Public health education with regard to prevention of HIV/AIDS in an educational outreach session in Angola.
Within the framework of the World Health Organization's (WHO) definition of health as a state of complete physical, mental and social well-being, and not merely the absence of disease or infirmity, reproductive health, or sexual health/hygiene, addresses the reproductive processes, functions and system at all stages of life. UN agencies claim sexual and reproductive health includes physical, as well as psychological well-being vis-a-vis sexuality.
Reproductive health implies that people are able to have a responsible, satisfying and safer sex life and that they have the capability to reproduce and the freedom to decide if, when and how often to do so. One interpretation of this implies that men and women ought to be informed of and to have access to safe, effective, affordable and acceptable methods of birth control; also access to appropriate health care services of sexual, reproductive medicine and implementation of health education programs to stress the importance of women to go safely through pregnancy and childbirth could provide couples with the best chance of having a healthy infant.
Individuals do face inequalities in reproductive health services.
Inequalities vary based on socioeconomic status, education level, age,
ethnicity, religion, and resources available in their environment. It is
possible for example, that low income individuals lack the resources
for appropriate health services and the knowledge to know what is
appropriate for maintaining reproductive health.
Reproductive health
The
WHO assessed in 2008 that "Reproductive and sexual ill-health accounts
for 20% of the global burden of ill-health for women, and 14% for men." Reproductive health is a part of sexual and reproductive health and rights. According to the United Nations Population Fund
(UNFPA), unmet needs for sexual and reproductive health deprive women
of the right to make "crucial choices about their own bodies and
futures", affecting family welfare. Women bear and usually nurture
children, so their reproductive health is inseparable from gender
equality. Denial of such rights also worsens poverty.
Adolescent health
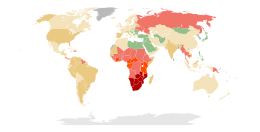
Teenage birth rate per 1,000 females aged 15–19, 2000–2009
Adolescent health
creates a major global burden and has a great deal of additional and
diverse complications compared to adult reproductive health such as
early pregnancy and parenting issues, difficulties accessing
contraception and safe abortions, lack of healthcare access, and high
rates of HIV and sexually transmitted infections, and mental health
issues. Each of those can be affected by outside political, economic and
socio-cultural influences.
For most adolescent females, they have yet to complete their body
growth trajectories, therefore adding a pregnancy exposes them to a
predisposition to complications. These complications range from anemia,
malaria, HIV and other STI's, postpartum bleeding and other postpartum
complications, mental health disorders such as depression and suicidal
thoughts or attempts. In 2016, adolescent birth rates between the ages of 15-19 was 45 per 1000. In 2014, 1 in 3 experienced sexual violence,
and there more than 1.2 million deaths. The top three leading causes of
death in females between the ages of 15-19 are maternal conditions
10.1%, self-harm 9.6%, and road conditions 6.1%.
The causes for teenage pregnancy are vast and diverse. In
developing countries, young women are pressured to marry for different
reasons. One reason is to bear children to help with work, another on a dowry system
to increase the families income, another is due to prearranged
marriages. These reasons tie back to financial needs of girls' family,
cultural norms, religious beliefs and external conflicts.
Adolescent pregnancy, especially in developing countries, carries increased health risks, and contributes to maintaining the cycle of poverty. The availability and type of sex education
for teenagers varies in different parts of the world. LGBT teens may
suffer additional problems if they live in places where homosexual
activity is socially disapproved and/or illegal; in extreme cases there
can be depression, social isolation and even suicide among LGBT youth.
Maternal health
Maternal Mortality Rate
worldwide, as defined by the number of maternal deaths per 100,000 live
births from any cause related to or aggravated by pregnancy or its
management, excluding accidental or incidental causes.
Ninety nine percent of maternal deaths occur in developing countries
and in 25 years, maternal mortality globally dropped to 44%.
Statistically, a woman's chance of survival during childbirth is
closely tied to her social economic status, access to healthcare, where
she lives geographically, and cultural norms.
