| Metastasis | |
|---|---|
| Synonyms | metastatic disease |
 | |
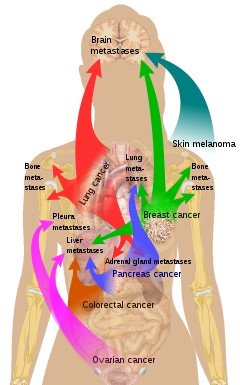
| Illustration showing hematogenous metastasis | |
| Pronunciation |
|
| Specialty | Oncology |
Metastasis is a pathogenic agent's spread from an initial or primary site to a different or secondary site within the host's body; it is typically spoken of as such spread by a cancerous tumor. The newly pathological sites, then, are metastases (mets). It is generally distinguished from cancer invasion, which is the direct extension and penetration by cancer cells into neighboring tissues.
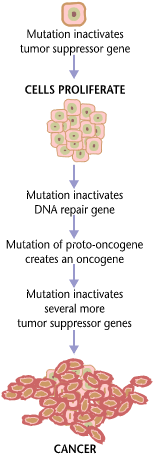
Cancer occurs after cells are genetically altered to proliferate rapidly and indefinitely. This uncontrolled proliferation by mitosis produces a primary heterogeneic tumor. The cells which constitute the tumor eventually undergo metaplasia, followed by dysplasia then anaplasia, resulting in a malignant phenotype. This malignancy allows for invasion into the circulation, followed by invasion to a second site for tumorigenesis.
Some cancer cells known as circulating tumor cells acquire the ability to penetrate the walls of lymphatic or blood vessels, after which they are able to circulate through the bloodstream to other sites and tissues in the body. This process is known (respectively) as lymphatic or hematogenous spread. After the tumor cells come to rest at another site, they re-penetrate the vessel or walls and continue to multiply, eventually forming another clinically detectable tumor. This new tumor is known as a metastatic (or secondary) tumor. Metastasis is one of the hallmarks of cancer, distinguishing it from benign tumors. Most cancers can metastasize, although in varying degrees. Basal cell carcinoma, for example, rarely metastasizes.
When tumor cells metastasize, the new tumor is called a secondary or metastatic tumor, and its cells are similar to those in the original or primary tumor. This means that if breast cancer metastasizes to the lungs, the secondary tumor is made up of abnormal breast cells, not of abnormal lung cells. The tumor in the lung is then called metastatic breast cancer, not lung cancer. Metastasis is a key element in cancer staging systems such as the TNM staging system, where it represents the "M". In overall stage grouping, metastasis places a cancer in Stage IV. The possibilities of curative treatment are greatly reduced, or often entirely removed, when a cancer has metastasized.
Signs and symptoms
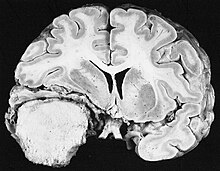
Cut surface of a liver showing multiple paler metastatic nodules originating from pancreatic cancer
Initially, nearby lymph nodes are struck early. The lungs, liver, brain, and bones are the most common metastasis locations from solid tumors.
- In lymph nodes, a common symptom is lymphadenopathy
- Lungs: cough, hemoptysis and dyspnea (shortness of breath)
- Liver: hepatomegaly (enlarged liver), nausea and jaundice
- Bones: bone pain, fracture of affected bones
- Brain: neurological symptoms such as headaches, seizures, and vertigo
Although advanced cancer may cause pain, it is often not the first symptom.
Some patients, however, do not show any symptoms.
When the organ gets a metastatic disease it begins to shrink until its lymph nodes burst, or undergo lysis.
Pathophysiology
Metastatic
tumors are very common in the late stages of cancer. The spread of
metastasis may occur via the blood or the lymphatics or through both
routes. The most common places for the metastases to occur are the lungs, liver, brain, and the bones.
Factors involved
Metastasis
involves a complex series of steps in which cancer cells leave the
original tumor site and migrate to other parts of the body via the
bloodstream, via the lymphatic system, or by direct extension. To do so,
malignant cells break away from the primary tumor and attach to and
degrade proteins that make up the surrounding extracellular matrix
(ECM), which separates the tumor from adjoining tissues. By degrading
these proteins, cancer cells are able to breach the ECM and escape. The
location of the metastases is not always random, with different types of
cancer tending to spread to particular organs and tissues at a rate
that is higher than expected by statistical chance alone.
