| Lumbar puncture | |
|---|---|

Lumbar puncture in a sitting position. The reddish-brown swirls on the patient's back are tincture of iodine (an antiseptic).
| |
| Other names | Spinal tap |
| ICD-9-CM | 03.31 |
| MeSH | D013129 |
| eMedicine | 80773 |
Lumbar puncture (LP), also known as a spinal tap, is a medical procedure in which a needle is inserted into the spinal canal, most commonly to collect cerebrospinal fluid (CSF) for diagnostic testing. The main reason for a lumbar puncture is to help diagnose diseases of the central nervous system, including the brain and spine. Examples of these conditions include meningitis and subarachnoid hemorrhage. It may also be used therapeutically in some conditions. Increased intracranial pressure (pressure in the skull) is a contraindication, due to risk of brain matter being compressed and pushed toward the spine. Sometimes, lumbar puncture cannot be performed safely (for example due to a severe bleeding tendency). It is regarded as a safe procedure, but post-dural-puncture headache is a common side effect.
The procedure is typically performed under local anesthesia using a sterile technique. A hypodermic needle is used to access the subarachnoid space and fluid collected. Fluid may be sent for biochemical, microbiological, and cytological analysis. Using ultrasound to landmark may increase success.
Lumbar puncture was first introduced in 1891 by the German physician Heinrich Quincke.
Medical uses
The reason for a lumbar puncture may be to make a diagnosis or to treat a disease.
Diagnosis
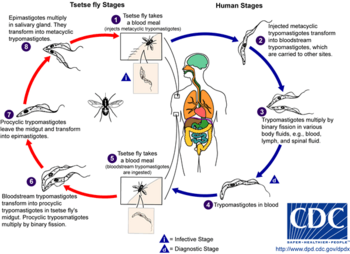
The chief diagnostic indications of lumbar puncture are for collection of cerebrospinal fluid (CSF). Analysis of CSF may exclude infectious, inflammatory, and neoplastic diseases affecting the central nervous system. The most common purpose is in suspected meningitis,
since there is no other reliable tool with which meningitis, a
life-threatening but highly treatable condition, can be excluded. A
lumbar puncture can also be used to detect whether someone has 'Stage 1'
or 'Stage 2' Trypanosoma brucei.
Young infants commonly require lumbar puncture as a part of the routine
workup for fever without a source. This is due to higher rates of
meningitis than in older persons. Infants also do not reliably show
classic symptoms of meningeal irritation (meningismus) like neck stiffness and headache the way adults do. In any age group, subarachnoid hemorrhage, hydrocephalus, benign intracranial hypertension,
and many other diagnoses may be supported or excluded with this test.
It may also be used to detect the presence of malignant cells in the
CSF, as in carcinomatous meningitis or medulloblastoma. CSF containing less than 10 red blood cells
(RBCs)/mm³ constitutes a "negative" tap in the context of a workup for
subarachnoid hemorrhage, for example. Taps that are "positive" have an
RBC count of 100/mm³ or more.
Treatment
Lumbar punctures may also be done to inject medications into the cerebrospinal fluid ("intrathecally"), particularly for spinal anesthesia or chemotherapy.
Serial lumbar punctures may be useful in temporary treatment of idiopathic intracranial hypertension
(IIH). This disease is characterized by increased pressure of CSF which
may cause headache and permanent loss of vision. While mainstays of
treatment are medication, in some cases lumbar puncture performed
multiple times may improve symptoms. It is not recommended as a staple
of treatment due to discomfort and risk of the procedure, and the short
duration of its efficacy.
Additionally, some people with normal pressure hydrocephalus
(characterized by urinary incontinence, a changed ability to walk
properly, and dementia) receive some relief of symptoms after removal of
CSF.
Contraindications
Lumbar puncture should not be performed in the following situations:
- Idiopathic (unidentified cause) increased intracranial pressure (ICP)
- Rationale: lumbar puncture in the presence of raised ICP may cause uncal herniation
- Exception: therapeutic use of lumbar puncture to reduce ICP, but only if obstruction (for example in the third ventricle of the brain) has been ruled out
- Precaution
- CT brain, especially in the following situations
- Age >65
- Reduced GCS
- Recent history of seizure
- Focal neurological signs
- Abnormal respiratory pattern
- Hypertension with bradycardia and deteriorating consciousness
- Ophthalmoscopy for papilledema
- CT brain, especially in the following situations
- Bleeding diathesis (relative)
- Coagulopathy
- Decreased platelet count (<50 10="" sup="" x="">9
- Skin infection at puncture site
Adverse effects
Headache
Post spinal headache with nausea is the most common complication; it often responds to pain medications and infusion of fluids. It was long taught that this complication can be prevented by strict maintenance of a supine posture
for two hours after the successful puncture; this has not been borne
out in modern studies involving large numbers of people. Doing the
procedure with the person on their side might decrease the risk.[13]
Intravenous caffeine injection is often quite effective in aborting
these spinal headaches. A headache that is persistent despite a long
period of bedrest and occurs only when sitting up may be indicative of a
CSF leak from the lumbar puncture site. It can be treated by more
bedrest, or by an epidural blood patch, where the person's own blood is injected back into the site of leakage to cause a clot to form and seal off the leak.