To compare, a woman dies of complications from childbirth every minute
in developing countries versus a total of 1% of total maternal mortality
deaths in developed countries. Women in developing countries have
little access to family planning services, different cultural practices,
have lack of information, birthing attendants, prenatal care, birth
control, postnatal care, lack of access to health care and are typically
in poverty. In 2015, those in low-income countries had access to
antenatal care visits averaged to 40% and were preventable. All these reasons lead to an increase in the Maternal Mortality Ratio (MMR).
One of the international Sustainable Development Goals developed by United Nations is to improve maternal health by a targeted 70 deaths per 100,000 live births by 2030.
Most models of maternal health encompass family planning,
preconception, prenatal, and postnatal care. All care after childbirth
recovery is typically excluded, which includes pre-menopause and aging into old age.[16]
During childbirth, women typically die from severe bleeding,
infections, high blood pressure during pregnancy, delivery
complications, or an unsafe abortion. Other reasons can be regional such
as complications related to diseases such as malaria and AIDS during
pregnancy. The younger the women is when she gives birth, the more at
risk her and her baby is for complications and possibly mortality.
Map of countries and territories by fertility rate as of 2018
There is a significant relationship between the quality of maternal services made
available and the greater financial standings of a country. Sub-Saharan Africa and South Asia
exemplify this as these regions are significantly deprived of medical staff and affordable health
opportunities. Most countries provide for their health services through a combination of
funding from government tax revenue and local households. Poorer nations or regions with
extremely concentrated wealth can leave citizens on the margins uncared for or overlooked.
However, the lack of proper leadership can result in a nation's public sectors being
mishandled or poorly performing despite said nation's resources and standing. In addition,
poorer nations funding their medical services through taxes places a greater financial burden on
the public and effectively the mothers themselves.
Responsibility and accountability on the part of mental health sectors are strongly
emphasized as to what will remedy the poor quality of maternal health globally. The impact
of different maternal health interventions across the globe stagger variously and are vastly
uneven. This is the result of a lack of political and financial commitment to the issue as most
safe motherhood programs internationally have to compete for significant funding. Some
resolve that if global survival initiatives were promoted and properly funded it would prove to be
mutually beneficial for the international community. Investing in maternal health would
ultimately advance several issues such as: gender inequality, poverty and general global health
standards. As it currently stands, pregnant women are subjugated to high financial costs
throughout the duration of their term internationally that are highly taxing and strenuous.
Contraception
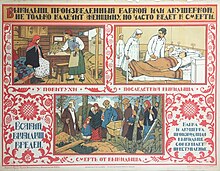
A page from De Morbo Gallico (On the French Disease), Gabriele Falloppio's treatise on syphilis. Published in 1564, it describes an early use of condoms.
Margaret Sanger, birth control advocate, and her sister Ethyl Byrne, on the courthouse steps in Brooklyn, New York City,
January 8, 1917, during their trial for opening a birth control clinic.
Contraception has been and still remains in some cultures a
controversial issue.
Access to reproductive health services is very poor in many countries. Women are often unable to access maternal health services due to lack of knowledge about the existence of such services or lack of freedom of movement. Some women are subjected to forced pregnancy
and banned from leaving the home. In many countries, women are not
allowed to leave home without a male relative or husband, and therefore
their ability to access medical services is limited. Therefore,
increasing women's autonomy is needed in order to improve reproductive
health, however doing may require a cultural shift. According to the
WHO, "All women need access to antenatal care in pregnancy, skilled care
during childbirth, and care and support in the weeks after childbirth".
The fact that the law allows certain reproductive health services, it does not necessary ensure that such services are de facto
available to people. The availability of contraception, sterilization
and abortion is dependent on laws, as well as social, cultural and
religious norms. Some countries have liberal laws regarding these
issues, but in practice it is very difficult to access such services due
to doctors, pharmacists and other social and medical workers being conscientious objectors.
