From Wikipedia, the free encyclopedia
The United States Food and Drug Administration (FDA or US FDA) is a federal agency of the Department of Health and Human Services. The FDA is responsible for protecting and promoting public health through the control and supervision of food safety, tobacco products, caffeine products, dietary supplements, prescription and over-the-counter pharmaceutical drugs (medications), vaccines, biopharmaceuticals, blood transfusions, medical devices, electromagnetic radiation emitting devices (ERED), cosmetics, animal foods & feed and veterinary products.
The FDA's primary focus is enforcement of the Federal Food, Drug, and Cosmetic Act
(FD&C), but the agency also enforces other laws, notably Section
361 of the Public Health Service Act, as well as associated regulations.
Much of this regulatory-enforcement work is not directly related to
food or drugs, but involves such things as regulating lasers, cellular phones, and condoms, as well as control of disease in contexts varying from household pets to human sperm donated for use in assisted reproduction.
The FDA is led by the Commissioner of Food and Drugs, appointed by the President with the advice and consent of the Senate. The Commissioner reports to the Secretary of Health and Human Services. Robert Califf is the current commissioner, as of 17 February 2022.
The FDA has its headquarters in unincorporated White Oak, Maryland. The agency also has 223 field offices and 13 laboratories located throughout the 50 states, the United States Virgin Islands, and Puerto Rico.
In 2008, the FDA began to post employees to foreign countries,
including China, India, Costa Rica, Chile, Belgium, and the United
Kingdom.
Organizational structure
Location
Headquarters
FDA headquarters facilities are currently located in Montgomery County and Prince George's County, Maryland.
White Oak Federal Research Center
Since 1990, the FDA has had employees and facilities on 130 acres (53 hectares) of the White Oak Federal Research Center in the White Oak area of Silver Spring, Maryland. In 2001, the General Services Administration (GSA) began new construction on the campus to consolidate the FDA's 25 existing operations in the Washington metropolitan area, its headquarters in Rockville,
and several fragmented office buildings. The first building, the Life
Sciences Laboratory, was dedicated and opened with 104 employees in
December 2003. As of December 2018, the FDA campus has a population of
10,987 employees housed in approximately 3,800,000 square feet (350,000
square metres) of space, divided into ten office and four laboratory
buildings. The campus houses the Office of the Commissioner (OC), the Office of Regulatory Affairs (ORA), the Center for Drug Evaluation and Research (CDER), the Center for Devices and Radiological Health (CDRH), the Center for Biologics Evaluation and Research (CBER) and offices for the Center for Veterinary Medicine (CVM).
With the passing of the FDA Reauthorization Act of 2017, the FDA
is projecting a 64% increase in employees to 18,000 over the next 15
years, and would like to add approximately 1,600,000 square feet
(150,000 square metres) of office and special use space to their
existing facilities. The National Capital Planning Commission approved a new master plan for this expansion in December 2018, and construction is expected to be completed by 2035, dependent on GSA appropriations.
Field locations
The Arkansas Laboratory in
Jefferson, Arkansas is the headquarters of the National Center for Toxicological Research.
Office of Regulatory Affairs
The Office of Regulatory Affairs
is considered the agency's "eyes and ears," conducting the vast
majority of the FDA's work in the field. Its employees, known as
Consumer Safety Officers, or more commonly known simply as
investigators, inspect production and warehousing facilities,
investigate complaints, illnesses, or outbreaks, and review
documentation in the case of medical devices, drugs, biological
products, and other items where it may be difficult to conduct a
physical examination or take a physical sample of the product. The
Office of Regulatory Affairs is divided into five regions, which are
further divided into 20 districts. Districts are based roughly on the
geographic divisions of the Federal court system.
Each district comprises a main district office and a number of Resident
Posts, which are FDA remote offices that serve a particular geographic
area. ORA also includes the Agency's network of regulatory laboratories,
which analyze any physical samples taken. Though samples are usually
food-related, some laboratories are equipped to analyze drugs,
cosmetics, and radiation-emitting devices.
Office of Criminal Investigations
Jamaica, Queens, New York Regional Office - USFDA
The Office of Criminal Investigations
was established in 1991 to investigate criminal cases. To do so, OCI
employs approximately 200 Special Agents nationwide who, unlike ORA
Investigators, are armed, have badges, and do not focus on technical
aspects of the regulated industries. Rather, OCI agents pursue and
develop cases when individuals and companies commit criminal actions,
such as fraudulent claims or knowingly and willfully shipping known
adulterated goods in interstate commerce. In many cases, OCI pursues
cases involving violations of Title 18 of the United States Code
(e.g., conspiracy, false statements, wire fraud, mail fraud), in
addition to prohibited acts as defined in Chapter III of the FD&C
Act. OCI Special Agents often come from other criminal investigations
backgrounds, and frequently work closely with the Federal Bureau of Investigation, Assistant Attorney General, and even Interpol.
OCI receives cases from a variety of sources—including ORA, local
agencies, and the FBI, and works with ORA Investigators to help develop
the technical and science-based aspects of a case.
