From Wikipedia, the free encyclopedia

PET/CT-System with 16-slice CT; the ceiling mounted device is an injection pump for CT contrast agent
PET is both a medical and research tool used in pre-clinical and clinical settings. It is used heavily in the imaging of tumors and the search for metastases within the field of clinical oncology,
and for the clinical diagnosis of certain diffuse brain diseases such
as those causing various types of dementias. PET is a valuable research
tool to learn and enhance our knowledge of the normal human brain, heart
function, and support drug development. PET is also used in
pre-clinical studies using animals. It allows repeated investigations
into the same subjects over time, where subjects can act as their own
control and substantially reduces the numbers of animals required for a
given study. This approach allows research studies to reduce the sample
size needed while increasing the statistical quality of its results.
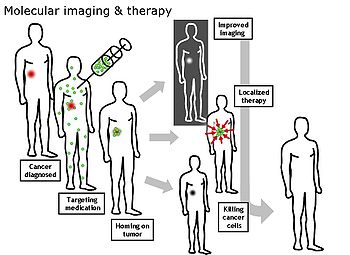
Physiological processes lead to anatomical changes in the body.
Since PET is capable of detecting biochemical processes as well as
expression of some proteins, PET can provide molecular-level information
much before any anatomic changes are visible. PET scanning does this by
using radiolabelled molecular probes that have different rates of
uptake depending on the type and function of tissue involved. Regional
tracer uptake in various anatomic structures can be visualized and
relatively quantified in terms of injected positron emitter within a PET
scan.
PET imaging is best performed using a dedicated PET scanner. It
is also possible to acquire PET images using a conventional dual-head gamma camera
fitted with a coincidence detector. The quality of gamma-camera PET
imaging is lower, and the scans take longer to acquire. However, this
method allows a low-cost on-site solution to institutions with low PET
scanning demand. An alternative would be to refer these patients to
another center or relying on a visit by a mobile scanner.
Alternative methods of medical imaging include single-photon emission computed tomography (SPECT), x-ray computed tomography (CT), magnetic resonance imaging (MRI) and functional magnetic resonance imaging (fMRI), and ultrasound. SPECT is an imaging technique similar to PET that uses radioligands to detect molecules in the body. SPECT is less expensive and provides inferior image quality than PET.
Oncology
Whole-body
PET scan using 18F-FDG. The normal brain and kidneys are labeled, and
radioactive urine from breakdown of the FDG is seen in the bladder. In
addition, a large metastatic tumor mass from colon cancer is seen in the
liver.
PET scanning with the tracer 18F-FDG is widely used in clinical oncology. FDG is a glucose analog that is taken up by glucose-using cells and phosphorylated by hexokinase (whose mitochondrial form is significantly elevated in rapidly growing malignant tumors). Metabolic trapping
of the radioactive glucose molecule allows the PET scan to be utilized.
The concentrations of imaged FDG tracer indicate tissue metabolic
activity as it corresponds to the regional glucose uptake. 18F-FDG is
used to explore the possibility of cancer spreading to other body sites (cancer metastasis).
These 18F-FDG PET scans for detecting cancer metastasis are the most
common in standard medical care (representing 90% of current scans). The
same tracer may also be used for the diagnosis of types of dementia. Less often, other radioactive tracers, usually but not always labelled with fluorine-18, are used to image the tissue concentration of different kinds of molecules of interest inside the body.
A typical dose of FDG used in an oncological scan has an effective radiation dose of 7.6 mSv. Because the hydroxy group that is replaced by fluorine-18 to generate FDG is required for the next step in glucose metabolism
in all cells, no further reactions occur in FDG. Furthermore, most
tissues (with the notable exception of liver and kidneys) cannot remove
the phosphate added by hexokinase. This means that FDG is trapped in any cell that takes it up until it decays, since phosphorylated
sugars, due to their ionic charge, cannot exit from the cell. This
results in intense radiolabeling of tissues with high glucose uptake,
such as the normal brain, liver, kidneys, and most cancers, which have a
higher glucose uptake than most normal tissue due to the Warburg effect. As a result, FDG-PET can be used for diagnosis, staging, and monitoring treatment of cancers, particularly in Hodgkin lymphoma, non-Hodgkin lymphoma, and lung cancer.
A 2020 review of research on the use of PET for Hodgkin lymphoma
found evidence that negative findings in interim PET scans are linked to
higher overall survival and progression-free survival; however, the certainty of the available evidence was moderate for survival, and very low for progression-free survival.