In developing regions of the world, there are about 214 million
women who want to avoid pregnancy but are unable to use safe and
effective family planning methods. When taken correctly, the combined oral contraceptive pill is over 99% effective at preventing pregnancy. However, it does not protect from sexually transmitted infections (STIs). Some methods, such as using condoms, achieve both protection from STIs and unwanted pregnancies. There are also natural family planning methods, which may be preferred by religious people, but some very conservative religious groups, such as the Quiverfull movement, oppose these methods too, because they advocate the maximization of procreation. One of the oldest ways to reduce unwanted pregnancy is coitus interruptus - still widely used in the developing world.
There are many types of contraceptives. One type of contraceptive includes barrier methods. One barrier method includes condoms for males and females. Both types stop sperm from entering the woman's uterus, thereby preventing pregnancy from occurring.
Another type of contraception is the birth control pill, which stops
ovulation from occurring by combining the chemicals progestin and
estrogen. Many women use this method of contraception, however they discontinue using it equally as much as they use it.
One reason for this is because of the side effects that may occur from
using the pill, and because some health care providers do not take
women's concerns about negative side effects seriously. The use of the birth control pill is common in western countries, and
two forms of combined oral contraceptives are on the World Health Organization's List of Essential Medicines, the most important medications needed in a basic health system.
There are many objections to the use of birth control, both
historically and in the present day. One argument against birth control
usage states that there is no need for birth control to begin with.
This argument was levied in 1968 when Richard Nixon was elected
president, and the argument stated that since birth rates were at their
lowest point since World War II ended, birth control was not necessary. Demographic planning arguments were also the basis of the population policy of Nicolae Ceaușescu in communist Romania, who adopted a very aggressive natalist policy which included outlawing abortion and contraception, routine pregnancy tests for women, taxes on childlessness,
and legal discrimination against childless people. Such policies
consider that coercion is an acceptable means of reaching demographic
targets. Religious objections are based on the view that premarital sex
should not happen, while married couples should have as many children
as possible. As such, the Catholic Church encourages premarital
abstinence from sex. This argument was written out in Humanae Vitae, a papal encyclical released in 1968.
The Catholic Church bases its argument against birth control pills on
the basis that birth control pills undermine the natural law of God.
The Catholic Church also argues against birth control on the basis of
family size, with Cardinal Mercier of Belgium arguing, "...the duties
of conscience are above worldly considerations, and besides, it is the
large families who are the best" (Reiterman, 216).
Another argument states that women should use natural methods of
contraception in place of artificial ones, such as having sexual
intercourse when one is infertile.
Support for contraception is based on views such as reproductive rights, women's rights, and the necessity to prevent child abandonment and child poverty.
The World Health Organization states that "By preventing unintended
pregnancy, family planning /contraception prevents deaths of mothers and
children".
Sexually transmitted infection
Estimated prevalence in % of HIV among young adults (15–49) per country as of 2011.
|
No data
<0 .10="" small="">
0.10–0.5
0.5–1
|
1–5
5–15
15–50
|
Deaths from syphilis in 2012 per million persons
Disability-adjusted life year for gonorrhea per 100, 000 inhabitants.
Condoms offer effective protection from STIs
A Sexually transmitted infection (STI) --previously known as a sexually transmitted disease (STD) or venereal disease (VD)-- is an infection that has a significant likelihood of transmission between humans by means of sexual activity. The CDC analyses the eight most common STI's: chlamydia, gonorrhea, hepatitis B virus (HBV), herpes simplex virus type 2 (HSV-2), human immunodeficiency virus (HIV), human papillomavirus (HPV), syphilis, and trichomoniasis.
There are more than 600 million cases of STI's worldwide and more than 20 million new cases within the United States. Numbers of such high magnitude weigh a heavy burden on the local and global economy. A study conducted at Oxford University in 2015 concluded that despite giving participants early antiviral medications (ART),
they still cost an estimated $256 billion over 2 decades. HIV testing
done at modest rates could reduce HIV infections by 21%, HIV retention
by 54% and HIV mortality rates by 64%, with a cost-effectiveness ration
of $45,300 per Quality-adjusted life year.
