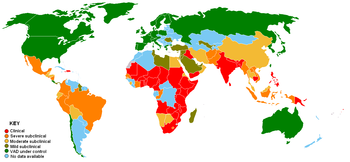
Prevalence of vitamin A deficiency, 1995.
Clinical
Severe subclinical
Moderate subclinical
|
Mild subclinical
VAD under control
No data available
|
Vitamin A deficiency (VAD) or hypovitaminosis A is a lack of vitamin A in blood and tissues. It is common in poorer countries, but rarely is seen in more developed countries. Nyctalopia (night blindness) is one of the first signs of VAD. Xerophthalmia, keratomalacia, and complete blindness can also occur since vitamin A has a major role in phototransduction. The three forms of vitamin A include retinols, beta-carotenes, and carotenoids.
Vitamin A deficiency is the leading cause of preventable childhood blindness, and is critical to achieving Millennium Development Goal 4 to reduce child mortality.
About 250,000 to 500,000 malnourished children in the developing world
go blind each year from a deficiency of vitamin A, around half of whom
die within a year of becoming blind. The United Nations Special Session on Children in 2002 set a goal of the elimination of VAD by 2010.
The prevalence of night blindness due to VAD is also high among
pregnant women in many developing countries. VAD also contributes to maternal mortality and other poor outcomes in pregnancy and lactation.
VAD also diminishes the ability to fight infections. In countries where children are not immunized, infectious diseases such as measles have higher fatality rates. As elucidated by Alfred Sommer,
even mild, subclinical deficiency can also be a problem, as it may
increase children's risk of developing respiratory and diarrheal
infections, decrease growth rate, slow bone development, and decrease
likelihood of survival from serious illness.
VAD is estimated to affect about one-third of children under the age of five around the world. It is estimated to claim the lives of 670,000 children under five annually.
Around 250,000–500,000 children in developing countries become blind
each year owing to VAD, with the highest prevalence in Southeast Asia
and Africa. According to the World Health Organization (WHO), VAD is
under control in the United States, but in developing countries, VAD is a
significant concern. Globally, 65% of all children aged 6 to 59 months
received two doses of vitamin A in 2013, fully protecting them against
VAD (80% in the least developed countries).
Signs and symptoms
The
common cause of blindness in developing countries is Vitamin A
deficiency (VAD). The WHO estimated in 1995 that 13.8 million children
to have some degree of visual loss related to VAD.
Night blindness and its worsened condition, xerophthalmia, are markers of Vitamin A deficiency (VAD) and collections of keratin in the conjunctiva, known as Bitot's spots, can be seen. Imtiaz's sign is the earliest ocular sign of VAD. Conjunctival epithelial defects occur around lateral aspect of the limbus
in the subclinical stage of VAD. These conjunctival epithelial defects
are not visible on a biomicroscope, but they take up black stain and
become readily visible after instillation of kajal (surma); this is called "Imtiaz's sign".
VAD can also lead to impaired immune function, cancer, and birth
defects. Vitamin A deficiency is one of several hypovitaminoses
implicated in follicular hyperkeratosis.
Night blindness
Night
blindness is the difficulty for the eyes to adjust to dim light.
Affected individuals are unable to distinguish images in low levels of
illumination. People with night blindness have poor vision in the
darkness, but see normally when adequate light is present.
VAD affects vision by inhibiting the production of rhodopsin, the eye pigment responsible for sensing low-light situations. Rhodopsin is found in the retina and is composed of retinal (an active form of vitamin A) and opsin
(a protein). Because the body cannot create retinal in sufficient
amounts, a diet low in vitamin A leads to a decreased amount of
rhodopsin in the eye, as the retinal is inadequate to bind with opsin.
Night blindness results.
Night blindness caused by VAD has been associated with the loss of goblet cells in the conjunctiva, a membrane covering the outer surface of the eye. Goblet cells are responsible for secretion of mucus,
and their absence results in xerophthalmia, a condition where the eyes
fail to produce tears. Dead epithelial and microbial cells accumulate on
the conjunctiva and form debris that can lead to infection and possibly
blindness.