A few other isotopes and radiotracers are slowly being introduced into oncology for specific purposes. For example, 11C-labelled metomidate (11C-metomidate) has been used to detect tumors of adrenocortical origin. Also, FDOPA PET/CT (or F-18-DOPA PET/CT) has proven to be a more sensitive alternative to finding and also localizing pheochromocytoma than the MIBG scan.
Neuroimaging
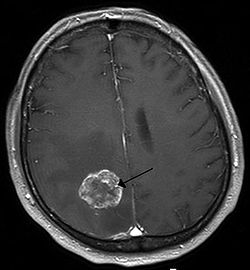
Neurology
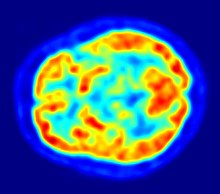
PET scan of the human brain
PET imaging with oxygen-15
indirectly measures blood flow to the brain. In this method, increased
radioactivity signal indicates increased blood flow which is assumed to
correlate with increased brain activity. Because of its 2-minute
half-life, 15O must be piped directly from a medical cyclotron for such uses, which is difficult.
PET imaging with 18F-FDG takes advantage of the fact that the brain is normally a rapid user of glucose. Standard 18F-FDG PET of the brain measures regional glucose use and can be used in neuropathological diagnosis.
Brain pathologies such as Alzheimer's disease greatly decrease brain metabolism of both glucose and oxygen in tandem. Therefore 18F-FDG
PET of the brain may also be used to successfully differentiate
Alzheimer's disease from other dementing processes, and also to make
early diagnoses of Alzheimer's disease. The advantage of 18F-FDG PET for these uses is its much wider availability. Some 18F based radioactive tracers used for Alzheimer's include florbetapir, flutemetamol, PiB and florbetaben, which are all used to detect amyloid-beta plaques (a potential biomarker for Alzheimer's) in the brain.
PET imaging with FDG can also be used for localization of seizure focus. A seizure focus will appear as hypometabolic during an interictal scan. Several radiotracers (i.e. radioligands) have been developed for PET that are ligands for specific neuroreceptor subtypes such as [11C] raclopride, [18F] fallypride and [18F] desmethoxyfallypride for dopamine D2/D3 receptors, [11C] McN 5652 and [11C] DASB for serotonin transporters, [18F] Mefway for serotonin 5HT1A receptors, [18F] Nifene for nicotinic acetylcholine receptors or enzyme substrates (e.g. 6-FDOPA for the AADC enzyme).
These agents permit the visualization of neuroreceptor pools in the
context of a plurality of neuropsychiatric and neurologic illnesses.
PET may also be used for the diagnosis of hippocampal sclerosis, which causes epilepsy. FDG, and the less common tracers flumazenil and MPPF have been explored for this purpose. If the sclerosis is unilateral (right hippocampus or left hippocampus), 18F-FDG uptake can be compared with the healthy side. Even if the diagnosis is difficult with MRI, it may be diagnosed with PET.
The development of a number of novel probes for noninvasive, in
vivo PET imaging of neuroaggregate in human brain has brought amyloid
imaging close to clinical use. The earliest amyloid imaging probes
included 2-(1-{6-[(2-[18F]fluoroethyl)(methyl)amino]-2-naphthyl}ethylidene)malononitrile ([18F]FDDNP) developed at the University of California, Los Angeles and N-methyl-[11C]2-(4'-methylaminophenyl)-6-hydroxybenzothiazole (termed Pittsburgh compound B) developed at the University of Pittsburgh. These amyloid imaging probes permit the visualization of amyloid
plaques in the brains of Alzheimer's patients and could assist
clinicians in making a positive clinical diagnosis of AD pre-mortem and
aid in the development of novel anti-amyloid therapies. [11C]PMP (N-[11C]methylpiperidin-4-yl
propionate) is a novel radiopharmaceutical used in PET imaging to
determine the activity of the acetylcholinergic neurotransmitter system
by acting as a substrate for acetylcholinesterase. Post-mortem
examination of AD patients have shown decreased levels of
acetylcholinesterase. [11C]PMP is used to map the
acetylcholinesterase activity in the brain, which could allow for
pre-mortem diagnoses of AD and help to monitor AD treatments. Avid Radiopharmaceuticals has developed and commercialized a compound called florbetapir that uses the longer-lasting radionuclide fluorine-18 to detect amyloid plaques using PET scans.