The risk of headache and need for analgesia and blood patch is
much reduced if "atraumatic" needles are used. This does not affect the
success rate of the procedure in other ways.
Other
Contact between the side of the lumbar puncture needle and a spinal nerve root can result in anomalous sensations (paresthesia)
in a leg during the procedure; this is harmless and people can be
warned about it in advance to minimize their anxiety if it should occur.
Serious complications of a properly performed lumbar puncture are extremely rare. They include spinal or epidural bleeding, adhesive arachnoiditis and trauma to the spinal cord or spinal nerve roots resulting in weakness or loss of sensation, or even paraplegia.
The latter is exceedingly rare, since the level at which the spinal
cord ends (normally the inferior border of L1, although it is slightly
lower in infants) is several vertebral spaces above the proper location
for a lumbar puncture (L3/L4). There are case reports of lumbar puncture
resulting in perforation of abnormal dural arterio-venous malformations, resulting in catastrophic epidural hemorrhage; this is exceedingly rare.
The procedure is not recommended when epidural infection
is present or suspected, when topical infections or dermatological
conditions pose a risk of infection at the puncture site or in patients
with severe psychosis or neurosis
with back pain. Some authorities believe that withdrawal of fluid when
initial pressures are abnormal could result in spinal cord compression
or cerebral herniation;
others believe that such events are merely coincidental in time,
occurring independently as a result of the same pathology that the
lumbar puncture was performed to diagnose. In any case, computed tomography of the brain is often performed prior to lumbar puncture if an intracranial mass is suspected.
Technique
Mechanism
The
brain and spinal cord are enveloped by a layer of cerebrospinal fluid,
125-150 ml in total (in adults) which acts as a shock absorber and
provides a medium for the transfer of nutrients and waste products. The
majority is produced by the choroid plexus in the brain and circulates from there to other areas, before being reabsorbed into the circulation (predominantly by the arachnoid granulations).
The cerebrospinal fluid can be accessed most safely in the lumbar cistern. Below the first or second lumbar vertebrae (L1 or L2) the spinal cord terminates (conus medullaris). Nerves continue down the spine below this, but in a loose bundle of nerve fibers called the cauda equina.
There is lower risk with inserting a needle into the spine at the level
of the cauda equina because these loose fibers move out of the way of
the needle without being damaged. The lumbar cistern extends into the sacrum.
Procedure
Illustration depicting lumbar puncture (spinal tap)
Spinal needles used in lumbar puncture.
Illustration depicting common positions for lumbar puncture procedure.
The person is usually placed on their side (left more commonly than
right). The patient bends the neck so the chin is close to the chest,
hunches the back, and brings knees toward the chest. This approximates a
fetal position
as much as possible. Patients may also sit on a stool and bend their
head and shoulders forward. The area around the lower back is prepared
using aseptic technique. Once the appropriate location is palpated,
local anaesthetic is infiltrated under the skin and then injected along
the intended path of the spinal needle. A spinal needle is inserted
between the lumbar vertebrae L3/L4, L4/L5 or L5/S1 and pushed in until there is a "give" as it enters the lumbar cistern wherein the ligamentum flavum is housed. The needle is again pushed until there is a second 'give' that indicates the needle is now past the dura mater. The arachnoid membrane and the dura mater exist in flush contact with one another in the living person's spine due to fluid pressure from CSF in the subarachnoid space
pushing the arachnoid membrane out towards the dura. Therefore, once
the needle has pierced the dura mater it has also traversed the thinner
arachnoid membrane. The needle is then in the subarachnoid space. The
stylet from the spinal needle is then withdrawn and drops of
cerebrospinal fluid are collected. The opening pressure of the
cerebrospinal fluid may be taken during this collection by using a
simple column manometer.
The procedure is ended by withdrawing the needle while placing pressure
on the puncture site. The spinal level is so selected to avoid spinal
injuries.
In the past, the patient would lie on their back for at least six hours
and be monitored for signs of neurological problems. There is no
scientific evidence that this provides any benefit. The technique
described is almost identical to that used in spinal anesthesia, except that spinal anesthesia is more often done with the patient in a seated position.
