| Major depressive disorder | |
|---|---|
| Synonyms | Clinical depression, major depression, unipolar depression, unipolar disorder, recurrent depression |
 |
|
| Vincent van Gogh's 1890 painting Sorrowing old man ('At Eternity's Gate') |
|
| Specialty | Psychiatry |
| Symptoms | Low mood, low self-esteem, loss of interest in normally enjoyable activities, low energy, pain without a clear cause[1] |
| Complications | Suicide[2] |
| Usual onset | 20s–30s[3][4] |
| Duration | > 2 weeks[1] |
| Causes | Genetic, environmental, and psychological factors[1] |
| Risk factors | Family history, major life changes, certain medications, chronic health problems, substance abuse[1][3] |
| Differential diagnosis | Sadness[3] |
| Treatment | Counseling, antidepressant medication, electroconvulsive therapy[1] |
| Frequency | 216 million (2015)[5] |
Major depressive disorder (MDD), also known simply as depression, is a mental disorder characterized by at least two weeks of low mood that is present across most situations.[1] It is often accompanied by low self-esteem, loss of interest in normally enjoyable activities, low energy, and pain without a clear cause.[1] People may also occasionally have false beliefs or see or hear things that others cannot.[1] Some people have periods of depression separated by years in which they are normal, while others nearly always have symptoms present.[3] Major depressive disorder can negatively affect a person's personal, work, or school life as well as sleeping, eating habits, and general health.[1][3] Between 2–7% of adults with major depression die by suicide,[2] and up to 60% of people who die by suicide had depression or another mood disorder.[6]
The cause is believed to be a combination of genetic, environmental, and psychological factors.[1] Risk factors include a family history of the condition, major life changes, certain medications, chronic health problems, and substance abuse.[1][3] About 40% of the risk appears to be related to genetics.[3] The diagnosis of major depressive disorder is based on the person's reported experiences and a mental status examination.[7] There is no laboratory test for major depression.[3] Testing, however, may be done to rule out physical conditions that can cause similar symptoms.[7] Major depression should be differentiated from sadness, which is a normal part of life and is less severe.[3] The United States Preventive Services Task Force (USPSTF) recommends screening for depression among those over the age 12,[8][9] while a prior Cochrane review found that the routine use of screening questionnaires have little effect on detection or treatment.[10]
Typically, people are treated with counseling and antidepressant medication.[1] Medication appears to be effective, but the effect may only be significant in the most severely depressed.[11][12] It is unclear whether medications affect the risk of suicide.[13] Types of counseling used include cognitive behavioral therapy (CBT) and interpersonal therapy.[1][14] If other measures are not effective electroconvulsive therapy (ECT) may be tried.[1] Hospitalization may be necessary in cases with a risk of harm to self and may occasionally occur against a person's wishes.[15]
Major depressive disorder affected approximately 216 million people (3% of the world's population) in 2015.[5] The percentage of people who are affected at one point in their life varies from 7% in Japan to 21% in France.[4] Lifetime rates are higher in the developed world (15%) compared to the developing world (11%).[4] It causes the second most years lived with disability, after low back pain.[16] The most common time of onset is in a person's 20s and 30s.[3][4] Females are affected about twice as often as males.[3][4] The American Psychiatric Association added "major depressive disorder" to the Diagnostic and Statistical Manual of Mental Disorders (DSM-III) in 1980.[17] It was a split of the previous depressive neurosis in the DSM-II, which also encompassed the conditions now known as dysthymia and adjustment disorder with depressed mood.[17] Those currently or previously affected may be stigmatized.[18]
Signs and symptoms
An 1892 lithograph of a woman diagnosed with depression
Major depression significantly affects a person's family and personal relationships, work or school life, sleeping and eating habits, and general health.[19] Its impact on functioning and well-being has been compared to that of other chronic medical conditions such as diabetes.[20]
A person having a major depressive episode usually exhibits a very low mood, which pervades all aspects of life, and an inability to experience pleasure in activities that were formerly enjoyed. Depressed people may be preoccupied with, or ruminate over, thoughts and feelings of worthlessness, inappropriate guilt or regret, helplessness, hopelessness, and self-hatred.[21] In severe cases, depressed people may have symptoms of psychosis. These symptoms include delusions or, less commonly, hallucinations, usually unpleasant.[22] Other symptoms of depression include poor concentration and memory (especially in those with melancholic or psychotic features),[23] withdrawal from social situations and activities, reduced sex drive, irritability,[24] and thoughts of death or suicide. Insomnia is common among the depressed. In the typical pattern, a person wakes very early and cannot get back to sleep.[25] Hypersomnia, or oversleeping, can also happen.[25] Some antidepressants may also cause insomnia due to their stimulating effect.[26]
A depressed person may report multiple physical symptoms such as fatigue, headaches, or digestive problems; physical complaints are the most common presenting problem in developing countries, according to the World Health Organization's criteria for depression.[27] Appetite often decreases, with resulting weight loss, although increased appetite and weight gain occasionally occur.[21] Family and friends may notice that the person's behavior is either agitated or lethargic.[25] Older depressed people may have cognitive symptoms of recent onset, such as forgetfulness,[23] and a more noticeable slowing of movements.[28] Depression often coexists with physical disorders common among the elderly, such as stroke, other cardiovascular diseases, Parkinson's disease, and chronic obstructive pulmonary disease.[29]
Depressed children may often display an irritable mood rather than a depressed mood,[21] and show varying symptoms depending on age and situation.[30] Most lose interest in school and show a decline in academic performance. They may be described as clingy, demanding, dependent, or insecure.[25] Diagnosis may be delayed or missed when symptoms are interpreted as normal moodiness.[21]
Associated conditions
Major depression frequently co-occurs with other psychiatric problems. The 1990–92 National Comorbidity Survey (US) reports that half of those with major depression also have lifetime anxiety and its associated disorders such as generalized anxiety disorder.[31] Anxiety symptoms can have a major impact on the course of a depressive illness, with delayed recovery, increased risk of relapse, greater disability and increased suicide attempts.[32] There are increased rates of alcohol and drug abuse and particularly dependence,[33] and around a third of individuals diagnosed with ADHD develop comorbid depression.[34] Post-traumatic stress disorder and depression often co-occur.[19] Depression may also coexist with attention deficit hyperactivity disorder (ADHD), complicating the diagnosis and treatment of both.[35] Depression is also frequently comorbid with alcohol abuse and personality disorders.[36]Depression and pain often co-occur. One or more pain symptoms are present in 65% of depressed patients, and anywhere from 5 to 85% of patients with pain will be suffering from depression, depending on the setting; there is a lower prevalence in general practice, and higher in specialty clinics. The diagnosis of depression is often delayed or missed, and the outcome can worsen if the depression is noticed but completely misunderstood.[37]
Depression is also associated with a 1.5- to 2-fold increased risk of cardiovascular disease, independent of other known risk factors, and is itself linked directly or indirectly to risk factors such as smoking and obesity. People with major depression are less likely to follow medical recommendations for treating and preventing cardiovascular disorders, which further increases their risk of medical complications.[38] In addition, cardiologists may not recognize underlying depression that complicates a cardiovascular problem under their care.[39]
