From Wikipedia, the free encyclopedia
| Porphyria |
|---|
 |
| Left
figure is urine on the first day while the right figure is urine after
three days of sun exposures showing the classic change in color to
purple. |
| Pronunciation |
|
|---|
| Specialty | Hematology, dermatology, neurology |
|---|
| Symptoms | Depending on subtype–abdominal pain, chest pain, vomiting, confusion, constipation, fever, seizures, blisters with sunlight |
|---|
| Usual onset | Recurrent attacks that last days to weeks |
|---|
| Causes | Usually genetic |
|---|
| Diagnostic method | Blood, urine, and stool tests, genetic testing |
|---|
| Differential diagnosis | Lead poisoning, alcoholic liver disease |
|---|
| Treatment | Depends on type and symptoms |
|---|
| Frequency | 1 to 100 in 50,000 people |
|---|
Porphyria is a group of diseases in which substances called
porphyrins build up, negatively affecting the skin or
nervous system. The types that affect the nervous system are also known as
acute porphyria, as symptoms are rapid in onset and last a short time. Symptoms of an attack include
abdominal pain,
chest pain,
vomiting, confusion,
constipation,
fever,
high blood pressure, and
high heart rate. The attacks usually last for days to weeks. Complications may include
paralysis,
low blood sodium levels, and
seizures. Attacks may be triggered by
alcohol,
smoking, hormonal changes, fasting, stress, or certain medications. If the skin is affected,
blisters or itching may occur with sunlight exposure.
Most types of porphyria are
inherited from one or both of a person's parents, and are due to a
mutation in one of the
genes that
make heme. They may be inherited in an
autosomal dominant,
autosomal recessive, or
X-linked dominant manner. One type,
porphyria cutanea tarda, may also be due to
increased iron in the liver,
hepatitis C, alcohol, or
HIV/AIDS. The underlying mechanism results in a decrease in the amount of
heme produced and a build-up of substances involved in making heme. Porphyrias may also be classified by whether the liver or the
bone marrow is affected. Diagnosis is typically made by blood, urine, and stool tests.
Genetic testing may be done to determine the specific mutation.
Treatment depends on the type of porphyria and a person's symptoms. The treatment of porphyria of the skin generally involves the avoidance of sunlight. The treatment for acute porphyria may involve giving intravenous heme or a
glucose solution. Rarely, a
liver transplant may be carried out.
The precise frequency of porphyria is unclear but it is estimated that it affects between 1 and 100 per 50,000 people. Rates vary around the world. Porphyria cutanea tarda is believed to be the most common type. The disease was described as early as 370 BC by
Hippocrates. The underlying mechanism was first described by
Felix Hoppe-Seyler in 1871. The name
porphyria is from the
Greek πορφύρα,
porphyra, meaning "
purple", a reference to the color of the urine that may occur during an attack.
Signs and symptoms
A skin rash in a person with porphyria
Acute porphyrias
The most severe episodes may involve neurological complications:
typically motor neuropathy (severe dysfunction of the peripheral nerves
that innervate muscle), which leads to muscle weakness and potentially
to
quadriplegia (paralysis of all four limbs) and
central nervous system symptoms such as
seizures and
coma. Occasionally, there may be short-lived psychiatric symptoms such as anxiety, confusion,
hallucinations, and, very rarely, overt psychosis. All these symptoms resolve once the acute attack passes.
Given the many presentations and the relatively low occurrence of
porphyria, patients may initially be suspected to have other, unrelated
conditions. For instance, the polyneuropathy of acute porphyria may be
mistaken for
Guillain–Barré syndrome, and porphyria testing is commonly recommended in those situations.
Chronic porphyrias
The non-acute porphyrias are X-linked dominant protoporphyria (XLDPP), congenital
erythropoietic porphyria (CEP),
porphyria cutanea tarda (PCT), and
erythropoietic protoporphyria
(EPP). None of these are associated with acute attacks; their primary
manifestation is with skin disease. For this reason, these four
porphyrias—along with two acute porphyrias, VP and HCP, that may also
involve skin manifestations—are sometimes called cutaneous porphyrias.
Skin disease is encountered where excess porphyrins accumulate in
the skin. Porphyrins are photoactive molecules, and exposure to light
results in promotion of electrons to higher energy levels. When these
return to the resting energy level or ground state, energy is released.