The upright seated position is advantageous in that there is less
distortion of spinal anatomy which allows for easier withdrawal of
fluid. Some practitioners prefer it for lumbar puncture in obese
patients, where lying on their side would cause a scoliosis
and unreliable anatomical landmarks. However, opening pressures are
notoriously unreliable when measured in the seated position. Therefore,
patients will ideally lie on their side if practitioners need to measure
opening pressure.
Reinsertion of the stylet may decrease the rate of post lumbar puncture headaches.
Although not available in all clinical settings, use of ultrasound
is helpful for visualizing the interspinous space and assessing the
depth of the spine from the skin. Use of ultrasound reduces the number
of needle insertions and redirections, and results in higher rates of
successful lumbar puncture. If the procedure is difficult, such as in people with spinal deformities such as scoliosis, it can also be performed under fluoroscopy (under continuous X-ray imaging).
Children
In
children, a sitting flexed position was as successful as lying on the
side with respect to obtaining non-traumatic CSF, CSF for culture, and
cell count. There was a higher success rate in obtaining CSF in the
first attempt in infants younger than 12 months in the sitting flexed
position.
The spine of an infant at the time of birth differs from the adult spine. The conus medullaris
(bottom of the spinal cord) terminates at the level of L1 in adults,
but may range in term neonates (newly born babies) from L1-L3 levels. It is important to insert the spinal needle below the conus medullaris at the L3/L4 or L4/L5 interspinous levels. With growth of the spine, the conus typically reaches the adult level (L1) by 2 years of age.
The ligamentum flavum and dura mater
are not as thick in infants and children as they are in adults.
Therefore, it is difficult to assess when the needle passes through them
into the subarachnoid space because the characteristic "pop" or "give"
may be subtle or nonexistent in the pediatric lumbar puncture. To
decrease the chances of inserting the spinal needle too far, some
clinicians use the "Cincinnati" method. This method involves removing
the stylet of the spinal needle once the needle has advanced through the
dermis. After removal of the stylet, the needle is inserted until CSF
starts to come out of the needle. Once all of the CSF is collected, the
stylet is then reinserted before removal of the needle.
Interpretation
Analysis
of the cerebrospinal fluid generally includes a cell count and
determination of the glucose and protein concentrations. The other
analytical studies of cerebrospinal fluid are conducted according to the
diagnostic suspicion.
Pressure determination
Lumbar puncture in a child suspected of having meningitis.
Increased CSF pressure can indicate congestive heart failure, cerebral edema, subarachnoid hemorrhage, hypo-osmolality resulting from hemodialysis, meningeal inflammation, purulent meningitis or tuberculous meningitis, hydrocephalus, or pseudotumor cerebri. In the setting of raised pressure (or normal pressure hydrocephalus, where the pressure is normal but there is excessive CSF), lumbar puncture may be therapeutic.
Decreased CSF pressure can indicate complete subarachnoid blockage, leakage of spinal fluid, severe dehydration, hyperosmolality, or circulatory collapse.
Significant changes in pressure during the procedure can indicate
tumors or spinal blockage resulting in a large pool of CSF, or
hydrocephalus associated with large volumes of CSF.
Cell count
The presence of white blood cells in cerebrospinal fluid is called pleocytosis. A small number of monocytes can be normal; the presence of granulocytes is always an abnormal finding. A large number of granulocytes often heralds bacterial meningitis.
White cells can also indicate reaction to repeated lumbar punctures,
reactions to prior injections of medicines or dyes, central nervous
system hemorrhage, leukemia, recent epileptic seizure, or a metastatic tumor. When peripheral blood contaminates the withdrawn CSF, a common procedural complication, white blood cells will be present along with erythrocytes, and their ratio will be the same as that in the peripheral blood.
The finding of erythrophagocytosis, where phagocytosed erythrocytes
are observed, signifies haemorrhage into the CSF that preceded the
lumbar puncture. Therefore, when erythrocytes are detected in the CSF
sample, erythrophagocytosis suggests causes other than a traumatic tap,
such as intracranial haemorrhage and haemorrhagic herpetic encephalitis. In which case, further investigations are warranted, including imaging and viral culture.
Microbiology
CSF can be sent to the microbiology lab for various types of smears and cultures to diagnose infections.
- Gram staining may demonstrate gram positive bacteria in bacterial meningitis.
- Microbiological culture is the gold standard for detecting bacterial meningitis. Bacteria, fungi, and viruses can all be cultured by using different techniques.
- Polymerase chain reaction (PCR) has been a great advance in the diagnosis of some types of meningitis, such as meningitis from herpesvirus and enterovirus. It has high sensitivity and specificity for many infections of the CNS, is fast, and can be done with small volumes of CSF. Even though testing is expensive, cost analyses of PCR testing in neonatal patients demonstrated savings via reduced cost of hospitalization.
