As a pill
As a capsule
As a tablet
As a softgel capsule used for fish oil or large amounts of vitamin E
As a shake and bottled powder
Production of cod liver oil, one of the first dietary supplement products manufactured in the 18th century
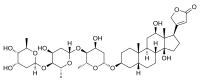
A dietary supplement is a manufactured product intended to supplement the diet when taken by mouth as a pill, capsule, tablet, or liquid. A supplement can provide nutrients
either extracted from food sources or synthetic, individually or in
combination, in order to increase the quantity of their consumption. The
class of nutrient compounds includes vitamins, minerals, fiber, fatty acids and amino acids.
Dietary supplements can also contain substances that have not been
confirmed as being essential to life, but are marketed as having a
beneficial biological effect, such as plant pigments or polyphenols. Animals can also be a source of supplement ingredients, as for example collagen
from chickens or fish. These are also sold individually and in
combination, and may be combined with nutrient ingredients. In the
United States and Canada, dietary supplements are considered a subset of
foods, and are regulated accordingly. The European Commission has also established harmonized rules to help insure that food supplements are safe and properly labeled. Among other countries, the definition of dietary supplements may vary as drugs or other classes of ingredients used in supplement products.
Creating an industry estimated to have a 2015 value of $37 billion, there are more than 50,000 dietary supplement products marketed just in the United States, where about 50% of the American adult population consumes dietary supplements. Multivitamins are the most commonly used product. For those who fail to consume a balanced diet, the United States National Institutes of Health states that certain supplements "may have value."
In the United States, it is against federal regulations for supplement manufacturers to claim
that these products prevent or treat any disease. Companies are allowed
to use what is referred to as "Structure/Function" wording if there is
substantiation of scientific evidence for a supplement providing a
potential health effect. An example would be "_____ helps maintain healthy joints", but the label must bear a disclaimer that the Food and Drug Administration
(FDA) "has not evaluated the claim and that the dietary supplement
product is not intended to "diagnose, treat, cure or prevent any
disease," because only a drug can legally make such a claim.
The FDA enforces these regulations, and also prohibits the sale of
supplements and supplement ingredients that are dangerous, or
supplements not made according to standardized good manufacturing practices (GMPs).
Definition
In the United States, the Dietary Supplement Health and Education Act
of 1994 provides this description: "The Dietary Supplement Health and
Education Act of 1994 (DSHEA) defines the term “dietary supplement” to
mean a product (other than tobacco) intended to supplement the diet that
bears or contains one or more of the following dietary ingredients: a
vitamin, a mineral, an herb or other botanical, an amino acid, a dietary
substance for use by man to supplement the diet by increasing the total
dietary intake, or a concentrate, metabolite, constituent, extract, or
combination of any of the aforementioned ingredients. Furthermore, a
dietary supplement must be labeled as a dietary supplement and be
intended for ingestion and must not be represented for use as
conventional food or as a sole item of a meal or of the diet. In
addition, a dietary supplement cannot be approved or authorized for
investigation as a new drug, antibiotic, or biologic, unless it was
marketed as a food or a dietary supplement before such approval or
authorization. Under DSHEA, dietary supplements are deemed to be food,
except for purposes of the drug definition."
Per DSHEA, dietary supplements are consumed orally, and are
mainly defined by what they are not: conventional foods (including meal
replacements), medical foods, preservatives or pharmaceutical drugs.
Products intended for use as a nasal spray, or topically, as a lotion
applied to the skin, do not qualify. FDA-approved drugs cannot be
ingredients in dietary supplements. Supplement products are or contain vitamins, nutritionally essential minerals, amino acids, essential fatty acids and non-nutrient substances extracted from plants or animals or fungi or bacteria, or in the instance of probiotics, are live bacteria. Dietary supplement ingredients may also be synthetic copies of naturally occurring substances (example: melatonin). All products with these ingredients are required to be labeled as dietary supplements.
Like foods and unlike drugs, no government approval is required to make
or sell dietary supplements; the manufacturer confirms the safety of
dietary supplements but the government does not; and rather than
requiring risk–benefit analysis to prove that the product can be sold
like a drug, such assessment is only used by the FDA to decide that a
dietary supplement is unsafe and should be removed from market.
