| Zoonosis | |
|---|---|
| Other names | Zoönosis |
 | |
| A dog with rabies. | |
| Pronunciation | |
| Specialty | Infectious disease |
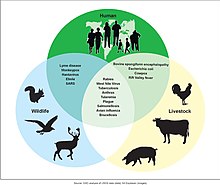
A zoonosis (plural zoonoses, or zoonotic diseases) is an infectious disease caused by a pathogen (an infectious agent, such as a bacterium, virus, parasite or prion) that has jumped from an animal (usually a vertebrate) to a human. Typically, the first infected human transmits the infectious agent to at least one other human, who, in turn, infects others.
Major modern diseases such as Ebola virus disease and salmonellosis are zoonoses. HIV was a zoonotic disease transmitted to humans in the early part of the 20th century, though it has now mutated to a separate human-only disease. Most strains of influenza that infect humans are human diseases, although many strains of bird flu and swine flu are zoonoses; these viruses occasionally recombine with human strains of the flu and can cause pandemics such as the 1918 Spanish flu or the 2009 swine flu. Taenia solium infection is one of the neglected tropical diseases with public health and veterinary concern in endemic regions. Zoonoses can be caused by a range of disease pathogens such as emergent viruses, bacteria, fungi and parasites; of 1,415 pathogens known to infect humans, 61% were zoonotic. Most human diseases originated in animals; however, only diseases that routinely involve non-human to human transmission, such as rabies, are considered direct zoonosis.
Zoonoses have different modes of transmission. In direct zoonosis the disease is directly transmitted from animals to humans through media such as air (influenza) or through bites and saliva (rabies). In contrast, transmission can also occur via an intermediate species (referred to as a vector), which carry the disease pathogen without getting sick. When humans infect animals, it is called reverse zoonosis or anthroponosis. The term is from Greek: ζῷον zoon "animal" and νόσος nosos "sickness".
Host genetics plays an important role in determining which animal viruses will be able to make copies of themselves in the human body. Dangerous animal viruses are those that require few mutations to begin replicating themselves in human cells. These viruses are dangerous since the required combinations of mutations might randomly arise in the natural reservoir.
Recently, there has been a rise in frequency of appearance of new zoonotic diseases. According to a report from the United Nations Environment Programme and International Livestock Research Institute named: "Preventing the next pandemic – Zoonotic diseases and how to break the chain of transmission" the causes are mostly environmental.
Causes
Zoonotic transmission can occur in any context in which there is contact with or consumption of animals, animal products, or animal derivatives. This can occur in a companionistic (pets), economic (farming, trade, butchering, etc.), predatory (hunting, butchering or consuming wild game) or research context. Recently, there has been a rise in frequency of appearance of new zoonotic diseases. According to a report from the United Nations Environment Programme and International Livestock Research Institute large part of the causes are environmental like climate change, unsustainable agriculture, exploitation of wildlife, land use change. Others are linked to changes in human society like more mobility. The organizations propose a set of measures to stop the rise.
Contamination of food or water supply
The most significant zoonotic pathogens causing foodborne diseases are Escherichia coli O157:H7, Campylobacter, Caliciviridae, and Salmonella.
In 2006 a conference held in Berlin focused on the issue of zoonotic pathogen effects on food safety, urging government intervention and public vigilance against the risks of catching food-borne diseases from farm-to-table dining.
Many food outbreaks can be linked to zoonotic pathogens. Many different types of food that have an animal origin can become contaminated. Some common foods linked to zoonotic contaminations include eggs, seafood, meat, dairy, and even some vegetables. Outbreaks involving contaminated food should be handled in preparedness plans to prevent widespread outbreaks and to efficiently and effectively contain outbreaks.
