The term diabetes
includes several different metabolic disorders that all, if left
untreated, result in abnormally high concentration of a sugar called glucose in the blood. Diabetes mellitus type 1 results when the pancreas no longer produces significant amounts of the hormone insulin, usually owing to the autoimmune destruction of the insulin-producing beta cells of the pancreas. Diabetes mellitus type 2, in contrast, is now thought to result from autoimmune attacks on the pancreas and/or insulin resistance.
The pancreas of a person with type 2 diabetes may be producing normal
or even abnormally large amounts of insulin. Other forms of diabetes
mellitus, such as the various forms of maturity onset diabetes of the young,
may represent some combination of insufficient insulin production and
insulin resistance. Some degree of insulin resistance may also be
present in a person with type 1 diabetes.
The main goal of diabetes management is, as far as possible, to restore carbohydrate metabolism to a normal state. To achieve this goal, individuals with an absolute deficiency of insulin require insulin replacement therapy, which is given through injections or an insulin pump. Insulin resistance, in contrast, can be corrected by dietary modifications and exercise. Other goals of diabetes management are to prevent or treat the many complications that can result from the disease itself and from its treatment.
The main goal of diabetes management is, as far as possible, to restore carbohydrate metabolism to a normal state. To achieve this goal, individuals with an absolute deficiency of insulin require insulin replacement therapy, which is given through injections or an insulin pump. Insulin resistance, in contrast, can be corrected by dietary modifications and exercise. Other goals of diabetes management are to prevent or treat the many complications that can result from the disease itself and from its treatment.
Overview
Goals
The treatment goals are related to effective control of blood glucose, blood pressure and lipids, to minimize the risk of long-term consequences associated with diabetes. They are suggested in clinical practice guidelines released by various national and international diabetes agencies.
The targets are:
- HbA1c of less than 6% or 7.0% if they are achievable without significant hypoglycemia
- Preprandial blood glucose: 3.9 to 7.2 mmol/L (70 to 130 mg/dl)
- 2-hour postprandial blood glucose: <10 dl="" mg="" mmol="" nbsp="" span="">
Goals should be individualized based on:
- Duration of diabetes
- Age/life expectancy
- Comorbidity
- Known cardiovascular disease or advanced microvascular disease
- Hypoglycemia awareness
In older patients, clinical practice guidelines by the American Geriatrics Society
states "for frail older adults, persons with life expectancy of less
than 5 years, and others in whom the risks of intensive glycemic control
appear to outweigh the benefits, a less stringent target such as HbA1c of 8% is appropriate".
Issues
The
primary issue requiring management is that of the glucose cycle. In
this, glucose in the bloodstream is made available to cells in the body;
a process dependent upon the twin cycles of glucose entering the
bloodstream, and insulin allowing appropriate uptake into the body
cells. Both aspects can require management. Another issue that ties
along with the glucose cycle is getting a balanced amount of the glucose
to the major organs so they are not affected negatively.
Complexities
Daily glucose and insulin cycle
The main complexities stem from the nature of the feedback loop of the glucose cycle, which is sought to be regulated:
- The glucose cycle is a system which is affected by two factors: entry of glucose into the bloodstream and also blood levels of insulin to control its transport out of the bloodstream
- As a system, it is sensitive to diet and exercise
- It is affected by the need for user anticipation due to the complicating effects of time delays between any activity and the respective impact on the glucose system
- Management is highly intrusive, and compliance is an issue, since it relies upon user lifestyle change and often upon regular sampling and measuring of blood glucose levels, multiple times a day in many cases
- It changes as people grow and develop
- It is highly individual
As diabetes is a prime risk factor for cardiovascular disease,
controlling other risk factors which may give rise to secondary
conditions, as well as the diabetes itself, is one of the facets of
diabetes management. Checking cholesterol, LDL, HDL and triglyceride levels may indicate hyperlipoproteinemia, which may warrant treatment with hypolipidemic drugs. Checking the blood pressure and keeping it within strict limits (using diet and antihypertensive treatment) protects against the retinal, renal and cardiovascular complications of diabetes. Regular follow-up by a podiatrist or other foot health specialists is encouraged to prevent the development of diabetic foot. Annual eye exams are suggested to monitor for progression of diabetic retinopathy.
Early advancements
Late
in the 19th century, sugar in the urine (glycosuria) was associated
with diabetes. Various doctors studied the connection. Frederick Madison Allen studied diabetes in 1909–12, then published a large volume, Studies Concerning Glycosuria and Diabetes, (Boston, 1913). He invented a fasting treatment for diabetes called the Allen treatment for diabetes. His diet was an early attempt at managing diabetes.
Blood sugar level
Blood sugar level is measured by means of a glucose meter,
with the result either in mg/dL (milligrams per deciliter in the US) or
mmol/L (millimoles per litre in Canada and Eastern Europe) of blood.
