| Hydrocephalus | |
|---|---|
| Other names | Water on the brain |
 | |
| Hydrocephalus as seen on a CT scan of the brain. The black areas in the middle of the brain (the lateral ventricles) are abnormally large and filled with fluid. | |
| Pronunciation |
|
| Specialty | Neurosurgery |
| Symptoms | Babies: rapid head growth, vomiting, sleepiness, seizures Older people: Headaches, double vision, poor balance, urinary incontinence, personality changes, mental impairment |
| Causes | Neural tube defects, meningitis, brain tumors, traumatic brain injury, intraventricular hemorrhage |
| Diagnostic method | Based on symptoms and medical imaging |
| Treatment | Surgery |
| Prognosis | Variable, often normal life |
| Frequency | 1.5 per 1,000 (babies) |
Hydrocephalus is a condition in which an accumulation of cerebrospinal fluid (CSF) occurs within the brain. This typically causes increased pressure inside the skull. Older people may have headaches, double vision, poor balance, urinary incontinence, personality changes, or mental impairment. In babies, it may be seen as a rapid increase in head size. Other symptoms may include vomiting, sleepiness, seizures, and downward pointing of the eyes.
Hydrocephalus can occur due to birth defects or be acquired later in life. Associated birth defects include neural tube defects and those that result in aqueductal stenosis. Other causes include meningitis, brain tumors, traumatic brain injury, intraventricular hemorrhage, and subarachnoid hemorrhage. The four types of hydrocephalus are communicating, noncommunicating, ex vacuo, and normal pressure. Diagnosis is typically made by physical examination and medical imaging.
Hydrocephalus is typically treated by the surgical placement of a shunt system. A procedure called a third ventriculostomy may be an option in a few people. Complications from shunts may include overdrainage, underdrainage, mechanical failure, infection, or obstruction. This may require replacement. Outcomes are variable, but many people with shunts live normal lives. Without treatment, death or permanent disability may occur.
About one to two per 1,000 newborns have hydrocephalus. Rates in the developing world may be higher. Normal pressure hydrocephalus is estimated to affect about 5 per 100,000 people, with rates increasing with age. Description of hydrocephalus by Hippocrates dates back more than 2,000 years. The word "hydrocephalus" is from the Greek ὕδωρ, hydōr, meaning "water" and κεφαλή, kephalē, meaning "head".
Signs and symptoms
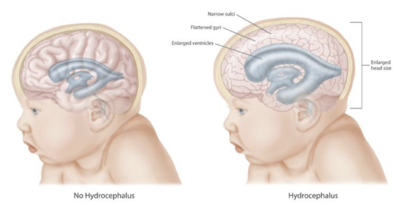
Illustration showing different effects of hydrocephalus on the brain and cranium
The clinical presentation of hydrocephalus varies with chronicity. Acute dilatation of the ventricular system
is more likely to manifest with the nonspecific signs and symptoms of
increased intracranial pressure (ICP). By contrast, chronic dilatation
(especially in the elderly population) may have a more insidious onset
presenting, for instance, with Hakim's triad (Adams' triad).
Symptoms of increased ICP may include headaches, vomiting, nausea, papilledema, sleepiness, or coma. Elevated ICP may result in uncal or tonsillar herniation, with resulting life-threatening brain stem compression.
Hakim's triad of gait instability, urinary incontinence, and dementia is a relatively typical manifestation of the distinct entity normal-pressure hydrocephalus. Focal neurological deficits may also occur, such as abducens nerve palsy and vertical gaze palsy (Parinaud syndrome due to compression of the quadrigeminal plate, where the neural centers coordinating the conjugated vertical eye movement are located). The symptoms depend on the cause of the blockage, the person's age, and how much brain tissue has been damaged by the swelling.
