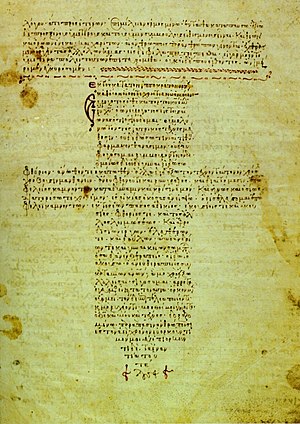
A 12th-century Byzantine manuscript of the Hippocratic Oath
AMA Code of Medical Ethics
Medical ethics is a system of moral principles that apply
values to the practice of clinical medicine and in scientific research.
Medical ethics is based on a set of values that professionals can refer
to in the case of any confusion or conflict. These values include the
respect for autonomy, non-maleficence, beneficence, and justice.
Such tenets may allow doctors, care providers, and families to create a
treatment plan and work towards the same common goal without any
conflict. It is important to note that these four values are non-hierarchical, meaning no one principle routinely “trumps” another.
The term medical ethics first dates back to 1803, when English author and physician Thomas Percival
published a document describing the requirements and expectations of
medical professionals within medical facilities. The Code of Ethics was
then adapted in 1847, relying heavily on Percival's words. Over the years in 1903, 1912, and 1947, revisions have been made to the original document. The practice of Medical Ethics is widely accepted and practiced throughout the world.
There are several other codes of conduct. The Hippocratic Oath discusses basic principles for medical professionals. This document dates back to the fifth century BCE. Both The Declaration of Helsinki (1964) and The Nuremberg Code
(1947) are two well-known and well respected documents contributing to
medical ethics. Other important markings in the history of Medical
Ethics include Roe v. Wade
in 1973 and the development of Hemodialysis in the 1960s. As this field
continues to develop and change throughout history, the focus remains
on fair, balanced, and moral thinking. Medical ethics encompasses a
practical application in clinical settings as well as scholarly work on
its history, philosophy, and sociology.
History
Historically, Western medical ethics may be traced to guidelines on the duty of physicians in antiquity, such as the Hippocratic Oath, and early Christian teachings. The first code of medical ethics, Formula Comitis Archiatrorum, was published in the 5th century, during the reign of the Ostrogothic king Theodoric the Great. In the medieval and early modern period, the field is indebted to Islamic scholarship such as Ishaq ibn Ali al-Ruhawi (who wrote the Conduct of a Physician, the first book dedicated to medical ethics), Avicenna's Canon of Medicine and Muhammad ibn Zakariya ar-Razi (known as Rhazes in the West), Jewish thinkers such as Maimonides, Roman Catholic scholastic thinkers such as Thomas Aquinas, and the case-oriented analysis (casuistry) of Catholic moral theology. These intellectual traditions continue in Catholic, Islamic and Jewish medical ethics.
By the 18th and 19th centuries, medical ethics emerged as a more self-conscious discourse. In England, Thomas Percival,
a physician and author, crafted the first modern code of medical
ethics. He drew up a pamphlet with the code in 1794 and wrote an
expanded version in 1803, in which he coined the expressions "medical
ethics" and "medical jurisprudence".
However, there are some who see Percival's guidelines that relate to
physician consultations as being excessively protective of the home
physician's reputation. Jeffrey Berlant is one such critic who considers
Percival's codes of physician consultations as being an early example
of the anti-competitive, "guild"-like nature of the physician community.
In 1815, the Apothecaries Act was passed by the Parliament of the United Kingdom.
It introduced compulsory apprenticeship and formal qualifications for
the apothecaries of the day under the license of the Society of
Apothecaries. This was the beginning of regulation of the medical
profession in the UK.
In 1847, the American Medical Association adopted its first code of ethics, with this being based in large part upon Percival's work. While the secularized field borrowed largely from Catholic medical ethics, in the 20th century a distinctively liberal Protestant approach was articulated by thinkers such as Joseph Fletcher. In the 1960s and 1970s, building upon liberal theory and procedural justice, much of the discourse of medical ethics went through a dramatic shift and largely reconfigured itself into bioethics.