Farming, ranching and animal husbandry
Contact with farm animals can lead to disease in farmers or others that come into contact with infected farm animals. Glanders primarily affects those who work closely with horses and donkeys. Close contact with cattle can lead to cutaneous anthrax infection, whereas inhalation anthrax infection is more common for workers in slaughterhouses, tanneries and wool mills. Close contact with sheep who have recently given birth can lead to clamydiosis, or enzootic abortion, in pregnant women, as well as an increased risk of Q fever, toxoplasmosis, and listeriosis in pregnant or the otherwise immunocompromised. Echinococcosis is caused by a tapeworm which can be spread from infected sheep by food or water contaminated with feces or wool. Bird flu is common in chickens. While rare in humans, the main public health worry is that a strain of bird flu will recombine with a human flu virus and cause a pandemic like the 1918 Spanish flu. In 2017, free range chickens in the UK were temporarily ordered to remain inside due to the threat of bird flu. Cattle are an important reservoir of cryptosporidiosis and mainly affects the immunocompromised. Reports have shown Minks can also get infected.
Veterinarians are exposed to unique occupational hazards and zoonotic diseases. In the US, studies have highlighted an increased risk to injuries and a lack of veterinary awareness for these hazards. Research has proved the importance for continued clinical veterinarian education on occupational risks associated with musculoskeletal injuries, animal bites, needle-sticks, and cuts.
A July 2020 report by the United Nations Environment Programme stated that the increase in zoonotic pandemics is directly attributable to anthropogenic destruction of nature and the increased global demand for meat, and that the industrial farming of pigs and chickens in particular will be a primary risk factor for the spillover of zoonotic diseases in the future.
Wild animal attacks
Insect vectors
- African sleeping sickness
- Dirofilariasis
- Eastern equine encephalitis
- Japanese encephalitis
- Saint Louis encephalitis
- Scrub typhus
- Tularemia
- Venezuelan equine encephalitis
- West Nile fever
- Western equine encephalitis
- Zika fever
Pets
Pets can transmit a number of diseases. Dogs and cats are routinely vaccinated against rabies. Pets can also transmit ringworm and Giardia, which are endemic in both animal and human populations. Toxoplasmosis is a common infection of cats; in humans it is a mild disease although it can be dangerous to pregnant women. Dirofilariasis is caused by Dirofilaria immitis through mosquitoes infected by mammals like dogs and cats. Cat-scratch disease is caused by Bartonella henselae and Bartonella quintana from fleas which are endemic in cats. Toxocariasis is infection of humans of any of species of roundworm, including species specific to the dog (Toxocara canis) or the cat (Toxocara cati). Cryptosporidiosis can be spread to humans from pet lizards, such as the leopard gecko. Encephalitozoon cuniculi is a microsporidial parasite carried by many mammals, including rabbits, and is an important opportunistic pathogen in people immunocompromised by HIV/AIDS, organ transplantation, or CD4+ T-lymphocyte deficiency.
Exhibition
Outbreaks of zoonoses have been traced to human interaction with and exposure to other animals at fairs, live animal markets, petting zoos, and other settings. In 2005, the Centers for Disease Control and Prevention (CDC) issued an updated list of recommendations for preventing zoonosis transmission in public settings. The recommendations, developed in conjunction with the National Association of State Public Health Veterinarians, include educational responsibilities of venue operators, limiting public animal contact, and animal care and management.
Hunting and bushmeat
- HIV
- SARS
Deforestation, biodiversity loss and environmental degradation
Kate Jones, chair of ecology and biodiversity at University College London, says zoonotic diseases are increasingly linked to environmental change and human behaviour. The disruption of pristine forests driven by logging, mining, road building through remote places, rapid urbanisation and population growth is bringing people into closer contact with animal species they may never have been near before. The resulting transmission of disease from wildlife to humans, she says, is now "a hidden cost of human economic development". In a guest article published by IPBES, Peter Daszak and three co-chairs of the 2019 Global Assessment Report on Biodiversity and Ecosystem Services, Josef Settele, Sandra Díaz and Eduardo Brondizio, write that "rampant deforestation, uncontrolled expansion of agriculture, intensive farming, mining and infrastructure development, as well as the exploitation of wild species have created a ‘perfect storm’ for the spillover of diseases from wildlife to people."