Other locations
The
FDA has a number of field offices across the United States, in addition
to international locations in China, India, Europe, the Middle East,
and Latin America.
Scope and funding
As of 2021, the FDA had responsibility for overseeing $2.7 trillion in food, medical, and tobacco products. Some 54% of its budget derives from the federal government, and 46% is covered by industry user fees for FDA services. For example, pharmaceutical firms pay fees to expedite drug reviews.
According to Forbes, the pharmaceutical firms provide 75% of the FDA's drug review budget.
Regulatory programs
Emergency approvals (EUA)
Emergency
Use Authorization (EUA) is a mechanism that was created to facilitate
the availability and use of medical countermeasures, including vaccines
and personal protective equipment, during public health emergencies such
as the Zika virus epidemic, the Ebola virus epidemic and the COVID-19
pandemic.
Regulations
The
programs for safety regulation vary widely by the type of product, its
potential risks, and the regulatory powers granted to the agency. For
example, the FDA regulates almost every facet of prescription drugs,
including testing, manufacturing, labeling, advertising, marketing,
efficacy, and safety—yet FDA regulation of cosmetics focuses primarily
on labeling and safety. The FDA regulates most products with a set of
published standards enforced by a modest number of facility inspections.
Inspection observations are documented on Form 483.
In June 2018, the FDA released a statement regarding new
guidelines to help food and drug manufacturers "implement protections
against potential attacks on the U.S. food supply".
One of the guidelines includes the Intentional Adulteration (IA) rule,
which requires strategies and procedures by the food industry to reduce
the risk of compromise in facilities and processes that are
significantly vulnerable.
The FDA also uses tactics of regulatory shaming,
mainly through online publication of non-compliance, warning letters,
and "shaming lists." Regulation by shaming harnesses firms' sensitivity
to reputational damage. For example, in 2018, the agency published an
online "black list," in which it named dozens of branded drug companies
that are supposedly using unlawful or unethical means to attempt to
impede competition from generic drug companies.
The FDA frequently works with other federal agencies, including the Department of Agriculture, the Drug Enforcement Administration, Customs and Border Protection, and the Consumer Product Safety Commission. They also often work with local and state government agencies in performing regulatory inspections and enforcement actions.
Food and dietary supplements
The regulation of food and dietary supplements by the Food and Drug
Administration is governed by various statutes enacted by the United States Congress and interpreted by the FDA. Pursuant to the Federal Food, Drug, and Cosmetic Act
and accompanying legislation, the FDA has authority to oversee the
quality of substances sold as food in the United States, and to monitor
claims made in the labeling of both the composition and the health benefits of foods.
The FDA subdivides substances that it regulates as food into various categories—including foods, food additives, added substances (human-made substances that are not intentionally introduced into food, but nevertheless end up in it), and dietary supplements. Dietary supplements or dietary ingredients include vitamins, minerals, herbs, amino acids, and. enzymes.
Specific standards the FDA exercises differ from one category to the
next. Furthermore, legislation had granted the FDA a variety of means to
address violations of standards for a given substance category.
Under the Dietary Supplement Health and Education Act of 1994
(DSHEA), the FDA is responsible for ensuring that manufacturers and
distributors of dietary supplements and dietary ingredients meet the
current requirements. These manufacturers and distributors are not
allowed to advertise their products in an adulterated way, and they are
responsible for evaluating the safety and labeling of their product.
The FDA has a "Dietary Supplement Ingredient Advisory List" that
includes ingredients that sometimes appear on dietary supplements but
need further evaluation further.
An ingredient is added to this list when it is excluded from use in a
dietary supplement, does not appear to be an approved food additive or
recognized as safe, and/or is subjected to the requirement for
pre-market notification without having a satisfied requirement.
"FDA-Approved" vs. "FDA-Accepted in Food Processing"
The FDA does not approve applied coatings used in the food processing industry.
There is no review process to approve the composition of nonstick
coatings; nor does the FDA inspect or test these materials. Through
their governing of processes, however, the FDA does have a set of
regulations that cover the formulation, manufacturing, and use of
nonstick coatings. Hence, materials like Polytetrafluoroethylene (Teflon) are not, and cannot be, considered as FDA Approved, rather, they are "FDA Compliant" or "FDA Acceptable".
Medical countermeasures (MCMs)
Medical countermeasures (MCMs) are products such as biologics and pharmaceutical drugs
that can protect from or treat the health effects of a chemical,
biological, radiological, or nuclear (CBRN) attack. MCMs can also be
used for prevention and diagnosis of symptoms associated with CBRN
attacks or threats.
The FDA runs a program called the "FDA Medical Countermeasures
Initiative" (MCMi), with programs funded by the federal government. It
helps support "partner" agencies and organisations prepare for public health emergencies that could require MCMs.
