Arachidonic acid (AA) is a 20-carbon ω-6 conditionally essential fatty acid. It sits at the head of the "arachidonic acid cascade" – more than 20 different signalling paths that control a wide array of bodily functions, but especially those functions involving inflammation, cell growth and the central nervous system. Most AA in the human body derives from dietary linoleic acid (another essential fatty acid, 18:2 ω-6), which is derived from nuts, seeds, vegetable oils and animal fats.
In the inflammatory response, two other groups of dietary essential fatty acids form cascades that parallel and compete with the arachidonic acid cascade. EPA (20:5 ω-3) provides the most important competing cascade. It is ingested from oily fish, and algae oil or derived from dietary alpha-linolenic acid found in, for instance, walnuts, hemp oil and flax oil. DGLA (20:3 ω-6) provides a third, less prominent cascade. It derives from dietary GLA (18:3 ω-6) found in, e.g. borage oil. These two parallel cascades soften the inflammatory promoting effects of certain eicosanoids made from AA. Low dietary intake of these less inflammatory promoting essential fatty acids, especially the ω-3s, is correlated with a variety of inflammation-related diseases.
Today, the usual diet in industrial countries contains much less ω-3 fatty acids than the diet of a century ago and a much greater amount of air pollution on a daily basis that evokes the inflammatory response. The diet from a century ago had much less ω-3 than the diet of early hunter-gatherers but also much less pollution than today. We can also look at the ratio of ω-3 to ω-6 in comparisons of their diets. These changes have been accompanied by increased rates of many diseases – the so-called diseases of civilization – that involve inflammatory processes. There is now very strong evidence that several of these diseases are ameliorated by increasing dietary ω-3, and good evidence for many others. There is also more preliminary evidence showing that dietary ω-3 can ease symptoms in several psychiatric disorders. Nonetheless, fish oil supplement studies have failed to support claims of preventing heart attacks or strokes.
Research regarding krill oil, another animal-based omega-3 source, is ongoing. Preliminary studies appear to indicate that the DHA and EPA omega-3 fatty acids found in krill oil may be more bio-available than in fish oil. Additionally, krill oil contains astaxanthin, a marine-source keto-carotenoid antioxidant that may act synergistically with EPA and DHA.
In the inflammatory response, two other groups of dietary essential fatty acids form cascades that parallel and compete with the arachidonic acid cascade. EPA (20:5 ω-3) provides the most important competing cascade. It is ingested from oily fish, and algae oil or derived from dietary alpha-linolenic acid found in, for instance, walnuts, hemp oil and flax oil. DGLA (20:3 ω-6) provides a third, less prominent cascade. It derives from dietary GLA (18:3 ω-6) found in, e.g. borage oil. These two parallel cascades soften the inflammatory promoting effects of certain eicosanoids made from AA. Low dietary intake of these less inflammatory promoting essential fatty acids, especially the ω-3s, is correlated with a variety of inflammation-related diseases.
Today, the usual diet in industrial countries contains much less ω-3 fatty acids than the diet of a century ago and a much greater amount of air pollution on a daily basis that evokes the inflammatory response. The diet from a century ago had much less ω-3 than the diet of early hunter-gatherers but also much less pollution than today. We can also look at the ratio of ω-3 to ω-6 in comparisons of their diets. These changes have been accompanied by increased rates of many diseases – the so-called diseases of civilization – that involve inflammatory processes. There is now very strong evidence that several of these diseases are ameliorated by increasing dietary ω-3, and good evidence for many others. There is also more preliminary evidence showing that dietary ω-3 can ease symptoms in several psychiatric disorders. Nonetheless, fish oil supplement studies have failed to support claims of preventing heart attacks or strokes.
Research regarding krill oil, another animal-based omega-3 source, is ongoing. Preliminary studies appear to indicate that the DHA and EPA omega-3 fatty acids found in krill oil may be more bio-available than in fish oil. Additionally, krill oil contains astaxanthin, a marine-source keto-carotenoid antioxidant that may act synergistically with EPA and DHA.
Eicosanoid series nomenclature
Eicosanoids are signalling molecules derived from the essential fatty
acids (EFA); they are a major pathway by which the EFAs act in the
body. There are four classes of eicosanoid and two or three series
within each class. Before discussing eicosanoid action, we will explain
the series nomenclature.
The plasma membranes of cells contain phospholipids, which are composed of a hydrophilic phosphate head and two hydrophobic fatty acid tails. Some of these fatty acids are 20-carbon polyunsaturated
essential fatty acids – AA, EPA or DGLA. In response to a variety of
inflammatory signals, these EFAs are cleaved out of the phospholipid and
released as free fatty acids. Next, the EFA is oxygenated (by either
of two pathways), then further modified, yielding the eicosanoids. Cyclooxygenase (COX) oxidation removes two C=C double bonds, leading to the TX, PG and PGI series.
Lipoxygenase oxidation removes no C=C double bonds, and leads to the LK.
