| Chronic fatigue syndrome | |
|---|---|
| Other names | Myalgic encephalomyelitis/ chronic fatigue syndrome (ME/CFS),
myalgic encephalomyelitis (ME), post-viral fatigue syndrome (PVFS),
chronic fatigue immune dysfunction syndrome (CFIDS), systemic exertion
intolerance disease (SEID), others |
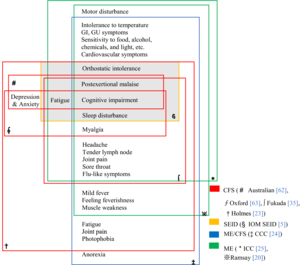 | |
| Chart of the symptoms of CFS according to various definitions | |
| Specialty | Rheumatology, rehabilitation medicine, endocrinology, Infectious disease, neurology, immunology, internal medicine, paediatrics, other specialists in ME/CFS |
| Symptoms | Worsening of symptoms with activity, long-term fatigue, others |
| Usual onset | 10 to 30 years old |
| Duration | Often for years |
| Causes | Unknown |
| Risk factors | Female sex, virus and bacterial infections, blood relatives with the illness, major injury, bodily response to severe stress and others |
| Diagnostic method | Based on symptoms |
| Treatment | Symptomatic |
| Prevalence | About 0.68 to 1% globally |
Chronic fatigue syndrome (CFS), also called myalgic encephalomyelitis (ME) or ME/CFS, is a complex, debilitating, long-term medical condition. Core symptoms are lengthy flare-ups of the illness following ordinary minor physical or mental activity, known as post-exertional malaise (PEM); greatly diminished capacity to do tasks that were routine before the illness; and sleep disturbances. The Center for Disease Control and Prevention's (CDC) diagnostic criteria also require at least one of the following: (1) orthostatic intolerance (difficulty sitting and standing upright) or (2) impaired memory or attention. Frequently and variably, other symptoms occur involving numerous body systems, and chronic pain is very common. The often incapacitating fatigue in ME/CFS is different from that caused by normal strenuous exertion, is not significantly relieved by rest, and is not due to a previous medical condition. Diagnosis is based on the person's symptoms because no confirmed diagnostic test is available.
The root cause(s) of the disease are unknown and the mechanisms are not fully understood. ME/CFS often starts after a flu-like infection, for instance after infectious mono. In some people, physical or mental stress may also act as a trigger. A genetic component is suspected, as ME/CFS can run in families. ME/CFS is associated with physical changes, including the nervous and immune system, and hormone production.
People with ME/CFS may recover or improve over time, but some will become severely affected and disabled for an extended period. No therapies or medications are approved to treat the cause of the illness; treatment is aimed at alleviation of symptoms. Pacing (personal activity management) can help to prevent flare-ups. Limited evidence suggests that counseling, personalized activity management, and the use of rintatolimod help improve some patients' functional abilities.
About 1% of primary-care patients have ME/CFS; estimates of incidence vary widely because various epidemiological studies have used different definitions. It has been estimated that 836,000 to 2.5 million Americans and 250,000 to 1,250,000 people in the United Kingdom have ME/CFS. ME/CFS occurs 1.5 to 2 times as often in women as in men. It most commonly affects adults between 40 and 60 years old, but can occur at other ages, including childhood. Other studies suggest that about 0.5% of children have ME/CFS, and that it is more common in adolescents than in younger children. Chronic fatigue syndrome is a major cause of school absence. ME/CFS significantly reduces health, happiness, productivity, and can also cause socio-emotional disruptions such as loneliness and alienation.
There is controversy over many aspects of the disorder. Various physicians, researchers, and patient advocates promote different names and diagnostic criteria. Results of studies of proposed causes and treatments are often poor or contradictory.
Signs and symptoms
The United States Centers for Disease Control and Prevention (CDC) recommends these criteria for diagnosis:
- Greatly lowered ability to do activities that were usual before the illness. This drop in activity level occurs along with fatigue and must last six months or longer.
- Worsening of symptoms after physical or mental activity that would not have caused a problem before the illness. The amount of activity that might aggravate the illness is difficult for a person to predict, and the decline often presents 12 to 48 hours after the activity. The 'relapse', or 'crash', may last days, weeks or longer. This is known as post-exertional malaise (PEM).
- Sleep problems; people may still feel weary after full nights of sleep, or may struggle to stay awake, fall asleep or stay asleep.
Additionally, one of the following symptoms must be present:
- Problems with thinking and memory (cognitive dysfunction, sometimes described as "brain fog")
- While standing or sitting upright; lightheadedness, dizziness, weakness, fainting or vision changes may occur (orthostatic intolerance)
Other common symptoms
Many, but not all people with ME/CFS report:
- Muscle pain, joint pain without swelling or redness, and headache
- Tender lymph nodes in the neck or armpits
- Sore throat
- Irritable bowel syndrome
- Chills and night sweats
- Allergies and sensitivities to foods, odors, chemicals, lights, or noise
- Shortness of breath
- Irregular heartbeat
Increased sensitivity to sensory stimuli and pain have also been observed in CFS.
Onset
The onset of ME/CFS may be gradual or sudden. When it begins suddenly, it often follows an episode of infectious-like symptoms or a known infection, and between 25% and 80% of patients report an infectious-like onset. When gradual, the illness may begin over the course of months or years with no apparent trigger. It's also frequent for the onset of ME/CFS to involve multiple triggering events that begin with minor symptoms and culminate in a final trigger leading to a noticeable onset. Studies disagree as to which pattern is more common. ME/CFS may also occur after physical trauma such as a car accident or surgery.