- Numerous antibody-mediated tests for CSF are available in some countries: these include rapid tests for antigens of common bacterial pathogens, treponemal titers for the diagnosis of neurosyphilis and Lyme disease, Coccidioides antibody, and others.
- The India ink test is still used for detection of meningitis caused by Cryptococcus neoformans, but the cryptococcal antigen (CrAg) test has a higher sensitivity.
Chemistry
Several substances found in cerebrospinal fluid are available for diagnostic measurement.
- Glucose is present in the CSF; the level is usually about 60% that in the peripheral circulation. A fingerstick or venipuncture at the time of lumbar puncture may therefore be performed to assess peripheral glucose levels and determine a predicted CSF glucose value. Decreased glucose levels can indicate fungal, tuberculous or pyogenic infections; lymphomas; leukemia spreading to the meninges; meningoencephalitic mumps; or hypoglycemia. A glucose level of less than one third of blood glucose levels in association with low CSF lactate levels is typical in hereditary CSF glucose transporter deficiency also known as De Vivo disease.
- Increased glucose levels in the fluid can indicate diabetes, although the 60% rule still applies.
- Increased levels of glutamine are often involved with hepatic encephalopathies, Reye's syndrome, hepatic coma, cirrhosis, hypercapnia and depression.
- Increased levels of lactate can occur the presence of cancer of the CNS, multiple sclerosis, heritable mitochondrial disease, low blood pressure, low serum phosphorus, respiratory alkalosis, idiopathic seizures, traumatic brain injury, cerebral ischemia, brain abscess, hydrocephalus, hypocapnia or bacterial meningitis.
- The enzyme lactate dehydrogenase can be measured to help distinguish meningitides of bacterial origin, which are often associated with high levels of the enzyme, from those of viral origin in which the enzyme is low or absent.
- Changes in total protein content of cerebrospinal fluid can result from pathologically increased permeability of the blood-cerebrospinal fluid barrier, obstructions of CSF circulation, meningitis, neurosyphilis, brain abscesses, subarachnoid hemorrhage, polio, collagen disease or Guillain–Barré syndrome, leakage of CSF, increases in intracranial pressure, or hyperthyroidism. Very high levels of protein may indicate tuberculous meningitis or spinal block.
- IgG synthetic rate is calculated from measured IgG and total protein levels; it is elevated in immune disorders such as multiple sclerosis, transverse myelitis, and neuromyelitis optica of Devic. Oligoclonal bands may be detected in CSF but not in serum, suggesting intrathecal antibody production.
| Infection | Appearance | WBCs / mm3 | Protein (g/l) | Glucose |
|---|---|---|---|---|
| Normal | Clear | <5 font=""> | 0.15 to 0.45 | > 2/3 of blood glucose |
| Bacterial | Yellowish, turbid | > 1,000 (mostly PMNs) | > 1 | Low |
| Viral | Clear | < 200 (mostly lymphocytes) | Mild increase | Normal or mildly low |
| Tuberculosis | Yellowish and viscous | Modest increase | Markedly Increased | Decreased |
| Fungal | Yellowish and viscous | < 50 (mostly lymphocytes) | Initially normal than increased
|
Normal or mildly low |
History
Lumbar puncture, early 20th century.
The first technique for accessing the dural space was described by the London physician Walter Essex Wynter. In 1889 he developed a crude cut down with cannulation
in four patients with tuberculous meningitis. The main purpose was the
treatment of raised intracranial pressure rather than for diagnosis. The technique for needle lumbar puncture was then introduced by the German physician Heinrich Quincke, who credits Wynter with the earlier discovery; he first reported his experiences at an internal medicine conference in Wiesbaden, Germany, in 1891. He subsequently published a book on the subject.
The lumbar puncture procedure was taken to the United States by Arthur H. Wentworth an assistant professor at the Harvard Medical School, based at Children's Hospital. In 1893 he published a long paper on diagnosing cerebrospinal meningitis by examining spinal fluid. However, he was criticized by antivivisectionists for having obtained spinal fluid from children. He was acquitted, but, nevertheless, he was uninvited from the then forming Johns Hopkins School of Medicine, where he would have been the first professor of pediatrics.
Historically lumbar punctures were also employed in the process of performing a pneumoencephalography,
a nowadays obsolete X-ray imaging study of the brain that was performed
extensively from the 1920s until the advent of modern non-invasive neuroimaging techniques such as MRI and CT
in the 1970s. During this quite painful procedure, CSF was replaced
with air or some other gas via the lumbar puncture in order to enhance
the appearance of certain areas of the brain on plain radiographs.