However, the study concluded that the United States has led to an
excess in infections, treatment costs, and deaths, even when
interventions do not improve over all survival rates.
There is a profound reduction on STI rates once those who are
sexually active are educated about transmissions, condom promotion,
interventions targeted at key and vulnerable populations through a
comprehensive Sex education courses or programs.
South Africa's policy addresses the needs of women at risk for HIV and
who are HIV positive as well as their partners and children. The policy
also promotes screening activities related to sexual health such as HIV
counseling and testing as well as testing for other STIs, tuberculosis,
cervical cancer, and breast cancer.
Young African American women are at a higher risk for STI's, including HIV.
A recent study published outside of Atlanta, Georgia collected data
(demographic, psychological, and behavioral measures) with a vaginal
swab to confirm the presence of STIs. They found a profound difference
that those women who had graduated from college were far less likely to
have STIs, potentially be benefiting from a reduction in vulnerability
to acquiring STIs/HIV as they gain in education status and potentially
move up in demographic areas and/or status.
Abortion
Globally, an estimated 25 million unsafe abortions occur each year. The vast majority of such unsafe abortions occur in developing countries in Africa, Asia and Latin America.
The abortion debate is the ongoing controversy surrounding the moral, legal, and religious status of induced abortion. The sides involved in the debate are the self-described “pro-choice” and “pro-life”
movements. “Pro-choice” emphasizes the right of women to decide whether
to terminate a pregnancy. “Pro-life” emphasizes the right of the embryo
or fetus to gestate to term and be born. Both terms are considered loaded in mainstream media, where terms such as “abortion rights” or “anti-abortion” are generally preferred.
Each movement has, with varying results, sought to influence public
opinion and to attain legal support for its position, with small numbers
of anti-abortion advocates using violence, such as murder and arson.
Articles from the World Health Organization call legal abortion a fundamental right of women regardless of where they live, and argue that unsafe abortion is a silent pandemic.
In 2005, it was estimated that 19-20 million abortions had
complications, some complications are permanent, while another estimated
68,000 women died from unsafe abortions.
Having access to safe abortion can have positive impacts on women's
health and life, and vice versa. "Legislation of abortion on request is
necessary but an insufficient step towards improving women's health.
In some countries where it abortion is legal, and has been for decades,
there has been no improvement in access to adequate services making
abortion unsafe due to lack of healthcare services. It is hard to get an
abortion due to legal and policy barriers, social and cultural barriers
(gender discrimination, poverty, religious restrictions, lack of
support etc., health system barriers (lack of facilities or trained
personnel), however safe abortions with trained personnel, good social
support, and access to facilities, can improve maternal health and
increase reproductive health later in life.
The Maputo Protocol, which was adopted by the African Union in the form of a protocol to the African Charter on Human and Peoples' Rights,
states at Article 14 (Health and Reproductive Rights) that: "(2).
States Parties shall take all appropriate measures to: [...] c) protect
the reproductive rights of women by authorising medical abortion in
cases of sexual assault, rape, incest, and where the continued pregnancy
endangers the mental and physical health of the mother or the life of
the mother or the foetus."
The Maputo Protocol is the first international treaty to recognize
abortion, under certain conditions, as a woman's human right.
The General comment No. 36 (2018) on article 6 of the International Covenant on Civil and Political Rights, on the right to life, adopted by the Human Rights Committee
in 2018, defines, for the first time ever, a human right to abortion -
in certain circumstances (however these UN general comments are
considered soft law, and, as such, not legally binding).