Physical functioning

CFS often causes significant disability, but the degree can vary greatly. Some people with mild CFS may lead relatively normal lives with vigilant energy management, while moderately affected patients may be unable to work or spend much time upright. People with severe CFS are generally housebound or bedbound, and may be unable to care for themselves.
The majority of people with CFS have significant difficulty engaging in work, school, and family activities for extended periods of time. An estimated 75% are unable to work because of their illness, and about 25% are housebound or bedridden for long periods, often decades. In one review on employment status, more than half of CFS patients were on disability benefits or temporary sick leave, and less than a fifth worked full-time. In children, CFS is a major cause of school absence. According to a 2009 study, patients exhibit a reduction in the complexity of their activities. Many people with CFS also experience strongly disabling chronic pain.
Symptoms can fluctuate over time, making the condition difficult to manage. Persons who feel better for a period may overextend their activities, triggering post-exertional malaise and a worsening of symptoms. Severity may also change over time, with periods of worsening, improvement or remission sometimes occurring.
People with CFS have decreased quality of life according to the SF-36 questionnaire, especially in the domains of vitality, physical functioning, general health, physical role, and social functioning. However, their scores in the "role emotional" and mental health domains were not substantially lower than healthy controls. A 2015 study found that people with CFS had lower health-related quality of life than 20 other chronic conditions, including multiple sclerosis, kidney failure, and lung cancer.
Cognitive functioning
Cognitive dysfunction is one of the most disabling aspects of CFS due to its negative impact on occupational and social functioning. 50–80% of people with CFS are estimated to have serious problems with cognition. Cognitive symptoms are mainly due to deficits in attention, memory, and reaction time. Measured cognitive abilities are found to be below projected normal values and likely to affect day-to-day activities, causing increases in common mistakes, forgetting scheduled tasks, or having difficulty responding when spoken to.
Simple and complex information-processing speed and functions entailing working memory over long time periods are moderately to extensively impaired. These deficits are generally consistent with the patient's perceptions. Perceptual abilities, motor speed, language, reasoning, and intelligence do not appear to be significantly altered. Patients who report poorer health status tend to also report more severe cognitive trouble, and better physical functioning is associated with less visuoperceptual difficulty and fewer language-processing complaints.
Inconsistencies of subjective and observed values of cognitive dysfunction reported across multiple studies are likely caused by a number of factors. Differences of research participants' cognitive abilities pre- and post-illness onset are naturally variable and are difficult to measure because of a lack of specialized analytical tools that can consistently quantify the specific cognitive difficulties in CFS.
Cause
The cause of ME/CFS is unknown. Both genetic and environmental factors are believed to contribute, but the genetic component is unlikely to be a single gene. Problems with the nervous and immune systems, and energy metabolism, may be factors. ME/CFS is a biological disease, not a psychiatric or psychological condition, and is not caused by deconditioning. However, the biological abnormalities found in research are not sensitive or specific enough for diagnosis.
Because the illness often follows a known or apparent viral illness, various infectious agents have been proposed, but a single cause has not been found. For instance, ME/CFS may start after mononucleosis, a H1N1 influenza infection, a varicella zoster virus infection (the virus that causes chickenpox), or SARS-CoV-1.
Risk factors
All ages, ethnic groups, and income levels are susceptible to the illness. The CDC states that while Caucasians may be diagnosed more frequently than other races in America, the illness is at least as prevalent among African Americans and Hispanics. A 2009 meta-analysis found that Asian Americans have a lower risk of CFS than White Americans, while Native Americans have a higher (probably a much higher) risk and African Americans probably have a higher risk. The review acknowledged that studies and data were limited.
More women than men get ME/CFS. A large 2020 meta-analysis estimated that between 1.5 and 2.0 times more cases are women. The review noted that different case definitions and diagnostic methods within datasets yielded a wide range of prevalence rates. The CDC estimates ME/CFS occurs up to four times more often in women than in men. The illness can occur at any age, but has the highest prevalence in people aged 40 to 60. ME/CFS is less prevalent among children and adolescents than among adults.
People with affected relatives appear to be more likely to get ME/CFS, implying the existence of genetic risk factors. People with a family history of neurological or autoimmune diseases are also at increased risk. Results of genetic studies have been largely contradictory or unreplicated. One study found an association with mildly deleterious mitochondrial DNA variants, and another found an association with certan variants of human leukocyte antigen genes.
Viral and other infections
Post-viral fatigue syndrome (PVFS) or post-viral syndrome describes a type of chronic fatigue syndrome that occurs following a viral infection. Viral infection is a significant risk factor for ME/CFS. Different types of viral infection can lead to ME/CFS, including airway infections, bronchitis, gastroenteritis, or an acute "flu-like illness". One review found higher Epstein–Barr virus (EBV) antibody activity in patients with ME/CFS, and that a subset were likely to have increased EBV activity compared to controls. Of people infected with EBV, around 8% to 15% develop ME/CFS, depending on criteria. Between 15% to 50% of people with long COVID also meet the diagnostic criteria for ME/CFS.
A systematic review found that fatigue severity was the main predictor of prognosis in CFS, and did not identify psychological factors linked to prognosis. Another review found that risk factors for developing post-viral fatigue or CFS after mononucleosis, dengue fever, or Q-fever included longer bed-rest during the illness, poorer pre-illness physical fitness, attributing symptoms to physical illness, belief that a long recovery time is needed, as well as pre-infection distress and fatigue. The same review found biological factors such as CD4 and CD8 activation and liver inflammation are predictors of sub-acute fatigue but not CFS.
A study analyzing the relationship between diagnostic labels and prognosis found that patients diagnosed with ME had the worst prognosis, and that patients with PVFS had the best. According to a review, it is unclear whether this was because people labeled with ME had a more severe or persistent illness, or because being labelled with ME adversely affects prognosis. The National Academy of Medicine report says it is a misconception that diagnosing ME/CFS worsens prognosis, and that accurate diagnosis is key to appropriate management.