The average normal person has an average fasting glucose level of
4.5 mmol/L (81 mg/dL), with a lows of down to 2.5 and up to 5.4 mmol/L
(65 to 98 mg/dL).
Optimal management of diabetes involves patients measuring and recording their own blood glucose
levels. By keeping a diary of their own blood glucose measurements and
noting the effect of food and exercise, patients can modify their
lifestyle to better control their diabetes. For patients on insulin,
patient involvement is important in achieving effective dosing and
timing.
Hypo and hyperglycemia
Levels
which are significantly above or below this range are problematic and
can in some cases be dangerous. A level of <3 .8="" a="" as="" described="" dl="" i="" is="" mg="" mmol="" nbsp="" usually="">hypoglycemic attack
(low blood sugar).
Most diabetics know when they are going to "go hypo" and usually are
able to eat some food or drink something sweet to raise levels. A
patient who is hyperglycemic (high glucose) can also become
temporarily hypoglycemic, under certain conditions (e.g. not eating
regularly, or after strenuous exercise, followed by fatigue). Intensive
efforts to achieve blood sugar levels close to normal have been shown
to triple the risk of the most severe form of hypoglycemia, in which the
patient requires assistance from by-standers in order to treat the
episode.
In the United States, there were annually 48,500 hospitalizations for
diabetic hypoglycemia and 13,100 for diabetic hypoglycemia resulting in
coma in the period 1989 to 1991, before intensive blood sugar control
was as widely recommended as today.
One study found that hospital admissions for diabetic hypoglycemia
increased by 50% from 1990–1993 to 1997–2000, as strict blood sugar
control efforts became more common.
Among intensively controlled type 1 diabetics, 55% of episodes of
severe hypoglycemia occur during sleep, and 6% of all deaths in
diabetics under the age of 40 are from nocturnal hypoglycemia in the
so-called 'dead-in-bed syndrome,' while National Institute of Health
statistics show that 2% to 4% of all deaths in diabetics are from
hypoglycemia. In children and adolescents following intensive blood sugar control, 21% of hypoglycemic episodes occurred without explanation.
In addition to the deaths caused by diabetic hypoglycemia, periods of
severe low blood sugar can also cause permanent brain damage.
Although diabetic nerve disease is usually associated with
hyperglycemia, hypoglycemia as well can initiate or worsen neuropathy in
diabetics intensively struggling to reduce their hyperglycemia.
Levels greater than 13–15 mmol/L (230–270 mg/dL) are considered
high, and should be monitored closely to ensure that they reduce rather
than continue to remain high. The patient is advised to seek urgent
medical attention as soon as possible if blood sugar levels continue to
rise after 2–3 tests. High blood sugar levels are known as hyperglycemia,
which is not as easy to detect as hypoglycemia and usually happens over
a period of days rather than hours or minutes. If left untreated, this
can result in diabetic coma and death.
A blood glucose test strip for an older style (i.e., optical color sensing) monitoring system
Prolonged and elevated levels of glucose in the blood, which is left
unchecked and untreated, will, over time, result in serious diabetic
complications in those susceptible and sometimes even death. There is
currently no way of testing for susceptibility to complications.
Diabetics are therefore recommended to check their blood sugar levels
either daily or every few days. There is also diabetes management software
available from blood testing manufacturers which can display results
and trends over time. Type 1 diabetics normally check more often, due to
insulin therapy.
A history of blood sugar level results is especially useful for
the diabetic to present to their doctor or physician in the monitoring
and control of the disease. Failure to maintain a strict regimen of
testing can accelerate symptoms of the condition, and it is therefore
imperative that any diabetic patient strictly monitor their glucose
levels regularly.
Glycemic control
Glycemic control is a medical term referring to the typical levels of blood sugar (glucose) in a person with diabetes mellitus.
Much evidence suggests that many of the long-term complications of
diabetes, especially the microvascular complications, result from many
years of hyperglycemia
(elevated levels of glucose in the blood). Good glycemic control, in
the sense of a "target" for treatment, has become an important goal of
diabetes care, although recent research suggests that the complications
of diabetes may be caused by genetic factors or, in type 1 diabetics, by the continuing effects of the autoimmune disease which first caused the pancreas to lose its insulin-producing ability.
Because blood sugar levels fluctuate throughout the day and
glucose records are imperfect indicators of these changes, the
percentage of hemoglobin which is glycosylated
is used as a proxy measure of long-term glycemic control in research
trials and clinical care of people with diabetes. This test, the hemoglobin A1c or glycosylated hemoglobin
reflects average glucoses over the preceding 2–3 months. In nondiabetic
persons with normal glucose metabolism the glycosylated hemoglobin is
usually 4–6% by the most common methods (normal ranges may vary by
method).
"Perfect glycemic control" would mean that glucose levels were
always normal (70–130 mg/dl, or 3.9–7.2 mmol/L) and indistinguishable
from a person without diabetes. In reality, because of the imperfections
of treatment measures, even "good glycemic control" describes blood
glucose levels that average somewhat higher than normal much of the
time. In addition, one survey of type 2 diabetics found that they rated
the harm to their quality of life from intensive interventions to
control their blood sugar to be just as severe as the harm resulting
from intermediate levels of diabetic complications.
