs. One hundred and eighty-one thousand inhabitants in Brazil who
were infected are being treated. That accounts for eighty percent of
those who needed immediate help. This aid from the government has had
positive results. Statistics show that there was a fifty percent
decrease in mortality rates, approximately sixty to eighty percent
decrease in morbidity rates and a seventy percent decrease in
hospitalization of infected people.
In very remote areas of South America, traditional healers are the only forms of health care people have.
In north Aymara and south Mapuche, where the indigenous groups have the
strongest voices, they still heavily use traditional medicine. The
government in Chile has implemented an Indigenous Health System to help
strengthen the health care system. Even with Chile's indigenous groups,
Chile still has the best public health services in South America.
They also have the lowest mortality rates in the area. Their health
care policies are centered around family and community well-being by
focusing on the strategies for prevention health strategies. Reports
have shown an increase in mental health issues, diabetes, and
cardiovascular diseases.
South America's economy is developing rapidly and has a great deal of industries.
The major industry in South America are agriculture. Other industries
are fishing, handicrafts, and natural resources. Its trade and
import-export market is continually thriving. In the past South American
countries moved slowly in regards to economic development. South
America began to build its economy ever since World War II. South
America's largest economies are Brazil, Chile, Argentina, and Columbia.
Venezuela, Peru, and Argentina's economy are growing very rapidly.