This accounts for the property of fluorescence typical of the
porphyrins. This causes local skin damage.
Two distinct patterns of skin disease are seen in porphyria:
- Immediate photosensitivity. This is typical of XLDPP and EPP. Following a variable period of sun exposure—typically
about 30 minutes—patients complain of severe pain, burning, and
discomfort in exposed areas. Typically, the effects are not visible,
though occasionally there may be some redness and swelling of the skin.
- Vesiculo-erosive skin disease. This—a reference to the characteristic blistering
(vesicles) and open sores (erosions) noted in patients—is the pattern
seen in CEP, PCT, VP, and HCP. The changes are noted only in sun-exposed
areas such as the face and back of the hands. Milder skin disease, such
as that seen in VP and HCP, consists of increased skin fragility in
exposed areas with a tendency to form blisters and erosions,
particularly after minor knocks or scrapes. These heal slowly, often
leaving small scars that may be lighter or darker than normal skin. More
severe skin disease is sometimes seen in PCT, with prominent lesions,
darkening of exposed skin such as the face, and hypertrichosis:
abnormal hair growth on the face, particularly the cheeks. The most
severe disease is seen in CEP and a rare variant of PCT known as hepatoerythropoietic porphyria
(HEP); symptoms include severe shortening of digits, loss of skin
appendages such as hair and nails, and severe scarring of the skin with
progressive disappearance of ears, lips, and nose. Patients may also
show deformed, discolored teeth or gum and eye abnormalities.
Cause
The porphyrias are generally considered genetic in nature.
Genetics
Subtypes of porphyrias depend on which enzyme is deficient.
| Porphyria type
|
Deficient enzyme
|
Type of porphyria
|
Inheritance
|
Symptoms
|
Prevalence
|
| X-linked dominant protoporphyria (XLDPP)
|
5-aminolevulinate (ALA) synthase (ALAS)
|
Erythropoietic
|
X-linked dominant
|
Photosensitivity, cirrhosis
|
Rare; about 50 cases reported
|
| Aminolevulinate dehydratase deficiency porphyria (ALADP)
|
5-aminolevulinate dehydratase (ALAD)
|
Hepatic
|
Autosomal recessive
|
Abdominal pain, neuropathy
|
Extremely rare; fewer than 10 cases ever reported.
|
| Acute intermittent porphyria (AIP)
|
Hydroxymethylbilane synthase (HMBS) formerly porphobilinogen deaminase (PBGD)
|
Hepatic
|
Autosomal dominant
|
Periodic abdominal pain, peripheral neuropathy, psychiatric disorders, tachycardia
|
|
| Congenital erythropoietic porphyria (CEP)
|
uroporphyrinogen synthase (UROS)
|
Erythropoietic
|
Autosomal recessive
|
Severe photosensitivity with erythema, swelling and blistering. Hemolytic anemia, splenomegaly
|
1 in 1,000,000 or less.
|
| Porphyria cutanea tarda (PCT)
|
uroporphyrinogen decarboxylase (UROD)
|
Hepatic
|
Approximately 80% sporadic, 20% Autosomal dominant
|
Photosensitivity with vesicles and bullae
|
1 in 10,000
|
| Hereditary coproporphyria (HCP)
|
coproporphyrinogen oxidase (CPOX)
|
Hepatic
|
Autosomal dominant
|
Photosensitivity, neurologic symptoms, colic
|
1 in 500,000
|
| Harderoporphyria
|
coproporphyrinogen oxidase (CPOX)
|
Erythropoietic
|
Autosomal recessive
|
Jaundice, anemia, enlarged liver and spleen, often neonatal. Photosensitivity later.
|
Extremely rare; fewer than 10 cases ever reported.
|
| Variegate porphyria (VP)
|
protoporphyrinogen oxidase (PPOX)
|
Hepatic
|
Autosomal dominant
|
Photosensitivity, neurologic symptoms, developmental delay
|
1 in 300 in South Africa
1 in 75,000 in Finland
|
| Erythropoietic protoporphyria (EPP)
|
Ferrochelatase (FECH)
|
Erythropoietic
|
Autosomal dominant
|
Photosensitivity with skin lesions. Gallstones, mild liver dysfunction |
1 in 75,000–200,000
|
In the autosomal recessive types, if a person inherits a single gene
they may become a carriers. Generally they do not have symptoms, but may
pass the gene onto offspring.