Medications
The Center for Drug Evaluation and Research
uses different requirements for the three main drug product types: new
drugs, generic drugs, and over-the-counter drugs. A drug is considered
"new" if it is made by a different manufacturer, uses different excipients
or inactive ingredients, is used for a different purpose, or undergoes
any substantial change. The most rigorous requirements apply to new molecular entities: drugs that are not based on existing medications.[33]
New medications
New drugs receive extensive scrutiny before FDA approval in a process called a new drug application (NDA). Under the Trump administration, the agency has worked to make the drug-approval process go faster.
Critics, however, argue that the FDA standards are not sufficiently
rigorous, allowing unsafe or ineffective drugs to be approved.
New drugs are available only by prescription by default. A change to
over-the-counter (OTC) status is a separate process, and the drug must
be approved through an NDA first. A drug that is approved is said to be
"safe and effective when used as directed".
Very rare, limited exceptions to this multi-step process
involving animal testing and controlled clinical trials can be granted
out of compassionate use protocols. This was the case during the 2015
Ebola epidemic with the use, by prescription and authorization, of ZMapp
and other experimental treatments, and for new drugs that can be used
to treat debilitating and/or very rare conditions for which no existing
remedies or drugs are satisfactory, or where there has not been an
advance in a long period of time. The studies are progressively longer,
gradually adding more individuals as they progress from stage I to stage
III, normally over a period of years, and normally involve drug
companies, the government and its laboratories, and often medical
schools and hospitals and clinics. However, any exceptions to the
aforementioned process are subject to strict review and scrutiny and
conditions, and are only given if a substantial amount of research and
at least some preliminary human testing has shown that they are believed
to be somewhat safe and possibly effective. (See FDA Special Protocol
Assessment about Phase III trials.)
Advertising and promotion
The FDA's Office of Prescription Drug Promotion reviews and regulates
prescription drug advertising and promotion through surveillance
activities and issuance of enforcement letters to pharmaceutical
manufacturers. Advertising and promotion for over-the-counter drugs is
regulated by the Federal Trade Commission.
The FDA also empowers third-party enforcer-firms to engage in some
regulatory oversight, e.g. the FDA expects pharmaceutical companies to
make sure that third-party suppliers and labs abide by the agency's
health and safety guidelines.
The drug advertising regulation
contains two broad requirements: (1) a company may advertise or promote
a drug only for the specific indication or medical use for which it was
approved by FDA. Also, an advertisement must contain a "fair balance"
between the benefits and the risks (side effects) of a drug.
The term off-label refers to the practice of prescribing a drug for a different purpose than what the FDA approved.
Post-market safety surveillance
After
NDA approval, the sponsor must then review and report to the FDA every
single patient adverse drug experience it learns of. They must report
unexpected serious and fatal adverse drug events within 15 days, and
other events on a quarterly basis. The FDA also receives directly adverse drug event reports through its MedWatch program. These reports are called "spontaneous reports" because reporting by consumers and health professionals is voluntary.
While this remains the primary tool of post-market safety surveillance,
FDA requirements for post-marketing risk management are increasing. As a
condition of approval, a sponsor may be required to conduct additional clinical trials, called Phase IV trials. In some cases, the FDA requires risk management plans called Risk Evaluation and Mitigation Strategies (REMS) for some drugs that require actions to be taken to ensure that the drug is used safely. For example, thalidomide
can cause birth defects, but has uses that outweigh the risks if men
and women taking the drugs do not conceive a child; a REMS program for
thalidomide mandates an auditable process to ensure that people taking
the drug take action to avoid pregnancy; many opioid drugs have REMS programs to avoid addiction and diversion of drugs. The drug isotretinoin has a REMS program called iPLEDGE.
Generic drugs
Generic drugs are chemical and therapeutic equivalents of name-brand drugs, normally whose patents have expired.
Approved generic drugs should have the same dosage, safety,
effectiveness, strength, stability, and quality, as well as route of
administration. In general, they are less expensive than their name
brand counterparts, are manufactured and marketed by rival companies
and, in the 1990s, accounted for about a third of all prescriptions
written in the United States.
For a pharmaceutical company to gain approval to produce a generic
drug, the FDA requires scientific evidence that the generic drug is
interchangeable with or therapeutically equivalent to the originally
approved drug. This is called an Abbreviated New Drug Application (ANDA). As of 2012, 80% of all FDA approved drugs are available in generic form.
Generic drug scandal
In 1989, a major scandal erupted involving the procedures used by the FDA to approve generic drugs for sale to the public.
Charges of corruption in generic drug approval first emerged in 1988
during the course of an extensive congressional investigation into the
FDA. The oversight subcommittee of the United States House Energy and Commerce Committee resulted from a complaint brought against the FDA by Mylan Laboratories Inc. of Pittsburgh.
When its application to manufacture generics were subjected to repeated
delays by the FDA, Mylan, convinced that it was being discriminated
against, soon began its own private investigation of the agency in 1987.
Mylan eventually filed suit against two former FDA employees and four
drug-manufacturing companies, charging that corruption within the
federal agency resulted in racketeering and in violations of antitrust law.