In the 1990s the American Diabetes Association
conducted a publicity campaign to persuade patients and physicians to
strive for average glucose and hemoglobin A1c values below 200 mg/dl
(11 mmol/l) and 8%. Currently many patients and physicians attempt to do
better than that.
As of 2015 the guidelines called for an HbA1c of
around 7% or a fasting glucose of less than 7.2 mmol/L (130 mg/dL);
however these goals may be changed after professional clinical
consultation, taking into account particular risks of hypoglycemia and life expectancy.
Despite guidelines recommending that intensive blood sugar control be
based on balancing immediate harms and long-term benefits, many people –
for example people with a life expectancy of less than nine years – who
will not benefit are over-treated and do not experience clinically meaningful benefits.
Poor glycemic control refers to persistently elevated blood
glucose and glycosylated hemoglobin levels, which may range from
200–500 mg/dl (11–28 mmol/L) and 9–15% or higher over months and years
before severe complications occur. Meta-analysis of large studies done
on the effects of tight
vs. conventional, or more relaxed, glycemic control in type 2 diabetics
have failed to demonstrate a difference in all-cause cardiovascular
death, non-fatal stroke, or limb amputation, but decreased the risk of
nonfatal heart attack by 15%. Additionally, tight glucose control
decreased the risk of progression of retinopathy and nephropathy, and
decreased the incidence peripheral neuropathy, but increased the risk of
hypoglycemia 2.4 times.
Monitoring
A modern portable blood glucose meter (OneTouch Ultra), displaying a reading of 5.4 mmol/L (98 mg/dL).
Relying on their own perceptions of symptoms of hyperglycemia or
hypoglycemia is usually unsatisfactory as mild to moderate hyperglycemia
causes no obvious symptoms in nearly all patients. Other considerations
include the fact that, while food takes several hours to be digested
and absorbed, insulin administration can have glucose lowering effects
for as little as 2 hours or 24 hours or more (depending on the nature of
the insulin preparation used and individual patient reaction). In
addition, the onset and duration of the effects of oral hypoglycemic
agents vary from type to type and from patient to patient.
Personal (home) glucose monitoring
Control and outcomes of both types 1 and 2 diabetes may be improved by patients using home glucose meters to regularly measure their glucose levels.
Glucose monitoring is both expensive (largely due to the cost of the
consumable test strips) and requires significant commitment on the part
of the patient. Lifestyle adjustments are generally made by the patients
themselves following training by a clinician.
Regular blood testing, especially in type 1 diabetics, is helpful
to keep adequate control of glucose levels and to reduce the chance of
long term side effects of the disease. There are many (at least 20+) different types of blood monitoring devices
available on the market today; not every meter suits all patients and
it is a specific matter of choice for the patient, in consultation with a
physician or other experienced professional, to find a meter that they
personally find comfortable to use. The principle of the devices is
virtually the same: a small blood sample is collected and measured. In
one type of meter, the electrochemical, a small blood sample is produced
by the patient using a lancet (a sterile pointed needle). The blood
droplet is usually collected at the bottom of a test strip, while the
other end is inserted in the glucose meter. This test strip contains
various chemicals so that when the blood is applied, a small electrical
charge is created between two contacts. This charge will vary depending
on the glucose levels within the blood. In older glucose meters, the
drop of blood is placed on top of a strip. A chemical reaction occurs
and the strip changes color. The meter then measures the color of the
strip optically.
Self-testing is clearly important in type I diabetes where the
use of insulin therapy risks episodes of hypoglycemia and home-testing
allows for adjustment of dosage on each administration. Its benefit in type 2 diabetes has been more controversial, but recent studies have resulted in guidance that self-monitoring does not improve blood glucose or quality of life.
Benefits of control and reduced hospital admission have been reported.
However, patients on oral medication who do not self-adjust their drug
dosage will miss many of the benefits of self-testing, and so it is
questionable in this group. This is particularly so for patients taking
monotherapy with metformin who are not at risk of hypoglycaemia. Regular 6 monthly laboratory testing of HbA1c
(glycated haemoglobin) provides some assurance of long-term effective
control and allows the adjustment of the patient's routine medication
dosages in such cases. High frequency of self-testing in type 2 diabetes
has not been shown to be associated with improved control.
The argument is made, though, that type 2 patients with poor long term
control despite home blood glucose monitoring, either have not had this
integrated into their overall management, or are long overdue for
tighter control by a switch from oral medication to injected insulin.
Continuous Glucose Monitoring (CGM)
CGM technology has been rapidly developing to give people living with
diabetes an idea about the speed and direction of their glucose changes.