Triggers
Acute
porphyria can be triggered by a number of drugs, most of which are
believed to trigger it by interacting with enzymes in the liver which
are made with heme. Such drugs include:
- Sulfonamides, including sulfadiazine, sulfasalazine and trimethoprim/sulfamethoxazole.
- Sulfonylureas like glibenclamide, gliclazide and glimepiride, although glipizide is thought to be safe.
- Barbiturates including thiopental, phenobarbital, primidone, etc.
- Systemic treatment with antifungals including fluconazole, griseofulvin, ketoconazole and voriconazole. (Topical use of these agents is thought to be safe due to minimal systemic absorption.)
- Certain antibiotics like rifapentine, rifampicin, rifabutine, isoniazid, nitrofurantoin and, possibly, metronidazole.
- Ergot derivatives including dihydroergotamine, ergometrine, ergotamine, methysergide, etc.
- Certain antiretroviral medications (e.g. indinavir, nevirapine, ritonavir, saquinavir, etc.)
- Progestogens
- Some anticonvulsants including: carbamazepine, ethosuximide, phenytoin, topiramate, valproate.
- Some painkillers like dextropropoxyphene, ketorolac, metamizole, pentazocine
- Some cancer treatments like bexarotene, busulfan, chlorambucil, estramustine, etoposide, flutamide, idarubicin, ifosfamide, irinotecan, ixabepilone, letrozole, lomustine, megestrol, mitomycin, mitoxantrone, paclitaxel, procarbazine, tamoxifen, topotecan
- Some antidepressants like imipramine, phenelzine, trazodone
- Some antipsychotics like risperidone, ziprasidone
- Some retinoids used for skin conditions like acitretin and isotretinoin
- Miscellaneous others including: cocaine, methyldopa, fenfluramine, disulfiram, orphenadrine, pentoxifylline, and sodium aurothiomalate.
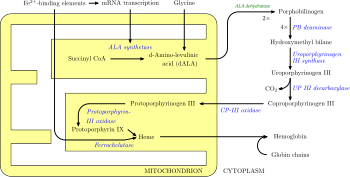
Pathogenesis
The body requires porphyrins to produce
heme,
which is used to carry oxygen in the blood among other things, but in
the porphyrias there is a deficiency (inherited or acquired) of the
enzymes
that transform the various porphyrins into others, leading to
abnormally high levels of one or more of these substances. Porphyrias
are classified in two ways, by symptoms and by pathophysiology.
Physiologically, porphyrias are classified as liver or erythropoietic
based on the sites of accumulation of
heme precursors, either in the
liver or in the
bone marrow and
red blood cells.
Deficiency in the
enzymes of the porphyrin pathway leads to insufficient production of
heme.
Heme function plays a central role in cellular
metabolism. This is not the main problem in the porphyrias; most
heme synthesis enzymes—even dysfunctional
enzymes—have enough residual activity to assist in
heme biosynthesis. The principal problem in these deficiencies is the accumulation of
porphyrins, the
heme
precursors, which are toxic to tissue in high concentrations. The
chemical properties of these intermediates determine the location of
accumulation, whether they induce
photosensitivity, and whether the intermediate is excreted (in the
urine or
feces).
There are eight
enzymes in the
heme biosynthetic pathway, four of which—the first one and the last three—are in the
mitochondria, while the other four are in the
cytosol. Defects in any of these can lead to some form of porphyria.
Variegate porphyria (also
porphyria variegata or
mixed porphyria), which results from a partial deficiency in
PROTO oxidase, manifests itself with skin lesions similar to those of
porphyria cutanea tarda combined with acute neurologic attacks.
Hereditary coproporphyria,
which is characterized by a deficiency in coproporphyrinogen oxidase,
coded for by the CPOX gene, may also present with both acute neurologic
attacks and cutaneous lesions. All other porphyrias are either skin- or
nerve-predominant.