Cause
The cause of major depressive disorder is unknown. The biopsychosocial model proposes that biological, psychological, and social factors all play a role in causing depression.[3][40] The diathesis–stress model specifies that depression results when a preexisting vulnerability, or diathesis, is activated by stressful life events. The preexisting vulnerability can be either genetic,[41][42] implying an interaction between nature and nurture, or schematic, resulting from views of the world learned in childhood.[43]Childhood abuse, either physical, sexual or psychological, are all risk factors for depression, among other psychiatric issues that co-occur such as anxiety and drug abuse. Childhood trauma also correlates with severity of depression, lack of response to treatment and length of illness. However, some are more susceptible to developing mental illness such as depression after trauma, and various genes have been suggested to control susceptibility.[44]
Genetics
The 5-HTTLPR, or serotonin transporter promoter gene's short allele has been associated with increased risk of depression. However, since the 1990s results have been inconsistent, with three recent reviews finding an effect and two finding none.[41][45][46][47][48] Other genes that have been linked to a gene-environment interaction include CRHR1, FKBP5 and BDNF, the first two of which are related to the stress reaction of the HPA axis, and the latter of which is involved in neurogenesis.Other health problems
Depression may also come secondary to a chronic or terminal medical condition such as HIV/AIDS, or asthma and may be labeled "secondary depression".[49][50] It is unknown if the underlying diseases induce depression through effect on quality of life, of through shared etiologies (such as degeneration of the basal ganglia in parkinson's disease or immune dysregulation in asthma).[51] Depression may also be iatrogenic (the result of healthcare), such as drug induced depression. Therapies associated with depression include interferon therapy, beta-blockers, Isotretinoin, contraceptives,[52] cardiac agents, anticonvulsants, antimigraine drugs, antipsychotics, and hormonal agents agents such as gonadotropin-releasing hormone agonist.[53] Drug abuse in early age is also associated with increased risk of developing depression later in life.[54] Depression that occurs as a result of pregnancy is called postpartum depression, and is thought to be the result of hormonal changes associated with pregnancy.[55] Seasonal affective disorder, a type of depression associated with seasonal changes in sunlight, is thought to be the result of decreased sunlight.[56]Pathophysiology
The pathophysiology of depression is not yet understood, but the current theories center around monoaminergic systems, the circadian rhythm, immunological dysfunction, HPA axis dysfunction and structural or functional abnormalities of emotional circuits.The monoamine theory, derived from the efficacy of monoaminergic drugs in treating depression, was the dominant theory until recently. The theory postulates that insufficient activity of monoamine neurotransmitters is the primary cause of depression. Evidence for the monoamine theory comes from multiple areas. Firstly, acute depletion of tryptophan, a necessary precursor of serotonin, a monoamine, can cause depression in those in remission or relatives of depressed patients; this suggests that decreased serotonergic neurotransmission is important in depression.[57] Secondly, the correlation between depression risk and polymorphisms in the 5-HTTLPR gene, which codes for serotonin receptors, suggests a link. Third, decreased size of the locus coeruleus, decreased activity of tyrosine hydroxylase, increased density of alpha-2 adrenergic receptor, and evidence from rat models suggest decreased adrenergic neurotransmission in depression.[58] Furthermore, decreased levels of homovanillic acid, altered response to dextroamphetamine, responses of depressive symptoms to dopamine receptor agonists, decreased dopamine receptor D1 binding in the striatum,[59] and polymorphism of dopamine receptor genes implicate dopamine in depression.[60][61] Lastly, increased activity of monoamine oxidase, which degrades monoamines, has been associated with depression.[62] However, this theory is inconsistent with the fact that serotonin depletion does not cause depression in healthy persons, the fact that antidepressants instantly increase levels of monoamines but take weeks to work, and the existence of atypical antidepressants which can be effective despite not targeting this pathway.[63] One proposed explanation for the therapeutic lag, and further support for the deficiency of monoamines, is a desensitization of self-inhibition in raphe nuclei by the increased serotonin mediated by antidepressants.[64] However, disinhibition of the dorsal raphe has been proposed to occur as a result of decreased serotonergic activity in tryptophan depletion, resulting in a depressed state mediated by increased serotonin. Further countering the monoamine hypothesis is the fact that rats with lesions of the dorsal raphe are not more depressive that controls, the finding of increased jugular 5-HIAA in depressed patients that normalized with SSRI treatment, and the preference for carbohydrates in depressed patients.[65] Already limited, the monoamine hypothesis has been further oversimplified when presented to the general public.[66]
Immune system abnormalities have been observed, including increased levels of cytokines involved in generating sickness behavior (which shares overlap with depression).[67][68][69] The effectiveness of nonsteroidal anti-inflammatory drugs (NSAIDs) and cytokine inhibitors in treating depression,[70] and normalization of cytokine levels after successful treatment further suggest immune system abnormalities in depression.[71]
HPA axis abnormalities have been suggested in depression given the association of CRHR1 with depression and the increased frequency of dexamethasone test non-suppression in depressed patients. However, this abnormality is not adequate as a diagnosis tool, because its sensitivity is only 44%.[72][73] These stress-related abnormalities have been hypothesized to be the cause of hippocampal volume reductions seen in depressed patients.[74] Furthermore, a meta-analysis yielded decreased dexamethasone suppression, and increased response to psychological stressors.[75] Further abnormal results have been obscured with the cortisol awakening response, with increased response being associated with depression.[76]
Theories unifying neuroimaging findings have been proposed. The first model proposed is the "Limbic Cortical Model", which involves hyperactivity of the ventral paralimbic regions and hypoactivity of frontal regulatory regions in emotional processing.[77] Another model, the "Corito-Striatal model", suggests that abnormalities of the prefrontal cortex in regulating striatal and subcortical structures results in depression.[78] Another model proposes hyperactivity of salience structures in identifying negative stimuli, and hypoactivity of cortical regulatory structures resulting in a negative emotional bias and depression, consistent with emotional bias studies.[79]
Diagnosis
Clinical assessment