"The order in which new generic drugs were approved was set by the FDA
employees even before drug manufacturers submitted applications" and,
according to Mylan, this illegal procedure was followed to give
preferential treatment to certain companies. During the summer of 1989,
three FDA officials (Charles Y. Chang, David J. Brancato, Walter Kletch)
pleaded guilty to criminal charges of accepting bribes from generic
drugs makers, and two companies (Par Pharmaceutical and its subsidiary Quad Pharmaceuticals) pleaded guilty to giving bribes.
Furthermore, it was discovered that several manufacturers had
falsified data submitted in seeking FDA authorization to market certain
generic drugs. Vitarine Pharmaceuticals of New York, which sought
approval of a generic version of the drug Dyazide,
a medication for high blood pressure, submitted Dyazide, rather than
its generic version, for the FDA tests. In April 1989, the FDA
investigated 11 manufacturers for irregularities; and later brought that
number up to 13. Dozens of drugs were eventually suspended or recalled
by manufacturers. In the early 1990s, the U.S. Securities and Exchange Commission
filed securities fraud charges against the Bolar Pharmaceutical
Company, a major generic manufacturer based in Long Island, New York.
Over-the-counter drugs
Over-the-counter (OTC) are drugs like aspirin that do not require a doctor's prescription.
The FDA has a list of approximately 800 such approved ingredients that
are combined in various ways to create more than 100,000 OTC drug
products. Many OTC drug ingredients had been previously approved
prescription drugs now deemed safe enough for use without a medical practitioner's supervision like ibuprofen.
Ebola treatment
In 2014, the FDA added an Ebola treatment being developed by Canadian pharmaceutical company Tekmira to the Fast Track program,
but halted the phase 1 trials in July pending the receipt of more
information about how the drug works. This was widely viewed as
increasingly important in the face of a major outbreak of the disease in West Africa that began in late March 2014 and ended in June 2016.
Coronavirus (COVID-19) testing
During the coronavirus pandemic, FDA granted emergency use authorization for personal protective equipment (PPE), in vitro diagnostic equipment, ventilators and other medical devices.
On March 18, 2020, FDA inspectors postponed most foreign facility
inspections and all domestic routine surveillance facility inspections. In contrast, the USDA's Food Safety and Inspection Service
(FSIS) continued inspections of meatpacking plants, which resulted in
145 FSIS field employees who tested positive for COVID-19, and three who
died.
Vaccines, blood and tissue products, and biotechnology
FDA scientist prepares blood donation samples for testing.
The Center for Biologics Evaluation and Research is the branch of the FDA responsible for ensuring the safety and efficacy of biological therapeutic agents.
These include blood and blood products, vaccines, allergenics, cell and
tissue-based products, and gene therapy products. New biologics are
required to go through a premarket approval process called a Biologics License Application (BLA), similar to that for drugs.
The original authority for government regulation of biological products was established by the 1902 Biologics Control Act, with additional authority established by the 1944 Public Health Service Act. Along with these Acts, the Federal Food, Drug, and Cosmetic Act
applies to all biologic products, as well. Originally, the entity
responsible for regulation of biological products resided under the National Institutes of Health; this authority was transferred to the FDA in 1972.
Medical and radiation-emitting devices
The Center for Devices and Radiological Health (CDRH) is the branch of the FDA responsible for the premarket approval of all medical devices, as well as overseeing the manufacturing, performance and safety of these devices. The definition of a medical device is given in the FD&C Act, and it includes products from the simple toothbrush to complex devices such as implantable neurostimulators. CDRH also oversees the safety performance of non-medical devices that emit certain types of electromagnetic radiation. Examples of CDRH-regulated devices include cellular phones, airport baggage screening equipment, television receivers, microwave ovens, tanning booths, and laser products.
CDRH regulatory powers include the authority to require certain
technical reports from the manufacturers or importers of regulated
products, to require that radiation-emitting products meet mandatory
safety performance standards, to declare regulated products defective,
and to order the recall of defective or noncompliant products. CDRH also
conducts limited amounts of direct product testing.
"FDA-Cleared" vs "FDA-Approved"
Clearance
requests are required for medical devices that prove they are
"substantially equivalent" to the predicate devices already on the
market. Approved requests are for items that are new or substantially
different and need to demonstrate "safety and efficacy", for example
they may be inspected for safety in case of new toxic hazards. Both
aspects need to be proved or provided by the submitter to ensure proper
procedures are followed.
Cosmetics
Cosmetics are regulated by the Center for Food Safety and Applied Nutrition,
the same branch of the FDA that regulates food. Cosmetic products are
not, in general, subject to premarket approval by the FDA unless they
make "structure or function claims" that make them into drugs (see Cosmeceutical).
However, all color additives must be specifically FDA approved before
manufacturers can include them in cosmetic products sold in the U.S. The
FDA regulates cosmetics labeling, and cosmetics that have not been
safety tested must bear a warning to that effect.