Diagnosis
Porphyrin studies
Porphyria is diagnosed through biochemical analysis of
blood,
urine, and
stool. In general, urine estimation of
porphobilinogen
(PBG) is the first step if acute porphyria is suspected. As a result of
feedback, the decreased production of heme leads to increased
production of precursors, PBG being one of the first substances in the
porphyrin synthesis pathway. In nearly all cases of acute porphyria syndromes, urinary PBG is markedly elevated except for the very rare
ALA dehydratase deficiency or in patients with symptoms due to
hereditary tyrosinemia type I. In cases of
mercury- or
arsenic poisoning-induced
porphyria, other changes in porphyrin profiles appear, most notably
elevations of uroporphyrins I & III, coproporphyrins I & III,
and pre-coproporphyrin.
Repeat testing during an attack and subsequent attacks may be
necessary in order to detect a porphyria, as levels may be normal or
near-normal between attacks. The urine screening test has been known to
fail in the initial stages of a severe, life-threatening attack of
acute intermittent porphyria.
Up to 90% of the genetic carriers of the more common, dominantly
inherited acute hepatic porphyrias (acute intermittent porphyria,
hereditary
coproporphyria, variegate porphyria) have been noted in DNA tests to be latent for classic symptoms and may require
DNA or
enzyme testing. The exception to this may be latent post-puberty genetic carriers of hereditary
coproporphyria.
As most porphyrias are
rare conditions,
general hospital labs typically do not have the expertise, technology,
or staff time to perform porphyria testing. In general, testing involves
sending samples of blood, stool, and urine to a reference laboratory. All samples to detect porphyrins must be handled properly. Samples should be taken during an acute attack; otherwise a
false negative result may occur. Samples must be protected from light and either refrigerated or preserved.
If all the porphyrin studies are negative, one must consider
pseudoporphyria. A careful medication review often will find the cause of pseudoporphyria.
Additional tests
Management
Acute porphyria
Carbohydrate administration
Often,
empirical treatment is required if the diagnostic suspicion of a
porphyria is high since acute attacks can be fatal. A high-carbohydrate
diet is typically recommended; in severe attacks, a
dextrose 10% infusion is commenced, which may aid in recovery by suppressing
heme
synthesis, which in turn reduces the rate of porphyrin accumulation.
However, this can worsen hyponatraemia and should be done with extreme
caution as it can prove fatal.
Heme analogs
Hematin (trade name Panhematin) and
heme arginate (trade name NormoSang) are the drugs of choice in acute porphyria, in the
United States and the
United Kingdom,
respectively. These drugs need to be given very early in an attack to
be effective; effectiveness varies amongst individuals. They are not
curative drugs but can shorten attacks and reduce the intensity of an
attack. Side effects are rare but can be serious. These heme-like
substances theoretically inhibit ALA synthase and hence the accumulation
of toxic precursors. In the United Kingdom, supplies of NormoSang are
kept at two national centers; emergency supply is available from
St Thomas's Hospital, London. In the United States,
Lundbeck manufactures and supplies Panhematin for infusion.
Heme arginate (NormoSang) is used during crises but also in preventive treatment to avoid crises, one treatment every 10 days.
Any sign of low blood sodium (
hyponatremia) or weakness should be treated with the addition of hematin, heme arginate, or even
tin mesoporphyrin,
as these are signs of impending syndrome of inappropriate antidiuretic
hormone (SIADH) or peripheral nervous system involvement that may be
localized or severe, progressing to
bulbar paresis and respiratory paralysis.
Cimetidine
Cimetidine has also been reported to be effective for acute porphyric crisis and possibly effective for long-term prophylaxis.
Symptom control
Pain is severe, frequently out of proportion to physical signs, and often requires the use of
opiates to reduce it to tolerable levels. Pain should be treated as early as medically possible.
Nausea can be severe; it may respond to
phenothiazine
drugs but is sometimes intractable. Hot baths and showers may lessen
nausea temporarily, though caution should be used to avoid burns or
falls.
Early identification
It is recommended that patients with a history of acute porphyria, and even genetic carriers, wear an
alert bracelet
or other identification at all times. This is in case they develop
severe symptoms, or in case of accidents where there is a potential for
drug exposure, and as a result they are unable to explain their
condition to healthcare professionals. Some drugs are absolutely
contraindicated for patients with any form of porphyria.