"Although States parties may adopt measures designed to regulate voluntary terminations of pregnancy, such measures must not result in violation of the right to life of a pregnant woman or girl, or her other rights under the Covenant. Thus, restrictions on the ability of women or girls to seek abortion must not, inter alia, jeopardize their lives, subject them to physical or mental pain or suffering which violates article 7, discriminate against them or arbitrarily interfere with their privacy. States parties must provide safe, legal and effective access to abortion where the life and health of the pregnant woman or girl is at risk, and where carrying a pregnancy to term would cause the pregnant woman or girl substantial pain or suffering, most notably where the pregnancy is the result of rape or incest or is not viable. [8] In addition, States parties may not regulate pregnancy or abortion in all other cases in a manner that runs contrary to their duty to ensure that women and girls do not have to undertake unsafe abortions, and they should revise their abortion laws accordingly. [9] For example, they should not take measures such as criminalizing pregnancies by unmarried women or apply criminal sanctions against women and girls undergoing abortion [10] or against medical service providers assisting them in doing so, since taking such measures compel women and girls to resort to unsafe abortion. States parties should not introduce new barriers and should remove existing barriers that deny effective access by women and girls to safe and legal abortion, including barriers caused as a result of the exercise of conscientious objection by individual medical providers."
When negotiating the Cairo Programme of Action at the 1994 International Conference on Population and Development
(ICPD), the issue was so contentious that delegates eventually decided
to omit any recommendation to legalize abortion, instead advising
governments to provide proper post-abortion care and to invest in
programs that will decrease the number of unwanted pregnancies.
The Committee on the Elimination of Discrimination against Women
considers the criminalization of abortion a "violations of women’s
sexual and reproductive health and rights" and a form of "gender based
violence"; paragraph 18 of its General recommendation No. 35 on gender based violence against women, updating general recommendation No. 19
states that: "Violations of women’s sexual and reproductive health and
rights, such as forced sterilizations, forced abortion, forced
pregnancy, criminalisation of abortion, denial or delay of safe
abortion and post abortion care, forced continuation of pregnancy,
abuse and mistreatment of women and girls seeking sexual and
reproductive health information, goods and services, are forms of gender based violence that, depending on the circumstances, may amount to torture or cruel, inhuman or degrading treatment." The same General Recommendation
also urges countries at paragraph 31 to [...] In particular, repeal:
a) Provisions that allow, tolerate or condone forms of gender
based violence against women, including [...] legislation that
criminalises abortion".
In 2008, the Parliamentary Assembly of the Council of Europe,
a group comprising members from 47 European countries, has adopted a
resolution calling for the decriminalization of abortion within
reasonable gestational limits and guaranteed access to safe abortion
procedures. The nonbinding resolution was passed on April 16 by a vote
of 102 to 69.
Accesses to abortion is not only a question of legality, but also an issue of overcoming de facto barriers, such as conscientious objections from medical stuff, high prices, lack of knowledge about the law, lack of access to medical care (especially in rural areas). The de facto
inability of women to access abortion even in countries where it is
legal is highly controversial because it results in a situation where
women have rights only on paper not in practice; the UN in its 2017
resolution on Intensification of efforts to prevent and eliminate all forms of violence against women and girls: domestic violence urged states to guarantee access to "safe abortion where such services are permitted by national law".
There are two primary arguments for maintaining legalized
abortion today in the U.S. The first is recognizing the full citizenship
of women. The Roe v. Wade court case on abortion compared the citizenship of women and fetuses Because the Constitution defines born people as citizens, Justice Harry Blackmun ruled that fetuses were not citizens. The citizenship of women is emphasized because fetuses are not individual entities that can exist without the woman.
Another reason why the full citizenship of women is defined by
advocates for abortion is that it recognizes the right of women to
manage their own bodies. Fertility affects women's bodies. The argument for abortion prevents others from making decisions that alter a woman's body.
Pro-choice advocates also attempt to confirm that state-mandated
education or other outside biases don't attempt to influence these
decisions. Feminists argue that women throughout history have had to justify their citizenship politically and socially. The right to manage one's own body is a matter of health, safety, and respect.
The citizenship of women and the right to manage their own bodies is a
societal confirmation that feminists highlight as a pro-choice
justification.
The second primary argument to uphold legalized abortion and
creating better access to it is the necessity of abortion and the health
and safety of pregnant women. There are two events that largely changed the course of public opinion about abortion in the U.S.
The first is Sherry Finkbine, who was denied access to an abortion by
the board of obstetrician-gynecologists at her local hospital.