Breast cancer, for example, tends to metastasize to the bones and
lungs. This specificity seems to be mediated by soluble signal molecules
such as chemokines and transforming growth factor beta. The body resists metastasis by a variety of mechanisms through the actions of a class of proteins known as metastasis suppressors, of which about a dozen are known.
Human cells exhibit three kinds of motion: collective motility, mesenchymal-type movement, and amoeboid movement.
Cancer cells often opportunistically switch between different kinds of
motion. Some cancer researchers hope to find treatments that can stop or
at least slow down the spread of cancer by somehow blocking some
necessary step in one or more kinds of motion.
Cancer researchers studying the conditions necessary for cancer
metastasis have discovered that one of the critical events required is
the growth of a new network of blood vessels, called tumor angiogenesis. It has been found that angiogenesis inhibitors would therefore prevent the growth of metastases.
Several different cell types are critical to tumor growth. In particular, endothelial progenitor cells
have been shown to have a strong influence on the growth of tumor
blood-vessels. Endothelial progenitor cells are also critical for
metastasis and angiogenesis. Endothelial progenitor cells are important in tumor growth, angiogenesis and metastasis, and can be marked using the Inhibitor of DNA Binding 1
(ID1). This novel finding meant that investigators gained the ability
to track endothelial progenitor cells from the bone marrow to the blood
to the tumor-stroma and even incorporated in tumor vasculature.
Endothelial progenitor cells incorporated in tumor vasculature suggests
that this cell type in blood-vessel development is important in a tumor
setting and metastasis. Furthermore, ablation of the endothelial
progenitor cells in the bone marrow can lead to a significant decrease
in tumor growth and vasculature development. Therefore, endothelial
progenitor cells are important in tumor biology and present novel
therapeutic targets.
NFAT
transcription factors are implicated in breast cancer, more
specifically in the process of cell motility as the basis of metastasis
formation. Indeed, NFAT1 (NFATC2) and NFAT5 are pro-invasive and
pro-migratory in breast carcinoma and NFAT3 (NFATc4) is an inhibitor of cell motility.
NFAT1 regulates the expression of the TWEAKR and its ligand TWEAK with the Lipocalin 2 to increase breast-cancer cell invasion and NFAT3 inhibits Lipocalin 2 expression to blunt the cell invasion.
Epigenetic
regulation also plays an important role in the metastatic outgrowth of
disseminated tumor cells. Metastases display alterations in histone
modifications, such as H3K4-methylation and H3K9-methylation, when
compared to matching primary tumors.
These epigenetic modifications in metastases may allow the
proliferation and survival of disseminated tumor cells in distant
organs.
A recent study shows that PKC-iota promotes melanoma cell
invasion by activating Vimentin during EMT. PKC-iota inhibition or
knockdown resulted an increase E-cadherin and RhoA levels while
decreasing total Vimentin, phophorylated Vimentin (S39) and Par6 in
metastatic melanoma cells. These results suggested that PKC-ι is
involved in signaling pathways which upregulate EMT in melanoma thereby
directly stimulates metastasis.
Recently, a series of high-profile experiments suggests that the
co-option of intercellular cross-talk mediated by exosome vesicles is a
critical factor involved in all steps of the invasion-metastasis
cascade.
Routes
Main sites of metastases for some common cancer types. Primary cancers are denoted by "...cancer" and their main metastasis sites are denoted by "...metastases".
Metastasis occurs by the following four routes:
Transcoelomic
The spread of a malignancy into body cavities can occur via penetrating the surface of the peritoneal, pleural, pericardial, or subarachnoid spaces. For example, ovarian tumors can spread transperitoneally to the surface of the liver.
Lymphatic spread
Lymphatic spread allows the transport of tumor cells to regional lymph nodes
near the primary tumor and ultimately, to other parts of the body. This
is called nodal involvement, positive nodes, or regional disease.
"Positive nodes" is a term that would be used by medical specialists to
describe regional lymph nodes that tested positive for malignancy. It is
common medical practice to test by biopsy at least one lymph node near a
tumor site when carrying out surgery to examine or remove a tumor. This
lymph node is then called a sentinel lymph node.
Lymphatic spread is the most common route of initial metastasis for carcinomas. In contrast, it is uncommon for a sarcoma
to metastasize via this route. Localized spread to regional lymph nodes
near the primary tumor is not normally counted as a metastasis,
although this is a sign of a worse outcome.