Pathophysiology
ME/CFS is associated with changes in several areas, including the nervous, immune, and endocrine systems. Reported neurological differences include altered brain structure and metabolism, and autonomic nervous system dysfunction. Observed immunological changes include decreased natural killer cell activity, increased cytokines, and slightly increased levels of certain antibodies. Endocrine differences, such as modestly low cortisol and HPA axis dysregulation, have been noted as well. Impaired energy production and the possibility of autoimmunity are other areas of interest.
Neurological

A range of neurological structural and functional abnormalities is found in people with CFS, including lowered metabolism at the brain stem and reduced blood flow to cortical areas of the brain; these differences are consistent with neurological illness, but not depression or psychological illness. The World Health Organization classes chronic fatigue syndrome as a central nervous system disease.
Some neuroimaging studies have observed prefrontal and brainstem hypometabolism; however, sample size was limited. Neuroimaging studies in persons with CFS have identified changes in brain structure and correlations with various symptoms. Results were not consistent across the neuroimaging brain structure studies, and more research is needed to resolve the discrepancies found between the disparate studies.
Tentative evidence suggests a relationship between autonomic nervous system dysfunction and diseases such as CFS, fibromyalgia, irritable bowel syndrome, and interstitial cystitis. However, it is unknown if this relationship is causative. Reviews of CFS literature have found autonomic abnormalities such as decreased sleep efficiency, increased sleep latency, decreased slow wave sleep, and abnormal heart rate response to tilt table tests, suggesting a role of the autonomic nervous system in CFS. However, these results were limited by inconsistency.
Central sensitization, or increased sensitivity to sensory stimuli such as pain have been observed in CFS. Sensitivity to pain increases after exertion, which is opposite to the normal pattern.
Immunological
Immunological abnormalities are frequently observed in those with CFS. Decreased NK cell activity is found more often in people with CFS and this correlates with severity of symptoms. People with CFS have an abnormal response to exercise, including increased production of complement products, increased oxidative stress combined with decreased antioxidant response, and increased Interleukin 10, and TLR4, some of which correlates with symptom severity. Increased levels of cytokines have been proposed to account for the decreased ATP production and increased lactate during exercise;however, the elevations of cytokine levels are inconsistent in specific cytokine, albeit frequently found. Similarities have been drawn between cancer and CFS with regard to abnormal intracellular immunological signaling. Abnormalities observed include hyperactivity of ribonuclease L, a protein activated by IFN, and hyperactivity of NF-κB.
Endocrine
Evidence points to abnormalities in the hypothalamic-pituitary-adrenal axis (HPA axis) in some people with ME/CFS, which may include lower cortisol levels, a decrease in the variation of cortisol levels throughout the day and decreased responsiveness of the HPA axis. This can be considered to be a "HPA axis phenotype" that is also present in some other conditions, including post-traumatic stress disorder and some autoimmune conditions. It is unclear whether or not decreased cortisol levels of the HPA axis plays a primary role as a cause of CFS, or has a secondary role in the continuation or worsening of symptoms later in the illness. In most healthy adults, the cortisol awakening response shows an increase in cortisol levels averaging 50% in the first half-hour after waking. In people with CFS, this increase apparently is significantly less, but methods of measuring cortisol levels vary, so this is not certain.
Autoimmunity
Autoimmunity has been proposed to be a factor in ME/CFS, but there are only a few relevant findings so far. There is a subset of patients with increased B cell activity and autoantibodies, possibly as a result of decreased NK cell regulation or viral mimicry. In 2015, a large German study found 29% of ME/CFS patients had elevated autoantibodies to M3 and M4 muscarinic acetylcholine receptors as well as to ß2 adrenergic receptors. Problems with these receptors can lead to impaired blood flow.
Energy metabolism
Objective signs of PEM have been found with the 2-day CPET, a test that involves taking VO2max tests on successive days. People with ME/CFS have lower performance and heart rate compared to healthy controls on the first test. On the second test, healthy people's scores stay the same or increase slightly, while people with ME/CFS have a decrease in anaerobic threshold, peak power output, and VO2max. Potential causes include impaired oxygen transport, impaired aerobic metabolism, and mitochondrial dysfunction.
Studies have observed mitochondrial abnormalities in cellular energy production, but recent focus has concentrated on secondary effects that may result in aberrant mitochondrial function because inherent problems with the mitochondria structure or genetics have not been replicated.
Diagnosis

No characteristic laboratory abnormalities are approved to diagnose ME/CFS; while physical abnormalities can be found, no single finding is considered sufficient for diagnosis. Blood, urine, and other tests are used to rule out other conditions that could be responsible for the symptoms. The CDC states that a medical history should be taken and a mental and physical examination should be done to aid diagnosis.
Diagnostic tools
The CDC recommends considering the questionnaires and tools described in the 2015 Institute of Medicine report, which include:
- The Chalder Fatigue Scale
- Multidimensional Fatigue Inventory
- Fisk Fatigue Impact Scale
- The Krupp Fatigue Severity Scale
- DePaul Symptom Questionnaire
- CDC Symptom Inventory for CFS
- Work and Social Adjustment Scale (WSAS)
- SF-36 / RAND-36
A two-day cardiopulmonary exercise test (CPET) is not necessary for diagnosis, although lower readings on the second day may be helpful in supporting a claim for Social Security disability. A two-day CPET cannot be used to rule out chronic fatigue syndrome.