Well-known medical ethics cases include:
- Albert Kligman's dermatology experiments
- Deep sleep therapy
- Doctors' Trial
- Greenberg v. Miami Children's Hospital Research Institute
- Henrietta Lacks
- Chester M. Southam's Cancer Injection Study
- Human radiation experiments
- Jesse Gelsinger
- Moore v. Regents of the University of California
- Surgical removal of body parts to try to improve mental health
- Medical Experimentation on Black Americans
- Milgram experiment
- Radioactive iodine experiments
- The Monster Study
- Plutonium injections
- The David Reimer case
- The Stanford Prison Experiment
- Tuskegee syphilis experiment
- Willowbrook State School
- Yanomami blood sample collection
Since the 1970s, the growing influence of ethics in contemporary medicine can be seen in the increasing use of Institutional Review Boards
to evaluate experiments on human subjects, the establishment of
hospital ethics committees, the expansion of the role of clinician
ethicists, and the integration of ethics into many medical school
curricula.
Values
A common framework used in the analysis of medical ethics is the "four principles" approach postulated by Tom Beauchamp and James Childress in their textbook Principles of biomedical ethics. It recognizes four basic moral principles, which are to be judged and
weighed against each other, with attention given to the scope of their
application. The four principles are:
- Respect for autonomy – the patient has the right to refuse or choose their treatment.
- Beneficence – a practitioner should act in the best interest of the patient.
- Non-maleficence – to not be the cause of harm. Also, "Utility" - to promote more good than harm
- Justice – concerns the distribution of scarce health resources, and the decision of who gets what treatment.
Autonomy
The
principle of autonomy views the rights of an individual to
self-determination. This is rooted in society's respect for individuals'
ability to make informed decisions about personal matters with freedom.
Autonomy has become more important as social values have shifted to
define medical quality in terms of outcomes that are important to the
patient and their family rather than medical professionals. The
increasing importance of autonomy can be seen as a social reaction
against the "paternalistic" tradition within healthcare.
Some have questioned whether the backlash against historically
excessive paternalism in favor of patient autonomy has inhibited the
proper use of soft paternalism to the detriment of outcomes for some patients.
The definition of autonomy is the ability of an individual to
make a rational, un-influenced decision. Therefore, it can be said that
autonomy is a general indicator of a healthy mind and body. The
progression of many terminal diseases are characterized by loss of
autonomy, in various manners and extents. For example, dementia almost
always results in the loss of autonomy. Dementia is a chronic and
progressive disease that attacks the brain and affects the ability to
make judgments, can induce memory loss, cause a decrease in rational
thinking and affect orientation.
Psychiatrists and clinical psychologists are often asked to
evaluate a patient's capacity for making life-and-death decisions at the
end of life. Persons with a psychiatric condition such as delirium or
clinical depression may lack capacity to make end-of-life decisions. For
these persons, a request to refuse treatment may be taken in the
context of their condition. Unless there is a clear advance directive to
the contrary, persons lacking mental capacity are treated according to
their best interests. This will involve an assessment involving people
who know the person best to what decisions the person would have made
had they not lost capacity.
Persons with the mental capacity to make end-of-life decisions may
refuse treatment with the understanding that it may shorten their life.
Psychiatrists and psychologists may be involved to support decision
making.
Beneficence
The
term beneficence refers to actions that promote the well being of
others. In the medical context, this means taking actions that serve the
best interests of patients and their families. However, uncertainty
surrounds the precise definition of which practices do in fact help
patients.
James Childress and Tom Beauchamp in Principle of Biomedical Ethics (1978) identify beneficence as one of the core values of healthcare ethics. Some scholars, such as Edmund Pellegrino, argue that beneficence is the only
fundamental principle of medical ethics. They argue that healing should
be the sole purpose of medicine, and that endeavors like cosmetic surgery and euthanasia are severely unethical and against the Hippocratic Oath.
Non-maleficence
The concept of non-maleficence is embodied by the phrase, "first, do no harm," or the Latin, primum non nocere. Many consider that should be the main or primary consideration (hence primum):
that it is more important not to harm your patient, than to do them
good, which is part of the hippocratic oath that doctors take.
This is partly because enthusiastic practitioners are prone to using
treatments that they believe will do good, without first having
evaluated them adequately to ensure they do no harm to the patient. Much
harm has been done to patients as a result, as in the saying, "The
treatment was a success, but the patient died." It is not only more
important to do no harm than to do good; it is also important to know
how likely it is that your treatment will harm a patient. So a
physician should go further than not prescribing medications they know
to be harmful—he or she should not prescribe medications (or otherwise
treat the patient) unless s/he knows that the treatment is unlikely to
be harmful; or at the very least, that patient understands the risks and
benefits, and that the likely benefits outweigh the likely risks.