Neuropsychology or cognitive neuroscience
To examine links between specific psychological processes or disorders and brain activity.
Psychiatry
Numerous
compounds that bind selectively to neuroreceptors of interest in
biological psychiatry have been radiolabeled with C-11 or F-18. Radioligands that bind to dopamine receptors (D1, D2 receptor, reuptake transporter), serotonin receptors (5HT1A, 5HT2A, reuptake transporter) opioid receptors
(mu and kappa) cholinergic receptors (nicotinic and muscarinic) and
other sites have been used successfully in studies with human subjects.
Studies have been performed examining the state of these receptors in
patients compared to healthy controls in schizophrenia, substance abuse, mood disorders and other psychiatric conditions.
Stereotactic surgery and radiosurgery
PET-image guided surgery facilitates treatment of intracranial tumors, arteriovenous malformations and other surgically treatable conditions.
Cardiology
Cardiology, atherosclerosis and vascular disease study: 18F-FDG PET can help in identifying hibernating myocardium. However, the cost-effectiveness of PET for this role versus SPECT is unclear. 18F-FDG PET imaging of atherosclerosis to detect patients at risk of stroke is also feasible. Also, it can help test the efficacy of novel anti-atherosclerosis therapies.
Infectious diseases
Imaging infections with molecular imaging
technologies can improve diagnosis and treatment follow-up. Clinically,
PET has been widely used to image bacterial infections using fluorodeoxyglucose
(FDG) to identify the infection-associated inflammatory response. Three
different PET contrast agents have been developed to image bacterial
infections in vivo are [18F]maltose, [18F]maltohexaose, and [18F]2-fluorodeoxysorbitol (FDS). FDS has the added benefit of being able to target only Enterobacteriaceae.
Bio-distribution studies
In pre-clinical trials, a new drug can be radiolabeled
and injected into animals. Such scans are referred to as
biodistribution studies. The information regarding drug uptake,
retention and elimination over time can be obtained quickly and
cost-effectively compare to the older technique of killing and
dissecting the animals. Commonly, drug occupancy at a purported site of
action can be inferred indirectly by competition studies between
unlabeled drug and radiolabeled compounds known apriori to bind with
specificity to the site. A single radioligand can be used this way to
test many potential drug candidates for the same target. A related
technique involves scanning with radioligands that compete with an
endogenous (naturally occurring) substance at a given receptor to
demonstrate that a drug causes the release of the natural substance.
Small animal imaging
A miniature animal PET has been constructed that is small enough for a fully conscious rat to be scanned. This RatCAP (Rat Conscious Animal PET) allows animals to be scanned without the confounding effects of anesthesia.
PET scanners designed specifically for imaging rodents, often referred
to as microPET, as well as scanners for small primates, are marketed for
academic and pharmaceutical research. The scanners are based on
microminiature scintillators and amplified avalanche photodiodes (APDs)
through a system that uses single-chip silicon photomultipliers.
In 2018 the UC Davis School of Veterinary Medicine
became the first veterinary center to employ a small clinical
PET-scanner as a pet-PET scan for clinical (rather than research) animal
diagnosis. Because of cost as well as the marginal utility of detecting
cancer metastases in companion animals (the primary use of this
modality), veterinary PET scanning is expected to be rarely available in
the immediate future.
Musculo-skeletal imaging
PET imaging has been used for imaging muscles and bones. 18F-FDG is the most commonly used tracer for imaging muscles, and NaF-F18 is the most widely used tracer for imaging bones.
Muscles
PET is a feasible technique for studying skeletal muscles during exercises like walking. Also, PET can provide muscle activation data about deep-lying muscles (such as the vastus intermedialis and the gluteus minimus) compared to techniques like electromyography,
which can be used only on superficial muscles directly under the skin.
However, a disadvantage is that PET provides no timing information about
muscle activation because it has to be measured after the exercise is
completed. This is due to the time it takes for FDG to accumulate in the
activated muscles.
Bones
Together with NaF-F18, PET for bone imaging
has been in use for 60 years for measuring regional bone metabolism and
blood flow using static and dynamic scans. Researchers have recently
started using NaF-18 to study bone metastasis as well.
Safety
PET scanning is non-invasive, but it does involve exposure to ionizing radiation.