In infants with hydrocephalus, CSF builds up in the central nervous system (CNS), causing the fontanelle (soft spot) to bulge and the head to be larger than expected. Early symptoms may also include:
- Eyes that appear to gaze downward
- Irritability
- Seizures
- Separated sutures
- Sleepiness
- Vomiting
Symptoms that may occur in older children can include:
- Brief, shrill, high-pitched cry
- Changes in personality, memory, or the ability to reason or think
- Changes in facial appearance and eye spacing (craniofacial disproportion)
- Crossed eyes or uncontrolled eye movements
- Difficulty feeding
- Excessive sleepiness
- Headaches
- Irritability, poor temper control
- Loss of bladder control (urinary incontinence)
- Loss of coordination and trouble walking
- Muscle spasticity (spasm)
- Slow growth (child 0–5 years)
- Delayed milestones
- Failure to thrive
- Slow or restricted movement
- Vomiting
Because hydrocephalus can injure the brain, thought and behavior may be adversely affected. Learning disabilities, including short-term memory loss,
are common among those with hydrocephalus, who tend to score better on
verbal IQ than on performance IQ, which is thought to reflect the
distribution of nerve damage to the brain.
However, the severity of hydrocephalus can differ considerably between
individuals, and some are of average or above-average intelligence.
Someone with hydrocephalus may have coordination and visual problems, or
clumsiness. They may reach puberty earlier than the average child (this
is called precocious puberty). About one in four develops epilepsy.
Cause
Congenital
A one-year-old girl with hydrocephalus showing "sunset eyes", before shunt surgery
Congenital hydrocephalus is present in the infant prior to birth, meaning the fetus developed hydrocephalus in utero during fetal development.
The most common cause of congenital hydrocephalus is aqueductal
stenosis, which occurs when the narrow passage between the third and
fourth ventricles in the brain is blocked or too narrow to allow
sufficient cerebral spinal fluid to drain. Fluid accumulates in the
upper ventricles, causing hydrocephalus.
Other causes of congenital hydrocephalus include neural-tube defects, arachnoid cysts, Dandy–Walker syndrome, and Arnold–Chiari malformation.
The cranial bones
fuse by the end of the third year of life. For head enlargement to
occur, hydrocephalus must occur before then. The causes are usually
genetic, but can also be acquired and usually occur within the first few
months of life, which include intraventricular matrix hemorrhages in premature infants, infections, type II Arnold-Chiari malformation, aqueduct atresia and stenosis, and Dandy-Walker malformation.
In newborns and toddlers with hydrocephalus, the head
circumference is enlarged rapidly and soon surpasses the 97th
percentile. Since the skull bones have not yet firmly joined together,
bulging, firm anterior and posterior fontanelles may be present even when the person is in an upright position.
The infant exhibits fretfulness, poor feeding, and frequent vomiting. As the hydrocephalus progresses, torpor
sets in, and infants show lack of interest in their surroundings. Later
on, their upper eyelids become retracted and their eyes are turned
downwards ("sunset eyes") (due to hydrocephalic pressure on the mesencephalic tegmentum and paralysis of upward gaze). Movements become weak and the arms may become tremulous. Papilledema is absent, but vision may be reduced. The head becomes so enlarged that they eventually may be bedridden.
About 80–90% of fetuses or newborn infants with spina bifida—often associated with meningocele or myelomeningocele—develop hydrocephalus.
Acquired
This condition is acquired as a consequence of CNS infections, meningitis, brain tumors, head trauma, toxoplasmosis, or intracranial hemorrhage (subarachnoid or intraparenchymal), and is usually painful.
Type
The cause of
hydrocephalus is not known with certainty and is probably
multifactorial. It may be caused by impaired CSF flow, reabsorption, or
excessive CSF production.
- Obstruction to CSF flow hinders its free passage through the ventricular system and subarachnoid space (e.g., stenosis of the cerebral aqueduct or obstruction of the interventricular foramina secondary to tumors, hemorrhages, infections or congenital malformations) and can cause increases in ICP.
- Hydrocephalus can also be caused by overproduction of CSF (relative obstruction) (e.g., choroid plexus papilloma, villous hypertrophy).
- Bilateral ureteric obstruction is a rare, but reported, cause of hydrocephalus.
Based on its underlying mechanisms, hydrocephalus can be classified
into communicating and noncommunicating (obstructive). Both forms can be
either congenital or acquired.
Communicating
Communicating
hydrocephalus, also known as nonobstructive hydrocephalus, is caused by
impaired CSF reabsorption in the absence of any obstruction of CSF flow
between the ventricles and subarachnoid space. This may be due to
functional impairment of the arachnoidal granulations (also called arachnoid granulations or Pacchioni's granulations), which are located along the superior sagittal sinus,
and is the site of CSF reabsorption back into the venous system.