Types
Vitamins
Pharmacies and supermarkets in the U.S. sell a large variety of vitamin dietary supplements
A vitamin is an organic compound required by an organism as a vital nutrient in limited amounts. An organic chemical compound (or related set of compounds) is called a vitamin when it cannot be synthesized
in sufficient quantities by an organism, and must be obtained from the
diet. The term is conditional both on the circumstances and on the
particular organism. For example, ascorbic acid
(vitamin C) is a vitamin for anthropoid primates, humans, guinea pigs
and bats, but not for other mammals. Vitamin D is not an essential
nutrient for people who get sufficient exposure to ultraviolet light,
either from the sun or an artificial source, as then they synthesize
vitamin D in skin.
Humans require thirteen vitamins in their diet, most of which are
actually groups of related molecules, "vitamers", (e.g. vitamin E
includes tocopherols and tocotrienols, vitamin K includes vitamin K1 and K2).
The list: vitamins A, C, D, E, K, Thiamine (B1), Riboflavin (B2),
Niacin (B3), Pantothenic Acid (B5), Vitamin B6, Biotin (B7), Folate (B9)
and Vitamin B12. Vitamin intake below recommended amounts can result in
signs and symptoms associated with vitamin deficiency. There is little
evidence of benefit when consumed as a dietary supplement by those who
are healthy and consuming a nutritionally adequate diet.
The U.S. Institute of Medicine sets Tolerable upper intake levels
(ULs) for some of the vitamins. This does not prevent dietary
supplement companies from selling products with content per serving
higher than the ULs. For example, the UL for vitamin D is 100 µg (4,000
IU), but products are available without prescription at 10,000 IU.
Dietary minerals
Minerals are the exogenous chemical elements indispensable for life. Four minerals: carbon, hydrogen, oxygen, and nitrogen,
are essential for life but are so ubiquitous in food and drink that
these are not considered nutrients and there are no recommended intakes
for these as minerals. The need for nitrogen is addressed by
requirements set for protein, which is composed of nitrogen-containing
amino acids. Sulfur
is essential, but for humans, not identified as having a recommended
intake per se. Instead, recommended intakes are identified for the
sulfur-containing amino acids methionine and cysteine. There are dietary
supplements which provide sulfur, such as taurine and methylsulfonylmethane.
The essential nutrient minerals for humans, listed in order by weight needed to be at the Recommended Dietary Allowance or Adequate Intake are potassium, chlorine, sodium, calcium, phosphorus, magnesium, iron, zinc, manganese, copper, iodine, chromium, molybdenum, selenium and cobalt (the last as a component of vitamin B12).
There are other minerals which are essential for some plants and
animals, but may or may not be essential for humans, such as boron and silicon.
Essential and purportedly essential minerals are marketed as dietary
supplements, individually and in combination with vitamins and other
minerals.
Although as a general rule, dietary supplement labeling and
marketing are not allowed to make disease prevention or treatment
claims, the U.S. FDA has for some foods and dietary supplements reviewed
the science, concluded that there is significant scientific agreement,
and published specifically worded allowed health claims. An initial
ruling allowing a health claim for calcium dietary supplements and
osteoporosis was later amended to include calcium supplements with or
without vitamin D, effective January 1, 2010. Examples of allowed
wording are shown below. In order to qualify for the calcium health
claim, a dietary supplement much contain at least 20% of the Reference
Dietary Intake, which for calcium means at least 260 mg/serving.
- "Adequate calcium throughout life, as part of a well-balanced diet, may reduce the risk of osteoporosis."
- "Adequate calcium as part of a healthful diet, along with physical activity, may reduce the risk of osteoporosis in later life."
- "Adequate calcium and vitamin D throughout life, as part of a well-balanced diet, may reduce the risk of osteoporosis."
- "Adequate calcium and vitamin D as part of a healthful diet, along with physical activity, may reduce the risk of osteoporosis in later life."
In the same year, the European Food Safety Authority also approved a
dietary supplement health claim for calcium and vitamin D and the
reduction of the risk of osteoporotic fractures by reducing bone loss.
The U.S. FDA also approved Qualified Health Claims (QHCs) for various
health conditions for calcium, selenium and chromium picolinate.