Decreasing night blindness requires the improvement of vitamin A
status in at-risk populations. Supplements and fortification of food
have been shown to be effective interventions. Supplement treatment for
night blindness includes massive doses of vitamin A (200,000 IU) in the
form of retinyl palmitate to be taken by mouth, which is administered
two to four times a year.
Intramuscular injections are poorly absorbed and are ineffective in
delivering sufficient bioavailable vitamin A. Fortification of food with
vitamin A is costly, but can be done in wheat, sugar, and milk.
Households may circumvent expensive fortified food by altering dietary
habits. Consumption of yellow-orange fruits and vegetables rich in carotenoids, specifically beta-carotene,
provides provitamin A precursors that can prevent VAD-related night
blindness. However, the conversion of carotene to retinol varies from
person to person and bioavailability of carotene in food varies.
Causes
In addition to dietary problems, other causes of VAD are known. Iron deficiency
can affect vitamin A uptake; other causes include fibrosis, pancreatic
insufficiency, inflammatory bowel disease, and small-bowel bypass
surgery.
Excess alcohol consumption can deplete vitamin A, and a stressed liver
may be more susceptible to vitamin A toxicity. People who consume large
amounts of alcohol should seek medical advice before taking vitamin A
supplements. In general, people should also seek medical advice before
taking vitamin A supplements if they have any condition associated with
fat malabsorption such as pancreatitis, cystic fibrosis, tropical sprue, and biliary obstruction.
Other causes of vitamin A deficiency are inadequate intake, fat
malabsorption, or liver disorders. Deficiency impairs immunity and
hematopoiesis and causes rashes and typical ocular effects (e.g.,
xerophthalmia, night blindness).
Infection rates
Along
with poor diet, a large amount of infection and disease is present in
many developing communities. Infection is very draining on vitamin A
reserves and this vitamin A deficit leaves the individual more
susceptible to infection;
increased documentation of xerophthalmia has been seen after an
outbreak of measles and the varying stages of xerophthalmia become a
good reference point for the extent of deficiency (with mortality
increasing with severity of the eye disease). In a longitudinal study of
preschool Indonesian children, susceptibility to disease increased nine
times when severe VAD was present.
The reason for the increased infection rate in vitamin A
deficient populations is the T-killer cells require the retinol
metabolite retinoic acid to proliferate correctly. Retinoic acid is a ligand for nuclear retinoic acid receptors that bind the promoter regions of specific genes, thus activating transcription and stimulating T cell replication.
A vitamin A-deficient diet will have a very limited amount of retinol,
so cell proliferation and replication will be suppressed, contributing
to a reduced number of T-cells and lymphocytes. Suppression of these
result in a lack of immune reaction if pathogens become present in the
body and consequently a greater susceptibility to incubation of disease.
VAD and infections aggravate each other, so with infection,
vitamin A levels are depleted, which in turn reduces intestinal
absorption of vitamin A.
Very often seen with VAD is protein energy malnutrition, in which the
synthesis of retinol binding protein (RBP) is decreased, consequently
the uptake of retinol is reduced.
This leads to an inability to use any vitamin A present as the RBP is
absent, so the retinol cannot be transported to the liver, maximising
the VAD.
Treatment
Treatment of VAD can be undertaken with both oral vitamin A and injectable forms, generally as vitamin A palmitate.
- As an oral form, the supplementation of vitamin A is effective for lowering the risk of morbidity, especially from severe diarrhea, and reducing mortality from measles and all-cause mortality. Vitamin A supplementation of children under five who are at risk of VAD can reduce all‐cause mortality by 23%. Some countries where VAD is a public-health problem address its elimination by including vitamin A supplements available in capsule form with national immunization days (NIDs) for polio eradication or measles. Additionally, the delivery of vitamin A supplements, during integrated child health events such as child health days, have helped ensure high coverage of vitamin A supplementation in a large number of least developed countries. Child health events enable many countries in West and Central Africa to achieve over 80% coverage of vitamin A supplementation. According to UNICEF data, in 2013 worldwide, 65% of children between the ages of 6 and 59 months were fully protected with two high-dose vitamin A supplements. Vitamin A capsules cost about US$0.02. The capsules are easy to handle; they do not need to be stored in a refrigerator or vaccine carrier. When the correct dosage is given, vitamin A is safe and has no negative effect on seroconversion rates for oral polio or measles vaccines. However, because the benefit of vitamin A supplements is transient, children need them regularly every four to six months. Since NIDs provide only one dose per year, NIDs-linked vitamin A distribution must be complemented by other programs to maintain vitamin A in children Maternal high supplementation benefits both mother and breast-fed infant: high-dose vitamin A supplementation of the lactating mother in the first month postpartum can provide the breast-fed infant with an appropriate amount of vitamin A through breast milk. However, high-dose supplementation of pregnant women should be avoided because it can cause miscarriage and birth defects.