While it still requires calibration from SMBG and is not indicated for
use in correction boluses, the accuracy of these monitors is increasing
with every innovation. The Libre Blood Sugar Diet Program utilizes the
CGM and Libre Sensor and by collecting all the data through a smart
phone and smart watch experts analyze this data 24/7 in Real Time. The
results are that certain foods can be identified as causing one's blood
sugar levels to rise and other foods as safe foods- that do not make a
person's blood sugar levels to rise. Each individual absorbs sugar
differently and this is why testing is a necessity.
HbA1c test
A useful test that has usually been done in a laboratory is the measurement of blood HbA1c levels. This is the ratio of glycated hemoglobin
in relation to the total hemoglobin. Persistent raised plasma glucose
levels cause the proportion of these molecules to go up. This is a test
that measures the average amount of diabetic control over a period
originally thought to be about 3 months (the average red blood cell
lifetime), but more recently
thought to be more strongly weighted to the most recent 2 to 4 weeks.
In the non-diabetic, the HbA1c level ranges from 4.0–6.0%; patients with
diabetes mellitus who manage to keep their HbA1c level below 6.5% are
considered to have good glycemic control. The HbA1c test is not
appropriate if there has been changes to diet or treatment within
shorter time periods than 6 weeks or there is disturbance of red cell
aging (e.g. recent bleeding or hemolytic anemia) or a hemoglobinopathy (e.g. sickle cell disease). In such cases the alternative Fructosamine test is used to indicate average control in the preceding 2 to 3 weeks.
Continuous glucose monitoring
The first CGM device made available to consumers was the GlucoWatch
biographer in 1999. This product is no longer sold. It was a
retrospective device rather than live. Several live monitoring devices
have subsequently been manufactured which provide ongoing monitoring of
glucose levels on an automated basis during the day.
Lifestyle modification
The British National Health Service
launched a programme targeting 100,000 people at risk of diabetes to
lose weight and take more exercise in 2016. In 2019 it was announced
that the programme was successful. The 17,000 people who attended most
of the healthy living sessions had, collectively lost nearly 60,000 kg,
and the programme was to be doubled in size.
Diet
Because high blood sugar caused by poorly controlled diabetes can
lead to a plethora of immediate and long-term complications, it is
critical to maintain blood sugars as close to normal as possible, and a
diet that produces more controllable glycemic variability is an
important factor in producing normal blood sugars.
People with type 1 diabetes who use insulin can eat whatever they want, preferably a healthy diet
with some carbohydrate content; in the long term it is helpful to eat a
consistent amount of carbohydrate to make blood sugar management
easier.
There is a lack of evidence of the usefulness of low-carbohydrate dieting for people with type 1 diabetes. Although for certain individuals it may be feasible to follow a low-carbohydrate regime combined with carefully-managed insulin dosing, this is hard to maintain and there are concerns about potential adverse health effects caused by the diet. In general people with type 1 diabetes are advised to follow an individualized eating plan rather than a pre-decided one.
Medications
Currently, one goal for diabetics is to avoid or minimize chronic diabetic complications, as well as to avoid acute problems of hyperglycemia or hypoglycemia. Adequate control of diabetes leads to lower risk of complications associated with unmonitored diabetes including kidney failure (requiring dialysis or transplant), blindness, heart disease and limb amputation. The most prevalent form of medication is hypoglycemic treatment through either oral hypoglycemics and/or insulin
therapy. There is emerging evidence that full-blown diabetes mellitus
type 2 can be evaded in those with only mildly impaired glucose
tolerance.
Patients with type 1 diabetes mellitus require direct injection
of insulin as their bodies cannot produce enough (or even any) insulin.
As of 2010, there is no other clinically available form of insulin
administration other than injection for patients with type 1: injection
can be done by insulin pump, by jet injector, or any of several forms of hypodermic needle.
Non-injective methods of insulin administration have been unattainable
as the insulin protein breaks down in the digestive tract. There are
several insulin application mechanisms under experimental development as
of 2004, including a capsule that passes to the liver and delivers
insulin into the bloodstream. There have also been proposed vaccines for type I using glutamic acid decarboxylase (GAD), but these are currently not being tested by the pharmaceutical companies that have sublicensed the patents to them.
For type 2 diabetics, diabetic management consists of a combination of diet, exercise, and weight loss,
in any achievable combination depending on the patient. Obesity is very
common in type 2 diabetes and contributes greatly to insulin
resistance. Weight reduction and exercise improve tissue sensitivity to
insulin and allow its proper use by target tissues.
Patients who have poor diabetic control after lifestyle modifications
are typically placed on oral hypoglycemics. Some Type 2 diabetics
eventually fail to respond to these and must proceed to insulin therapy.
A study conducted in 2008 found that increasingly complex and costly
diabetes treatments are being applied to an increasing population with
type 2 diabetes. Data from 1994 to 2007 was analyzed and it was found
that the mean number of diabetes medications per treated patient
increased from 1.14 in 1994 to 1.63 in 2007.