A diagnostic assessment may be conducted by a suitably trained general practitioner, or by a psychiatrist or psychologist,[19] who records the person's current circumstances, biographical history, current symptoms, and family history. The broad clinical aim is to formulate the relevant biological, psychological, and social factors that may be impacting on the individual's mood. The assessor may also discuss the person's current ways of regulating mood (healthy or otherwise) such as alcohol and drug use. The assessment also includes a mental state examination, which is an assessment of the person's current mood and thought content, in particular the presence of themes of hopelessness or pessimism, self-harm or suicide, and an absence of positive thoughts or plans.[19] Specialist mental health services are rare in rural areas, and thus diagnosis and management is left largely to primary-care clinicians.[80] This issue is even more marked in developing countries.[81] The mental health examination may include the use of a rating scale such as the Hamilton Rating Scale for Depression[82] or the Beck Depression Inventory[83] or the Suicide Behaviors Questionnaire-Revised.[84] The score on a rating scale alone is insufficient to diagnose depression to the satisfaction of the DSM or ICD, but it provides an indication of the severity of symptoms for a time period, so a person who scores above a given cut-off point can be more thoroughly evaluated for a depressive disorder diagnosis.[85] Several rating scales are used for this purpose.[85]Primary-care physicians and other non-psychiatrist physicians have more difficulty with underrecognition and undertreatment of depression compared to psychiatric physicians, in part because of the physical symptoms that often accompany depression, in addition to the many potential patient, provider, and system barriers that the authors describe. A review found that non-psychiatrist physicians miss about two-thirds of cases, though this has improved somewhat in more recent studies.[86]
Before diagnosing a major depressive disorder, in general a doctor performs a medical examination and selected investigations to rule out other causes of symptoms. These include blood tests measuring TSH and thyroxine to exclude hypothyroidism; basic electrolytes and serum calcium to rule out a metabolic disturbance; and a full blood count including ESR to rule out a systemic infection or chronic disease.[87] Adverse affective reactions to medications or alcohol misuse are often ruled out, as well. Testosterone levels may be evaluated to diagnose hypogonadism, a cause of depression in men.[88] Vitamin D levels might be evaluated, as low levels of vitamin D have been associated with greater risk for depression.[89]
Subjective cognitive complaints appear in older depressed people, but they can also be indicative of the onset of a dementing disorder, such as Alzheimer's disease.[90][91] Cognitive testing and brain imaging can help distinguish depression from dementia.[92] A CT scan can exclude brain pathology in those with psychotic, rapid-onset or otherwise unusual symptoms.[93] In general, investigations are not repeated for a subsequent episode unless there is a medical indication.
No biological tests confirm major depression.[94] Biomarkers of depression have been sought to provide an objective method of diagnosis. There are several potential biomarkers, including Brain-Derived Neurotrophic Factor and various functional MRI techniques. One study developed a decision tree model of interpreting a series of fMRI scans taken during various activities. In their subjects, the authors of that study were able to achieve a sensitivity of 80% and a specificity of 87%, corresponding to a negative predictive value of 98% and a positive predictive value of 32% (positive and negative likelihood ratios were 6.15, 0.23, respectively). However, much more research is needed before these tests could be used clinically.[95]
DSM-IV-TR and ICD-10 criteria
The most widely used criteria for diagnosing depressive conditions are found in the American Psychiatric Association's revised fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR), and the World Health Organization's International Statistical Classification of Diseases and Related Health Problems (ICD-10), which uses the name depressive episode for a single episode and recurrent depressive disorder for repeated episodes.[96] The latter system is typically used in European countries, while the former is used in the US and many other non-European nations,[97] and the authors of both have worked towards conforming one with the other.[98]Both DSM-IV-TR and ICD-10 mark out typical (main) depressive symptoms.[99] ICD-10 defines three typical depressive symptoms (depressed mood, anhedonia, and reduced energy), two of which should be present to determine depressive disorder diagnosis.[100][101] According to DSM-IV-TR, there are two main depressive symptoms—depressed mood and anhedonia. At least one of these must be present to make a diagnosis of major depressive episode.[102]
Major depressive disorder is classified as a mood disorder in DSM-IV-TR.[103] The diagnosis hinges on the presence of single or recurrent major depressive episodes.[21] Further qualifiers are used to classify both the episode itself and the course of the disorder. The category Depressive Disorder Not Otherwise Specified is diagnosed if the depressive episode's manifestation does not meet the criteria for a major depressive episode. The ICD-10 system does not use the term major depressive disorder but lists very similar criteria for the diagnosis of a depressive episode (mild, moderate or severe); the term recurrent may be added if there have been multiple episodes without mania.[96]
Major depressive episode
A major depressive episode is characterized by the presence of a severely depressed mood that persists for at least two weeks.[21] Episodes may be isolated or recurrent and are categorized as mild (few symptoms in excess of minimum criteria), moderate, or severe (marked impact on social or occupational functioning). An episode with psychotic features—commonly referred to as psychotic depression—is automatically rated as severe. If the patient has had an episode of mania or markedly elevated mood, a diagnosis of bipolar disorder is made instead.[104] Depression without mania is sometimes referred to as unipolar because the mood remains at one emotional state or "pole".[105] DSM-IV-TR excludes cases where the symptoms are a result of bereavement, although it is possible for normal bereavement to evolve into a depressive episode if the mood persists and the characteristic features of a major depressive episode develop.[106] The criteria have been criticized because they do not take into account any other aspects of the personal and social context in which depression can occur.[107] In addition, some studies have found little empirical support for the DSM-IV cut-off criteria, indicating they are a diagnostic convention imposed on a continuum of depressive symptoms of varying severity and duration:[108] Excluded are a range of related diagnoses, including dysthymia, which involves a chronic but milder mood disturbance;[109] recurrent brief depression, consisting of briefer depressive episodes;[110][111] minor depressive disorder, whereby only some symptoms of major depression are present;[112] and adjustment disorder with depressed mood, which denotes low mood resulting from a psychological response to an identifiable event or stressor.[113]Subtypes
The DSM-IV-TR recognizes five further subtypes of MDD, called specifiers, in addition to noting the length, severity and presence of psychotic features:- Melancholic depression is characterized by a loss of pleasure in most or all activities, a failure of reactivity to pleasurable stimuli, a quality of depressed mood more pronounced than that of grief or loss, a worsening of symptoms in the morning hours, early-morning waking, psychomotor retardation, excessive weight loss (not to be confused with anorexia nervosa), or excessive guilt.[114]
- Atypical depression is characterized by mood reactivity (paradoxical anhedonia) and positivity, significant weight gain or increased appetite (comfort eating), excessive sleep or sleepiness (hypersomnia), a sensation of heaviness in limbs known as leaden paralysis, and significant social impairment as a consequence of hypersensitivity to perceived interpersonal rejection.[115]
- Catatonic depression is a rare and severe form of major depression involving disturbances of motor behavior and other symptoms. Here, the person is mute and almost stuporous, and either remains immobile or exhibits purposeless or even bizarre movements. Catatonic symptoms also occur in schizophrenia or in manic episodes, or may be caused by neuroleptic malignant syndrome.[116]
- Postpartum depression, or mental and behavioral disorders associated with the puerperium, not elsewhere classified,[96] refers to the intense, sustained and sometimes disabling depression experienced by women after giving birth. Postpartum depression has an incidence rate of 10–15% among new mothers. The DSM-IV mandates that, in order to qualify as postpartum depression, onset occur within one month of delivery. It has been said that postpartum depression can last as long as three months.[117]