In practice, however, many treatments carry some risk of harm. In
some circumstances, e.g. in desperate situations where the outcome
without treatment will be grave, risky treatments that stand a high
chance of harming the patient will be justified, as the risk of not
treating is also very likely to do harm. So the principle of non-maleficence is not absolute, and balances against the principle of beneficence (doing good), as the effects of the two principles together often give rise to a double effect
(further described in next section). Even basic actions like taking a
blood sample or an injection of a drug cause harm to the patient's body.
Euthanasia also goes against the principle of beneficence because the patient dies as a result of the medical treatment by the doctor.
Dr. Watts putting on gloves before surgery.
Double effect
Double effect refers to two types of consequences that may be produced by a single action, and in medical ethics it is usually regarded as the combined effect of beneficence and non-maleficence.
A commonly cited example of this phenomenon is the use of morphine or other analgesic
in the dying patient. Such use of morphine can have the beneficial
effect of easing the pain and suffering of the patient while
simultaneously having the maleficent effect of shortening the life of
the patient through the deactivation of the respiratory system.
Respect for human rights
The human rights era started with the formation of the United Nations in 1945, which was charged with the promotion of human rights. The Universal Declaration of Human Rights
(1948) was the first major document to define human rights. Medical
doctors have an ethical duty to protect the human rights and human dignity of the patient so the advent of a document that defines human rights has had its effect on medical ethics. Most codes of medical ethics now require respect for the human rights of the patient.
The Council of Europe promotes the rule of law and observance of human rights in Europe. The Council of Europe adopted the European Convention on Human Rights and Biomedicine (1997) to create a uniform code of medical ethics for its 47 member-states. The Convention applies international human rights law
to medical ethics. It provides special protection of physical integrity
for those who are unable to consent, which includes children.
No organ or tissue removal may be carried out on a person who does not have the capacity to consent under Article 5.
As of December 2013, the Convention had been ratified or acceded to by twenty-nine member-states of the Council of Europe.
The United Nations Educational, Scientific and Cultural Organization (UNESCO) also promotes the protection of human rights and human dignity.
According to UNESCO, "Declarations are another means of defining norms,
which are not subject to ratification. Like recommendations, they set
forth universal principles to which the community of States wished to
attribute the greatest possible authority and to afford the broadest
possible support." UNESCO adopted the Universal Declaration on Human Rights and Biomedicine
to advance the application of international human rights law in medical
ethics. The Declaration provides special protection of human rights for
incompetent persons.
In applying and advancing scientific knowledge, medical practice and associated technologies, human vulnerability should be taken into account. Individuals and groups of special vulnerability should be protected and the personal integrity of such individuals respected.
Conflicts
Between autonomy and beneficence/non-maleficence
Autonomy
can come into conflict with beneficence when patients disagree with
recommendations that healthcare professionals believe are in the
patient's best interest. When the patient's interests conflict with the
patient's welfare, different societies settle the conflict in a wide
range of manners. In general, Western medicine defers to the wishes of a
mentally competent patient to make their own decisions, even in cases
where the medical team believes that they are not acting in their own
best interests. However, many other societies prioritize beneficence
over autonomy.
Examples include when a patient does not want a treatment because of, for example, religious or cultural views. In the case of euthanasia, the patient, or relatives of a patient, may want to end the life of the patient. Also, the patient may want an unnecessary treatment, as can be the case in hypochondria or with cosmetic surgery;
here, the practitioner may be required to balance the desires of the
patient for medically unnecessary potential risks against the patient's
informed autonomy in the issue. A doctor may want to prefer autonomy
because refusal to please the patient's self-determination would harm
the doctor-patient relationship.
Individuals' capacity for informed decision-making may come into
question during resolution of conflicts between autonomy and
beneficence. The role of surrogate medical decision makers is an
extension of the principle of autonomy.
On the other hand, autonomy and beneficence/non-maleficence may
also overlap. For example, a breach of patients' autonomy may cause
decreased confidence for medical services in the population and
subsequently less willingness to seek help, which in turn may cause
inability to perform beneficence.
The principles of autonomy and beneficence/non-maleficence may
also be expanded to include effects on the relatives of patients or even
the medical practitioners, the overall population and economic issues
when making medical decisions.