Patient education and compliance with treatment is very important
in managing the disease. Improper use of medications and insulin can be
very dangerous causing hypo- or hyper-glycemic episodes.
Insulin
Insulin pen used to administer insulin
For type 1 diabetics, there will always be a need for insulin
injections throughout their life, as the pancreatic beta cells of a type
1 diabetic are not capable of producing sufficient insulin. However,
both type 1 and type 2 diabetics can see dramatic improvements in blood
sugars through modifying their diet, and some type 2 diabetics can fully
control the disease by dietary modification.
Insulin therapy
requires close monitoring and a great deal of patient education, as
improper administration is quite dangerous. For example, when food
intake is reduced, less insulin is required. A previously satisfactory
dosing may be too much if less food is consumed causing a hypoglycemic
reaction if not intelligently adjusted. Exercise decreases insulin
requirements as exercise increases glucose uptake by body cells whose
glucose uptake is controlled by insulin, and vice versa. In addition,
there are several types of insulin with varying times of onset and
duration of action.
Several companies are currently working to develop a
non-invasive version of insulin, so that injections can be avoided.
Mannkind has developed an inhalable version, while companies like Novo Nordisk,
Oramed and BioLingus have efforts undergoing for an oral product.
Also oral combination products of insulin and a GLP-1 agonist are being
developed.
Insulin therapy creates risk because of the inability to
continuously know a person's blood glucose level and adjust insulin
infusion appropriately. New advances in technology have overcome much
of this problem. Small, portable insulin infusion pumps are available
from several manufacturers. They allow a continuous infusion of small
amounts of insulin to be delivered through the skin around the clock,
plus the ability to give bolus doses when a person eats or has elevated
blood glucose levels. This is very similar to how the pancreas works,
but these pumps lack a continuous "feed-back" mechanism. Thus, the user
is still at risk of giving too much or too little insulin unless blood
glucose measurements are made.
A further danger of insulin treatment is that while diabetic
microangiopathy is usually explained as the result of hyperglycemia,
studies in rats indicate that the higher than normal level of insulin
diabetics inject to control their hyperglycemia may itself promote small
blood vessel disease.
While there is no clear evidence that controlling hyperglycemia
reduces diabetic macrovascular and cardiovascular disease, there are
indications that intensive efforts to normalize blood glucose levels may
worsen cardiovascular and cause diabetic mortality.
Driving
Paramedics
in Southern California attend a diabetic man who lost effective control
of his vehicle due to low blood sugar (hypoglycemia) and drove it over
the curb and into the water main and backflow valve in front of this
industrial building. He was not injured, but required emergency
intravenous glucose.
Studies conducted in the United States and Europe
showed that drivers with type 1 diabetes had twice as many collisions
as their non-diabetic spouses, demonstrating the increased risk of
driving collisions in the type 1 diabetes population. Diabetes can
compromise driving safety in several ways. First, long-term
complications of diabetes can interfere with the safe operation of a
vehicle. For example, diabetic retinopathy (loss of peripheral vision or visual acuity), or peripheral neuropathy
(loss of feeling in the feet) can impair a driver’s ability to read
street signs, control the speed of the vehicle, apply appropriate
pressure to the brakes, etc.
Second, hypoglycemia can affect a person’s thinking process, coordination, and state of consciousness. This disruption in brain functioning is called neuroglycopenia. Studies have demonstrated that the effects of neuroglycopenia impair driving ability.
A study involving people with type 1 diabetes found that individuals
reporting two or more hypoglycemia-related driving mishaps differ
physiologically and behaviorally from their counterparts who report no
such mishaps.
For example, during hypoglycemia, drivers who had two or more mishaps
reported fewer warning symptoms, their driving was more impaired, and
their body released less epinephrine (a hormone that helps raise BG).
Additionally, individuals with a history of hypoglycemia-related driving
mishaps appear to use sugar at a faster rate and are relatively slower at processing information.
These findings indicate that although anyone with type 1 diabetes may
be at some risk of experiencing disruptive hypoglycemia while driving,
there is a subgroup of type 1 drivers who are more vulnerable to such
events.
Given the above research findings, it is recommended that drivers
with type 1 diabetes with a history of driving mishaps should never
drive when their BG is less than 70 mg/dl (3.9 mmol/l). Instead, these
drivers are advised to treat hypoglycemia and delay driving until their
BG is above 90 mg/dl (5 mmol/l).
Such drivers should also learn as much as possible about what causes
their hypoglycemia, and use this information to avoid future
hypoglycemia while driving.
Studies funded by the National Institutes of Health (NIH) have
demonstrated that face-to-face training programs designed to help
individuals with type 1 diabetes better anticipate, detect, and prevent
extreme BG can reduce the occurrence of future hypoglycemia-related
driving mishaps. An internet-version of this training has also been shown to have significant beneficial results.
Additional NIH funded research to develop internet interventions
specifically to help improve driving safety in drivers with type 1
diabetes is currently underway.