18F-FDG, which is now the standard radiotracer used for PET neuroimaging and cancer patient management, has an effective radiation dose of 14 mSv.
The amount of radiation in 18F-FDG is similar to the effective dose of spending one year in the American city of Denver, Colorado (12.4 mSv/year).
For comparison, radiation dosage for other medical procedures range
from 0.02 mSv for a chest x-ray and 6.5–8 mSv for a CT scan of the
chest. Average civil aircrews are exposed to 3 mSv/year, and the whole body occupational dose limit for nuclear energy workers in the USA is 50mSv/year. For scale, see Orders of magnitude (radiation).
For PET-CT scanning, the radiation exposure may be substantial—around 23–26 mSv (for a 70 kg person—dose is likely to be higher for higher body weights).
Operation
Radionuclides and radiotracers
Schematic view of a detector block and ring of a PET scanner
Radionuclides are incorporated either into compounds normally used by the body such as glucose (or glucose analogues), water, or ammonia, or into molecules that bind to receptors or other sites of drug action. Such labelled compounds are known as radiotracers.
PET technology can be used to trace the biologic pathway of any
compound in living humans (and many other species as well), provided it
can be radiolabeled with a PET isotope. Thus, the specific processes
that can be probed with PET are virtually limitless, and radiotracers
for new target molecules and processes are continuing to be synthesized;
as of this writing there are already dozens in clinical use and
hundreds applied in research. In 2020 by far the most commonly used
radiotracer in clinical PET scanning is the carbohydrate derivative fludeoxyglucose (18F)
(18F-FDG). This radiotracer is used in essentially all scans for
oncology and most scans in neurology, and thus makes up the large
majority of radiotracer (>95%) used in PET and PET-CT scanning.
Due to the short half-lives of most positron-emitting radioisotopes, the radiotracers have traditionally been produced using a cyclotron
in close proximity to the PET imaging facility. The half-life of
fluorine-18 is long enough that radiotracers labeled with fluorine-18
can be manufactured commercially at offsite locations and shipped to
imaging centers. Recently rubidium-82 generators have become commercially available. These contain strontium-82, which decays by electron capture to produce positron-emitting rubidium-82.
The use of positron-emitting isotopes of metals in PET scans has
been reviewed, including elements not listed above, such as lanthanides.
Immuno-PET
The isotope 89Zr
has been applied to the tracking and quantification of molecular
antibodies with positron emission tomography (PET) cameras (a method
called "immuno-PET").
The biological half-life of antibodies is typically on the order of days, see daclizumab and erenumab by way of example. To visualize and quantify the distribution of such antibodies in the body, the PET isotope 89Zr is well suited because its physical half-life matches the typical biological half-life of antibodies, see table above.
Emission
Schema of a PET acquisition process
To conduct the scan, a short-lived radioactive tracer isotope
is injected into the living subject (usually into blood circulation).
Each tracer atom has been chemically incorporated into a biologically
active molecule. There is a waiting period while the active molecule
becomes concentrated in tissues of interest; then the subject is placed
in the imaging scanner. The molecule most commonly used for this purpose
is F-18 labeled fluorodeoxyglucose
(FDG), a sugar, for which the waiting period is typically an hour.
During the scan, a record of tissue concentration is made as the tracer
decays.
As the radioisotope undergoes positron emission decay (also known as positive beta decay), it emits a positron, an antiparticle of the electron
with opposite charge. The emitted positron travels in tissue for a
short distance (typically less than 1 mm, but dependent on the isotope), during which time it loses kinetic energy, until it decelerates to a point where it can interact with an electron. The encounter annihilates both electron and positron, producing a pair of annihilation (gamma) photons moving in approximately opposite directions. These are detected when they reach a scintillator in the scanning device, creating a burst of light which is detected by photomultiplier tubes or silicon avalanche photodiodes
(Si APD). The technique depends on simultaneous or coincident detection
of the pair of photons moving in approximately opposite directions
(they would be exactly opposite in their center of mass frame,
but the scanner has no way to know this, and so has a built-in slight
direction-error tolerance). Photons that do not arrive in temporal
"pairs" (i.e. within a timing-window of a few nanoseconds) are ignored.
Localization of the positron annihilation event
The
most significant fraction of electron–positron annihilations results in
two 511 keV gamma photons being emitted at almost 180 degrees to each
other; hence, it is possible to localize their source along a straight
line of coincidence (also called the line of response, or LOR).