Euthanasia
There is disagreement among American physicians as to whether the
non-maleficence principle excludes the practice of euthanasia.
Euthanasia is currently legal in the states of Washington DC,
California, Colorado, Oregon, Vermont, and Washington. Around the world,
there are different organizations that campaign to change legislation
about the issue of physician-assisted death, or PAD. Examples of such organizations are the Hemlock Society of the United States and the Dignity in Dying
campaign in the United Kingdom. These groups believe that doctors
should be given the right to end a patient's life only if the patient is
conscious enough to decide for themselves, is knowledgeable about the
possibility of alternative care, and has willingly asked to end their
life or requested access to the means to do so.
This argument is disputed in other parts of the world. For
example, in the state of Louisiana, giving advice or supplying the means
to end a person's life is considered a criminal act and can be charged
as a felony. In state courts, this crime is comparable to manslaughter.
The same laws apply in the states of Mississippi and Nebraska.
Informed consent
Informed consent in ethics usually refers to the idea that a person
must be fully informed about and understand the potential benefits and
risks of their choice of treatment. A correlate to "informed consent" is
the concept of informed refusal.
An uninformed person is at risk of mistakenly making a choice not
reflective of his or her values or wishes. It does not specifically mean
the process of obtaining consent, or the specific legal requirements,
which vary from place to place, for capacity to consent. Patients can
elect to make their own medical decisions or can delegate
decision-making authority to another party. If the patient is
incapacitated, laws around the world designate different processes for
obtaining informed consent, typically by having a person appointed by
the patient or their next of kin make decisions for them. The value of informed consent is closely related to the values of autonomy and truth telling.
Confidentiality
Confidentiality is commonly applied to conversations between doctors
and patients. This concept is commonly known as patient-physician
privilege. Legal protections prevent physicians from revealing their
discussions with patients, even under oath in court.
Confidentiality is mandated in America by the Health Insurance Portability and Accountability Act of 1996 known as HIPAA
, specifically the Privacy Rule, and various state laws, some more
rigorous than HIPAA. However, numerous exceptions to the rules have been
carved out over the years. For example, many states require physicians
to report gunshot wounds to the police and impaired drivers to the
Department of Motor Vehicles. Confidentiality is also challenged in
cases involving the diagnosis of a sexually transmitted disease in a
patient who refuses to reveal the diagnosis to a spouse, and in the
termination of a pregnancy in an underage patient, without the knowledge
of the patient's parents. Many states in the U.S. have laws governing
parental notification in underage abortion.
Traditionally, medical ethics has viewed the duty of
confidentiality as a relatively non-negotiable tenet of medical
practice. More recently, critics like Jacob Appel have argued for a more
nuanced approach to the duty that acknowledges the need for flexibility
in many cases.
Confidentiality is an important issue in primary care ethics,
where physicians care for many patients from the same family and
community, and where third parties often request information from the
considerable medical database typically gathered in primary health care.
Control and resolution
To ensure that appropriate ethical values are being applied within hospitals, effective hospital accreditation requires that ethical considerations are taken into account, for example with respect to physician integrity, conflict of interest, research ethics and organ transplantation ethics.
Guidelines
There
is much documentation of the history and necessity of the Declaration
of Helsinki. The first code of conduct for research including medical
ethics was the Nuremberg Code. This document had large ties to Nazi war
crimes, as it was introduced in 1947, so it didn't make much of a
difference in terms of regulating practice. This issue called for the
creation of the Declaration. There are some stark differences between
the Nuremberg Code and the Declaration of Helsinki, including the way it
is written. Nuremberg was written in a very concise manner, with a
simple explanation. The Declaration of Helsinki is written with a
thorough explanation in mind and including many specific commentaries.
In the United Kingdom, General Medical Council provides clear overall modern guidance in the form of its 'Good Medical Practice' statement. Other organizations, such as the Medical Protection Society and a number of university departments, are often consulted by British doctors regarding issues relating to ethics.
Ethics committees
Often, simple communication is not enough to resolve a conflict, and a hospital ethics committee must convene to decide a complex matter.
These bodies are composed primarily of healthcare professionals, but may also include philosophers, lay people, and clergy – indeed, in many parts of the world their presence is considered mandatory in order to provide balance.
With respect to the expected composition of such bodies in the US, Europe and Australia, the following applies.