- Seasonal affective disorder (SAD) is a form of depression in which depressive episodes come on in the autumn or winter, and resolve in spring. The diagnosis is made if at least two episodes have occurred in colder months with none at other times, over a two-year period or longer.[118]
Screening
In 2016, the United States Preventive Services Task Force (USPSTF) recommended screening in the adult populations with evidence that it increases the detection of people with depression and with proper treatment improves outcomes.[8] They recommend screening in those between the age of 12 to 18 as well.[9]A Cochrane review from 2005 found screening programs do not significantly improve detection rates, treatment, or outcome.[10]
Differential diagnoses
To confirm major depressive disorder as the most likely diagnosis, other potential diagnoses must be considered, including dysthymia, adjustment disorder with depressed mood, or bipolar disorder. Dysthymia is a chronic, milder mood disturbance in which a person reports a low mood almost daily over a span of at least two years. The symptoms are not as severe as those for major depression, although people with dysthymia are vulnerable to secondary episodes of major depression (sometimes referred to as double depression).[109] Adjustment disorder with depressed mood is a mood disturbance appearing as a psychological response to an identifiable event or stressor, in which the resulting emotional or behavioral symptoms are significant but do not meet the criteria for a major depressive episode.[113] Bipolar disorder, also known as manic–depressive disorder, is a condition in which depressive phases alternate with periods of mania or hypomania. Although depression is currently categorized as a separate disorder, there is ongoing debate because individuals diagnosed with major depression often experience some hypomanic symptoms, indicating a mood disorder continuum.[119] Further differential diagnoses involve chronic fatigue syndrome.[120]Other disorders need to be ruled out before diagnosing major depressive disorder. They include depressions due to physical illness, medications, and substance abuse. Depression due to physical illness is diagnosed as a Mood disorder due to a general medical condition. This condition is determined based on history, laboratory findings, or physical examination. When the depression is caused by a medication, drug of abuse, or exposure to a toxin, it is then diagnosed as a specific mood disorder (previously called Substance-induced mood disorder in the DSM-IV-TR).[3]
Prevention
Preventative efforts may result in decreases in rates of the condition of between 22 and 38%.[121] Eating large amounts of fish may also reduce the risk.[122]Behavioral interventions, such as interpersonal therapy and cognitive-behavioral therapy, are effective at preventing new onset depression.[121][123][124] Because such interventions appear to be most effective when delivered to individuals or small groups, it has been suggested that they may be able to reach their large target audience most efficiently through the Internet.[125]
However, an earlier meta-analysis found preventive programs with a competence-enhancing component to be superior to behavior-oriented programs overall, and found behavioral programs to be particularly unhelpful for older people, for whom social support programs were uniquely beneficial. In addition, the programs that best prevented depression comprised more than eight sessions, each lasting between 60 and 90 minutes, were provided by a combination of lay and professional workers, had a high-quality research design, reported attrition rates, and had a well-defined intervention.[126]
The Netherlands mental health care system provides preventive interventions, such as the "Coping with Depression" course (CWD) for people with sub-threshold depression. The course is claimed to be the most successful of psychoeducational interventions for the treatment and prevention of depression (both for its adaptability to various populations and its results), with a risk reduction of 38% in major depression and an efficacy as a treatment comparing favorably to other psychotherapies.[123][127]
Management
The three most common treatments for depression are psychotherapy, medication, and electroconvulsive therapy. Psychotherapy is the treatment of choice (over medication) for people under 18. The UK National Institute for Health and Care Excellence (NICE) 2004 guidelines indicate that antidepressants should not be used for the initial treatment of mild depression, because the risk-benefit ratio is poor. The guidelines recommend that antidepressants treatment in combination with psychosocial interventions should be considered for:- People with a history of moderate or severe depression
- Those with mild depression that has been present for a long period
- As a second line treatment for mild depression that persists after other interventions
- As a first line treatment for moderate or severe depression.
American Psychiatric Association treatment guidelines recommend that initial treatment should be individually tailored based on factors including severity of symptoms, co-existing disorders, prior treatment experience, and patient preference. Options may include pharmacotherapy, psychotherapy, exercise, electroconvulsive therapy (ECT), transcranial magnetic stimulation (TMS) or light therapy. Antidepressant medication is recommended as an initial treatment choice in people with mild, moderate, or severe major depression, and should be given to all patients with severe depression unless ECT is planned.[129]
Treatment options are much more limited in developing countries, where access to mental health staff, medication, and psychotherapy is often difficult. Development of mental health services is minimal in many countries; depression is viewed as a phenomenon of the developed world despite evidence to the contrary, and not as an inherently life-threatening condition.[130] A 2014 Cochrane review found insufficient evidence to determine the effectiveness of psychological versus medical therapy in children.[131]
Lifestyle
Physical exercise is recommended for management of mild depression,[132] and has a moderate effect on symptoms.[133] Exercise has also been found to be effective for (unipolar) major depression.[134] It is equivalent to the use of medications or psychological therapies in most people.[133] In older people it does appear to decrease depression.[135] Exercise may be recommended to people who are willing, motivated, and physically healthy enough to participate in an exercise program as treatment.[134]There is a small amount of evidence that skipping a night's sleep may improve depressive symptoms, with the effects usually showing up within a day. This effect is usually temporary. Besides sleepiness, this method can cause a side effect of mania or hypomania.[136]
In observational studies smoking cessation has benefits in depression as large as or larger than those of medications.[137]
Besides exercise, sleep and diet may play a role in depression, and interventions in these areas may be an effective add-on to conventional methods.[138]
Counseling
Psychotherapy can be delivered to individuals, groups, or families by mental health professionals. A 2015 review found that cognitive behavioral therapy appears to be similar to antidepressant medication in terms of effect.[139] A 2012 review found psychotherapy to be better than no treatment but not other treatments.[140] With more complex and chronic forms of depression, a combination of medication and psychotherapy may be used.[141][142] A 2014 Cochrane review found that work-directed interventions combined with clinical interventions helped to reduce sick days taken by people with depression.[143] There is moderate-quality evidence that psychological therapies are a useful addition to standard antidepressant treatment of treatment-resistant depression in the short term.[144]Psychotherapy has been shown to be effective in older people.[145][146] Successful psychotherapy appears to reduce the recurrence of depression even after it has been terminated or replaced by occasional booster sessions.