Neurologic and psychiatric disorders
Patients who experience frequent attacks can develop chronic
neuropathic pain in extremities as well as chronic pain in the
abdomen.
Intestinal pseudo-obstruction,
ileus,
intussusception, hypoganglionosis, and
encopresis
in children have been associated with porphyrias. This is thought to be
due to axonal nerve deterioration in affected areas of the nervous
system and vagal nerve dysfunction. Pain treatment with long-acting
opioids, such as
morphine, is often indicated, and, in cases where seizure or neuropathy is present,
Gabapentin is known to improve outcome.
Seizures often accompany this disease. Most seizure medications exacerbate this condition. Treatment can be problematic:
barbiturates especially must be avoided. Some
benzodiazepines are safe and, when used in conjunction with newer anti-seizure medications such as
gabapentin,
offer a possible regimen for seizure control. Gabapentin has the
additional feature of aiding in the treatment of some kinds of
neuropathic pain.
Magnesium sulfate and bromides have also been used in porphyria seizures; however, development of
status epilepticus in porphyria may not respond to magnesium alone. The addition of
hematin or
heme arginate has been used during
status epilepticus.
Depression often accompanies the disease and is best dealt with by treating the offending symptoms and if needed the judicious use of
antidepressants.
Some psychotropic drugs are porphyrinogenic, limiting the therapeutic
scope. Other psychiatric symptoms such as anxiety, restlessness,
insomnia, depression, mania, hallucinations, delusions, confusion,
catatonia, and psychosis may occur.
Underlying liver disease
Some liver diseases may cause porphyria even in the absence of genetic predisposition. These include
hemochromatosis and
hepatitis C. Treatment of iron overload may be required.
Patients with the acute porphyrias (
AIP,
HCP,
VP) are at increased risk over their life for
hepatocellular carcinoma (primary liver cancer) and may require monitoring. Other typical risk factors for liver cancer need not be present.
Hormone treatment
Hormonal fluctuations that contribute to cyclical attacks in women have been treated with oral contraceptives and
luteinizing hormones
to shut down menstrual cycles. However, oral contraceptives have also
triggered photosensitivity and withdrawal of oral contraceptives has
triggered attacks.
Androgens and fertility hormones have also triggered attacks. In 2019,
givosiran was approved in the United States for the treatment of acute hepatic porphyria.
Erythropoietic porphyria
These are associated with accumulation of porphyrins in erythrocytes and are rare.
The pain, burning, swelling, and itching that occur in
erythropoietic porphyrias generally require avoidance of bright
sunlight. Most kinds of
sunscreen are not effective, but SPF-rated long-sleeve shirts, hats, bandanas, and gloves can help.
Chloroquine may be used to increase porphyrin secretion in some EPs.
Blood transfusion is occasionally used to suppress innate heme production.
The rarest is congenital erythropoietic porphyria (C.E.P.), otherwise known as
Gunther's disease.
The signs may present from birth and include severe photosensitivity,
brown teeth that fluoresce in ultraviolet light due to deposition of
Type 1 porphyrins, and later
hypertrichosis. Hemolytic anemia usually develops. Pharmaceutical-grade
beta carotene may be used in its treatment.
A bone marrow transplant has also been successful in curing CEP in a
few cases, although long-term results are not yet available.
Epidemiology
Rates of all types of porphyria taken together have been estimated to be approximately one in 25,000 in the
United States. The worldwide prevalence has been estimated to be between one in 500 and one in 50,000 people.
Porphyrias have been detected in all races and in multiple ethnic
groups on every continent. There are high incidence reports of AIP in
areas of India and Scandinavia. More than 200 genetic variants of AIP
are known, some of which are specific to families, although some strains
have proven to be repeated mutations.
History
The links between porphyrias and mental illness have been noted
for decades. In the early 1950s, patients with porphyrias (occasionally
referred to as "porphyric hemophilia") and severe symptoms of depression or catatonia were treated with
electroshock therapy.
Vampires and werewolves
Porphyria has been suggested as an explanation for the origin of
vampire and
werewolf legends, based upon certain perceived similarities between the condition and the
folklore.