QHCs are supported by scientific evidence, but do not meet the more
rigorous “significant scientific agreement” standard required for an
authorized health claim. If dietary supplement companies choose to make
such a claim then the FDA stipulates the exact wording of the QHC to be
used on labels and in marketing materials. The wording can be onerous:
"One study suggests that selenium intake may reduce the risk of bladder
cancer in women. However, one smaller study showed no reduction in risk.
Based on these studies, FDA concludes that it is highly uncertain that
selenium supplements reduce the risk of bladder cancer in women."
Proteins and amino acids
Protein-containing supplements, either ready-to-drink or as powders
to be mixed into water, are marketed as aids to people recovering from
illness or injury, those hoping to thwart the sarcopenia of old age, to athletes who believe that strenuous physical activity increases protein requirements, to people hoping to lose weight while minimizing muscle loss, i.e., conducting a protein-sparing modified fast, and to people who want to increase muscle size for performance and appearance. Whey protein is a popular ingredient, but products may also incorporate casein, soy, pea, hemp or rice protein.
According to US & Canadian Dietary Reference Intake guidelines, the protein Recommended Dietary Allowance
(RDA) for adults is based on 0.8 grams protein per kilogram body
weight. The recommendation is for sedentary and lightly active people. Scientific reviews can conclude that a high protein diet, when combined with exercise, will increase muscle mass and strength, or conclude the opposite.
The International Olympic Committee recommends protein intake targets
for both strength and endurance athletes at about 1.2-1.8 g/kg body mass
per day.
One review proposed a maximum daily protein intake of approximately 25%
of energy requirements, i.e., approximately 2.0 to 2.5 g/kg.
The same protein ingredients marketed as dietary supplements can be incorporated into meal replacement and medical food
products, but those are regulated and labeled differently from
supplements. In the United States, "meal replacement" products are foods
and are labeled as such. These typically contain protein,
carbohydrates, fats, vitamins and minerals. There may be content claims
such as "good source of protein", "low fat" or "lactose free."
Medical foods, also nutritionally complete, are designed to be used
while a person is under the care of a physician or other licensed
healthcare professional. Liquid medical food products - example Ensure - are available in regular and high protein versions.
Proteins are chains of amino acids.
Nine of these proteinogenic amino acids are considered essential for
humans because they cannot be produced from other compounds by the human
body and so must be taken in as food. Recommended intakes, expressed as
milligrams per kilogram of body weight per day, have been established.
Other amino acids may be conditionally essential for certain ages or
medical conditions. Amino acids, individually and in combinations, are
sold as dietary supplements. The claim for supplementing with the branched chain amino acids
leucine, valine and isoleucine is for stimulating muscle protein
synthesis. A review of the literature concluded this claim was
unwarranted. In elderly people, supplementation with just leucine resulted in a modest (0.99 kg) increase in lean body mass. The non-essential amino acid arginine,
consumed in sufficient amounts, is thought to act as a donor for the
synthesis of nitric oxide, a vasodilator. A review confirmed blood
pressure lowering. Taurine,
a popular dietary supplement ingredient with claims made for sports
performance, is technically not an amino acid. It is synthesized in the
body from the amino acid cysteine.
Bodybuilding supplements
Bodybuilding supplements are dietary supplements commonly used by those involved in bodybuilding, weightlifting, mixed martial arts, and athletics for the purpose of facilitating an increase in lean body mass.
The intent is to increase muscle, increase body weight, improve
athletic performance, and for some sports, to simultaneously decrease
percent body fat so as to create better muscle definition. Among the
most widely used are high protein drinks, branched-chain amino acids (BCAA), glutamine, arginine, essential fatty acids, creatine, HMB, and weight loss products.
Supplements are sold either as single ingredient preparations or in the
form of "stacks" – proprietary blends of various supplements marketed
as offering synergistic advantages. While many bodybuilding supplements
are also consumed by the general public the frequency of use will differ
when used specifically by bodybuilders. One meta-analysis concluded
that for athletes participating in resistance exercise training and
consuming protein supplements for an average of 13 weeks, total protein
intake up to 1.6 g/kg of body weight
per day would result in an increase in strength and fat-free mass, i.e.
muscle, but that higher intakes would not further contribute. The muscle mass increase was statistically significant but modest - averaging 0.3 kg for all trials and 1.0–2.0 kg, for protein intake ≥1.6 g/kg/day.