Definitions
Many sets of diagnostic criteria for ME/CFS have been proposed. Required symptoms vary. The four most commly cited are post-exertional malaise, fatigue, cognitive impairment, and sleep disruption. Notable definitions include:
- Centers for Disease Control and Prevention (CDC) definition (1994), is also called the Fukuda definition and is a revision of the Holmes or CDC 1988 scoring system. The 1994 criteria require the presence of four or more symptoms beyond fatigue, while the 1988 criteria require six to eight.
- The 2003 Canadian consensus criteria state: "A patient with ME/CFS will meet the criteria for fatigue, post-exertional malaise and/or fatigue, sleep dysfunction, and pain; have two or more neurological/cognitive manifestations and one or more symptoms from two of the categories of autonomic, neuroendocrine, and immune manifestations; and the illness persists for at least 6 months".
- The Myalgic Encephalomyelitis International Consensus Criteria (ICC) published in 2011 is based on the Canadian working definition and has an accompanying primer for clinicians. The ICC does not have a six months waiting time for diagnosis. The ICC requires post-exertional neuroimmune exhaustion (PENE) which has similarities with post-exertional malaise, plus at least three neurological symptoms, at least one immune or gastrointestinal or genitourinary symptom, and at least one energy metabolism or ion transportation symptom. Unrefreshing sleep or sleep dysfunction, headaches or other pain, and problems with thinking or memory, and sensory or movement symptoms are all required under the neurological symptoms criterion. According to the ICC, patients with post-exertional neuroimmune exhaustion but only partially meeting the criteria should be given the diagnosis of atypical myalgic encephalomyelitis.
- The 2015 definition by the National Academy of Medicine (then referred to as the "Institute of Medicine") is not a definition of exclusion (differential diagnosis is still required). "Diagnosis requires that the patient have the following three symptoms: 1) A substantial reduction or impairment in the ability to engage in pre-illness levels of occupational, educational, social, or personal activities, that persists for more than 6 months and is accompanied by fatigue, which is often profound, is of new or definite onset (not lifelong), is not the result of ongoing excessive exertion, and is not substantially alleviated by rest, and 2) post-exertional malaise* 3) Unrefreshing sleep*; At least one of the two following manifestations is also required: 1) Cognitive impairment* 2) Orthostatic intolerance" and notes that "*Frequency and severity of symptoms should be assessed. The diagnosis of ME/CFS should be questioned if patients do not have these symptoms at least half the time with moderate, substantial, or severe intensity."
The 2021 UK NICE guidelines employ a definition of ME/CFS that requires severe fatigue, post-exertional malaise, unrefreshing sleep or sleep disturbance, and cognitive difficulties.
Differential diagnosis
Certain medical conditions have similar symptoms as ME/CFS and should be evaluated before a diagnosis of ME/CFS can be confirmed. While alternative diagnoses are explored, advice can be given on symptom management, to avoid delays in care. Post-exertional malaise often acts as a distinguishing feature of ME/CFS. A diagnosis of ME/CFS is only confirmed after 6 months of symptoms, to exclude acute medical conditions or problems related to lifestyle, which may resolve within that time frame.
Examples of possible differential diagnoses span a large set of specialties, and depend on patient history. Examples are infectious diseases (such as Epstein–Barr virus, HIV infection, tuberculosis, Lyme disease), neuroendocrine disorder (such as diabetes, hypothyroidism, Addison's disease, adrenal insufficiency), blood disorders (such as anemia) and some cancers. Various rheumatological and auto-immune diseases may also have overlapping symptoms with ME/CFS, such as Sjögren's syndrome, lupus and arthritis. Furthermore, evaluation of psychiatric diseases (such as depression, substance use disorder and anorexia nervosa) and neurological disorders (such as obstructive sleep apnea, narcolepsy, Parkinson's, multiple sclerosis, craniocervical instability) may be warranted. Finally, sleep disorders, coeliac disease, connective tissue disorders and side effects of medications may also explain symptoms.
Joint and muscle pain without swelling or inflammation is a feature of ME/CFS, but is more associated with fibromyalgia. Modern definitions of fibromyalgia not only include widespread pain, but also fatigue, sleep disturbances and cognitive issues, making the two syndromes difficult to distinguish. The two are often co-diagnosed. Ehlers–Danlos syndromes (EDS) may also have similar symptoms.
Like with other chronic illnesses, depression and anxiety co-occur frequently with ME/CFS. Depression may be differentially diagnosed from ME/CFS by feelings of worthlessness, the inability to feel pleasure, loss of interest and/or guilt; and the absence of bodily symptoms such autonomic dysfunction, pain, migraines or post-exertional malaise.
Symptom Management
There is no approved drug treatment, therapy or cure for ME/CFS, although some symptoms can be treated or managed. Pacing, or managing one's activities to stay within their energy limits, can reduce episodes of post-exertional malaise. Addressing sleep problems with good sleep hygiene, or medication if required, may be beneficial. Chronic pain is common in ME/CFS, and the CDC recommends consulting with a pain management specialist if over-the-counter painkillers are insufficient. The debilitating nature of ME/CFS can cause depression or other psychological problems, which should be treated accordingly. For cognitive impairment, adaptations like organizers and calendars may be helpful. Comorbid conditions are common and should be treated if present.
The CDC recommends a strategy treating the most disabling symptom first, and the NICE guideline specifies the need for shared decision-making between patients and medical teams. NICE recognized that symptoms of severe ME/CFS may be misunderstood as neglect or abuse and recommends assessment for safeguarding of persons suspected of having ME/CFS be evaluated by professionals with experience and understanding of the illness. Clinical management varies widely, with many patients receiving combinations of therapies.
Comorbid conditions that may interact with and worsen ME/CFS symptoms care are common, and treating these may be beneficial. The most commonly diagnosed include fibromyalgia, irritable bowel syndrome, depression, anxiety, allergies, and chemical sensitivities.