The lymphatic system does eventually drain from the thoracic duct and right lymphatic duct into the systemic venous system at the venous angle and into the brachiocephalic veins, and therefore these metastatic cells can also eventually spread through the haematogenous route.
Lymph node with almost complete replacement by metastatic melanoma. The brown pigment is focal deposition of melanin
Hematogenous spread
This is typical route of metastasis for sarcomas, but it is also the favored route for certain types of carcinoma, such as renal cell carcinoma originating in the kidney.
Because of their thinner walls, veins are more frequently invaded than
are arteries, and metastasis tends to follow the pattern of venous flow. That is, hematogenous spread often follows distinct patterns depending on the location of the primary tumor. For example, colorectal cancer spreads primarily through the portal vein to the liver.
Canalicular spread
Some tumors, especially carcinomas
may metastasize along anatomical canalicular spaces. These spaces
include for example the bile ducts, the urinary system, the airways and
the subarachnoid space.
The process is similar to that of transcoelomic spread. However, often
it remains unclear whether simultaneously diagnosed tumors of a
canalicular system are one metastatic process or in fact independent
tumors caused by the same agent (field cancerization).
Organ-specific targets
There
is a propensity for certain tumors to seed in particular organs. This
was first discussed as the "seed and soil" theory by Stephen Paget in 1889. The propensity for a metastatic cell to spread to a particular organ is termed 'organotropism'. For example, prostate cancer usually metastasizes to the bones. In a similar manner, colon cancer has a tendency to metastasize to the liver. Stomach cancer often metastasizes to the ovary in women, then it is called a Krukenberg tumor.
According to the "seed and soil" theory, it is difficult for
cancer cells to survive outside their region of origin, so in order to
metastasize they must find a location with similar characteristics. For example, breast tumor cells, which gather calcium ions from breast milk, metastasize to bone tissue, where they can gather calcium ions from bone. Malignant melanoma spreads to the brain, presumably because neural tissue and melanocytes arise from the same cell line in the embryo.
In 1928, James Ewing
challenged the "seed and soil" theory and proposed that metastasis
occurs purely by anatomic and mechanical routes. This hypothesis has
been recently utilized to suggest several hypotheses about the life
cycle of circulating tumor cells (CTCs) and to postulate that the
patterns of spread could be better understood through a 'filter and
flow' perspective.
However, contemporary evidences indicate that the primary tumor may
dictate organotropic metastases by inducing the formation of pre-metastatic niches at distant sites, where incoming metastatic cells may engraft and colonize.
Specifically, exosome vesicles secreted by tumors have been shown to
home to pre-metastatic sites, where they activate pro-metastatic
processes such as angiogenesis and modify the immune contexture, so as
to foster a favorable microenvironment for secondary tumor growth.
Metastasis and primary cancer
It
is theorized that metastasis always coincides with a primary cancer,
and, as such, is a tumor that started from a cancer cell or cells in
another part of the body. However, over 10% of patients presenting to oncology units
will have metastases without a primary tumor found. In these cases,
doctors refer to the primary tumor as "unknown" or "occult," and the
patient is said to have cancer of unknown primary origin (CUP) or unknown primary tumors (UPT). It is estimated that 3% of all cancers are of unknown primary origin. Studies have shown that, if simple questioning does not reveal the cancer's source (coughing up blood—"probably lung", urinating blood—"probably bladder"), complex imaging will not either. In some of these cases a primary tumor may appear later.
The use of immunohistochemistry
has permitted pathologists to give an identity to many of these
metastases. However, imaging of the indicated area only occasionally
reveals a primary. In rare cases (e.g., of melanoma), no primary tumor is found, even on autopsy.
It is therefore thought that some primary tumors can regress
completely, but leave their metastases behind. In other cases, the tumor
might just be too small and/or in an unusual location to be diagnosed.
Diagnosis
The
cells in a metastatic tumor resemble those in the primary tumor. Once
the cancerous tissue is examined under a microscope to determine the
cell type, a doctor can usually tell whether that type of cell is
normally found in the part of the body from which the tissue sample was
taken.
For instance, breast cancer
cells look the same whether they are found in the breast or have spread
to another part of the body. So, if a tissue sample taken from a tumor
in the lung contains cells that look like breast cells, the doctor
determines that the lung tumor is a secondary tumor. Still, the
determination of the primary tumor can often be very difficult, and the
pathologist may have to use several adjuvant techniques, such as immunohistochemistry, FISH (fluorescent in situ hybridization), and others. Despite the use of techniques, in some cases the primary tumor remains unidentified.