U.S. recommendations suggest that Research and Ethical Boards (REBs) should have five or more members, including at least one scientist, one non-scientist, and one person not affiliated with the institution. The REB should include people knowledgeable in the law and standards of practice and professional conduct. Special memberships are advocated for handicapped or disabled concerns, if required by the protocol under review.
The European Forum for Good Clinical Practice (EFGCP) suggests that REBs include two practicing physicians who share experience in biomedical research and are independent from the institution where the research is conducted; one lay person; one lawyer; and one paramedical professional, e.g. nurse or pharmacist. They recommend that a quorum include both sexes from a wide age range and reflect the cultural make-up of the local community.
The 1996 Australian Health Ethics Committee recommendations were entitled, "Membership Generally of Institutional Ethics Committees". They suggest a chairperson be preferably someone not employed or otherwise connected with the institution. Members should include a person with knowledge and experience in professional care, counseling or treatment of humans; a minister of religion or equivalent, e.g. Aboriginal elder; a layman; a laywoman; a lawyer and, in the case of a hospital-based ethics committee, a nurse.
The assignment of philosophers or religious clerics will reflect the importance attached by the society to the basic values involved. An example from Sweden with Torbjörn Tännsjö on a couple of such committees indicates secular trends gaining influence.
Medical ethics in an online world
In
increasing frequency, medical researchers are researching activities in
online environments such as discussion boards and bulletin boards, and
there is concern that the requirements of informed consent and privacy
are not applied, although some guidelines do exist.
One issue that has arisen, however, is the disclosure of
information. While researchers wish to quote from the original source in
order to argue a point, this can have repercussions when the identity
of the patient is not kept confidential. The quotations and other
information about the site can be used to identify the patient, and
researchers have reported cases where members of the site, bloggers and
others have used this information as 'clues' in a game in an attempt to
identify the site. Some researchers have employed various methods of "heavy disguise." including discussing a different condition from that under study.
Cultural concerns
Culture differences can create difficult medical ethics problems. Some cultures have spiritual or magical theories about the origins and cause of disease, for example, and reconciling these beliefs with the tenets of Western medicine can be very difficult.
Truth-telling
The
WMA International Code of Medical Ethics explicitly states, "A
physician shall...report to the appropriate authorities those physicians
who practice unethically or incompetently or who engage in fraud or
deception."
There is also the conflict with physicians who are tempted to report
made up incidents or make an incident worse than what it was for their
own personal motives. In vice versa, a physician might be hesitant to
report an incident because of personal friendship he or she may have
with his or her colleague.
Online business practices and privacy
Healthcare
websites have the responsibility to ensure that the private medical
records of their online visitors are secure from being marketed and
monetized into the hands of drug companies, occupation records,
insurancers. The delivery of diagnosis online leads patients to believe
that doctors in some parts of the country are at the direct service of
drug companies, finding diagnosis as convenient as what drug still has
patent rights on it.
Physicians and drug companies are found to be competing for top ten
search engine ranks to lower costs of selling these drugs with little to
no patient involvement.
With the expansion of internet healthcare platforms, online
practitioner legitimacy and privacy accountability face unique
challenges such as e-paparazzi, online information brokers, industrial
spies, unlicensed information providers that work outside of traditional
medical codes for profit. The American Medical Association (AMA) states
that medical websites have the responsibility to ensure the health care
privacy of online visitors and protect patient records from being
marketed and monetized into the hands of insurance companies, employers,
and marketers. With
the rapid unification of healthcare, business practices, computer
science and e-commerce to create these online diagnostic websites,
efforts to maintain health care system's ethical confidentiality
standard need to keep up as well. Over the next few years, the
Department of Health and Human Services have stated that they will be
working towards lawfully protecting the online privacy and digital
transfers of patient Electronic Medical Records (EMR) under The Health
Insurance Portability and Accountability Act (HIPAA).
Humanitarian medical volunteerism
One
concern regarding the intersection of medical ethics and humanitarian
medical aid is how such assistance can be as harmful as it is helpful to
the community being served. One such example being how political forces
may control how foreign humanitarian aid can be utilized in the region
it is meant to be provided in. This would be congruous in situations
where political strife could lead such aid being used in favor of one
group over another. Another example of how foreign humanitarian aid can
be misused in its intended community includes the possibility of
dissonance forming between a foreign humanitarian aid group and the
community being served.