Pacing
Pacing, or activity management, is an illness management strategy based on the observation that symptoms tend to increase following mental or physical exertion. It was developed for ME/CFS in the 1980s, and is now commonly used as a management strategy in chronic illnesses and in chronic pain.
Its two forms are symptom-contingent pacing, in which the decision to stop (and rest or change an activity) is determined by self-awareness of an exacerbation of symptoms, and time-contingent pacing, which is determined by a set schedule of activities that a patient estimates he or she is able to complete without triggering post-exertional malaise (PEM). Thus, the principle behind pacing for CFS is to avoid overexertion and an exacerbation of symptoms. It is not aimed at treating the illness as a whole. Those whose illness appears stable may gradually increase activity and exercise levels, but according to the principle of pacing, must rest or reduce their activity levels if it becomes clear that they have exceeded their limits. Use of a heart-rate monitor with pacing to monitor and manage activity levels is recommended by a number of patient groups, and the CDC considers it useful for some individuals to help avoid post-exertional malaise.
Energy envelope theory
Energy envelope theory, considered to be consistent with pacing, is a management strategy suggested in the 2011 international consensus criteria for ME, which refers to using an "energy bank budget". Energy envelope theory was devised by psychologist Leonard Jason, who previously had CFS. Energy envelope theory states that patients should stay within, and avoid pushing through, the envelope of energy available to them, so as to reduce the post-exertional malaise "payback" caused by overexertion. This may help them make "modest gains" in physical functioning. Several studies have found energy envelope theory to be a helpful management strategy, noting that it reduces symptoms and may increase the level of functioning in CFS. Energy envelope theory does not recommend unilaterally increasing or decreasing activity and is not intended as a therapy or cure for CFS. It has been promoted by various patient groups. Some patient groups recommend using a heart rate monitor to increase awareness of exertion and enable patients to stay within their aerobic threshold envelope.
Exercise
Stretching, movement therapies, and toning exercises are recommended for pain in patients with ME/CFS. In many chronic illnesses, aerobic exercise is beneficial, but in chronic fatigue syndrome, the CDC does not recommend it. The CDC states:
Any activity or exercise plan for people with ME/CFS needs to be carefully designed with input from each patient. While vigorous aerobic exercise can be beneficial for many chronic illnesses, patients with ME/CFS do not tolerate such exercise routines. Standard exercise recommendations for healthy people can be harmful for patients with ME/CFS. However, it is important that patients with ME/CFS undertake activities that they can tolerate...
Short periods of low-intensity exercise to improve stamina may be possible in a subset of people with ME/CFS. Exercise should only be attempted after pacing has been implemented effectively. The amount of exercise should be varied based on the symptom severity of each day, to avoid PEM.
Graded exercise therapy (GET) involving fixed increments in exercise over time, is not recommended for people with ME/CFS. Newer reviews of GET dispute it's effectiveness and safety. Few clinical trials contained enough detail about adverse effects.
Counseling
Chronic illness often impacts mental health. Psychotherapy may help patients manage the stress of being ill, apply self-management strategies for their symptoms, and cope with physical pain. Cognitive behavioral therapy (CBT) may be offered to people with a new ME/CFS diagnosis to give them tools to cope with the disease and help with rehabilitation. Family sessions may be useful to teach about the severe disability from ME/CFS. Depression or anxiety resulting from ME/CFS is common, and CBT may be a useful treatment.
Diet and nutrition
A proper diet is a significant contributor to the health of any individual. Medical consultation about diet and supplements is recommended for persons with ME/CFS. Persons with ME/CFS may also benefit from nutritional support if deficiencies are detected by medical testing. However, nutritional supplements may interact with prescribed medication.
Bowel issues are a common symptom of ME/CFS. For some, eliminating certain food groups, such as caffeine, alcohol or dairy, can alleviate symptoms. People with severe ME/CFS may have significant trouble getting nutrition. Intravenous feeding (via blood) or tube feeding may be necessary to address this, or to address electrolyte imbalances.
Proposed treatments for curative intent
There are no approved treatments for ME/CFS. Cognitive behavior therapy (CBT) and graded exercise therapy (GET) have been proposed, but their safety and efficacy are disputed. The drug rintatolimod has been trialed and has been approved in Argentina.
Graded exercise therapy
Graded exercise therapy (GET) is a programme of physical therapy that starts at a patient's baseline and gradually increases over time. Like CBT, it assumes that patients' fears of activity and deconditioning play a significant role, and its safety and efficacy are debated.
The 2021 NICE guidelines removed GET as a recommended treatment due to low quality evidence regarding benefit, with the guidelines now telling clinicians not to prescribe "any programme that ... uses fixed incremental increases in physical activity or exercise, for example, graded exercise therapy." The CDC withdrew their recommendation for GET in 2017.
Cognitive behavioral therapy
Cognitive behavioral therapy for ME/CFS is a variant of CBT that assumes a cognitive-behavioral model of ME/CFS. In this model, people with ME/CFS mistakenly attribute their illness solely to physical causes, and their condition is perpetuated by a fear of triggering symptoms, which leads to a vicious cycle of deconditioning and avoidance of activity. CBT aims to help patients view unhelpful thoughts and behaviors as factors in their illness. This model has been criticized as lacking evidence and being at odds with the biological changes associated with ME/CFS, and the use of this type of CBT has been the subject of much controversy.
NICE removed their recommendation for this form of CBT in 2021, replacing it with a recommendation to offer patient CBT for help coping with distress that illness causes. The guidelines emphasize that CBT for people with ME/CFS should not assume that unhelpful beliefs cause their illness, and should not be portrayed as curative. Similarly, the CDC stopped recommending CBT as a treatment in 2017, recommending counseling as a coping method instead.