According to the industry advocacy group the American Council on Science and Health,
though the cosmetic industry is predominantly responsible in ensuring
the safety of its products, the FDA also has the power to intervene when
necessary to protect the public but in general does not require
pre-market approval or testing. The ACSH says that companies are
required to place a warning note on their products if they have not been
tested and that experts in cosmetic ingredient reviews also play a role
in monitoring safety through influence on the use of ingredients, but
also lack legal authority. According to the ACSH, overall the
organization has reviewed about 1,200 ingredients and has suggested that
several hundred be restricted, but there is no standard or systemic
method for reviewing chemicals for safety and a clear definition of what
is meant by 'safety' so that all chemicals are tested on the same
basis.
Veterinary products
The Center for Veterinary Medicine (CVM) is a center of the FDA that regulates food additives and drugs that are given to animals.
CVM regulates animal drugs, animal food including pet animal, and
animal medical devices. The FDA's requirements to prevent the spread of bovine spongiform encephalopathy are also administered by CVM through inspections of feed manufacturers. CVM does not regulate vaccines for animals; these are handled by the United States Department of Agriculture.
Tobacco products
The FDA regulates tobacco products with authority established by the 2009 Family Smoking Prevention and Tobacco Control Act. This Act requires color warnings on cigarette packages and printed advertising, and text warnings from the U.S. Surgeon General.[66]
The nine new graphic warning labels were announced by the FDA in
June 2011 and were scheduled to be required to appear on packaging by
September 2012. The implementation date is uncertain, due to ongoing
proceedings in the case of R.J. Reynolds Tobacco Co. v. U.S. Food and Drug Administration. R.J. Reynolds, Lorillard, Commonwealth Brands, Liggett Group and Santa Fe Natural Tobacco Company have filed suit in Washington, D.C. federal court claiming that the graphic labels are an unconstitutional way of forcing tobacco companies to engage in anti-smoking advocacy on the government's behalf.
A First Amendment lawyer, Floyd Abrams,
is representing the tobacco companies in the case, contending requiring
graphic warning labels on a lawful product cannot withstand
constitutional scrutiny. The Association of National Advertisers and the American Advertising Federation
have also filed a brief in the suit, arguing that the labels infringe
on commercial free speech and could lead to further government intrusion
if left unchallenged. In November 2011, Federal judge Richard Leon
of the U.S. District Court for the District of Columbia temporarily
halted the new labels, likely delaying the requirement that tobacco
companies display the labels. The U.S. Supreme Court ultimately could decide the matter.
In July 2017, the FDA announced a plan that would reduce the current levels of nicotine permitted in tobacco cigarettes.
Regulation of living organisms
With acceptance of premarket notification 510(k) k033391 in January 2004, the FDA granted Ronald Sherman permission to produce and market medical maggots for use in humans or other animals as a prescription medical device.
Medical maggots represent the first living organism allowed by the Food
and Drug Administration for production and marketing as a prescription
medical device.
In June 2004, the FDA cleared Hirudo medicinalis (medicinal leeches) as the second living organism legal to use as a medical device.
The FDA also requires that milk be pasteurized to remove bacteria.
International Cooperation
In February 2011, President Barack Obama and Canadian Prime Minister Stephen Harper issued a "Declaration on a Shared Vision for Perimeter Security and Economic Competitiveness"
and announced the creation of the Canada-United States Regulatory
Cooperation Council (RCC) "to increase regulatory transparency and
coordination between the two countries."
Under the RCC mandate, the FDA and Health Canada
undertook a "first of its kind" initiative by selecting "as its first
area of alignment common cold indications for certain over-the-counter antihistamine ingredients (GC 2013-01-10)."
A more recent example of the FDA's international work is their
2018 cooperation with regulatory and law-enforcement agencies worldwide
through Interpol as part of Operation Pangea XI. The FDA targeted 465 websites that illegally sold potentially dangerous, unapproved versions of opioid, oncology, and antiviral prescription drugs to U.S. consumers. The agency focused on transaction laundering schemes in order to uncover the complex online drug network.
Science and research programs
FDA lab at Building 64 in Silver Spring, Maryland
The FDA carries out research and development activities
to develop technology and standards that support its regulatory role,
with the objective of resolving scientific and technical challenges
before they become impediments.
The FDA's research efforts include the areas of biologics, medical
devices, drugs, women's health, toxicology, food safety and applied
nutrition, and veterinary medicine.
Data management
The FDA has collected a large amount of data through the decades. The OpenFDA project was created to enable easy access of the data for the public and was officially launched in June 2014.[86][87]
History
Up until the 20th century, there were few federal laws regulating the
contents and sale of domestically produced food and pharmaceuticals,
with one exception being the short-lived Vaccine Act of 1813. The history of the FDA can be traced to the latter part of the 19th century and the Division of Chemistry of the U.S. Department of Agriculture, which itself derived from the Copyright and Patent Clause. Under Harvey Washington Wiley,
appointed chief chemist in 1883, the Division began conducting research
into the adulteration and misbranding of food and drugs on the American
market. Wiley's advocacy came at a time when the public had become aroused to hazards in the marketplace by muckraking journalists like Upton Sinclair, and became part of a general trend for increased federal regulations in matters pertinent to public safety during the Progressive Era. The Biologics Control Act of 1902 was put in place after a diphtheria
antitoxin derived from tetanus-contaminated serum caused the deaths of
thirteen children in St. Louis, Missouri. The serum was originally
collected from a horse named Jim who had contracted tetanus.