After oxidation, the eicosanoids are further modified, making a series. Members of a series are differentiated by an ABC...
letter, and are numbered by the number of double bonds, which does not
change within a series. For example, cyclooxygenase action upon AA (with 4 double bonds) leads to the series-2 thromboxanes (TXA2, TXB2... ) each with two double bonds. Cyclooxygenase action on EPA (with 5 double bonds) leads to the series-3 thromboxanes (TXA3, TXB3... ) each with three double bonds. There are exceptions to this pattern, some of which indicate stereochemistry (PGF2α).
Table (1) shows these sequences for AA (20:4 ω-6). The sequences for EPA (20:5 ω-3) and DGLA (20:3 ω-6) are analogous.
| Dietary Essential Fatty Acid |
Abbr | Formula carbons:double bonds ω |
Eicosanoid product series | ||
|---|---|---|---|---|---|
| TX PG PGI |
LK | Effects | |||
| Gamma-linolenic acid via Dihomo gamma linolenic acid |
GLA DGLA |
18:3ω6 20:3ω6 |
series-1 | series-3 | less inflammatory |
| Arachidonic acid | AA | 20:4ω6 | series-2 | series-4 | more inflammatory |
| Eicosapentaenoic acid | EPA | 20:5ω3 | series-3 | series-5 | less inflammatory |
All the prostenoids are substituted prostanoic acids.
Cyberlipid Center's Prostenoid page illustrates the parent compound and the rings associated with each series–letter.
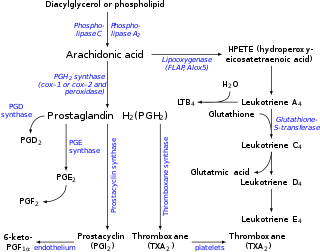
Arachidonic acid cascade in inflammation
In the arachidonic acid cascade, dietary linoleic acid (18:2 ω-6) is desaturated and lengthened to form arachidonic acid, esterified into a phospholipid in the cell membrane. Next, in response to many inflammatory stimuli, such as air pollution, smoking, second-hand smoke, hydrogenated vegetable oils and other exogenous toxins; phospholipase is generated and cleaves this phospholipid, releasing AA as a free fatty acid. AA can then be oxygenated and then further modified to form eicosanoids – autocrine and paracrine agents that bind receptors on the cell or its neighbors to alert the immune system of the cell damage. Alternatively, AA can diffuse into the cell nucleus and interact with transcription factors to control DNA transcription for cytokines or other hormones.
Mechanisms of ω-3 eicosanoid action
Figure (2) Essential fatty acid production and metabolism to form eicosanoids
The eicosanoids from AA generally promote inflammation. Those from GLA (via
DGLA) and from EPA are generally less inflammatory, or inactive, or
even anti-inflammatory. (This generalization is qualified: an
eicosanoid may be pro-inflammatory in one tissue and anti-inflammatory
in another. See discussion of PGE2 at Calder or Tilley.)
Figure (2) shows the ω-3 and -6 synthesis chains, along with the major eicosanoids from AA, EPA and DGLA.
Dietary ω-3 and GLA counter the inflammatory effects of AA's eicosanoids in three ways – displacement, competitive inhibition and direct counteraction.
Displacement
Dietary ω-3 decreases tissue concentrations of AA.
Animal studies show that increased dietary ω-3 results in decreased AA in brain and other tissue. Linolenic acid (18:3 ω-3) contributes to this by displacing linoleic acid (18:2 ω-6) from the elongase and desaturase enzymes that produce AA. EPA inhibits phospholipase A2's release of AA from cell membrane. Other mechanisms involving the transport of EFAs may also play a role.
The reverse is also true – high dietary linoleic acid decreases
the body's conversion of α-linolenic acid to EPA. However, the effect
is not as strong; the desaturase has a higher affinity for α-linolenic
acid than it has for linoleic acid.
Competitive Inhibition
DGLA
and EPA compete with AA for access to the cyclooxygenase and
lipoxygenase enzymes. So the presence of DGLA and EPA in tissues lowers
the output of AA's eicosanoids. For example, dietary GLA increases tissue DGLA and lowers TXB2. Likewise, EPA inhibits the production of series-2 PG and TX. Although DGLA forms no LTs, a DGLA derivative blocks the transformation of AA to LTs.
Counteraction
Some DGLA and EPA derived eicosanoids counteract their AA derived counterparts. For example, DGLA yields PGE1, which powerfully counteracts PGE2. EPA yields the antiaggregatory prostacyclin PGI3. It also yields the leuokotriene LTB5 which vitiates the action of the AA-derived LTB4.