Various neurologic conditions may result in communicating hydrocephalus,
including subarachnoid/intraventricular hemorrhage, meningitis, and
congenital absence of arachnoid villi. Scarring and fibrosis of the
subarachnoid space following infectious, inflammatory, or hemorrhagic
events can also prevent resorption of CSF, causing diffuse ventricular
dilatation.
Noncommunicating
Noncommunicating hydrocephalus, or obstructive hydrocephalus, is caused by a CSF-flow obstruction.
- Foramen of Monro obstruction may lead to dilation of one, or if large enough (e.g., in colloid cyst), both lateral ventricles.
- The aqueduct of Sylvius, normally narrow, may be obstructed by a number of genetic or acquired lesions (e.g., atresia, ependymitis, hemorrhage, or tumor) and lead to dilation of both lateral ventricles, as well as the third ventricle.
- Fourth ventricle obstruction leads to dilatation of the aqueduct, as well as the lateral and third ventricles (e.g., Chiari malformation).
- The foramina of Luschka and foramen of Magendie may be obstructed due to congenital malformation (e.g., Dandy-Walker malformation).
Other
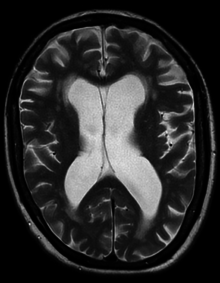
Hydrocephalus ex vacuo from vascular dementia as seen on MRI
- Normal pressure hydrocephalus (NPH) is a particular form of chronic communicating hydrocephalus, characterized by enlarged cerebral ventricles, with only intermittently elevated cerebrospinal fluid pressure. Characteristic triad of symptoms are; dementia, apraxic gait and urinary incontinence. The diagnosis of NPH can be established only with the help of continuous intraventricular pressure recordings (over 24 hours or even longer), since more often than not instant measurements yield normal pressure values. Dynamic compliance studies may be also helpful. Altered compliance (elasticity) of the ventricular walls, as well as increased viscosity of the cerebrospinal fluid, may play a role in the pathogenesis.
- Hydrocephalus ex vacuo also refers to an enlargement of cerebral ventricles and subarachnoid spaces, and is usually due to brain atrophy (as it occurs in dementias), post-traumatic brain injuries, and even in some psychiatric disorders, such as schizophrenia. As opposed to hydrocephalus, this is a compensatory enlargement of the CSF-spaces in response to brain parenchyma loss; it is not the result of increased CSF pressure.
Mechanism
Spontaneous intracerebral and intraventricular hemorrhage with hydrocephalus shown on CT scan
3D cast of lateral ventricles in hydrocephalus
Hydrocephalus is usually due to blockage of CSF outflow in the
ventricles or in the subarachnoid space over the brain. In a person
without hydrocephalus, CSF continuously circulates through the brain,
its ventricles and the spinal cord
and is continuously drained away into the circulatory system.
Alternatively, the condition may result from an overproduction of the
CSF, from a congenital malformation blocking normal drainage of the
fluid, or from complications of head injuries or infections.
Compression of the brain by the accumulating fluid eventually may cause neurological symptoms such as convulsions, intellectual disability, and epileptic seizures.
These signs occur sooner in adults, whose skulls are no longer able to
expand to accommodate the increasing fluid volume within. Fetuses,
infants, and young children with hydrocephalus typically have an
abnormally large head, excluding the face, because the pressure of the
fluid causes the individual skull bones—which have yet to fuse—to bulge
outward at their juncture points. Another medical sign,
in infants, is a characteristic fixed downward gaze with whites of the
eyes showing above the iris, as though the infant were trying to examine
its own lower eyelids.
The elevated ICP may cause compression of the brain, leading to
brain damage and other complications. Conditions among affected
individuals vary widely.
If the foramina of the fourth ventricle or the cerebral aqueduct
are blocked, CSF can accumulate within the ventricles. This condition is
called internal hydrocephalus and it results in increased CSF pressure.