In June 1906, President Theodore Roosevelt signed into law the Pure Food and Drug Act of 1906, also known as the "Wiley Act" after its chief advocate. The Act prohibited, under penalty of seizure of goods, the interstate transport of food that had been "adulterated".
The Act applied similar penalties to the interstate marketing of
"adulterated" drugs, in which the "standard of strength, quality, or
purity" of the active ingredient was not either stated clearly on the
label or listed in the United States Pharmacopeia or the National Formulary.
The responsibility for examining food and drugs for such
"adulteration" or "misbranding" was given to Wiley's USDA Bureau of
Chemistry.
Wiley used these new regulatory powers to pursue an aggressive campaign
against the manufacturers of foods with chemical additives, but the
Chemistry Bureau's authority was soon checked by judicial decisions,
which narrowly defined the bureau's powers and set high standards for
proof of fraudulent intent.
In 1927, the Bureau of Chemistry's regulatory powers were reorganized
under a new USDA body, the Food, Drug, and Insecticide Administration. This name was shortened to the Food and Drug Administration (FDA) three years later.
By the 1930s, muckraking
journalists, consumer protection organizations, and federal regulators
began mounting a campaign for stronger regulatory authority by
publicizing a list of injurious products that had been ruled permissible
under the 1906 law, including radioactive beverages, mascara that could cause blindness, and worthless "cures" for diabetes and tuberculosis. The resulting proposed law did not get through the Congress of the United States for five years, but was rapidly enacted into law following the public outcry over the 1937 Elixir Sulfanilamide tragedy, in which over 100 people died after using a drug formulated with a toxic, untested solvent.
President Franklin Delano Roosevelt signed the Federal Food, Drug, and Cosmetic Act
into law on June 24, 1938. The new law significantly increased federal
regulatory authority over drugs by mandating a pre-market review of the
safety of all new drugs, as well as banning false therapeutic claims in
drug labeling without requiring that the FDA prove fraudulent intent.
Soon after passage of the 1938 Act, the FDA began to designate
certain drugs as safe for use only under the supervision of a medical
professional, and the category of "prescription-only" drugs was securely codified into law by the Durham-Humphrey Amendment in 1951. These developments confirmed extensive powers for the FDA to enforce post-marketing recalls of ineffective drugs.
Medical
Officer Alexander Fleming, M. D., examines a portion of a 240-volume
new drug application around the late 1980s. Applications grew
considerably after the efficacy mandate under the 1962 Drug Amendments.
Outside of the US, the drug thalidomide was marketed for the relief of general nausea and morning sickness, but caused birth defects and even the death of thousands of babies when taken during pregnancy. American mothers were largely unaffected as Frances Oldham Kelsey of the FDA refused to authorize the medication for market. In 1962, the Kefauver-Harris Amendment to the FD&C Act was passed, which represented a "revolution" in FDA regulatory authority.
The most important change was the requirement that all new drug
applications demonstrate "substantial evidence" of the drug's efficacy
for a marketed indication, in addition to the existing requirement for
pre-marketing demonstration of safety. This marked the start of the FDA
approval process in its modern form.
These reforms had the effect of increasing the time, and the difficulty, required to bring a drug to market. One of the most important statutes in establishing the modern American pharmaceutical market was the 1984 Drug Price Competition and Patent Term Restoration Act,
more commonly known as the "Hatch-Waxman Act" after its chief sponsors.
The act extended the patent exclusivity terms of new drugs, and tied
those extensions, in part, to the length of the FDA approval process for
each individual drug. For generic manufacturers, the Act created a new
approval mechanism, the Abbreviated New Drug Application
(ANDA), in which the generic drug manufacturer need only demonstrate
that their generic formulation has the same active ingredient, route of
administration, dosage form, strength, and pharmacokinetic
properties ("bioequivalence") as the corresponding brand-name drug.
This Act has been credited with, in essence, creating the modern generic
drug industry.
Concerns about the length of the drug approval process were
brought to the fore early in the AIDS epidemic. In the mid- and late
1980s, ACT-UP
and other HIV activist organizations accused the FDA of unnecessarily
delaying the approval of medications to fight HIV and opportunistic
infections.
Partly in response to these criticisms, the FDA issued new rules to
expedite approval of drugs for life-threatening diseases, and expanded
pre-approval access to drugs for patients with limited treatment
options. All of the initial drugs approved for the treatment of HIV/AIDS were approved through these accelerated approval mechanisms.
Frank Young, then commissioner of the FDA, was behind the Action Plan
Phase II, established in August 1987 for quicker approval of AIDS
medication.