- Food fortification is also useful for improving VAD. A variety of oily and dry forms of the retinol esters, retinyl acetates, and retinyl palmitate are available for food fortification of vitamin A. Margarine and oil are the ideal food vehicles for vitamin A fortification. They protect vitamin A from oxidation during storage and prompt absorption of vitamin A. Beta-carotene and retinyl acetate or retinyl palmitate are used as a form of vitamin A for vitamin A fortification of fat-based foods. Fortification of sugar with retinyl palmitate as a form of vitamin A has been used extensively throughout Central America. Cereal flours, milk powder, and liquid milk are also used as food vehicles for vitamin A fortification. Genetic engineering is another method that could be used to fortify food, and golden rice is a genetic engineering project designed to fortify rice with beta-carotene (which humans can convert into vitamin A) and thereby prevent and/or treat VAD. Although opposition to genetically modified foods resulted in the destruction of a field trial of golden rice prototypes in 2013, development of golden rice has proceeded and developers are currently (as of September 2018) awaiting regulatory approval to publicly release golden rice in the Philippines.
- Dietary diversification can also control VAD. Nonanimal sources of vitamin A like fruits and vegetables contain preformed vitamin A and account for greater than 80% of intake for most individuals in the developing world. The increase in consumption of vitamin A-rich foods of animal origin has beneficial effects on VAD.
The richest animal sources of vitamin A (retinol) are livers (beef liver - 100 grams provides around 32,000 IUs, and cod liver oil - 10 g provides around 10,000 IUs ).
Researchers at the U. S. Agricultural Research Service
have been able to identify genetic sequences in corn that are
associated with higher levels of beta-carotene, the precursor to vitamin
A. They found that breeders can cross certain variations of corn to
produce a crop with an 18-fold increase in beta-carotene. Such
advancements in nutritional plant breeding could one day aid in the
illnesses related to VAD in developing countries.
Global initiatives
Global
efforts to support national governments in addressing VAD are led by
the Global Alliance for Vitamin A (GAVA), which is an informal
partnership between A2Z, the Canadian International Development Agency, Helen Keller International, Micronutrient Initiative, UNICEF, USAID, and the World Bank. Joint GAVA activity is coordinated by the Micronutrient Initiative.
Vitamin Angels has committed itself to eradicating childhood blindness
due to VAD on the planet by the year 2020. Operation 20/20 was launched
in 2007 and will cover 18 countries. The program gives children two
high-dose vitamin A and antiparasitic supplements (twice a year for four
years), which provides children with enough of the nutrient during
their most vulnerable years to prevent them from going blind and
suffering from other life-threatening diseases related to VAD.
About 75% the vitamin A required for supplementation activity by developing countries is supplied by the Micronutrient Initiative with support from the Canadian International Development Agency.
An estimated 1.25 million deaths due to VAD have been averted in 40 countries since 1998.
In 2008, an estimated annual investment of US$60 million in
vitamin A and zinc supplementation combined would yield benefits of more
than US$1 billion per year, with every dollar spent generating benefits
of more than US$17. These combined interventions were ranked by the Copenhagen Consensus 2008 as the world’s best development investment.
Epidemiology
Disability-adjusted life year for vitamin A deficiency per 100,000 inhabitants in 2002.
no data
less than 35
35–70
70–105
105–140
140–175
175–210
210–245
245–280
280–315
315–350
350–400
more than 400