Exenatide
The U.S. Food and Drug Administration (FDA) has approved a treatment called Exenatide, based on the saliva of a Gila monster, to control blood sugar in patients with type 2 diabetes.
Other regimens
Artificial Intelligence researcher Dr. Cynthia Marling, of the Ohio University Russ College of Engineering and Technology, in collaboration with the Appalachian Rural Health Institute Diabetes Center, is developing a case based reasoning
system to aid in diabetes management. The goal of the project is to
provide automated intelligent decision support to diabetes patients and
their professional care providers by interpreting the ever-increasing
quantities of data provided by current diabetes management technology
and translating it into better care without time consuming manual effort
on the part of an endocrinologist or diabetologist. This type of Artificial Intelligence-based treatment shows some promise with initial testing of a prototype system producing best practice
treatment advice which anaylizing physicians deemed to have some degree
of benefit over 70% of the time and advice of neutral benefit another
nearly 25% of the time.
Use of a "Diabetes Coach" is becoming an increasingly popular way to manage diabetes. A Diabetes Coach is usually a Certified diabetes educator
(CDE) who is trained to help people in all aspects of caring for their
diabetes. The CDE can advise the patient on diet, medications, proper
use of insulin injections and pumps, exercise, and other ways to manage
diabetes while living a healthy and active lifestyle. CDEs can be found
locally or by contacting a company which provides personalized diabetes
care using CDEs. Diabetes Coaches can speak to a patient on a
pay-per-call basis or via a monthly plan.
Dental care
High blood glucose in diabetic people is a risk factor for developing gum and tooth problems, especially in post-puberty and aging individuals. Diabetic patients have greater chances of developing oral health problems such as tooth decay, salivary gland dysfunction, fungal infections, inflammatory skin disease, periodontal disease or taste impairment and thrush of the mouth.
The oral problems in persons suffering from diabetes can be prevented
with a good control of the blood sugar levels, regular check-ups and a
very good oral hygiene. By maintaining a good oral status, diabetic persons prevent losing their teeth as a result of various periodontal conditions.
Diabetic persons must increase their awareness about oral
infections as they have a double impact on health. Firstly, people with
diabetes are more likely to develop periodontal disease, which causes
increased blood sugar levels, often leading to diabetes complications.
Severe periodontal disease can increase blood sugar, contributing to
increased periods of time when the body functions with a high blood
sugar. This puts diabetics at increased risk for diabetic complications.
The first symptoms of gum and tooth infection in diabetic persons are decreased salivary flow and burning mouth or tongue.
Also, patients may experience signs like dry mouth, which increases the
incidence of decay. Poorly controlled diabetes usually leads to gum
recession, since plaque creates more harmful proteins in the gums.
Tooth decay and cavities are some of the first oral problems that
individuals with diabetes are at risk for. Increased blood sugar levels
translate into greater sugars and acids that attack the teeth and lead
to gum diseases. Gingivitis can also occur as a result of increased blood sugar levels along with an inappropriate oral hygiene. Periodontitis
is an oral disease caused by untreated gingivitis and which destroys
the soft tissue and bone that support the teeth. This disease may cause
the gums to pull away from the teeth which may eventually loosen and
fall out. Diabetic people tend to experience more severe periodontitis
because diabetes lowers the ability to resist infection
and also slows healing. At the same time, an oral infection such as
periodontitis can make diabetes more difficult to control because it
causes the blood sugar levels to rise.
To prevent further diabetic complications as well as serious oral
problems, diabetic persons must keep their blood sugar levels under
control and have a proper oral hygiene. A study in the Journal of
Periodontology found that poorly controlled type 2 diabetic patients are
more likely to develop periodontal disease than well-controlled
diabetics are.
At the same time, diabetic patients are recommended to have regular
checkups with a dental care provider at least once in three to four
months. Diabetics who receive good dental care and have good insulin
control typically have a better chance at avoiding gum disease to help
prevent tooth loss.
Dental care is therefore even more important for diabetic
patients than for healthy individuals. Maintaining the teeth and gum
healthy is done by taking some preventing measures such as regular
appointments at a dentist and a very good oral hygiene. Also, oral
health problems can be avoided by closely monitoring the blood sugar
levels. Patients who keep better under control their blood sugar levels
and diabetes are less likely to develop oral health problems when
compared to diabetic patients who control their disease moderately or
poorly.
Poor oral hygiene is a great factor to take under consideration
when it comes to oral problems and even more in people with diabetes.
Diabetic people are advised to brush their teeth at least twice a day,
and if possible, after all meals and snacks. However, brushing in the morning and at night is mandatory as well as flossing and using an anti-bacterial mouthwash. Individuals who suffer from diabetes are recommended to use toothpaste that contains fluoride
as this has proved to be the most efficient in fighting oral infections
and tooth decay. Flossing must be done at least once a day, as well
because it is helpful in preventing oral problems by removing the plaque
between the teeth, which is not removed when brushing.