Rintatolimod
Rintatolimod is a double-stranded RNA drug developed to modulate an antiviral immune reaction through activation of toll-like receptor 3. In several clinical trials of CFS, the treatment has shown a reduction in symptoms, but improvements were not sustained after discontinuation. Evidence supporting the use of rintatolimod is deemed low to moderate. The US FDA has denied commercial approval, called a new drug application, citing several deficiencies and gaps in safety data in the trials, and concluded that the available evidence is insufficient to demonstrate its safety or efficacy in CFS. Rintatolimod has been approved for marketing and treatment for persons with ME/CFS in Argentina, and in 2019, FDA regulatory requirements were met for exportation of rintatolimod to the country.
Prognosis
Information on the prognosis of ME/CFS is limited, and the course of the illness is variable. According to the NICE guideline, ME/CFS "varies in long-term outlook from person to person." Complete recovery, partial improvement, and worsening are all possible. Symptoms generally fluctuate over days, weeks, or longer periods, and some people may experience periods of remission. Overall, "many will need to adapt to living with ME/CFS." Some people who improve need to manage their activities in order to prevent relapse. Children and teenagers are more likely to recover or improve than adults.
A 2005 systematic review found that for untreated CFS, "the median full recovery rate was 5% (range 0–31%) and the median proportion of patients who improved during follow-up was 39.5% (range 8–63%)," and that 8 to 30% of patients were able to return to work. Age at onset, a longer duration of follow-up, less fatigue severity at baseline, and other factors were occasionally, but non consistently, related to outcome. Another review found that children have a better prognosis than adults, with 54–94% having recovered by follow-up, compared to less than 10% of adults returning to pre-illness levels of functioning.
Epidemiology

Reported prevalence rates vary widely depending on how CFS/ME is defined and diagnosed. Based on the 1994 CDC diagnostic criteria, the global prevalence rate for CFS is 0.89%. In comparison, estimates using the 1988 CDC "Holmes" criteria and 2003 Canadian criteria for ME produced an incidence rate of only 0.17%. Between 836,000 and 2.5 million Americans have ME/CFS, but 84–91% of these are undiagnosed, and over 250,000 people in England and Wales are estimated to be affected. The worldwide prevalence is 17 and 24 million.
Females are diagnosed about 1.5 to 2.0 times more often with CFS/ME than males. An estimated 0.5% of children have ME/CFS, and more adolescents are affected with the illness than younger children.
The incidence rate according to age has two peaks, one at 10–19 and another at 30–39 years, and the rate of prevalence is highest between ages 40 and 60.
History
Myalgic encephalomyelitis
- From 1934 onwards, outbreaks of a previously unknown illness began to be recorded by doctors. Initially considered to be occurrences of poliomyelitis, the illness was subsequently referred to as "epidemic neuromyasthenia".
- In the 1950s, the term "benign myalgic encephalomyelitis" was used in relation to a comparable outbreak at the Royal Free Hospital in London. The descriptions of each outbreak were varied, but included symptoms of malaise, tender lymph nodes, sore throat, pain, and signs of encephalomyelitis. The cause of the condition was not identified, although it appeared to be infectious, and the term "benign myalgic encephalomyelitis" was chosen to reflect the lack of mortality, the severe muscular pains, symptoms suggesting damage to the nervous system, and to the presumed inflammatory nature of the disorder. Björn Sigurðsson disapproved of the name, stating that the illness is rarely benign, does not always cause muscle pain, and is possibly never encephalomyelitic. The syndrome appeared in sporadic as well as epidemic cases.
- In 1969, benign myalgic encephalomyelitis appeared as an entry to the International Classification of Diseases under Diseases of the nervous system.
- In 1986, Ramsay published the first diagnostic criteria for ME, in which the condition was characterized by: 1) muscle fatiguability in which, even after minimal physical effort, three or more days elapse before full muscle power is restored; 2) extraordinary variability or fluctuation of symptoms, even in the course of one day; and 3) chronicity.
- By 1988, the continued work of Ramsay had demonstrated that, although the disease rarely resulted in mortality, it was often severely disabling. Because of this, Ramsay proposed that the prefix "benign" be dropped.
Chronic fatigue syndrome
- In the mid-1980s, two large outbreaks of an illness that resembled mononucleosis drew national attention in the United States. Located in Nevada and New York, the outbreaks involved an illness characterized by "chronic or recurrent debilitating fatigue, and various combinations of other symptoms, including a sore throat, lymph node pain and tenderness, headache, myalgia, and arthralgias". An initial link to the Epstein–Barr virus had the illness acquire the name "chronic Epstein–Barr virus syndrome".
- In 1987, the CDC convened a working group to reach a consensus on the clinical features of the illness. The working group concluded that CFS was not new, and that the many different names given to it previously reflected widely differing concepts of the illness's cause and epidemiology. The CDC working group chose "chronic fatigue syndrome" as a more neutral and inclusive name for the illness, but noted that "myalgic encephalomyelitis" was widely accepted in other parts of the world.
- In 1988, the first definition of CFS was published. Although the cause of the illness remained unknown, several attempts were made to update this definition, most notably in 1994.
- The most widely referenced diagnostic criteria and definition of CFS for research and clinical purposes were published in 1994 by the CDC.
- In 2006, the CDC commenced a national program to educate the American public and health-care professionals about CFS.
Other medical terms
A range of both theorised and confirmed medical entities and naming conventions have appeared historically in the medical literature dealing with ME and CFS. These include:
- Epidemic neuromyasthenia was a term used for outbreaks with symptoms resembling poliomyelitis.
- Iceland disease and Akureyri disease were synonymous terms used for an outbreak of fatigue symptoms in Iceland.