As of 2010, annual sales of sport nutrition products in the United States was over US$2.7 billion according to a publication by Consumer Reports.
Essential fatty acids
Fish oil is a commonly used fatty acid supplement because it is a source of omega-3 fatty acids.
Fatty acids are strings of carbon atoms, having a range of lengths. If
links are all single (C-C), then the fatty acid is called saturated; with one double bond (C=C), it is called monounsaturated; if there are two or more double bonds (C=C=C), it is called polyunsaturated.
Only two fatty acids, both polyunsaturated, are considered essential to
be obtained from the diet, as the others are synthesized in the body.
The "essential" fatty acids are alpha-linolenic acid (ALA), an omega-3 fatty acid, and linoleic acid (LA), an omega-6 fatty acid. ALA can be elongated in the body to create other omega-3 fatty acids: eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA).
Plant oils, particularly seed and nut oils, contain ALA. Food sources of EPA and DHA are oceanic fish, whereas dietary supplement sources include fish oil, krill oil and marine algae extracts. The European Food Safety Authority
(EFSA) identifies 250 mg/day for a combined total of EPA and DHA as
Adequate Intake, with a recommendation that women pregnant or lactating
consume an additional 100 to 200 mg/day of DHA. In the United States and Canada are Adequate Intakes for ALA and LA over various stages of life, but there are no intake levels specified for EPA and/or DHA.
Supplementation with EPA and/or DHA does not appear to affect the risk of death, cancer or heart disease. Furthermore, studies of fish oil supplements have failed to support claims of preventing heart attacks or strokes.
In 2017, the American Heart Association issued a science advisory
stating that it could not recommend use of omega-3 fish oil supplements
for primary prevention of cardiovascular disease or stroke, although it reaffirmed supplementation for people who have a history of coronary heart disease.
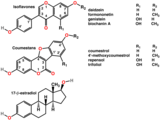
Natural products
St. John's wort petals used in natural product supplements
Dietary supplements can be manufactured using intact sources or extracts from plants, animals, algae, fungi or lichens, including such examples as ginkgo biloba, curcumin, cranberry, St. John’s wort, ginseng, resveratrol, glucosamine and collagen. Products bearing promotional claims of health benefits are sold without requiring a prescription in pharmacies, supermarkets, specialist shops, military commissaries, buyers clubs, direct selling organizations, and the internet. While most of these products have a long history of use in herbalism and various forms of traditional medicine, concerns exist about their actual efficacy, safety and consistency of quality.
Canada has published a manufacturer and consumer guide describing
quality, licensing, standards, identities, and common contaminants of
natural products. In 2016, sales of herbal supplements just in the United States were $7.5 billion, with the market growing at about 8% per year. Italy, Germany and Eastern European countries were leading consumers of botanical supplements in 2016, with European Union market growth forecast to be $8.7 billion by 2020.
Probiotics
In humans, the large intestine is host to more than 1,000 species of
microorganisms, mostly bacteria, numbering in the tens of trillions. "Probiotic"
in the context of dietary supplements is the theory that by orally
consuming specific live bacteria (or yeast) species, it is possible to
influence the large intestine microbiota,
with consequent health benefits. Although there are numerous claimed
benefits of using probiotic supplements, such as maintaining gastrointestinal health, in part by lowering risk of and severity of constipation or diarrhea, and improving immune health, including lower risk of and severity of acute upper respiratory tract infections, i.e., the common cold, such claims are not all supported by sufficient clinical evidence.
A review based on interviews with dozens of experts in microbiome
research expressed concern about "...how biomedical research is co-opted
by commercial entities that place profit over health."
The concern is timely, as through 2021, probiotic supplements are
expected to be the fastest growing segment of the dietary supplement
market worldwide, while at the same time, the global health benefits
market for probiotic-containing yogurt (a food, not a dietary
supplement) is declining.
As with all dietary supplements, in the United States
inappropriate label health claims such as preventing or treating disease
are opposed by the FDA and deceptive advertisements by the Federal Trade Commission.