Although she was privileged enough to afford the trip, Finkbine was
forced to travel to Sweden for an abortion to avoid caring for a damaged
fetus in addition to four children. The other event that changed public opinion was the outbreak of rubella in the 1950s and 60s.
Because rubella disrupted the growth of fetuses and caused deformities
during pregnancy, the California Therapeutic Abortion Act was signed in
1967. This Act allowed doctors to perform abortions when the pregnancy risked the physical or mental health of the pregnant person.
These two events are commonly used to show how the health and safety of
pregnant women are contingent upon abortions as well as the ability to
give birth to and adequately take care of a child. Another argument in
favor of legalized abortion to service necessity are the reasons why an
abortion might be necessary. Nearly half of all pregnancies in the
United States are unintended, and over half of all unintended
pregnancies in the United States are met with abortion.
Unintended pregnancy can lead to serious harm to women and children for
reasons such as not being able to afford to raise a baby,
inaccessibility to time off of work, difficulties facing single
motherhood, difficult socio-economic conditions for women.
Unintended pregnancies also have a greater potential for putting women
of color at risk due to systematically produced environmental hazards
from proximity to pollution, access to livable income, and affordable
healthy food. These factors as threats to the health and safety of pregnant women run parallel to data that shows the number of abortions in the United States did not decline while laws restricting legal access to abortion were implemented.
At a global level, the region with the strictest abortion laws is considered to be Latin America, a region strongly influenced by the Catholic Church in Latin America.
Female genital mutilation
Prevalence of FGM by country, according to a 2013 UNICEF report
Anti-FGM road sign, Bakau, Gambia, 2005
Female genital mutilation (FGM), also known as female genital
circumcision or cutting, is the traditional, non-medical practice of
altering or injuring the female reproductive organs, often by removing
all or parts of the external genitalia.
It is mostly practiced in 30 countries in Africa, the Middle East, and
Asia, and affects over 200 million women and girls worldwide. More
severe forms of FGM are highly concentrated in Djibouti, Eritrea,
Ethiopia, Somalia, and Sudan.
The WHO categorizes FGM into four types:
- Type I (Cliteridectomy) is the removal of all or part of the clitoris. This may or may not include removing the prepuce along with the clitoral glans.
- Type II (Excision) is the removal of the clitoris along with all or part of the labia minora. This may or may not include removing all or part of the labia majora.
- Type III (Infibulation) is the act of removing the inner or outer labia and sealing the wound, leaving only a narrow opening.
- Type IV refers to "all other harmful procedures to the female genitalia for non-medical purposes (piercing, scraping, cauterizing of the genital area)."
FGM often takes the form of a traditional celebration conducted by an
elder or community leader. The age that women undergo the procedure
varies depending on the culture, although it is most commonly performed
on prepubescent girls. Certain cultures value FGM as coming of age
ritual for girls, and use it to preserve a woman's virginity and
faithfulness to the husband after marriage. It is also closely connected
with some traditional ideals of female beauty and hygiene. FGM may or may not have religious connotations depending on the circumstances.
There are no health benefits of FGM, as it interferes with the
natural functions of a woman's and girls' bodies, such as causing severe
pain, shock, hemorrhage, tetanus or sepsis (bacterial infection), urine
retention, open sores in the genital region and injury to nearby
genital tissue, recurrent bladder and urinary tract infections, cysts,
increased risk of infertility, childbirth complications and newborn
deaths. Sexual problems are 1.5 more likely to occur in women who have
undergone FGM, they may experience painful intercourse, have less sexual
satisfaction, and be two times more likely to report lack of sexual
desire. In addition, the maternal and fetal death rate is significantly
higher due to childbirth complications.
FGM can have severe negative psychological effects on women, both
during and after the procedure. These can include long-term symptoms of
depression, anxiety, post-traumatic stress disorder, and low
self-esteem.