- Low natural killer syndrome, a term used mainly in Japan, reflected research showing diminished in vitro activity of natural killer cells isolated from patients.
- Neurasthenia had been proposed as a historical diagnosis that occupied a similar medical and cultural space to CFS.
- Royal Free disease was named after the historically significant outbreak in 1955 at the Royal Free Hospital used as an informal synonym for "benign myalgic encephalomyelitis".
- Tapanui flu was a term commonly used in New Zealand, deriving from the name of a town, Tapanui, where numerous people had the syndrome.
Society and culture

Naming
Many names have been proposed for the illness. Currently, the most commonly used are "chronic fatigue syndrome", "myalgic encephalomyelitis", and the umbrella term "myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)". Reaching consensus on a name is challenging because the cause and pathology remain unknown.
Many patients object to the term "chronic fatigue syndrome". They consider the term too simplistic and trivialising, which in turn prevents the illness from being taken seriously. At the same time, there are also issues with the use of "myalgic encephalomyelitis, as there is only limited evidence of brain inflammation implied by the name. The umbrella term ME/CFS would retain the better-known phrase CFS without trivialising the disease, but some people object to this name too as they see CFS and ME as distinct illnesses.
A 2015 report from the Institute of Medicine recommended the illness be renamed "systemic exertion intolerance disease", (SEID), and suggested new diagnostic criteria, proposing post-exertional malaise (PEM), impaired function, and sleep problems are core symptoms of ME/CFS. While the new name was not widely adopted, the diagnostic criteria were taken over by the CDC. Like CFS, SEID only focuses on a single symptom and patient opinions have generally been negative.
Economic impact
Economic costs due to CFS are "significant". A 2021 paper by Leonard Jason and Arthur Mirin estimated the impact in the US to be $36-51 billion per year, or $31,592 to $41,630 per person, considering both lost wages and healthcare costs. The CDC estimated direct healthcare costs alone at $9–14 billion annually. A 2017 estimate for the annual economic burden in the United Kingdom was £3.3 billion.
Awareness day
12 May is designated as ME/CFS International Awareness Day. The day is observed so that stakeholders have an occasion to improve the knowledge of "the public, policymakers, and health-care professionals about the symptoms, diagnosis, and treatment of ME/CFS, as well as the need for a better understanding of this complex illness." It was chosen because it is the birthday of Florence Nightingale, who had an illness appearing similar to ME/CFS or fibromyalgia.
Doctor–patient relations
People with CFS face stigma in healthcare settings, and doctors may have trouble managing an illness that lacks a clear cause or treatment. There has been much disagreement over proposed causes, diagnosis, and treatment of the illness. Some doctors believe it is psychological. Most patients are convinced their illness is physical instead, straining doctor-patient relationships. Clinicians may be unfamiliar with CFS, as it is often not covered in medical school. Due to this unfamiliarity, patients may go undiagnosed for years, or be misdiagnosed with mental conditions. A substantial portion of doctors are uncertain about how to diagnose or manage CFS. In a 2006 survey of GPs in southwest England, 75% accepted it as a "recognisable clinical entity", but 48% did not feel confident in diagnosing it, and 41% in managing it.
The NAM report refers to CFS as "stigmatized", and the majority of patients report negative healthcare experiences. These patients may feel that their doctor inappropriately calls their illness psychological or doubts the severity of their symptoms. They may also feel forced to prove that they are legitimately ill. Some may be given outdated treatments that provoke symptoms or assume their illness is due to unhelpful thoughts and deconditioning. In a 2009 survey, only 35% of patients considered their physicians experienced with CFS and only 23% thought their doctors knew enough to treat it.
Blood donation
In 2010, several national blood banks adopted measures to discourage or prohibit individuals diagnosed with CFS from donating blood, based on concern following the 2009 claim of a link between CFS and a retrovirus which was subsequently shown to be unfounded. Organizations adopting these or similar measures included the Canadian Blood Services, the New Zealand Blood Service, the Australian Red Cross Blood Service and the American Association of Blood Banks. In November 2010, the UK National Blood Service permanently deferred ME/CFS patients from donating blood to prevent potential harm to the donor. Donation policy in the UK now states, "The condition is relapsing by nature and donation may make symptoms worse, or provoke a relapse in an affected individual."
Controversy
Much contention has arisen over the cause, pathophysiology, nomenclature, and diagnostic criteria of CFS. Historically, many professionals within the medical community were unfamiliar with CFS, or did not recognize it as a real condition; nor did agreement exist on its prevalence or seriousness. Some people with CFS reject any psychological component.
In 1970, two British psychiatrists, McEvedy and Beard, reviewed the case notes of 15 outbreaks of benign myalgic encephalomyelitis and concluded that it was caused by mass hysteria on the part of patients, or altered medical perception of the attending physicians. Their conclusions were based on previous studies that found many normal physical test results, a lack of a discernible cause, and a higher prevalence of the illness in females. Consequently, the authors recommended that the disease should be renamed "myalgia nervosa". This perspective was rejected in a series of case studies by Melvin Ramsay and other staff of the Royal Free Hospital, the center of a significant outbreak. The psychological hypothesis posed by McEvedy and Beard created great controversy, and convinced a generation of health professionals in the UK that this could be a plausible explanation for the condition, resulting in neglect by many medical specialties. The specialty that did take a major interest in the illness was psychiatry.
Because of the controversy, sociologists hypothesized that stresses of modern living might be a cause of the illness, while some in the media used the term "Yuppie flu" and called it a disease of the middle class. People with disabilities from CFS were often not believed and were accused of being malingerers. The November 1990 issue of Newsweek ran a cover story on CFS, which although supportive of an organic cause of the illness, also featured the term 'yuppie flu', reflecting the stereotype that CFS mainly affected yuppies. The implication was that CFS is a form of burnout. The term 'yuppie flu' is considered offensive by both patients and clinicians.