In practice, the LOR has a non-zero width as the emitted photons are
not exactly 180 degrees apart. If the resolving time of the detectors is
less than 500 picoseconds rather than about 10 nanoseconds, it is possible to localize the event to a segment of a chord, whose length is determined by the detector timing resolution. As the timing resolution improves, the signal-to-noise ratio
(SNR) of the image will improve, requiring fewer events to achieve the
same image quality. This technology is not yet common, but it is
available on some new systems.
Image reconstruction
The
raw data collected by a PET scanner are a list of 'coincidence events'
representing near-simultaneous detection (typically, within a window of 6
to 12 nanoseconds of each other) of annihilation photons by a pair of
detectors. Each coincidence event represents a line in space connecting
the two detectors along which the positron emission occurred (i.e., the
line of response (LOR)).
Analytical techniques, much like the reconstruction of computed tomography (CT) and single-photon emission computed tomography (SPECT) data, are commonly used, although the data set
collected in PET is much poorer than CT, so reconstruction techniques
are more difficult. Coincidence events can be grouped into projection
images, called sinograms.
The sinograms are sorted by the angle of each view and tilt (for 3D
images). The sinogram images are analogous to the projections captured
by computed tomography
(CT) scanners, and can be reconstructed in a similar way. The
statistics of data thereby obtained are much worse than those obtained
through transmission tomography. A normal PET data set has millions of
counts for the whole acquisition, while the CT can reach a few billion
counts. This contributes to PET images appearing "noisier" than CT. Two
major sources of noise in PET are scatter (a detected pair of photons,
at least one of which was deflected from its original path by
interaction with matter in the field of view, leading to the pair being
assigned to an incorrect LOR) and random events (photons originating
from two different annihilation events but incorrectly recorded as a
coincidence pair because their arrival at their respective detectors
occurred within a coincidence timing window).
In practice, considerable pre-processing of the data is
required—correction for random coincidences, estimation and subtraction
of scattered photons, detector dead-time
correction (after the detection of a photon, the detector must "cool
down" again) and detector-sensitivity correction (for both inherent
detector sensitivity and changes in sensitivity due to angle of
incidence).
Filtered back projection
(FBP) has been frequently used to reconstruct images from the
projections. This algorithm has the advantage of being simple while
having a low requirement for computing resources. Disadvantages are that
shot noise
in the raw data is prominent in the reconstructed images, and areas of
high tracer uptake tend to form streaks across the image. Also, FBP
treats the data deterministically—it does not account for the inherent
randomness associated with PET data, thus requiring all the
pre-reconstruction corrections described above.
Statistical, likelihood-based approaches:
Statistical, likelihood-based iterative expectation-maximization algorithms such as the Shepp-Vardi algorithm
are now the preferred method of reconstruction. These algorithms compute
an estimate of the likely distribution of annihilation events that led
to the measured data, based on statistical principles. The advantage is a
better noise profile and resistance to the streak artifacts common with
FBP, but the disadvantage is higher computer resource requirements. A
further advantage of statistical image reconstruction techniques is that
the physical effects that would need to be pre-corrected for when using
an analytical reconstruction algorithm, such as scattered photons,
random coincidences, attenuation and detector dead-time, can be
incorporated into the likelihood model being used in the reconstruction,
allowing for additional noise reduction. Iterative reconstruction has
also been shown to result in improvements in the resolution of the
reconstructed images, since more sophisticated models of the scanner
physics can be incorporated into the likelihood model than those used by
analytical reconstruction methods, allowing for improved quantification
of the radioactivity distribution.
Research has shown that Bayesian methods that involve a Poisson likelihood function and an appropriate prior probability (e.g., a smoothing prior leading to total variation regularization or a Laplacian distribution leading to  -based regularization in a wavelet or other domain), such as via Ulf Grenander's Sieve estimator
or via Bayes penalty methods
or via I.J. Good's roughness method
may yield superior performance to expectation-maximization-based
methods which involve a Poisson likelihood function but do not involve
such a prior.
-based regularization in a wavelet or other domain), such as via Ulf Grenander's Sieve estimator
or via Bayes penalty methods
or via I.J. Good's roughness method
may yield superior performance to expectation-maximization-based
methods which involve a Poisson likelihood function but do not involve
such a prior.
Attenuation correction: Quantitative PET Imaging requires attenuation correction. In these systems attenuation correction is based on a transmission scan using 68Ge rotating rod source.