Cognitive behavioral therapy
Cognitive behavioral therapy (CBT) currently has the most research evidence for the treatment of depression in children and adolescents, and CBT and interpersonal psychotherapy (IPT) are preferred therapies for adolescent depression.[147] In people under 18, according to the National Institute for Health and Clinical Excellence, medication should be offered only in conjunction with a psychological therapy, such as CBT, interpersonal therapy, or family therapy.[148] Cognitive behavioral therapy has also been shown to reduce the number of sick days taken by people with depression, when used in conjunction with primary care.[143]The most-studied form of psychotherapy for depression is CBT, which teaches clients to challenge self-defeating, but enduring ways of thinking (cognitions) and change counter-productive behaviors. Research beginning in the mid-1990s suggested that CBT could perform as well as or better than antidepressants in patients with moderate to severe depression.[149][150] CBT may be effective in depressed adolescents,[151] although its effects on severe episodes are not definitively known.[152] Several variables predict success for cognitive behavioral therapy in adolescents: higher levels of rational thoughts, less hopelessness, fewer negative thoughts, and fewer cognitive distortions.[153] CBT is particularly beneficial in preventing relapse.[154][155]
Cognitive behavioral therapy and occupational programs (including modification of work activities and assistance) have been shown to be effective in reducing sick days taken by workers with depression.[143]
Variants
Several variants of cognitive behavior therapy have been used in those with depression, the most notable being rational emotive behavior therapy,[156] and mindfulness-based cognitive therapy.[157] Mindfulness based stress reduction programs may reduce depression symptoms.[158][159] Mindfulness programs also appear to be a promising intervention in youth.[160]Psychoanalysis
Psychoanalysis is a school of thought, founded by Sigmund Freud, which emphasizes the resolution of unconscious mental conflicts.[161] Psychoanalytic techniques are used by some practitioners to treat clients presenting with major depression.[162] A more widely practiced therapy, called psychodynamic psychotherapy, is in the tradition of psychoanalysis but less intensive, meeting once or twice a week. It also tends to focus more on the person's immediate problems, and has an additional social and interpersonal focus.[163] In a meta-analysis of three controlled trials of Short Psychodynamic Supportive Psychotherapy, this modification was found to be as effective as medication for mild to moderate depression.[164]Antidepressants
Sertraline (Zoloft) is used primarily to treat major depression in adults.
Conflicting results have arisen from studies that look at the effectiveness of antidepressants in people with acute, mild to moderate depression.[165] Stronger evidence supports the usefulness of antidepressants in the treatment of depression that is chronic (dysthymia) or severe.
While small benefits were found, researchers Irving Kirsch and Thomas Moore state they may be due to issues with the trials rather than a true effect of the medication.[166] In a later publication, Kirsch concluded that the overall effect of new-generation antidepressant medication is below recommended criteria for clinical significance.[12] Similar results were obtained in a meta analysis by Fornier.[11]
A review commissioned by the National Institute for Health and Care Excellence concluded that there is strong evidence that SSRIs have greater efficacy than placebo on achieving a 50% reduction in depression scores in moderate and severe major depression, and that there is some evidence for a similar effect in mild depression.[167] Similarly, a Cochrane systematic review of clinical trials of the generic tricyclic antidepressant amitriptyline concluded that there is strong evidence that its efficacy is superior to placebo.[168]
In 2014 the U.S. FDA published a systematic review of all antidepressant maintenance trials submitted to the agency between 1985 and 2012. The authors concluded that maintenance treatment reduced the risk of relapse by 52% compared to placebo, and that this effect was primarily due to recurrent depression in the placebo group rather than a drug withdrawal effect.[11]
To find the most effective antidepressant medication with minimal side-effects, the dosages can be adjusted, and if necessary, combinations of different classes of antidepressants can be tried. Response rates to the first antidepressant administered range from 50–75%, and it can take at least six to eight weeks from the start of medication to remission.[129] Antidepressant medication treatment is usually continued for 16 to 20 weeks after remission, to minimize the chance of recurrence,[129] and even up to one year of continuation is recommended.[169] People with chronic depression may need to take medication indefinitely to avoid relapse.[19]
Selective serotonin reuptake inhibitors (SSRIs) are the primary medications prescribed, owing to their relatively mild side-effects, and because they are less toxic in overdose than other antidepressants.[170] People who do not respond to one SSRI can be switched to another antidepressant, and this results in improvement in almost 50% of cases.[171] Another option is to switch to the atypical antidepressant bupropion.[172] Venlafaxine, an antidepressant with a different mechanism of action, may be modestly more effective than SSRIs.[173] However, venlafaxine is not recommended in the UK as a first-line treatment because of evidence suggesting its risks may outweigh benefits,[174] and it is specifically discouraged in children and adolescents.[175][176]
For child and adolescent depression, fluoxetine is recommended if medication are used.[177] Fluoxetine; however, appears to have only slight benefit in children,[177][178] while other antidepressants have not been shown to be effective.[177] There is also insufficient evidence to determine effectiveness in those with depression complicated by dementia.[179] Any antidepressant can cause low serum sodium levels (also called hyponatremia);[180] nevertheless, it has been reported more often with SSRIs.[170] It is not uncommon for SSRIs to cause or worsen insomnia; the sedating antidepressant mirtazapine can be used in such cases.[181][182]
Irreversible monoamine oxidase inhibitors, an older class of antidepressants, have been plagued by potentially life-threatening dietary and drug interactions. They are still used only rarely, although newer and better-tolerated agents of this class have been developed.[183] The safety profile is different with reversible monoamine oxidase inhibitors such as moclobemide where the risk of serious dietary interactions is negligible and dietary restrictions are less strict.[184]
For children, adolescents, and probably young adults between 18 and 24 years old, there is a higher risk of both suicidal ideations and suicidal behavior in those treated with SSRIs.[185][186] For adults, it is unclear whether SSRIs affect the risk of suicidality. One review found no connection;[187] another an increased risk;[188] and a third no risk in those 25–65 years old and a decrease risk in those more than 65.[189] A black box warning was introduced in the United States in 2007 on SSRI and other antidepressant medications due to increased risk of suicide in patients younger than 24 years old.[190] Similar precautionary notice revisions were implemented by the Japanese Ministry of Health.[191]