In January 1964, L. Illis's 1963 paper, "On Porphyria and the
Aetiology of Werewolves," was published in
Proceedings of the Royal Society of Medicine. Later,
Nancy Garden argued for a connection between porphyria and the vampire belief in her 1973 book,
Vampires. In 1985, biochemist
David Dolphin's paper for the
American Association for the Advancement of Science,
"Porphyria, Vampires, and Werewolves: The Aetiology of European
Metamorphosis Legends," gained widespread media coverage, popularizing
the idea.
The theory has been rejected by a few folklorists and researchers
as not accurately describing the characteristics of the original
werewolf and vampire legends or the disease, and as potentially
stigmatizing people with porphyria.
As it was believed that the folkloric vampire could move
about freely in daylight hours, as opposed to the 20th century variant,
congenital erythropoietic porphyria cannot readily explain the folkloric
vampire but may be an explanation of the vampire as we know it in the
20th century. In addition, the folkloric vampire, when unearthed, was
always described as looking quite healthy ("as they were in life"),
while due to disfiguring aspects of the disease, sufferers would not
have passed the exhumation test. Individuals with congenital
erythropoietic porphyria do not crave blood. The enzyme (hematin)
necessary to alleviate symptoms is not absorbed intact on oral
ingestion, and drinking blood would have no beneficial effect on the
sufferer. Finally, and most important, the fact that vampire reports
were literally rampant in the 18th century, and that congenital
erythropoietic porphyria is an extremely rare manifestation of a rare
disease, makes it an unlikely explanation of the folkloric vampire.
Notable cases

- King George III. The mental illness exhibited by George III in the regency crisis of 1788 has inspired several attempts at retrospective diagnosis. The first, written in 1855, thirty-five years after his death, concluded that he had acute mania. M. Guttmacher, in 1941, suggested manic-depressive psychosis
as a more likely diagnosis. The first suggestion that a physical
illness was the cause of King George's mental derangement came in 1966,
in a paper called "The Insanity of King George III: A Classic Case of
Porphyria", with a follow-up in 1968, "Porphyria in the Royal Houses of Stuart, Hanover and Prussia". The papers, by a mother/son psychiatrist
team, were written as though the case for porphyria had been proven,
but the response demonstrated that many experts, including those more
intimately familiar with the manifestations of porphyria, were
unconvinced. Many psychiatrists disagreed with the diagnosis, suggesting
bipolar disorder as far more probable. The theory is treated in Purple Secret,
which documents the ultimately unsuccessful search for genetic evidence
of porphyria in the remains of royals suspected to have had it. In 2005, it was suggested that arsenic (which is known to be porphyrogenic) given to George III with antimony may have caused his porphyria.
This study found high levels of arsenic in King George's hair. In
2010, one analysis of historical records argued that the porphyria claim
was based on spurious and selective interpretation of contemporary
medical and historical sources. The mental illness of George III is the basis of the plot in The Madness of King George, a 1994 British film based upon the 1991 Alan Bennett play, The Madness of George III.
The closing credits of the film include the comment that the King's
symptoms suggest that he had porphyria and notes that the disease is
"periodic, unpredictable, and hereditary".
- Mary, Queen of Scots. It is believed that Mary, Queen of Scots, King George III's ancestor, also had acute intermittent porphyria, although this is subject to much debate. It is assumed she inherited the disorder, if indeed she had it, from her father, James V of Scotland. Both father and daughter endured well-documented attacks that could fall within the constellation of symptoms of porphyria.
- Maria I of Portugal.
Maria I—known as "Maria the Pious" or "Maria the Mad" because of both
her religious fervor and her acute mental illness, which made her
incapable of handling state affairs after 1792 – is also thought to have
had porphyria. Francis Willis,
the same physician who treated George III, was even summoned by the
Portuguese court but returned to England after the court limited the
treatments he could oversee. Contemporary sources, such as Secretary of
State for Foreign Affairs Luís Pinto de Sousa Coutinho, noted that the queen had ever-worsening stomach pains and abdominal spasms: hallmarks of porphyria.
- Vlad III. Vlad III was also said to have had acute porphyria, which may have started the notion that vampires were allergic to sunlight.
- Vincent van Gogh. Other commentators have suggested that Vincent van Gogh may have had acute intermittent porphyria.
- Physician Archie Cochrane. He was born with porphyria, which caused health problems throughout his life.