Some women report that the procedure was carried out without their
consent and knowledge, and describe feelings of fear and helplessness
while it was taking place. A 2018 study found that larger quantities of
the hormone cortisol
were secreted in women who had undergone FGM, especially those who had
experienced more severe forms of the procedure and at an early age. This
marks the body's chemical response to trauma and stress, and can
indicate a greater risk for developing symptoms of PTSD and other trauma
disorders, although there are limited studies showing a direct
correlation.
Legislation has been introduced in certain countries to prevent
FGM. A 2016 survey of 30 countries showed 24 had policies to manage and
prevent FGM, although the process to provide funding, education, and
resources were often inconsistent and lacking. Some countries have seen a
slight decline in FGM rates, while others show little to no change.
The Istanbul Convention prohibits FGM (Article 38).
Child and forced marriage
Poster against child and forced marriage
The practice of forcing young girls into early marriage, common in
many parts of the world, is threatening their reproductive health.
According to the World Health Organization:
"The sexual and reproductive health of the female in a child marriage is likely to be jeopardized, as these young girls are often forced into sexual intercourse with an older male spouse with more sexual experience. The female spouse often lacks the status and the knowledge to negotiate for safe sex and contraceptive practices, increasing the risk of acquiring HIV or other sexually transmitted infections, as well as the probability of pregnancy at an early age."
Niger has the highest prevalence of child marriage under 18 in the world, while Bangladesh has the highest rate of marriage of girls under age 15. Practices such as bride price and dowry can contribute to child and forced marriages.
International Conference on Population and Development, 1994
The International Conference on Population and Development (ICPD) was held in Cairo,
Egypt, from 5 to 13 September 1994. Delegations from 179 States took
part in negotiations to finalize a Programme of Action on population and
development for the next 20 years. Some 20,000 delegates from various
governments, UN agencies, NGOs, and the media gathered for a discussion of a variety of population issues, including immigration, infant mortality, birth control, family planning, and the education of women.
In the ICPD Program of Action, 'reproductive health' is defined as:
a state of complete physical, mental and social well-being and...not merely the absence of disease or infirmity, in all matters relating to the reproductive system and its functions and processes. Reproductive health therefore implies that people are able to have a satisfying and safe sex life and that they have the capability to reproduce and the freedom to decide if, when and how often to do so. Implicit in this last condition are the right of men and women to be informed [about] and to have access to safe, effective, affordable and acceptable methods of family planning of their choice, as well as other methods of birth control which are not against the law, and the right of access to appropriate health-care services that will enable women to go safely through pregnancy and childbirth and provide couples with the best chance of having a healthy infant.
This definition of the term is also echoed in the United Nations Fourth World Conference on Women, or the so-called Beijing Declaration of 1995.
However, the ICPD Program of Action, even though it received the
support of a large majority of UN Member States, does not enjoy the
status of an international legal instrument; it is therefore not legally
binding.
The Program of Action endorses a new strategy which emphasizes
the numerous linkages between population and development and focuses on
meeting the needs of individual women and men rather than on achieving demographic targets. The ICPD
achieved consensus on four qualitative and quantitative goals for the
international community, the final two of which have particular
relevance for reproductive health:
- Reduction of maternal mortality: A reduction of maternal mortality rates and a narrowing of disparities in maternal mortality within countries and between geographical regions, socio-economic and ethnic groups.
- Access to reproductive and sexual health services including family planning: Family planning counseling, pre-natal care, safe delivery and post-natal care, prevention and appropriate treatment of infertility, prevention of abortion and the management of the consequences of abortion, treatment of reproductive tract infections, sexually transmitted diseases and other reproductive health conditions; and education, counseling, as appropriate, on human sexuality, reproductive health and responsible parenthood. Services regarding HIV/AIDS, breast cancer, infertility, delivery, hormone therapy, sex reassignment therapy, and abortion should be made available. Active discouragement of female genital mutilation (FGM).
The keys to this new approach are empowering women, providing them
with more choices through expanded access to education and health
services, and promoting skill development and employment. The programme
advocates making family planning universally available by 2015 or
sooner, as part of a broadened approach to reproductive health and
rights, provides estimates of the levels of national resources and
international assistance that will be required, and calls on governments
to make these resources available.