In two instances, state governments have sought to legalize drugs
that the FDA has not approved. Under the theory that federal law,
passed pursuant to Constitutional authority, overrules conflicting state
laws, federal authorities still claim the authority to seize, arrest,
and prosecute for possession and sales of these substances, even in states where they are legal under state law. The first wave was the legalization by 27 states of laetrile
in the late 1970s. This drug was used as a treatment for cancer, but
scientific studies both before and after this legislative trend found it
ineffective. The second wave concerned medical marijuana in the 1990s and 2000s. Though Virginia passed legislation
allowing doctors to recommend cannabis for glaucoma or the side effects
of chemotherapy, a more widespread trend began in California with the Compassionate Use Act of 1996.
When the FDA requested Endo Pharmaceuticals on June 8, 2017, to remove oxymorphone hydrochloride from the market, it was the first such request in FDA history.
21st century reforms
Critical Path Initiative
The Critical Path Initiative
is the FDA's effort to stimulate and facilitate a national effort to
modernize the sciences through which FDA-regulated products are
developed, evaluated, and manufactured. The Initiative was launched in
March 2004, with the release of a report entitled Innovation/Stagnation:
Challenge and Opportunity on the Critical Path to New Medical Products.
Patients' rights to access unapproved drugs
The Compassionate Investigational New Drug program was created after Randall v. U.S. ruled in favor of Robert C. Randall in 1978, creating a program for medical marijuana.
A 2006 court case, Abigail Alliance v. von Eschenbach,
would have forced radical changes in FDA regulation of unapproved
drugs. The Abigail Alliance argued that the FDA must license drugs for
use by terminally ill patients with "desperate diagnoses," after they
have completed Phase I testing. The case won an initial appeal in May 2006, but that decision was reversed by a March 2007 rehearing. The US Supreme Court declined to hear the case, and the final decision denied the existence of a right to unapproved medications.
Critics
of the FDA's regulatory power argue that the FDA takes too long to
approve drugs that might ease pain and human suffering faster if brought
to market sooner. The AIDS crisis created some political efforts to
streamline the approval process. However, these limited reforms were
targeted for AIDS drugs, not for the broader market. This has led to
the call for more robust and enduring reforms that would allow patients,
under the care of their doctors, access to drugs that have passed the
first round of clinical trials.
Post-marketing drug safety monitoring
The widely publicized recall of Vioxx, a non-steroidal anti-inflammatory drug (NSAID) now estimated to have contributed to fatal heart attacks
in thousands of Americans, played a strong role in driving a new wave
of safety reforms at both the FDA rulemaking and statutory levels. The
FDA approved Vioxx in 1999, and initially hoped it would be safer than
previous NSAIDs due to its reduced risk of intestinal tract bleeding.
However, a number of pre and post-marketing studies suggested that Vioxx
might increase the risk of myocardial infarction, and results from the
APPROVe trial in 2004 conclusively demonstrated this.
Faced with numerous lawsuits, the manufacturer voluntarily
withdrew it from the market. The example of Vioxx has been prominent in
an ongoing debate over whether new drugs should be evaluated on the
basis of their absolute safety, or their safety relative to existing
treatments for a given condition. In the wake of the Vioxx recall, there
were widespread calls by major newspapers, medical journals, consumer
advocacy organizations, lawmakers, and FDA officials for reforms in the FDA's procedures for pre- and post-market drug safety regulation.
In 2006, a Congressional committee was appointed by the Institute of Medicine
to review pharmaceutical safety regulation in the U.S. and to issue
recommendations for improvements. The committee was composed of 16
experts, including leaders in clinical medicine medical research,
economics, biostatistics, law, public policy, public health, and the allied health professions, as well as current and former executives from the pharmaceutical, hospital, and health insurance
industries. The authors found major deficiencies in the current FDA
system for ensuring the safety of drugs on the American market. Overall,
the authors called for an increase in the regulatory powers, funding,
and independence of the FDA.
Some of the committee's recommendations were incorporated into drafts
of the PDUFA IV amendment, which was signed into law as the Food and Drug Administration Amendments Act of 2007.
As of 2011, Risk Minimization Action Plans (RiskMAPS) have been
created to ensure risks of a drug never outweigh the benefits of that
drug within the post-marketing period. This program requires that
manufacturers design and implement periodic assessments of their
programs' effectiveness. The Risk Minimization Action Plans are set in
place depending on the overall level of risk a prescription drug is
likely to pose to the public.
Pediatric drug testing
Prior
to the 1990s, only 20% of all drugs prescribed for children in the
United States were tested for safety or efficacy in a pediatric
population. This became a major concern of pediatricians
as evidence accumulated that the physiological response of children to
many drugs differed significantly from those drugs' effects on adults.
Children react differently to the drugs because of many reasons,
including size, weight, etc. There were several reasons that few medical
trials were done with children. For many drugs, children represented
such a small proportion of the potential market, that drug manufacturers
did not see such testing as cost-effective.
Also, the belief that children are ethically restricted in their ability to give informed consent brought increased governmental and institutional hurdles to approval of these clinical trials, and greater concerns about legal liability.
Thus, for decades, most medicines prescribed to children in the U.S.
were done so in a non-FDA-approved, "off-label" manner, with dosages
"extrapolated" from adult data through body weight and body-surface-area
calculations.