Probiotic foods and dietary supplements are allowed to make claims
using Structure:Function vocabulary as long as human trial evidence is
adequate. In 2005, the FDA issued a Warning Letter to UAS Laboratories
for disease treatment claims (colds, flu, ulcers, elevated blood
cholesterol, colon cancer...). The company revised label and website
content and continued to sell the product. In 2011 the company was found to have resumed the label and website claims, and the FDA seized product and stopped production.
In 2010 a FTC action was brought against a probiotic food company for
exaggerated health claims, resulting in a multimillion-dollar fine and
revisions to future advertising. In the European Union a more restrictive approach has been taken by the EFSA.
All proposed health claims were rejected on the grounds that the
science was not sufficient, and no health claims are permitted. Foods
with live microorganisms (yogurt, kefir) can be sold, but without
claims.
Probiotic supplements are generally regarded as safe. The
greatest concern, evidenced by reviews reporting on case studies, is
that for people with compromised gut wall integrity there may be a risk
of systemic infection. For this reason, probiotic research is expected
to exclude bacteria species that are antibiotic resistant.
Industry
In 2015, the American market for dietary supplements was valued at $37 billion, with the economic impact in the United States for 2016 estimated at $122 billion, including employment wages and taxes. One 2016 analysis estimated the total market for dietary supplements could reach $278 billion worldwide by 2024.
Controversy
Adulteration
Over the period 2008 to 2011, the Government Accountability Office (GAO) of the United States received 6,307 reports of health problems (identified as adverse events)
from use of dietary supplements containing a combination of ingredients
in manufactured vitamins, minerals or other supplement products, with 92% of tested herbal supplements containing lead and 80% containing other chemical contaminants. Using undercover
staff, the GAO also found that supplement retailers intentionally
engaged in "unequivocal deception" to sell products advertised with
baseless health claims, particularly to elderly consumers. Consumer Reports also reported unsafe levels of arsenic, cadmium, lead and mercury in several protein powder products. The Canadian Broadcasting Corporation (CBC) reported that protein spiking, i.e., the addition of amino acids to manipulate protein content analysis, was common. Many of the companies involved challenged CBC's claim.
A 2013 study on herbal supplements found that many products were
of low quality, one third did not contain the active ingredient(s)
claimed, and one third contained unlisted substances. In a genetic analysis of herbal supplements, 78% of samples contained animal DNA that was not identified as an ingredient on the product labels.
In some botanical products, undeclared ingredients were used to
increase the bulk of the product and reduce its cost of manufacturing,
while potentially violating certain religious and/or cultural
limitations on consuming animal ingredients, such as cow, buffalo or
deer. In 2015, the New York Attorney General
identified four major retailers with dietary supplement products that
contained fraudulent and potentially dangerous ingredients, requiring
the companies to remove the products from retail stores.
A study of dietary supplements sold between 2007 and 2016 identified 776 that contained unlisted pharmaceutical drugs, many of which could interact with other medications and lead to hospitalization. 86% of the adulterated supplements were marketed for weight loss and sexual performance, with many containing prescription erectile dysfunction medication. Muscle building supplements were contaminated with anabolic steroids, and multiple products contained antidepressants and antihistamines. Despite these findings, fewer than half of the adulterated supplements were recalled.
Litigation against false health claims
The United States Food and Drug Administration, Office of
Inspections, Compliance, Enforcement, and Criminal Investigations,
monitors supplement products for accuracy in advertising and labeling,
and when finding violations, warns manufacturers of impending enforcement action, including search and seizure, injunction, and/or financial penalties, such as for a Maine supplement company in 2017. The United States Federal Trade Commission, which litigates against deceptive advertising, established a consumer center to assist reports of false health claims in product advertising for dietary supplements, and, in 2017, successfully sued nine manufacturers for deceptive advertising of dietary supplements.
Adverse effects
In the United States, manufacturers of dietary supplements are
required to demonstrate safety of their products before approval is
granted for commerce. Despite this caution, numerous adverse effects have been reported, including muscle cramps, hair loss, joint pain, liver disease, and allergic reactions, with 29% of the adverse effects resulting in hospitalization, and 20% in serious injuries or illnesses.
By more than five-fold, the highest incidence of health problems
derived from "combination products", whereas supplements for vitamins
and minerals, lipid products, and herbal products were less likely to
cause adverse effects.