Other medications
There is some evidence that omega-3 fatty acids fish oil supplements containing high levels of eicosapentaenoic acid (EPA) to docosahexaenoic acid (DHA) are effective in the treatment of, but not the prevention of major depression.[192] However, a Cochrane review determined there was insufficient high quality evidence to suggest Omega-3 fatty acids were effective in depression.[193] There is limited evidence that vitamin D supplementation is of value in alleviating the symptoms of depression in individuals who are vitamin D deficient.[194] There is some preliminary evidence that COX-2 inhibitors have a beneficial effect on major depression.[195] Lithium appears effective at lowering the risk of suicide in those with bipolar disorder and unipolar depression to nearly the same levels as the general population.[196] There is a narrow range of effective and safe dosages of lithium thus close monitoring may be needed.[197] Low-dose thyroid hormone may be added to existing antidepressants to treat persistent depression symptoms in people who have tried multiple courses of medication.[198] Limited evidence suggests stimulants such as amphetamine and modafinil may be effective in the short term, or as add on therapy.[199][200] Also, it is suggested that folate supplement may have a role in depression management.[201]Electroconvulsive therapy
Electroconvulsive therapy (ECT) is a standard psychiatric treatment in which seizures are electrically induced in patients to provide relief from psychiatric illnesses.[202]:1880 ECT is used with informed consent[203] as a last line of intervention for major depressive disorder.[204]A round of ECT is effective for about 50% of people with treatment-resistant major depressive disorder, whether it is unipolar or bipolar.[205] Follow-up treatment is still poorly studied, but about half of people who respond relapse within twelve months.[206]
Aside from effects in the brain, the general physical risks of ECT are similar to those of brief general anesthesia.[207]:259 Immediately following treatment, the most common adverse effects are confusion and memory loss.[204][208] ECT is considered one of the least harmful treatment options available for severely depressed pregnant women.[209]
A usual course of ECT involves multiple administrations, typically given two or three times per week until the patient is no longer suffering symptoms. ECT is administered under anesthetic with a muscle relaxant.[210] Electroconvulsive therapy can differ in its application in three ways: electrode placement, frequency of treatments, and the electrical waveform of the stimulus. These three forms of application have significant differences in both adverse side effects and symptom remission. After treatment, drug therapy is usually continued, and some patients receive maintenance ECT.[204]
ECT appears to work in the short term via an anticonvulsant effect mostly in the frontal lobes, and longer term via neurotrophic effects primarily in the medial temporal lobe.[211]
Transcranial magnetic stimulation
Transcranial magnetic stimulation (TMS) or deep transcranial magnetic stimulation is a noninvasive method used to stimulate small regions of the brain.[212] TMS was approved by the FDA for treatment-resistant major depressive disorder in 2008[213] and as of 2014 evidence supports that it is probably effective.[214] The American Psychiatric Association[215] the Canadian Network for Mood and Anxiety Disorders,[216] and the Royal Australia and New Zealand College of Psychiatrists have endorsed rTMS for trMDD.[217]Other
Bright light therapy reduces depression symptom severity, with benefit was found for both seasonal affective disorder and for nonseasonal depression, and an effect similar to those for conventional antidepressants. For non-seasonal depression, adding light therapy to the standard antidepressant treatment was not effective.[218] For non-seasonal depression where light was used mostly in combination with antidepressants or wake therapy a moderate effect was found, with response better than control treatment in high-quality studies, in studies that applied morning light treatment, and with people who respond to total or partial sleep deprivation.[219] Both analyses noted poor quality, short duration, and small size of most of the reviewed studies. There is insufficient evidence for Reiki[220] and dance movement therapy in depression.[221]Prognosis
Major depressive episodes often resolve over time whether or not they are treated. Outpatients on a waiting list show a 10–15% reduction in symptoms within a few months, with approximately 20% no longer meeting the full criteria for a depressive disorder.[222] The median duration of an episode has been estimated to be 23 weeks, with the highest rate of recovery in the first three months.[223]Studies have shown that 80% of those suffering from their first major depressive episode will suffer from at least 1 more during their life,[224] with a lifetime average of 4 episodes.[225] Other general population studies indicate that around half those who have an episode recover (whether treated or not) and remain well, while the other half will have at least one more, and around 15% of those experience chronic recurrence.[226] Studies recruiting from selective inpatient sources suggest lower recovery and higher chronicity, while studies of mostly outpatients show that nearly all recover, with a median episode duration of 11 months. Around 90% of those with severe or psychotic depression, most of whom also meet criteria for other mental disorders, experience recurrence.[227][228]
Recurrence is more likely if symptoms have not fully resolved with treatment. Current guidelines recommend continuing antidepressants for four to six months after remission to prevent relapse. Evidence from many randomized controlled trials indicates continuing antidepressant medications after recovery can reduce the chance of relapse by 70% (41% on placebo vs. 18% on antidepressant). The preventive effect probably lasts for at least the first 36 months of use.[229]
Those people experiencing repeated episodes of depression require ongoing treatment in order to prevent more severe, long-term depression. In some cases, people must take medications for long periods of time or for the rest of their lives.[230]
Cases when outcome is poor are associated with inappropriate treatment, severe initial symptoms that may include psychosis, early age of onset, more previous episodes, incomplete recovery after 1 year, pre-existing severe mental or medical disorder, and family dysfunction as well.[231]