In an initial FDA attempt to address this issue they produced the
1994 FDA Final Rule on Pediatric Labeling and Extrapolation, which
allowed manufacturers to add pediatric labeling information, but
required drugs that had not been tested for pediatric safety and
efficacy to bear a disclaimer to that effect. However, this rule failed
to motivate many drug companies to conduct additional pediatric drug
trials. In 1997, the FDA proposed a rule to require pediatric drug
trials from the sponsors of New Drug Applications. However, this new rule was successfully preempted in federal court as exceeding the FDA's statutory authority.
While this debate was unfolding, Congress used the Food and Drug Administration Modernization Act of 1997
to pass incentives that gave pharmaceutical manufacturers a six-month
patent term extension on new drugs submitted with pediatric trial data.
The Best Pharmaceuticals for Children Act of 2007 reauthorized these provisions and allowed the FDA to request NIH-sponsored
testing for pediatric drug testing, although these requests are subject
to NIH funding constraints. In the Pediatric Research Equity Act of
2003, Congress codified the FDA's authority to mandate
manufacturer-sponsored pediatric drug trials for certain drugs as a
"last resort" if incentives and publicly funded mechanisms proved
inadequate.
Priority review voucher (PRV)
The priority review voucher is a provision of the Food and Drug Administration Amendments Act of 2007, which awards a transferable "priority review voucher" to any company that obtains approval for a treatment for a neglected tropical diseases. The system was first proposed by Duke University faculty David Ridley, Henry Grabowski, and Jeffrey Moe in their 2006 Health Affairs paper: "Developing Drugs for Developing Countries". President Obama signed into law the Food and Drug Administration Safety and Innovation Act of 2012, which extended the authorization until 2017.
Rules for generic biologics
Since the 1990s, many successful new drugs for the treatment of cancer, autoimmune diseases, and other conditions have been protein-based biotechnology drugs, regulated by the Center for Biologics Evaluation and Research. Many of these drugs are extremely expensive; for example, the anti-cancer drug Avastin costs $55,000 for a year of treatment, while the enzyme replacement therapy drug Cerezyme costs $200,000 per year, and must be taken by Gaucher's disease patients for life.
Biotechnology drugs do not have the simple, readily verifiable
chemical structures of conventional drugs, and are produced through
complex, often proprietary, techniques, such as transgenic mammalian
cell cultures. Because of these complexities, the 1984 Hatch-Waxman Act did not include biologics in the Abbreviated New Drug Application
(ANDA) process. This precluded the possibility of generic drug
competition for biotechnology drugs. In February 2007, identical bills
were introduced into the House to create an ANDA process for the
approval of generic biologics, but were not passed.
Mobile medical applications
In 2013, a guidance was issued to regulate mobile medical applications
and protect users from their unintended use. This guidance
distinguishes the apps subjected to regulation based on the marketing
claims of the apps.
Incorporation of the guidelines during the development phase of these
apps has been proposed for expedited market entry and clearance.
Criticism
The FDA has regulatory oversight over a large array of products that affect the health and life of American citizens.
As a result, the FDA's powers and decisions are carefully monitored by
several governmental and non-governmental organizations. A $1.8 million 2006 Institute of Medicine
report on pharmaceutical regulation in the U.S. found major
deficiencies in the current FDA system for ensuring the safety of drugs
on the American market. Overall, the authors called for an increase in
the regulatory powers, funding, and independence of the FDA.
A 2022 article from Politico
raised concerns that food is not a high priority at the FDA. The report
explains the FDA has structural and leadership problems in the food
division and is often deferential to industry. This might be attributed to lobbying and influence of big food companies in Washington, D.C.
During the COVID-19 pandemic, the FDA received criticism for
punishing small distilleries that made hand sanitizers to help meet the
unexpected demand. After receiving $14,000 fines from the FDA, some
producers stated, "I wish we'd never done it. I will not put myself on
this same chopping block again."




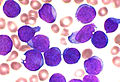
![Most common cancers in US males, by occurrence[20]](https://upload.wikimedia.org/wikipedia/commons/thumb/3/37/Most_common_cancers_-_male%2C_by_occurrence.png/360px-Most_common_cancers_-_male%2C_by_occurrence.png)
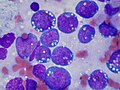
![in US males, by mortality[20]](https://upload.wikimedia.org/wikipedia/commons/thumb/a/a7/Most_common_cancers_-_male%2C_by_mortality.png/340px-Most_common_cancers_-_male%2C_by_mortality.png)
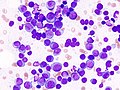
![in US females, by occurrence[20]](https://upload.wikimedia.org/wikipedia/commons/thumb/c/c5/Most_common_cancers_-_female%2C_by_occurrence.png/360px-Most_common_cancers_-_female%2C_by_occurrence.png)
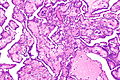
![in US females, by mortality[20]](https://upload.wikimedia.org/wikipedia/commons/thumb/a/a4/Most_common_cancers_-_female%2C_by_mortality.png/360px-Most_common_cancers_-_female%2C_by_mortality.png)