Diabetic patients must get professional dental cleanings every six months. In cases when dental surgery is needed, it is necessary to take some special precautions such as adjusting diabetes medication or taking antibiotics to prevent infection. Looking for early signs of gum disease (redness, swelling, bleeding gums) and informing the dentist about them is also helpful in preventing further complications. Quitting smoking is recommended to avoid serious diabetes complications and oral diseases.
Diabetic persons are advised to make morning appointments to the
dental care provider as during this time of the day the blood sugar
levels tend to be better kept under control. Not least, individuals who
suffer from diabetes must make sure both their physician and dental care
provider are informed and aware of their condition, medical history and
periodontal status.
Medication nonadherence
Because
many patients with diabetes have two or more comorbidities, they often
require multiple medications. The prevalence of medication nonadherence
is high among patients with chronic conditions, such as diabetes, and
nonadherence is associated with public health issues and higher health
care costs. One reason for nonadherence is the cost of medications.
Being able to detect cost-related nonadherence is important for health
care professionals, because this can lead to strategies to assist
patients with problems paying for their medications. Some of these
strategies are use of generic drugs or therapeutic alternatives,
substituting a prescription drug with an over-the-counter medication,
and pill-splitting. Interventions to improve adherence can achieve
reductions in diabetes morbidity and mortality, as well as significant
cost savings to the health care system.
Smartphone apps have been found to improve self-management and health
outcomes in people with diabetes through functions such as specific
reminder alarms,
while working with mental health professionals has also been found to
help people with diabetes develop the skills to manage their medications
and challenges of self-management effectively.
Psychological mechanisms and adherence
As
self-management of diabetes typically involves lifestyle modifications,
adherence may pose a significant self-management burden on many
individuals.
For example, individuals with diabetes may find themselves faced with
the need to self-monitor their blood glucose levels, adhere to healthier
diets and maintain exercise regimens regularly in order to maintain
metabolic control and reduce the risk of developing cardiovascular
problems. Barriers to adherence have been associated with key
psychological mechanisms: knowledge of self-management, beliefs about
the efficacy of treatment and self-efficacy/perceived control.
Such mechanisms are inter-related, as one's thoughts (e.g. one's
perception of diabetes, or one's appraisal of how helpful
self-management is) is likely to relate to one's emotions (e.g.
motivation to change), which in turn, affects one's self-efficacy (one's
confidence in their ability to engage in a behaviour to achieve a
desired outcome).
As diabetes management is affected by an individual's emotional
and cognitive state, there has been evidence suggesting the
self-management of diabetes is negatively affected by diabetes-related
distress and depression.
There is growing evidence that there is higher levels of clinical
depression in patients with diabetes compared to the non-diabetic
population. Depression in individuals with diabetes has been found to be associated with poorer self-management of symptoms. This suggests that it may be important to target mood in treatment.
To this end, treatment programs such as the Cognitive Behavioural Therapy - Adherence and Depression program (CBT-AD)
have been developed to target the psychological mechanisms underpinning
adherence. By working on increasing motivation and challenging
maladaptive illness perceptions, programs such as CBT-AD aim to enhance
self-efficacy and improve diabetes-related distress and one's overall
quality of life.
Research
Type 1 diabetes
Diabetes type 1 is caused by the destruction of enough beta cells to produce symptoms; these cells, which are found in the Islets of Langerhans in the pancreas, produce and secrete insulin, the single hormone responsible for allowing glucose to enter from the blood into cells (in addition to the hormone amylin, another hormone required for glucose homeostasis). Hence, the phrase "curing diabetes type 1" means "causing a maintenance or restoration of the endogenous
ability of the body to produce insulin in response to the level of
blood glucose" and cooperative operation with counterregulatory
hormones.
This section deals only with approaches for curing the underlying
condition of diabetes type 1, by enabling the body to endogenously, in vivo,
produce insulin in response to the level of blood glucose. It does not
cover other approaches, such as, for instance, closed-loop integrated
glucometer/insulin pump products, which could potentially increase the
quality-of-life for some who have diabetes type 1, and may by some be
termed "artificial pancreas".
Encapsulation approach
The Bio-artificial pancreas: a cross section of bio-engineered tissue with encapsulated islet cells delivering endocrine hormones in response to glucose
A biological approach to the artificial pancreas is to implant bioengineered tissue containing islet cells, which would secrete the amounts of insulin, amylin and glucagon needed in response to sensed glucose.
When islet cells have been transplanted via the Edmonton protocol, insulin production (and glycemic control) was restored, but at the expense of continued immunosuppression drugs. Encapsulation
of the islet cells in a protective coating has been developed to block
the immune response to transplanted cells, which relieves the burden of
immunosuppression and benefits the longevity of the transplant.
Stem cells
Research is being done at several locations in which islet cells are developed from stem cells.