Depressed individuals have a shorter life expectancy than those without depression, in part because depressed patients are at risk of dying by suicide.[232] However, they also have a higher rate of dying from other causes,[233] being more susceptible to medical conditions such as heart disease.[234] Up to 60% of people who die by suicide have a mood disorder such as major depression, and the risk is especially high if a person has a marked sense of hopelessness or has both depression and borderline personality disorder.[235] The lifetime risk of suicide associated with a diagnosis of major depression in the US is estimated at 3.4%, which averages two highly disparate figures of almost 7% for men and 1% for women[236] (although suicide attempts are more frequent in women).[237] The estimate is substantially lower than a previously accepted figure of 15%, which had been derived from older studies of hospitalized patients.[238]
Depression is often associated with unemployment and poverty.[239] Major depression is currently the leading cause of disease burden in North America and other high-income countries, and the fourth-leading cause worldwide. In the year 2030, it is predicted to be the second-leading cause of disease burden worldwide after HIV, according to the World Health Organization.[240] Delay or failure in seeking treatment after relapse, and the failure of health professionals to provide treatment, are two barriers to reducing disability.[241]
Epidemiology

Disability-adjusted life year for unipolar depressive disorders per 100,000 inhabitants in 2004.[242]
no data
<700 div="">
700–775
775–850
850–925
925–1000
1000–1075
1075–1150
1150–1225
1225–1300
1300–1375
1375–1450
>;1450
Major depressive disorder affects approximately 216 million people in 2015 (3% of the global population).[5] The percentage of people who are affected at one point in their life varies from 7% in Japan to 21% in France.[4] In most countries the number of people who have depression during their lives falls within an 8–18% range.[4] In North America, the probability of having a major depressive episode within a year-long period is 3–5% for males and 8–10% for females.[243][244] Major depression to be about twice as common in women as in men, although it is unclear why this is so, and whether factors unaccounted for are contributing to this.[245] The relative increase in occurrence is related to pubertal development rather than chronological age, reaches adult ratios between the ages of 15 and 18, and appears associated with psychosocial more than hormonal factors.[245] Depression is a major cause of disability worldwide.[246]
People are most likely to develop their first depressive episode between the ages of 30 and 40, and there is a second, smaller peak of incidence between ages 50 and 60.[247] The risk of major depression is increased with neurological conditions such as stroke, Parkinson's disease, or multiple sclerosis, and during the first year after childbirth.[248] It is also more common after cardiovascular illnesses, and is related more to a poor outcome than to a better one.[234][249] Studies conflict on the prevalence of depression in the elderly, but most data suggest there is a reduction in this age group.[250] Depressive disorders are more common to observe in urban than in rural population and the prevalence is in groups with stronger socioeconomic factors i.e. homelessness.[251]
History
Diagnoses of depression go back at least as far as Hippocrates
The Ancient Greek physician Hippocrates described a syndrome of melancholia as a distinct disease with particular mental and physical symptoms; he characterized all "fears and despondencies, if they last a long time" as being symptomatic of the ailment.[252] It was a similar but far broader concept than today's depression; prominence was given to a clustering of the symptoms of sadness, dejection, and despondency, and often fear, anger, delusions and obsessions were included.[253]
The term depression itself was derived from the Latin verb deprimere, "to press down".[254] From the 14th century, "to depress" meant to subjugate or to bring down in spirits. It was used in 1665 in English author Richard Baker's Chronicle to refer to someone having "a great depression of spirit", and by English author Samuel Johnson in a similar sense in 1753.[255] The term also came into use in physiology and economics. An early usage referring to a psychiatric symptom was by French psychiatrist Louis Delasiauve in 1856, and by the 1860s it was appearing in medical dictionaries to refer to a physiological and metaphorical lowering of emotional function.[256] Since Aristotle, melancholia had been associated with men of learning and intellectual brilliance, a hazard of contemplation and creativity. The newer concept abandoned these associations and through the 19th century, became more associated with women.[253]
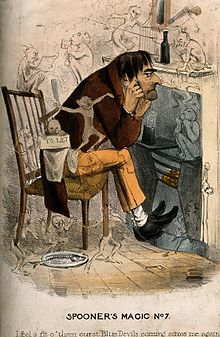
A historical caricature of a man with an approaching depression
Although melancholia remained the dominant diagnostic term, depression gained increasing currency in medical treatises and was a synonym by the end of the century; German psychiatrist Emil Kraepelin may have been the first to use it as the overarching term, referring to different kinds of melancholia as depressive states.[257]
Sigmund Freud likened the state of melancholia to mourning in his 1917 paper Mourning and Melancholia. He theorized that objective loss, such as the loss of a valued relationship through death or a romantic break-up, results in subjective loss as well; the depressed individual has identified with the object of affection through an unconscious, narcissistic process called the libidinal cathexis of the ego. Such loss results in severe melancholic symptoms more profound than mourning; not only is the outside world viewed negatively but the ego itself is compromised.[258] The patient's decline of self-perception is revealed in his belief of his own blame, inferiority, and unworthiness.[259] He also emphasized early life experiences as a predisposing factor.[253] Adolf Meyer put forward a mixed social and biological framework emphasizing reactions in the context of an individual's life, and argued that the term depression should be used instead of melancholia.[260] The first version of the DSM (DSM-I, 1952) contained depressive reaction and the DSM-II (1968) depressive neurosis, defined as an excessive reaction to internal conflict or an identifiable event, and also included a depressive type of manic-depressive psychosis within Major affective disorders.[261]
In the mid-20th century, researchers theorized that depression was caused by a chemical imbalance in neurotransmitters in the brain, a theory based on observations made in the 1950s of the effects of reserpine and isoniazid in altering monoamine neurotransmitter levels and affecting depressive symptoms.[262] The chemical imbalance theory has never been proven.[263]
The term "unipolar" (along with the related term "bipolar") was coined by the neurologist and psychiatrist Karl Kleist, and subsequently used by his disciples Edda Neele and Karl Leonhard.[264]
The term Major depressive disorder was introduced by a group of US clinicians in the mid-1970s as part of proposals for diagnostic criteria based on patterns of symptoms (called the "Research Diagnostic Criteria", building on earlier Feighner Criteria),[265] and was incorporated into the DSM-III in 1980.[266] To maintain consistency the ICD-10 used the same criteria, with only minor alterations, but using the DSM diagnostic threshold to mark a mild depressive episode, adding higher threshold categories for moderate and severe episodes.[99][266] The ancient idea of melancholia still survives in the notion of a melancholic subtype.