Examples of this could include the relationships being viewed between
aid workers, style of dress, or the lack of education regarding local
culture and customs.
Conflicts of interest
Physicians should not allow a conflict of interest
to influence medical judgment. In some cases, conflicts are hard to
avoid, and doctors have a responsibility to avoid entering such
situations. Research has shown that conflicts of interests are very
common among both academic physicians and physicians in practice.
Referral
Doctors who receive income from referring patients for medical tests have been shown to refer more patients for medical tests. This practice is proscribed by the American College of Physicians Ethics Manual. Fee splitting
and the payments of commissions to attract referrals of patients is
considered unethical and unacceptable in most parts of the world.
Vendor relationships
Studies show that doctors can be influenced by drug company inducements, including gifts and food. Industry-sponsored Continuing Medical Education (CME) programs influence prescribing patterns. Many patients surveyed in one study agreed that physician gifts from drug companies influence prescribing practices.
A growing movement among physicians is attempting to diminish the
influence of pharmaceutical industry marketing upon medical practice, as
evidenced by Stanford University's ban on drug company-sponsored
lunches and gifts. Other academic institutions that have banned
pharmaceutical industry-sponsored gifts and food include the Johns
Hopkins Medical Institutions, University of Michigan, University of
Pennsylvania, and Yale University.
Treatment of family members
The American Medical Association (AMA) states that "Physicians generally should not treat themselves or members of their immediate family".
This code seeks to protect patients and physicians because professional
objectivity can be compromised when the physician is treating a loved
one. Studies from multiple health organizations have illustrated that
physician-family member relationships may cause an increase in
diagnostic testing and costs.
Many doctors still treat their family members. Doctors who do so must
be vigilant not to create conflicts of interest or treat
inappropriately.
Physicians that treat family members need to be conscious of
conflicting expectations and dilemmas when treating relatives, as
established medical ethical principles may not be morally imperative
when family members are confronted with serious illness.
Sexual relationships
Sexual relationships between doctors and patients can create ethical conflicts, since sexual consent may conflict with the fiduciary
responsibility of the physician. Out of the many disciplines in current
medicine, there are studies that have been conducted in order to
ascertain the occurrence of Doctor-Patient sexual misconduct. Results
from those studies appear to indicate that certain disciplines are more
likely to be offenders than others. Psychiatrists and
Obstetrician-Gynecologists for example, are two disciplines noted for
having a higher rate of sexual misconduct.
The violation of ethical conduct between doctors and patients also has
an association with the age and sex of doctor and patient. Male
physicians aged 40–49 and 50–59 years are two groups that have been
found to be more likely to have been reported for sexual misconduct,
while women aged 20–39 have been found to make up a significant portion
of reported victims of sexual misconduct. Doctors who enter into sexual relationships with patients face the threats of losing their medical license and prosecution. In the early 1990s, it was estimated that 2-9% of doctors had violated this rule.
Sexual relationships between physicians and patients' relatives may
also be prohibited in some jurisdictions, although this prohibition is
highly controversial.
Futility
The concept of medical futility has been an important topic in
discussions of medical ethics. What should be done if there is no chance
that a patient will survive but the family members insist on advanced
care? Previously, some articles defined futility as the patient having
less than a one percent chance of surviving. Some of these cases are
examined in court.
Advance directives include living wills and durable powers of attorney for health care.
In many cases, the "expressed wishes" of the patient are documented in
these directives, and this provides a framework to guide family members
and health care
professionals in the decision-making process when the patient is
incapacitated. Undocumented expressed wishes can also help guide
decisions in the absence of advance directives, as in the Quinlan case in Missouri.
"Substituted judgment" is the concept that a family member can
give consent for treatment if the patient is unable (or unwilling) to
give consent themselves. The key question for the decision-making
surrogate is not, "What would you like to do?", but instead, "What do
you think the patient would want in this situation?".
Courts have supported family's arbitrary definitions of futility to include simple biological survival, as in the Baby K
case (in which the courts ordered a child born with only a brain stem
instead of a complete brain to be kept on a ventilator based on the
religious belief that all life must be preserved).
In some hospitals, medical futility is referred to as "non-beneficial care."
Baby Doe Law
establishes state protection for a disabled child's right to life,
ensuring that this right is protected even over the wishes of parents or
guardians in cases where they want to withhold treatment.