The production of CSF continues, even when the passages that normally
allow it to exit the brain are blocked. Consequently, fluid builds
inside the brain, causing pressure that dilates the ventricles and
compresses the nervous tissue. Compression of the nervous tissue usually results in irreversible brain damage. If the skull bones are not completely ossified
when the hydrocephalus occurs, the pressure may also severely enlarge
the head. The cerebral aqueduct may be blocked at the time of birth or may become blocked later in life because of a tumor growing in the brainstem.
Treatment
Procedures
Baby recovering from shunt surgery
Hydrocephalus treatment is surgical, creating a way for the excess fluid to drain away. In the short term, an external ventricular drain
(EVD), also known as an extraventricular drain or ventriculostomy,
provides relief. In the long term, some people will need any of various
types of cerebral shunt. It involves the placement of a ventricular catheter (a tube made of silastic)
into the cerebral ventricles to bypass the flow
obstruction/malfunctioning arachnoidal granulations and drain the excess
fluid into other body cavities, from where it can be resorbed. Most
shunts drain the fluid into the peritoneal cavity (ventriculoperitoneal shunt), but alternative sites include the right atrium (ventriculoatrial shunt), pleural cavity (ventriculopleural shunt), and gallbladder. A shunt system can also be placed in the lumbar space of the spine and have the CSF redirected to the peritoneal cavity (lumbar-peritoneal shunt). An alternative treatment for obstructive hydrocephalus in selected people is the endoscopic third ventriculostomy (ETV), whereby a surgically created opening in the floor of the third ventricle allows the CSF to flow directly to the basal cisterns,
thereby shortcutting any obstruction, as in aqueductal stenosis. This
may or may not be appropriate based on individual anatomy. For infants,
ETV is sometimes combined with choroid plexus cauterization, which
reduces the amount of cerebrospinal fluid produced by the brain. The
technique, known as ETV/CPC, was pioneered in Uganda by neurosurgeon Benjamin Warf and is now in use in several U.S. hospitals.
Hydrocephalus can be successfully treated by placing a drainage tube
(shunt) between the brain ventricles and abdominal cavity. Some risk
exists of infection being introduced into the brain through these shunts, however, and the shunts must be replaced as the person grows.
External hydrocephalus
External
hydrocephalus is a condition generally seen in infants which involves
enlarged fluid spaces or subarachnoid spaces around the outside of the
brain. This is generally a benign condition that resolves spontaneously by two years of age
and therefore usually does not require insertion of a shunt. Imaging
studies and a good medical history can help to differentiate external
hydrocephalus from subdural hemorrhages or symptomatic chronic extra-axial fluid collections which are accompanied by vomiting, headaches, and seizures.
Shunt complications
Examples
of possible complications include shunt malfunction, shunt failure, and
shunt infection, along with infection of the shunt tract following
surgery (the most common reason for shunt failure is infection of the
shunt tract). Although a shunt generally works well, it may stop working
if it disconnects, becomes blocked (clogged) or infected, or it is
outgrown. If this happens, the CSF begins to accumulate again and a
number of physical symptoms develop (headaches, nausea, vomiting, photophobia/light sensitivity), some extremely serious, such as seizures.
The shunt failure rate is also relatively high (of the 40,000 surgeries
performed annually to treat hydrocephalus, only 30% are a person's
first surgery) and people not uncommonly have multiple shunt revisions
within their lifetimes.
Another complication can occur when CSF drains more rapidly than it is produced by the choroid plexus, causing symptoms of listlessness, severe headaches, irritability, light sensitivity, auditory hyperesthesia (sound sensitivity), nausea, vomiting, dizziness, vertigo, migraines, seizures, a change in personality, weakness in the arms or legs, strabismus, and double vision to appear when the person is vertical. If the person lies down, the symptoms usually vanish quickly. A CT scan
may or may not show any change in ventricle size, particularly if the
person has a history of slit-like ventricles. Difficulty in diagnosing
over-drainage can make treatment of this complication particularly
frustrating for people and their families. Resistance to traditional analgesic pharmacological therapy may also be a sign of shunt overdrainage or failure.
The diagnosis of CSF buildup is complex and requires specialist
expertise. Diagnosis of the particular complication usually depends on
when the symptoms appear, that is, whether symptoms occur when the
person is upright or in a prone position, with the head at roughly the
same level as the feet.