In 2009, the journal Science published a study that identified the XMRV retrovirus in a population of people with CFS. Other studies failed to reproduce this finding, and in 2011, the editor of Science formally retracted its XMRV paper while the Proceedings of the National Academy of Sciences similarly retracted a 2010 paper which had appeared to support the finding of a connection between XMRV and CFS.
Research funding
United Kingdom
The lack of research funding and the funding bias towards biopsychosocial studies and against biomedical studies has been highlighted a number of times by patient groups and a number of UK politicians. A parliamentary inquiry by an ad hoc group of parliamentarians in the United Kingdom, set up and chaired by former MP, Dr Ian Gibson, called the Group on Scientific Research into CFS/ME, was addressed by a government minister claiming that few good biomedical research proposals have been submitted to the Medical Research Council (MRC) in contrast to those for psychosocial research. They were also told by other scientists of proposals that have been rejected, with claims of bias against biomedical research. The MRC confirmed to the group that from April 2003 to November 2006, it has turned down 10 biomedical applications relating to CFS/ME and funded five applications relating to CFS/ME, mostly in the psychiatric/psychosocial domain.
In 2008, the MRC set up an expert group to consider how the MRC might encourage new high-quality research into CFS/ME and partnerships between researchers already working on CFS/ME and those in associated areas. It currently lists CFS/ME with a highlight notice, inviting researchers to develop high-quality research proposals for funding. In February 2010, the All-Party Parliamentary Group on ME (APPG on ME) produced a legacy paper, which welcomed the recent MRC initiative, but felt that far too much emphasis in the past had been on psychological research, with insufficient attention to biomedical research, and that further biomedical research must be undertaken to help discover a cause and more effective forms of management for this disease.
A 2016 report by ME Research looking at UK funding for ME/CFS between January 2006 and December 2015 found that 99 grants had been funded, totalling £49 million, with the largest number of studies being related to "Biological and endogenous factors".
Controversy surrounds psychologically oriented models of the disease and behavioral treatments conducted in the UK.
United States
In 1998, $13 million for CFS research was found to have been redirected or improperly accounted for by the United States CDC, and officials at the agency misled Congress about the irregularities. The agency stated that they needed the funds to respond to other public-health emergencies. The director of a US national patient advocacy group charged the CDC had a bias against studying the disease. The CDC pledged to improve their practices and to restore the $13 million to CFS research over three years.
On 29 October 2015, the National Institutes of Health declared its intent to increase research on ME/CFS. The NIH Clinical Center was to study individuals with ME/CFS, and the National Institute of Neurological Disorders and Stroke would lead the Trans-NIH ME/CFS Research Working Group as part of a multi-institute research effort.
Notable cases
In 1989, The Golden Girls (1985–1992) featured chronic fatigue syndrome in a two-episode arc, "Sick and Tired: Part 1" and "Part 2", in which protagonist Dorothy Zbornak, portrayed by Bea Arthur, after a lengthy battle with her doctors in an effort to find a diagnosis for her symptoms, is finally diagnosed with CFS. American author Ann Bannon had CFS. Laura Hillenbrand, author of the popular book Seabiscuit, has struggled with CFS since age 19.
Research

Current research into ME/CFS may lead to a better understanding of the disease's causes, biomarkers to aid in diagnosis, and treatments to relieve symptoms. The emergence of long COVID has sparked increased interest in ME/CFS, as the two conditions may share pathology, and a treatment for one may treat the other.
Causes
Recent research suggests dysfunction in many biological processes. These changes may share a common cause, but the true relationship between them is currently unknown. Metabolic areas of interest include disruptions in amino acid metabolism, the TCA cycle, ATP synthesis, and potentially increased lipid metabolism. Other research has investigated immune dysregulation and its potential connections to mitochondrial dysfunction. Autoimmunity has been proposed as a cause, but evidence is scant. People with ME/CFS may have abnormal gut microbiota, which has been proposed to affect mitochondria or nervous system function.
Several small studies have investigated the genetics of ME/CFS, but none of their findings have been replicated. A larger study, DecodeME, is currently underway in the United Kingdom.
Treatments
Various drug treatments for ME/CFS are being explored. The types of drugs under investigation often target the nervous system, the immune system or autoimmunity, or pain directly. More recently, there has been a growing interest in drugs targeting energy metabolism.
Drugs targetting the immune system include rintatolimod. Low-dose naltrexone, which works against neuro-inflammation, is being studied as of 2023. Rituximab, a drug that depletes B cells, was studied and found to be ineffective. Other options targetting auto-immunity are immune absorption, whereby a large set of (auto)antibodies is removed from the blood.
Biomarkers
Many biomarkers for ME/CFS have been proposed based on research findings. But due to the use of a number of case definitions in research, some of which are non-specific such as the Sharpe ("Oxford") and Fukuda ("old CDC") definitions, no biomarkers have been widely validated or broadly clinically implemented. Proposed markers include electrical measurements of blood cells and a combination of immune cell death rate and function.
Challenges
ME/CFS affects multiple bodily systems, varies widely in severity, and fluctuates over time, creating heterogeneity within patient groups and making it very difficult to identify a singular cause. This variation may also cause treatments that are effective for some patients to have no effect or a negative effect in others. Dividing patients into subtypes may help manage this heterogeneity.
The existence of multiple diagnostic criteria, and variations in how scientists apply them, complicate comparisons between studies. Some definitions, like the Oxford and Fukuda criteria, may fail to distinguish between chronic fatigue in general and ME/CFS, which requires PEM in modern definitions. Definitions also vary in which co-occurring conditions preclude a diagnosis of ME/CFS.