Sustainable Development Goals
Half of the development goals put on by the United Nations started in 2000 to 2015 with the Millennium Development Goals (MDGs). Reproductive health was Goal 5 out of 8. To monitor the progress, the UN agreed to four indicators:
- Contraceptive prevalence rates
- Adolescent birth rate
- Antenatal care coverage
- Unmet need for family planning
Progress was slow, and according to the WHO in 2005, about 55% of women did not have sufficient antenatal care and 24% had no access to family planning services.
The MDGs expired in 2015 and were replaced with a more comprehensive
set of goals to cover a span of 2016-2030 with a total of 17 goals,
called the Sustainable Development Goals.
All 17 goals are comprehensive in nature and build off one another, but
goal 3 is "To ensure health lives and promote wellbeing for all at all
ages". Specific goals are to reduce global maternal mortality ratio to
less than 70 per 100,000 live births, end preventable deaths of newborns
and children, reduce the number by 50% of accidental deaths globally,
strengthen the treatment and prevention programs of substance abuse and
alcohol.
By region
Africa
World AIDS Day 2006 event in Kenya.
Prevalence of HIV/AIDS in Africa
HIV/AIDS in Africa is a major public health problem. Sub-Saharan
Africa is the worst affected world region for prevalence of HIV,
especially among young women. 90% of the children in the world living
with HIV are in sub-Saharan Africa.
In most African countries, the total fertility rate is very high,
often due to lack of access to contraception and family planning, and
practices such as forced and child marriage. Niger, Angola, Mali,
Burundi and Somalia have very high fertility rates.
The updated contraceptive guidelines in South Africa
attempt to improve access by providing special service delivery and
access considerations for sex workers, lesbian, gay, bisexual,
transgender and intersex individuals, migrants, men, adolescents, women
who are perimenopausal, have a disability, or chronic condition. They
also aim to increase access to long acting contraceptive methods,
particularly the copper IUD, and the introductions of single rod
progestogen implant and combined oestrogen and progestogen injectables.
The copper IUD has been provided significantly less frequently than
other contraceptive methods but signs of an increase in most provinces
were reported. The most frequently provided method was injectable
progesterone, which the article acknowledged was not ideal and
emphasised condom use with this method because it can increase the risk
of HIV: The product made up 49% of South Africa's contraceptive use and
up to 90% in some provinces.
Tanzanian
provider perspectives address the obstacles to consistent contraceptive
use in their communities. It was found that the capability of
dispensaries to service patients was determined by inconsistent
reproductive goals, low educational attainment, misconceptions about the
side effects of contraceptives, and social factors such as gender
dynamics, spousal dynamics, economic conditions, religious norms,
cultural norms, and constraints in supply chains. A provider referenced
and example of propaganda spread about the side effects of
contraception: "There are influential people, for example elders and
religious leaders. They normally convince people that condoms contain
some microorganisms and contraceptive pills cause cancer". Another said
that women often had pressure from their spouse or family that caused
them to use birth control secretly or to discontinue use, and that women
frequently preferred undetectable methods for this reason. Access was
also hindered as a result of a lack in properly trained medical
personnel: "Shortage of the medical attendant...is a challenge, we are
not able to attend to a big number of clients, also we do not have
enough education which makes us unable to provide women with the methods
they want". The majority of medical centers were staffed by people
without medical training and few doctors and nurses, despite federal
regulations, due to lack of resources. One center had only one person
who was able to insert and remove implants, and without her they were
unable to service people who wanted an implant inserted or removed.
Another dispensary that carried two methods of birth control shared that
they sometimes run out of both materials at the same time. Constraints
in supply chains sometimes cause dispensaries to run out of
contraceptive materials. Providers also claimed that more male
involvement and education would be helpful.
Public health officials, researchers, and programs can gain a more
comprehensive picture of the barriers they face, and the efficacy of
current approaches to family planning, by tracking specific,
standardized family planning and reproductive health indicators.