| Thrombus | |
|---|---|
| Other names | Blood clot |
 | |
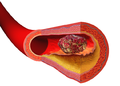
| Diagram of a thrombus (blood clot) that has blocked a blood vessel valve | |
| Specialty | Vascular surgery |
A thrombus, colloquially called a blood clot, is the final product of the blood coagulation step in hemostasis. There are two components to a thrombus: aggregated platelets and red blood cells that form a plug, and a mesh of cross-linked fibrin protein. The substance making up a thrombus is sometimes called cruor. A thrombus is a healthy response to injury intended to prevent bleeding, but can be harmful in thrombosis, when clots obstruct blood flow through healthy blood vessels.
Mural thrombi are thrombi that adhere to the wall of a blood vessel. They occur in large vessels such as the heart and aorta, and can restrict blood flow but usually do not block it entirely. They appear grey-red with alternating light and dark lines (known as lines of Zahn) which represent bands of entrapped white blood cells and red blood cells (darker).
Cause
Virchow's triad describes the pathogenesis of thrombus formation:
- Endothelial injury: Injury to the endothelium (interior surface of blood vessel), causing platelet activation and aggregation
- Common causes include: trauma, smoking, hypertension, atheroma
- Stasis: Blood stasis promotes greater contact between platelets/coagulative factors with vascular endothelium.
- Common causes of stasis include anything that leads to prolonged immobility and reduced blood flow such as: trauma/broken bones and extended air travel
- Hypercoagulability (also called thrombophilia; any disorder of the blood that predisposes to thrombosis)
Disseminated intravascular coagulation
(DIC) involves widespread microthrombi formation throughout the
majority of the blood vessels. This is due to excessive consumption of
coagulation factors and subsequent activation of fibrinolysis using all of the body's available platelets and clotting factors. The end result is hemorrhaging and ischaemic necrosis of tissue/organs. Causes are septicaemia, acute leukaemia, shock, snake bites, fat emboli from broken bones, or other severe traumas. DIC may also be seen in pregnant females. Treatment involves the use of fresh frozen plasma to restore the level of clotting factors in the blood, as well as platelets and heparin to prevent further thrombi formation.
Classification
Thrombi are classified in three major groups depending on the relative amount of platelets and red blood cells (RBCs).
The three major groups are:
- White thrombi (characterized by predominance of platelets)
- Red thrombi (characterized by predominance of red blood cells)
- Mixed thrombi (with features of both white and red thrombi - an intermediate).
Pathophysiology
Animation
of the formation of an occlusive thrombus in a vein. A few platelets
attach themselves to the valve lips, constricting the opening and
causing more platelets and red blood cells to aggregate and coagulate.
Coagulation of unmoving blood on both sides of the blockage may
propagate a clot in both directions.
A thrombus occurs when the hemostatic process, which normally occurs
in response to injury, becomes activated in an uninjured or slightly
injured vessel. A thrombus in a large blood vessel will decrease blood
flow through that vessel (termed a mural thrombus). In a small blood
vessel, blood flow may be completely cut off (termed an occlusive
thrombus), resulting in death of tissue supplied by that vessel. If a
thrombus dislodges and becomes free-floating, it is considered an embolus.
Some of the conditions which increase the risk of blood clots developing include atrial fibrillation (a form of cardiac arrhythmia), heart valve replacement, a recent heart attack (also known as a myocardial infarction), extended periods of inactivity, and genetic or disease-related deficiencies in the blood's clotting abilities.
Formation
Platelet activation occurs through injuries that damage the endothelium of the blood vessels, exposing the enzyme called factor VII, a protein normally circulating within the vessels, to the tissue factor, which is a protein encoded by the F3 gene.
The platelet activation can potentially cause a cascade, eventually leading to the formation of the thrombus. This process is regulated through thromboregulation.
- Micrograph showing a thrombus (center of image) within a blood vessel of the placenta. H&E stain.
Prevention and treatment
Blood clot prevention and treatment reduce the risk of stroke, heart attack and pulmonary embolism. Heparin and warfarin
are used to inhibit the formation and growth of existing thrombi, with
the former used for acute anticoagulation while the latter is used for
long-term anticoagulation. The mechanism of action of heparin and warfarin are different as they work on different pathways of the coagulation cascade. Heparin works by binding to and activating the enzyme inhibitor antithrombin III, an enzyme that acts by inactivating thrombin and factor Xa. In contrast, warfarin works by inhibiting vitamin K epoxide reductase, an enzyme needed to synthesize vitamin K dependent clotting factors II, VII, IX, and X.
Bleeding time with heparin and warfarin therapy can be measured with
the partial thromboplastin time (PTT) and prothrombin time (PT),
respectively.
Some treatments have been derived from bacteria. One drug is streptokinase, which is an enzyme secreted by several streptococcal bacteria. This drug is administered intravenously and can be used to dissolve blood clots in coronary vessels.
However, streptokinase is nonspecific and can digest almost any
protein, which can lead to many secondary problems. Another
clot-dissolving enzyme that works faster and is more specific is tissue plasminogen activator (tPA). This drug is made by transgenic bacteria and it converts plasminogen into the clot-dissolving enzyme, plasmin. There are also some anticoagulants that come from animals that work by dissolving fibrin. For example, Haementeria ghilianii, an Amazon leech, produces an enzyme called hementin from its salivary glands. As of 2012, this enzyme has been successfully produced by genetically engineered bacteria and is administered to cardiac patients.
More recent research indicates that tPA could have toxic effects
in the central nervous system. In cases of severe stroke, tPA can cross
the blood-brain barrier
and enter interstitial fluid, where it then increases excitotoxicity,
potentially affecting permeability of the blood-brain barrier, and may even cause cerebral hemorrhaging.
Prognosis
Thrombus formation can have one of four outcomes: propagation, embolization, dissolution, and organization and recanalization.
- Propagation of a thrombus occurs towards the direction of the heart and involves the accumulation of additional platelets and fibrin. This means that it is anterograde in veins or retrograde in arteries.
- Embolization occurs when the thrombus breaks free from the vascular wall and becomes mobile, thereby traveling to other sites in the vasculature. A venous embolus (mostly from deep vein thrombosis in the lower limbs) will travel through the systemic circulation, reach the right side of the heart, and travel through the pulmonary artery, resulting in a pulmonary embolism. Arterial thrombosis resulting from hypertension or atherosclerosis can become mobile and the resulting emboli can occlude any artery or arteriole downstream of the thrombus formation. This means that cerebral stroke, myocardial infarction, or any other organ can be affected.
- Dissolution occurs when the fibrinolytic mechanisms break up the thrombus and blood flow is restored to the vessel. This may be aided by fibrinolytic drugs such as Tissue Plasminogen Activator (tPA) in instances of coronary artery occlusion. The best response to fibrinolytic drugs is within a couple of hours, before the fibrin meshwork of the thrombus has been fully developed.
- Organization and recanalization involves the ingrowth of smooth muscle cells, fibroblasts and endothelium into the fibrin-rich thrombus. If recanalization proceeds it provides capillary-sized channels through the thrombus for continuity of blood flow through the entire thrombus but may not restore sufficient blood flow for the metabolic needs of the downstream tissue.