Among general reasons for the possible harmful effects of dietary
supplements are: a) absorption in a short time, b) manufacturing
quality and contamination, and c) enhancing both positive and negative
effects at the same time. The incidence of liver injury
from herbal and dietary supplements is about 16–20% of all supplement
products causing injury, with the occurrence growing globally over the
early 21st century. The most common liver injuries from weight loss and bodybuilding supplements involve hepatocellular damage with resulting jaundice, and the most common supplement ingredients attributed to these injuries are green tea catechins, anabolic steroids, and the herbal extract, aegeline. Weight loss supplements have also had adverse psychiatric effects.
Society and culture
Public health
Work done by scientists in the early 20th century on identifying
individual nutrients in food and developing ways to manufacture them
raised hopes that optimal health could be achieved and diseases
prevented by adding them to food and providing people with dietary
supplements; while there were successes in preventing vitamin deficiencies, and preventing conditions like neural tube defects by supplementation and food fortification with folic acid,
no targeted supplementation or fortification strategies to prevent
major diseases like cancer or cardiovascular diseases have proved
successful.
For example, while increased consumption of fruits and vegetables
are related to decreases in mortality, cardiovascular diseases and
cancers, supplementation with key factors found in fruits and vegetable,
like antioxidants, vitamins, or minerals, do not help and some have been found to be harmful in some cases.
In general as of 2016, robust clinical data is lacking, that shows
that any kind of dietary supplementation does more good than harm for
people who are healthy and eating a reasonable diet but there is clear
data showing that dietary pattern and lifestyle choices are associated
with health outcomes.
As a result of the lack of good data for supplementation and the
strong data for dietary pattern, public health recommendations for healthy eating urge people to eat a plant-based diet of whole foods, minimizing processed food, salt and sugar and to get exercise daily, and to abandon Western pattern diets and a sedentary lifestyle.
Legal regulation
United States
The regulation of food and dietary supplements by the U.S. Food and
Drug Administration is governed by various statutes enacted by the United States Congress and interpreted by the U.S. Food and Drug Administration ("FDA"). Pursuant to the Federal Food, Drug, and Cosmetic Act ("the Act") and accompanying legislation, the FDA has authority to oversee the quality of substances sold as food in the United States, and to monitor claims made in the labeling about both the composition and the health benefits of foods.
Substances which the FDA regulates as food are subdivided into various categories, including foods, food additives,
added substances (man-made substances which are not intentionally
introduced into food, but nevertheless end up in it), and dietary
supplements. The specific standards which the FDA exercises differ from
one category to the next. Furthermore, the FDA has been granted a
variety of means by which it can address violations of the standards for
a given category of substances.
Dietary supplement manufacture is required to comply with the
good manufacturing practices established in 2007. The FDA can visit
manufacturing facilities, send Warning Letters if not in compliance with GMPs, stop production, and if there is a health risk, require that the company conduct a recall.
European Union
The European Union's (EU) Food Supplements Directive of 2002 requires that supplements be demonstrated to be safe, both in dosages and in purity.
Only those supplements that have been proven to be safe may be sold in
the EU without prescription. As a category of food, food supplements
cannot be labeled with drug claims but can bear health claims and nutrition claims.
The dietary supplements industry in the United Kingdom
(UK), one of the 28 countries in the bloc, strongly opposed the
Directive. In addition, a large number of consumers throughout Europe,
including over one million in the UK, and various doctors and
scientists, had signed petitions by 2005 against what are viewed by the
petitioners as unjustified restrictions of consumer choice. In 2004, along with two British trade associations, the Alliance for Natural Health (ANH) had a legal challenge to the Food Supplements Directive referred to the European Court of Justice by the High Court in London.
Although the European Court of Justice's Advocate General
subsequently said that the bloc's plan to tighten rules on the sale of vitamins and food supplements should be scrapped,
he was eventually overruled by the European Court, which decided that
the measures in question were necessary and appropriate for the purpose
of protecting public health.
ANH, however, interpreted the ban as applying only to synthetically
produced supplements, and not to vitamins and minerals normally found in
or consumed as part of the diet.
Nevertheless, the European judges acknowledged the Advocate General's
concerns, stating that there must be clear procedures to allow
substances to be added to the permitted list based on scientific
evidence. They also said that any refusal to add the product to the list
must be open to challenge in the courts.