Stem cell research has also been suggested as a potential avenue
for a cure since it may permit regrowth of Islet cells which are
genetically part of the treated individual, thus perhaps eliminating the
need for immuno-suppressants.[48] This new method autologous
nonmyeloablative hematopoietic stem cell transplantation was developed
by a research team composed by Brazilian and American scientists (Dr.
Julio Voltarelli, Dr. Carlos Eduardo Couri, Dr Richard Burt, and
colleagues) and it was the first study to use stem cell therapy in human
diabetes mellitus This was initially tested in mice and in 2007 there
was the first publication of stem cell therapy to treat this form of
diabetes.
Until 2009, there was 23 patients included and followed for a mean
period of 29.8 months (ranging from 7 to 58 months). In the trial,
severe immunosuppression with high doses of cyclophosphamide and
anti-thymocyte globulin is used with the aim of "turning off" the
immunologic system", and then autologous hematopoietic stem cells are
reinfused to regenerate a new one. In summary it is a kind of
"immunologic reset" that blocks the autoimmune attack against residual
pancreatic insulin-producing cells. Until December 2009, 12 patients
remained continuously insulin-free for periods ranging from 14 to 52
months and 8 patients became transiently insulin-free for periods
ranging from 6 to 47 months. Of these last 8 patients, 2 became
insulin-free again after the use of sitagliptin, a DPP-4 inhibitor
approved only to treat type 2 diabetic patients and this is also the
first study to document the use and complete insulin-independendce in
humans with type 1 diabetes with this medication. In parallel with
insulin suspension, indirect measures of endogenous insulin secretion
revealed that it significantly increased in the whole group of patients,
regardless the need of daily exogenous insulin use.
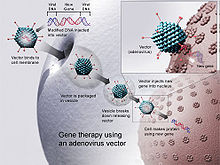
Gene therapy
Gene therapy: Designing a viral vector to deliberately infect cells with DNA to carry on the viral production of insulin in response to the blood sugar level.
Technology for gene therapy
is advancing rapidly such that there are multiple pathways possible to
support endocrine function, with potential to practically cure diabetes.
- Gene therapy can be used to manufacture insulin directly: an oral medication, consisting of viral vectors containing the insulin sequence, is digested and delivers its genes to the upper intestines. Those intestinal cells will then behave like any viral infected cell, and will reproduce the insulin protein. The virus can be controlled to infect only the cells which respond to the presence of glucose, such that insulin is produced only in the presence of high glucose levels. Due to the limited numbers of vectors delivered, very few intestinal cells would actually be impacted and would die off naturally in a few days. Therefore, by varying the amount of oral medication used, the amount of insulin created by gene therapy can be increased or decreased as needed. As the insulin-producing intestinal cells die off, they are boosted by additional oral medications.
- Gene therapy might eventually be used to cure the cause of beta cell destruction, thereby curing the new diabetes patient before the beta cell destruction is complete and irreversible.
- Gene therapy can be used to turn duodenum cells and duodenum adult stem cells into beta cells which produce insulin and amylin naturally. By delivering beta cell DNA to the intestine cells in the duodenum, a few intestine cells will turn into beta cells, and subsequently adult stem cells will develop into beta cells. This makes the supply of beta cells in the duodenum self replenishing, and the beta cells will produce insulin in proportional response to carbohydrates consumed.
Type 2 diabetes
Type 2 diabetes is usually first treated by increasing physical activity, and eliminating saturated fat and reducing sugar and carbohydrate intake with a goal of losing weight.
These can restore insulin sensitivity even when the weight loss is
modest, for example around 5 kg (10 to 15 lb), most especially when it
is in abdominal fat deposits. Diets that are very low in saturated fats
have been claimed to reverse insulin resistance.
Cognitive Behavioural Therapy is an effective intervention for
improving adherence to medication, depression and glycaemic control,
with enduring and clinically meaningful benefits for diabetes
self-management and glycaemic control in adults with type 2 diabetes and
comorbid depression.
Testosterone replacement therapy may improve glucose tolerance and insulin sensitivity in diabetic hypogonadal men. The mechanisms by which testosterone decreases insulin resistance is under study.
Moreover, testosterone may have a protective effect on pancreatic beta
cells, which is possibly exerted by androgen-receptor-mediated
mechanisms and influence of inflammatory cytokines.
Recently it has been suggested that a type of gastric bypass surgery
may normalize blood glucose levels in 80–100% of severely obese
patients with diabetes. The precise causal mechanisms are being
intensively researched; its results may not simply be attributable to
weight loss, as the improvement in blood sugars seems to precede any
change in body mass. This approach may become a treatment for some
people with type 2 diabetes, but has not yet been studied in prospective
clinical trials. This surgery may have the additional benefit of reducing the death rate from all causes by up to 40% in severely obese people. A small number of normal to moderately obese patients with type 2 diabetes have successfully undergone similar operations.
MODY
is a rare genetic form of diabetes, often mistaken for Type 1 or Type
2. The medical management is variable and depends on each individual
case.