Transmission scans directly measure attenuation values at 511keV. Attenuation occurs when photons
emitted by the radiotracer inside the body are absorbed by intervening
tissue between the detector and the emission of the photon. As different
LORs must traverse different thicknesses of tissue, the photons are
attenuated differentially. The result is that structures deep in the
body are reconstructed as having falsely low tracer uptake. Contemporary
scanners can estimate attenuation using integrated x-ray CT equipment, in place of earlier equipment that offered a crude form of CT using a gamma ray (positron emitting) source and the PET detectors.
While attenuation-corrected images are generally more faithful
representations, the correction process is itself susceptible to
significant artifacts. As a result, both corrected and uncorrected
images are always reconstructed and read together.
2D/3D reconstruction: Early PET scanners had only a single
ring of detectors, hence the acquisition of data and subsequent
reconstruction was restricted to a single transverse plane. More modern
scanners now include multiple rings, essentially forming a cylinder of
detectors.
There are two approaches to reconstructing data from such a
scanner: 1) treat each ring as a separate entity, so that only
coincidences within a ring are detected, the image from each ring can
then be reconstructed individually (2D reconstruction), or 2) allow
coincidences to be detected between rings as well as within rings, then
reconstruct the entire volume together (3D).
3D techniques have better sensitivity (because more coincidences
are detected and used) and therefore less noise, but are more sensitive
to the effects of scatter and random coincidences, as well as requiring
correspondingly greater computer resources. The advent of sub-nanosecond
timing resolution detectors affords better random coincidence
rejection, thus favoring 3D image reconstruction.
Time-of-flight (TOF) PET: For modern systems with a higher
time resolution (roughly 3 nanoseconds) a technique called
"Time-of-flight" is used to improve the overall performance.
Time-of-flight PET makes use of very fast gamma-ray detectors and data
processing system which can more precisely decide the difference in time
between the detection of the two photons. Although it is technically
impossible to localize the point of origin of the annihilation event
exactly (currently within 10 cm) thus image reconstruction is still
needed, TOF technique gives a remarkable improvement in image quality,
especially signal-to-noise ratio.
Combination of PET with CT or MRI
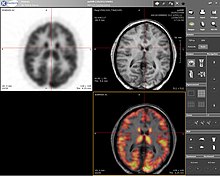
Complete body PET-CT fusion image
Brain PET-MRI fusion image
PET scans are increasingly read alongside CT or magnetic resonance imaging (MRI) scans, with the combination (called "co-registration")
giving both anatomic and metabolic information (i.e., what the
structure is, and what it is doing biochemically). Because PET imaging
is most useful in combination with anatomical imaging, such as CT,
modern PET scanners are now available with integrated high-end
multi-detector-row CT scanners (so-called "PET-CT"). Because the two
scans can be performed in immediate sequence during the same session,
with the patient not changing position between the two types of scans,
the two sets of images are more precisely registered,
so that areas of abnormality on the PET imaging can be more perfectly
correlated with anatomy on the CT images. This is very useful in showing
detailed views of moving organs or structures with higher anatomical
variation, which is more common outside the brain.
At the Jülich Institute of Neurosciences and Biophysics, the world's largest PET-MRI device began operation in April 2009: a 9.4-tesla
magnetic resonance tomograph (MRT) combined with a positron emission
tomograph (PET). Presently, only the head and brain can be imaged at
these high magnetic field strengths.
For brain imaging, registration of CT, MRI and PET scans may be
accomplished without the need for an integrated PET-CT or PET-MRI
scanner by using a device known as the N-localizer.
Limitations
The
minimization of radiation dose to the subject is an attractive feature
of the use of short-lived radionuclides. Besides its established role as
a diagnostic technique, PET has an expanding role as a method to assess
the response to therapy, in particular, cancer therapy,
where the risk to the patient from lack of knowledge about disease
progress is much greater than the risk from the test radiation. Since
the tracers are radioactive, the elderly and pregnant are unable to use it due to risks posed by radiation.
Limitations to the widespread use of PET arise from the high costs of cyclotrons needed to produce the short-lived radionuclides
for PET scanning and the need for specially adapted on-site chemical
synthesis apparatus to produce the radiopharmaceuticals after
radioisotope preparation. Organic radiotracer molecules that will
contain a positron-emitting radioisotope cannot be synthesized first and
then the radioisotope prepared within them, because bombardment with a
cyclotron to prepare the radioisotope destroys any organic carrier for
it. Instead, the isotope must be prepared first, then afterward, the
chemistry to prepare any organic radiotracer (such as FDG)
accomplished very quickly, in the short time before the isotope decays.