Research
Examples of ongoing government research organizations to better
understand the potential health properties and safety of dietary
supplements are the European Food Safety Authority, the Office of Dietary Supplements of the United States National Institutes of Health, the Natural and Non-prescription Health Products Directorate of Canada, and the Therapeutic Goods Administration of Australia. Together with public and private research groups, these agencies construct databases
on supplement properties, perform research on quality, safety, and
population trends of supplement use, and evaluate the potential clinical
efficacy of supplements for maintaining health or lowering disease
risk.
Databases
As continual research on the properties of supplements accumulates,
databases or fact sheets for various supplements are updated regularly,
including the Dietary Supplement Label Database, Dietary Supplement Ingredient Database, and Dietary Supplement Facts Sheets of the United States.
In Canada where a license is issued when a supplement product has been
proven by the manufacturer and government to be safe, effective and of
sufficient quality for its recommended use, an eight-digit Natural
Product Number is assigned and recorded in a Licensed Natural Health
Products Database. The European Food Safety Authority maintains a compendium of botanical ingredients used in manufacturing of dietary supplements.
In 2015, the Australian Government's Department of Health published the results of a review of herbal supplements to determine if any were suitable for coverage by health insurance. Establishing guidelines to assess safety and efficacy of botanical supplement products, the European Medicines Agency provided criteria for evaluating and grading the quality of clinical research in preparing monographs about herbal supplements. In the United States, the National Center for Complementary and Integrative Health of the National Institutes of Health provides fact sheets evaluating the safety, potential effectiveness and side effects of many botanical products.
Quality and safety
To assure supplements have sufficient quality, standardization, and
safety for public consumption, research efforts have focused on
development of reference materials for supplement manufacturing and
monitoring. High-dose products have received research attention, especially for emergency situations such as vitamin A deficiency in malnutrition of children, and for women taking folate supplements to reduce the risk of breast cancer.
Population monitoring
In the United States, the National Health and Nutrition Examination Survey
(NHANES) has investigated habits of using dietary supplements in
context of total nutrient intakes from the diet in adults and children.
Over the period of 1999 to 2012, use of multivitamins decreased, and
there was wide variability in the use of individual supplements among
subgroups by age, sex, race/ethnicity, and educational status. Particular attention has been given to use of folate supplements by young women to reduce the risk of fetal neural tube defects.
Clinical studies
Research initiatives to improve knowledge of the possible health
benefits of supplementing with essential nutrients to lower disease risk
have been extensive. As examples, just in 2017 were reviews on
- vitamin D, providing evidence for protection against acute respiratory tract infections
- iron, to deter maternal iron deficiency anemia and adverse effects on the fetus
- folate, to lower the risk of stroke and cardiovascular disease
- multiple supplements for which there was no evidence of benefit to lower risk of death, cardiovascular disease or cancer
A 2017 review indicated a rising incidence of liver injury from use
of herbal and dietary supplements, particularly those with steroids,
green tea extract, or multiple ingredients.
Absence of benefit
The potential benefit of using essential nutrient dietary supplements
to lower the risk of diseases has been refuted by findings of no effect
or weak evidence in numerous clinical reviews, such as for
cardiovascular diseases, cancer, HIV, or tuberculosis.
Reporting bias
A review of clinical trials registered at clinicaltrials.gov,
which would include both drugs and supplements, reported that nearly
half of completed trials were sponsored wholly or partially by industry.
This does not automatically imply bias, but there is evidence that
because of selective non-reporting, results in support of a potential
drug or supplement ingredient are more likely to be published than
results that do not demonstrate a statistically significant benefit. One review reported that fewer than half of the registered clinical trials resulted in publication in peer-reviewed journals.
Future
Improving public information about use of dietary supplements
involves investments in professional training programs, further studies
of population and nutrient needs, expanding the database information,
enhancing collaborations between governments and universities, and
translating dietary supplement research into useful information for
consumers, health professionals, scientists, and policymakers. Future demonstration of efficacy from use of dietary supplements requires high-quality clinical research using rigorously-qualified products and compliance with established guidelines for reporting of clinical trial results (e.g., CONSORT guidelines).