The paradox of dietary GLA
Dietary oxidized linoleic acid
(LA, 18:2 ω-6) is inflammatory. In the body, LA is desaturated to form
GLA (18:3 ω-6), yet dietary GLA is anti-inflammatory. Some observations
partially explain this paradox: LA competes with α-linolenic acid,
(ALA, 18:3 ω-3) for Δ6-desaturase, and thereby eventually inhibits
formation of anti-inflammatory EPA (20:5 ω-3). In contrast, GLA does
not compete for Δ6-desaturase. GLA's elongation product DGLA
(20:3 ω-6) competes with 20:4 ω-3 for the Δ5-desaturase, and it might
be expected that this would make GLA inflammatory, but it is not,
perhaps because this step isn't rate-determining. Δ6-desaturase does appear to be the rate-limiting step; 20:4 ω-3 does not significantly accumulate in bodily lipids.
DGLA inhibits inflammation through both competitive inhibition and direct counteraction (see above.)
Dietary GLA leads to sharply increased DGLA in the white blood cells'
membranes, where LA does not. This may reflect white blood cells' lack
of desaturase. Supplementing dietary GLA increases serum DGLA without
increasing serum AA.
It is likely that some dietary GLA eventually forms AA and
contributes to inflammation. Animal studies indicate the effect is
small. The empirical observation of GLA's actual effects argues that DGLA's anti-inflammatory effects dominate.
Complexity of pathways
Eicosanoid signaling paths are complex.
It is therefore difficult to characterize the action of any particular eicosanoid.
For example, PGE2 binds four receptors, dubbed EP1–4.
Each is coded by a separate gene, and some exist in multiple isoforms.
Each EP receptor in turn couples to a G protein.
The EP2, EP4 and one isoform of the EP3 receptors couple to Gs.
This increases intracellular cAMP and is anti-inflammatory.
EP1 and other EP3 isoforms couple to Gq.
This leads to increased intracellular calcium and is pro-inflammatory.
Finally, yet another EP3 isoform couples to Gi, which both decreases cAMP and increases calcium.
Many immune-system cells express multiple receptors that couple these apparently opposing pathways.
Presumably, EPA-derived PGE3 has a somewhat different effect of on this system, but it is not well-characterized.
The arachidonic acid cascade in the central nervous system (CNS)
The arachidonic acid cascade is arguably the most elaborate signaling system neurobiologists have to deal with. Daniele Piomelli Arachidonic Acid
The arachidonic acid cascade proceeds somewhat differently in the brain. Neurohormones, neuromodulators or neurotransmitters act as first messengers. They activate phospholipidase to release AA from neuron cell membranes as a free fatty acid. During its short lifespan, free AA may affect the activity of the neuron's ion channels and protein kinases. Or it may be metabolized to form eicosanoids, epoxyeicosatrienoic acids (EETs), neuroprotectin D or various endocannabinoids (anandamide and its analogs.)
The actions of eicosanoids within the brain are not as well
characterized as they are in inflammation. It is theorized that they act
within the neuron as second messengers controlling presynaptic inhibition and the activation of protein kinase C.
They also act as paracrine mediators, acting across synapses to nearby
cells. Although detail on the effects of these signals is scant,
(Piomelli, 2000) comments:
Neurons in the CNS are organized as interconnected groups of functionally related cells (e.g., in sensory systems). A diffusible factor released from a neuron into the interstitial fluid, and able to interact with membrane receptors on adjacent cells, would be ideally used to "synchronize" the activity of an ensemble of interconnected neural cells. Furthermore, during development and in certain forms of learning, postsynaptic cells may secrete regulatory factors which diffuse back to the presynaptic component, determining its survival as an active terminal, the amplitude of its sprouting, and its efficacy in secreting neurotransmitters—a phenomenon known as retrograde regulation. The participation of arachidonic acid metabolites in retrograde signaling and in other forms of local modulation of neuronal activity has been proposed.
| Arachidonic Acid Cascade | ||
|---|---|---|
| In inflammation | In the brain | |
| Major effect on | Inflammation in tissue | Neuronal excitability |
| AA released from | White blood cells | Neurons |
| Triggers for AA release | Inflammatory stimuli | Neurotransmitters, neurohormones and neuromodulators |
| Intracellular effects on | DNA transcription of cytokines and other mediators of inflammation |
Activity of ion channels and protein kinases |
| Metabolized to form | Eicosanoids, resolvins, isofurans, isoprostanes, lipoxins, epoxyeicosatrienoic acids (EETs) |
Eicosanoids, neuroprotectin D, EETs and some endocannabinoids |
The EPA and DGLA cascades are also present in the brain and their
eicosanoid metabolites have been detected. The ways in which these
differently affect mental and neural processes are not nearly as well
characterized as are the effects in inflammation.
Further discussion
Figure (2) shows two pathways from EPA to DHA, including the exceptional Sprecher's shunt.
5-LO acts at the fifth carbon from the carboxyl group.
Other lipoxygenases—8-LO, 12-LO and 15-LO—make other eicosanoid-like products.
To act, 5-LO uses the nuclear-membrane enzyme 5-lipoxygenase-activating protein (FLAP), first to a hydroperoxyeicosatetraenoic acid (HPETE), then to the first leuokotriene, LTA.