Standardized protocols for inserting cerebral shunts have been shown to reduce shunt infections.
History
Skull of a hydrocephalic child (1800s)
References to hydrocephalic skulls can be found in ancient Egyptian medical literature from 2,500 BC to 500 AD.
Hydrocephalus was described more clearly by the ancient Greek physician
Hippocrates in the fourth century BC, while a more accurate description
was later given by the Roman physician Galen in the second century AD.
The first clinical description of an operative procedure for hydrocephalus appears in the Al-Tasrif (1,000 AD) by the Arab surgeon Abulcasis, who clearly described the evacuation of superficial intracranial fluid in hydrocephalic children. He described it in his chapter on neurosurgical disease, describing infantile hydrocephalus as being caused by mechanical compression. He wrote:
The skull of a newborn baby is often full of liquid, either because the matron has compressed it excessively or for other, unknown reasons. The volume of the skull then increases daily, so that the bones of the skull fail to close. In this case, we must open the middle of the skull in three places, make the liquid flow out, then close the wound and tighten the skull with a bandage.
Historical specimen of an infant with severe hydrocephalus, probably untreated
In 1881, a few years after the landmark study of Retzius and Key, Carl Wernicke pioneered sterile ventricular puncture and external drainage of CSF for the treatment of hydrocephalus.
It remained an intractable condition until the 20th century, when
cerebral shunt and other neurosurgical treatment modalities were
developed.
It is a lesser-known medical condition; relatively little
research is conducted to improve treatment, and still no cure has been
found. In developing countries, the condition often goes untreated at
birth. Before birth, the condition is difficult to diagnose, and access
to medical treatment is limited. However, when head swelling is
prominent, children are taken at great expense for treatment. By then,
brain tissue is undeveloped and neurosurgery is rare and difficult.
Children more commonly live with undeveloped brain tissue and
consequential intellectual disabilities and restrictions.
Society and culture
Name
The word "hydrocephalus" is from the Greek ὕδωρ, hydōr meaning "water" and κεφαλή, kephalē meaning "head". Other names for hydrocephalus include "water on the brain", a historical name, and "water baby syndrome".
Awareness campaign
Hydrocephalus awareness ribbon
September was designated National Hydrocephalus Awareness Month in July 2009 by the U.S. Congress in H.Res. 373.
The resolution campaign is due in part to the advocacy work of the
Pediatric Hydrocephalus Foundation. Prior to July 2009, no awareness
month for this condition had been designated. Many of the hydrocephalus
organizations within the U.S. use various ribbon designs as a part of their awareness and fundraising activities.
Exceptional case
One
exceptional case of hydrocephalus was a man whose brain shrank to a
thin sheet of tissue, due to a buildup of cerebrospinal fluid in his
skull. As a child, the man had a shunt, but it was removed when he was
14. In July 2007, at age 44, he went to a hospital due to mild weakness
in his left leg. When doctors learned of the man's medical history, they
performed a CT and MRI scan, and were astonished to see "massive
enlargement" of the lateral ventricles in the skull. Dr. Lionel Feuillet
of Hôpital de la Timone in Marseille said, "The images were most unusual... the brain was virtually absent."
Intelligence tests showed the person had an IQ of 75, considered
"borderline intellectual functioning", just above what would be
officially considered mentally challenged.
The person was a married father of two children, and worked as a
civil servant, leading an at least superficially normal life, despite
having enlarged ventricles with a decreased volume of brain tissue.
"What I find amazing to this day is how the brain can deal with
something which you think should not be compatible with life", commented
Dr. Max Muenke, a pediatric brain-defect specialist at the National Human Genome Research Institute.
"If something happens very slowly over quite some time, maybe over
decades, the different parts of the brain take up functions that would
normally be done by the part that is pushed to the side."
Notable cases
- Author Sherman Alexie, born with the condition, wrote about it in his semi-autobiographical junior fiction novel The Absolutely True Diary of a Part-Time Indian.
- Prince William, Duke of Gloucester (1689–1700) probably contracted meningitis at birth, which resulted in this condition.
- Emperor Ferdinand I of Austria (1793–1875) became emperor in 1835 despite various health issues including hydrocephalus and epilepsy.