The new definitions of depression were widely accepted, albeit with some conflicting findings and views. There have been some continued empirically based arguments for a return to the diagnosis of melancholia.[267][268] There has been some criticism of the expansion of coverage of the diagnosis, related to the development and promotion of antidepressants and the biological model since the late 1950s.[269]
Society and culture
The 16th American president Abraham Lincoln had "melancholy", a condition that now may be referred to as clinical depression.[270]
Terminology
The term "depression" is used in a number of different ways. It is often used to mean this syndrome but may refer to other mood disorders or simply to a low mood. People's conceptualizations of depression vary widely, both within and among cultures. "Because of the lack of scientific certainty," one commentator has observed, "the debate over depression turns on questions of language. What we call it—'disease,' 'disorder,' 'state of mind'—affects how we view, diagnose, and treat it."[271] There are cultural differences in the extent to which serious depression is considered an illness requiring personal professional treatment, or is an indicator of something else, such as the need to address social or moral problems, the result of biological imbalances, or a reflection of individual differences in the understanding of distress that may reinforce feelings of powerlessness, and emotional struggle.[272][273]The diagnosis is less common in some countries, such as China. It has been argued that the Chinese traditionally deny or somatize emotional depression (although since the early 1980s, the Chinese denial of depression may have modified).[274] Alternatively, it may be that Western cultures reframe and elevate some expressions of human distress to disorder status. Australian professor Gordon Parker and others have argued that the Western concept of depression "medicalizes" sadness or misery.[275][276] Similarly, Hungarian-American psychiatrist Thomas Szasz and others argue that depression is a metaphorical illness that is inappropriately regarded as an actual disease.[277] There has also been concern that the DSM, as well as the field of descriptive psychiatry that employs it, tends to reify abstract phenomena such as depression, which may in fact be social constructs.[278] American archetypal psychologist James Hillman writes that depression can be healthy for the soul, insofar as "it brings refuge, limitation, focus, gravity, weight, and humble powerlessness."[279] Hillman argues that therapeutic attempts to eliminate depression echo the Christian theme of resurrection, but have the unfortunate effect of demonizing a soulful state of being.
Stigma
Historical figures were often reluctant to discuss or seek treatment for depression due to social stigma about the condition, or due to ignorance of diagnosis or treatments. Nevertheless, analysis or interpretation of letters, journals, artwork, writings, or statements of family and friends of some historical personalities has led to the presumption that they may have had some form of depression. People who may have had depression include English author Mary Shelley,[280] American-British writer Henry James,[281] and American president Abraham Lincoln.[282] Some well-known contemporary people with possible depression include Canadian songwriter Leonard Cohen[283] and American playwright and novelist Tennessee Williams.[284] Some pioneering psychologists, such as Americans William James[285][286] and John B. Watson,[287] dealt with their own depression.There has been a continuing discussion of whether neurological disorders and mood disorders may be linked to creativity, a discussion that goes back to Aristotelian times.[288][289] British literature gives many examples of reflections on depression.[290] English philosopher John Stuart Mill experienced a several-months-long period of what he called "a dull state of nerves", when one is "unsusceptible to enjoyment or pleasurable excitement; one of those moods when what is pleasure at other times, becomes insipid or indifferent". He quoted English poet Samuel Taylor Coleridge's "Dejection" as a perfect description of his case: "A grief without a pang, void, dark and drear, / A drowsy, stifled, unimpassioned grief, / Which finds no natural outlet or relief / In word, or sigh, or tear."[291][292] English writer Samuel Johnson used the term "the black dog" in the 1780s to describe his own depression,[293] and it was subsequently popularized by depression sufferer former British Prime Minister Sir Winston Churchill.[293]
Social stigma of major depression is widespread, and contact with mental health services reduces this only slightly. Public opinions on treatment differ markedly to those of health professionals; alternative treatments are held to be more helpful than pharmacological ones, which are viewed poorly.[294] In the UK, the Royal College of Psychiatrists and the Royal College of General Practitioners conducted a joint Five-year Defeat Depression campaign to educate and reduce stigma from 1992 to 1996;[295] a MORI study conducted afterwards showed a small positive change in public attitudes to depression and treatment.[296]
Research
Trials are looking at the effects of botulinum toxins on depression. The idea is that the drug is used to make the person look less frowning and that this stops the negative facial feedback from the face.[297] In 2015 it turned out, however, that the partly positive effects that had been observed until then could have been placebo effects.[298]MDD has been studied by taking MRI scans of patients with depression have revealed a number of differences in brain structure compared to those who are not depressed. Meta-analyses of neuroimaging studies in major depression reported that, compared to controls, depressed patients had increased volume of the lateral ventricles and adrenal gland and smaller volumes of the basal ganglia, thalamus, hippocampus, and frontal lobe (including the orbitofrontal cortex and gyrus rectus).[299][300] Hyperintensities have been associated with patients with a late age of onset, and have led to the development of the theory of vascular depression.[301]
Elderly
Depression is especially common among those over 65 years of age and increases in frequency with age beyond this age.[302] In addition the risk of depression increases in relation to the age and frailty of the individual.[302] Depression is one the most important factors which negatively impact quality of life in adults as well as the elderly.[302] Both symptoms and treatment among the elderly differ from those of the rest of the adult populations.[302]As with many other diseases it is common among the elderly not to present classical depressive symptoms.[302] Diagnosis and treatment is further complicated in that the elderly are often simultaneously treated with a number of other drugs, and often have other concurrent diseases.[302] Treatment differs in that studies of SSRI-drugs have shown lesser and often inadequate effect among the elderly, while other drugs with more clear effects have adverse effects which can be especially difficult to handle among the elderly.[302] Duloxetine is an SNRI-drug with documented effect on recurring depression among the elderly, but has adverse effects in form of dizziness, dryness of the mouth, diarrhea, and constipation.[302]
Problem solving therapy was as of 2015 the only psychological therapy with proven effect, and can be likened to a simpler form of cognitive behavioral therapy.[302] However, elderly with depression are seldom offered any psychological treatment, and the evidence surrounding which other treatments are effective is incomplete.[302] Electroconvulsive therapy (ECT or electric-shock therapy) has been used as treatment of the elderly, and register-studies suggest it is effective although less so among the elderly than among the rest of the adult population.[302]
The risks involved with treatment of depression among the elderly as opposed to benefits is not entirely clear.[302] Awaiting more evidence on how depression-treatment among the elderly is best designed it is important to follow up treatment results, and to reconsider changing treatments if it does not help.[302]