Metastatic cancers may be found at the same time as the primary
tumor, or months or years later. When a second tumor is found in a
patient that has been treated for cancer in the past, it is more often a
metastasis than another primary tumor.
It was previously thought that most cancer cells have a low
metastatic potential and that there are rare cells that develop the
ability to metastasize through the development of somatic mutations.
According to this theory, diagnosis of metastatic cancers is only
possible after the event of metastasis. Traditional means of diagnosing
cancer (e.g. a biopsy)
would only investigate a subpopulation of the cancer cells and would
very likely not sample from the subpopulation with metastatic potential.
The somatic
mutation theory of metastasis development has not been substantiated in
human cancers. Rather, it seems that the genetic state of the primary
tumor reflects the ability of that cancer to metastasize. Research comparing gene expression between primary and metastatic adenocarcinomas
identified a subset of genes whose expression could distinguish primary
tumors from metastatic tumors, dubbed a "metastatic signature." Up-regulated genes in the signature include: SNRPF, HNRPAB, DHPS and securin. Actin, myosin and MHC class II
down-regulation was also associated with the signature. Additionally,
the metastatic-associated expression of these genes was also observed in
some primary tumors, indicating that cells with the potential to
metastasize could be identified concurrently with diagnosis of the
primary tumor. Recent work identified a form of genetic instability in cancer called chromosome instability (CIN) as a driver of metastasis.
In aggressive cancer cells, loose DNA fragments from unstable
chromosomes spill in the cytosol leading to the chronic activation of
innate immune pathways, which are hijacked by cancer cells to spread to
distant organs.
Expression of this metastatic signature has been correlated with a
poor prognosis and has been shown to be consistent in several types of
cancer. Prognosis was shown to be worse for individuals whose primary
tumors expressed the metastatic signature. Additionally, the expression of these metastatic-associated genes was shown to apply to other cancer types in addition to adenocarcinoma. Metastases of breast cancer, medulloblastoma and prostate cancer all had similar expression patterns of these metastasis-associated genes.
The identification of this metastasis-associated signature
provides promise for identifying cells with metastatic potential within
the primary tumor and hope for improving the prognosis of these
metastatic-associated cancers. Additionally, identifying the genes
whose expression is changed in metastasis offers potential targets to
inhibit metastasis.
- Micrograph of thyroid cancer (papillary thyroid carcinoma) in a lymph node of the neck. H&E stain
- CT image of multiple liver metastases
- CT image of a lung metastasis
- Metastasis proven by liver biopsy (tumor (adenocarcinoma) - lower two-thirds of image). H&E stain.
Management
Treatment
and survival is determined, to a great extent, by whether or not a
cancer remains localized or spreads to other locations in the body. If
the cancer metastasizes to other tissues or organs it usually
dramatically increases a patient's likelihood of death. Some
cancers—such as some forms of leukemia, a cancer of the blood, or malignancies in the brain—can kill without spreading at all.
Once a cancer has metastasized it may still be treated with radiosurgery, chemotherapy, radiation therapy, biological therapy, hormone therapy, surgery,
or a combination of these interventions ("multimodal therapy"). The
choice of treatment depends on a large number of factors, including the
type of primary cancer,
the size and location of the metastases, the patient's age and general
health, and the types of treatments used previously. In patients
diagnosed with CUP it is often still possible to treat the disease even
when the primary tumor cannot be located.
Current treatments are rarely able to cure metastatic cancer though some tumors, such as testicular cancer and thyroid cancer, are usually curable.
Palliative care,
care aimed at improving the quality of life of people with major
illness, has been recommended as part of management programs for
metastasis.
Research
Although metastasis is widely accepted to be the result of the tumor cells migration, there is a hypothesis saying that some metastases are the result of inflammatory processes by abnormal immune cells.
The existence of metastatic cancers in the absence of primary tumors
also suggests that metastasis is not always caused by malignant cells
that leave primary tumors.
History
In
March 2014 researchers discovered the oldest complete example of a human
with metastatic cancer. The tumors had developed in a 3,000-year-old
skeleton found in 2013 in a tomb in Sudan
dating back to 1200 BC. The skeleton was analyzed using radiography and
a scanning electron microscope. These findings were published in the Public Library of Science journal.
Etymology
Metastasis is a Greek word meaning "displacement", from μετά, meta, "next", and στάσις, stasis, "placement".