Few hospitals and universities are capable of maintaining such systems,
and most clinical PET is supported by third-party suppliers of
radiotracers that can supply many sites simultaneously. This limitation
restricts clinical PET primarily to the use of tracers labelled with
fluorine-18, which has a half-life of 110 minutes and can be transported
a reasonable distance before use, or to rubidium-82 (used as rubidium-82 chloride) with a half-life of 1.27 minutes, which is created in a portable generator and is used for myocardial perfusion
studies. Nevertheless, in recent years a few on-site cyclotrons with
integrated shielding and "hot labs" (automated chemistry labs that are
able to work with radioisotopes) have begun to accompany PET units to
remote hospitals. The presence of the small on-site cyclotron promises
to expand in the future as the cyclotrons shrink in response to the high
cost of isotope transportation to remote PET machines.
In recent years the shortage of PET scans has been alleviated in the
US, as rollout of radiopharmacies to supply radioisotopes has grown
30%/year.
Because the half-life of fluorine-18 is about two hours, the
prepared dose of a radiopharmaceutical bearing this radionuclide will
undergo multiple half-lives of decay during the working day. This
necessitates frequent recalibration of the remaining dose (determination
of activity per unit volume) and careful planning with respect to
patient scheduling.
History
The concept of emission and transmission tomography was introduced by David E. Kuhl,
Luke Chapman and Roy Edwards in the late 1950s. Their work later led to
the design and construction of several tomographic instruments at the University of Pennsylvania. In 1975 tomographic imaging techniques were further developed by Michel Ter-Pogossian, Michael E. Phelps, Edward J. Hoffman and others at Washington University School of Medicine.
Work by Gordon Brownell, Charles Burnham and their associates at the Massachusetts General Hospital
beginning in the 1950s contributed significantly to the development of
PET technology and included the first demonstration of annihilation
radiation for medical imaging.
Their innovations, including the use of light pipes and volumetric
analysis, have been important in the deployment of PET imaging. In 1961,
James Robertson and his associates at Brookhaven National Laboratory
built the first single-plane PET scan, nicknamed the "head-shrinker."
One of the factors most responsible for the acceptance of
positron imaging was the development of radiopharmaceuticals. In
particular, the development of labeled 2-fluorodeoxy-D-glucose (2FDG) by
the Brookhaven group under the direction of Al Wolf and Joanna Fowler
was a major factor in expanding the scope of PET imaging. The compound was first administered to two normal human volunteers by Abass Alavi
in August 1976 at the University of Pennsylvania. Brain images obtained
with an ordinary (non-PET) nuclear scanner demonstrated the
concentration of FDG in that organ. Later, the substance was used in
dedicated positron tomographic scanners, to yield the modern procedure.
The logical extension of positron instrumentation was a design
using two 2-dimensional arrays. PC-I was the first instrument using this
concept and was designed in 1968, completed in 1969 and reported in
1972. The first applications of PC-I in tomographic mode as
distinguished from the computed tomographic mode were reported in 1970.
It soon became clear to many of those involved in PET development that a
circular or cylindrical array of detectors was the logical next step in
PET instrumentation. Although many investigators took this approach,
James Robertson and Zang-Hee Cho were the first to propose a ring system that has become the prototype of the current shape of PET.
The PET-CT scanner, attributed to David Townsend and Ronald Nutt, was named by Time as the medical invention of the year in 2000.
Cost
As of August 2008, Cancer Care Ontario
reports that the current average incremental cost to perform a PET scan
in the province is Can$1,000–1,200 per scan. This includes the cost of
the radiopharmaceutical and a stipend for the physician reading the
scan.
In the United States,
a PET scan is estimated to be ~$5,000, and most insurance companies
don't pay for routine PET scans after cancer treatment due to the fact
that these scans are often unnecessary and present potentially more
risks than benefits.
In England, the National Health Service reference cost (2015–2016) for an adult outpatient PET scan is £798.
In Australia, as of July 2018, the Medicare Benefits Schedule Fee for whole body FDG PET ranges from A$953 to A$999, depending on the indication for the scan.
Quality control
The overall performance of PET systems can be evaluated by quality control tools such as the Jaszczak phantom.