An April 2020 study published in the Proceedings of the Royal Society Part B found that increased virus spillover events from animals to humans can be linked to biodiversity loss and environmental degradation, as humans further encroach on wildlands to engage in agriculture, hunting and resource extraction they become exposed to pathogens which normally would remain in these areas. Such spillover events have been tripling every decade since 1980. An August 2020 study published in Nature concludes that the anthropogenic destruction of ecosystems for the purpose of expanding agriculture and human settlements reduces biodiversity and allows for smaller animals such as bats and rats, who are more adaptable to human pressures and also carry the most zoonotic diseases, to proliferate. This in turn can result in more pandemics.
In October 2020, the Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services published its report on the 'era of pandemics' by 22 experts in a variety of fields, and concluded that anthropogenic destruction of biodiversity is paving the way to the pandemic era, and could result in as many as 850,000 viruses being transmitted from animals – in particular birds and mammals – to humans. The increased pressure on ecosystems is being driven by the "exponential rise" in consumption and trade of commodities such as meat, palm oil, and metals, largely facilitated by developed nations, and by a growing human population. According to Peter Daszak, the chair of the group who produced the report, "there is no great mystery about the cause of the Covid-19 pandemic, or of any modern pandemic. The same human activities that drive climate change and biodiversity loss also drive pandemic risk through their impacts on our environment."
Climate change
According to a report from the United Nations Environment Programme and International Livestock Research Institute named: "Preventing the next pandemic – Zoonotic diseases and how to break the chain of transmission" climate change is one of the 7 human – related causes of increase in the number of zoonotic diseases. The University of Sydney issued in March 2021 a study that examines factors, increasing the likelihood of epidemics and pandemics like the COVID-19 pandemic. The researchers found that "pressure on ecosystems, climate change and economic development are key factors" in doing so. More zoonotic diseases were found in high-income countries.
A 2021 study found possible links between climate change and transmission of COVID-19 by bats. The authors suggest that climate-driven changes in the distribution and richness of bat species harboring coronaviruses may have occurred in eastern Asian hotspots (southern China, Myanmar and Laos), constituting a driver behind the evolution and spread of the virus.
Secondary transmission
- Ebola and Marburg
History
During most of human prehistory groups of hunter-gatherers were probably very small. Such groups probably made contact with other such bands only rarely. Such isolation would have caused epidemic diseases to be restricted to any given local population, because propagation and expansion of epidemics depend on frequent contact with other individuals who have not yet developed an adequate immune response. To persist in such a population, a pathogen either had to be a chronic infection, staying present and potentially infectious in the infected host for long periods, or it had to have other additional species as reservoir where it can maintain itself until further susceptible hosts are contacted and infected. In fact, for many 'human' diseases, the human is actually better viewed as an accidental or incidental victim and a dead-end host. Examples include rabies, anthrax, tularemia and West Nile virus. Thus, much of human exposure to infectious disease has been zoonotic.
Through religious scripture, different civilizations as early as 500 years B.C.E had dietary laws that prohibit or allow the consumption of certain animals. Christian and Hebrew religions have reflected these traditions in the Book of Leviticus, while Islamic religions spread the laws throughout the Quran, referring to these rules as Haram and Halal. Some consider these dietary rules evolved, among other reasons, to reduce the risk of contracting diseases from animals.
Many modern diseases, even epidemic diseases, started out as zoonotic diseases. It is hard to establish with certainty which diseases jumped from other animals to humans, but there is increasing evidence from DNA and RNA sequencing, that measles, smallpox, influenza, HIV, and diphtheria came to humans this way. Various forms of the common cold and tuberculosis also are adaptations of strains originating in other species. Some experts have suggested that all human viral infections were originally zoonotic.
Zoonoses are of interest because they are often previously unrecognized diseases or have increased virulence in populations lacking immunity. The West Nile virus appeared in the United States in 1999 in the New York City area, and moved through the country in the summer of 2002, causing much distress. Bubonic plague is a zoonotic disease, as are salmonellosis, Rocky Mountain spotted fever, and Lyme disease.
A major factor contributing to the appearance of new zoonotic pathogens in human populations is increased contact between humans and wildlife. This can be caused either by encroachment of human activity into wilderness areas or by movement of wild animals into areas of human activity. An example of this is the outbreak of Nipah virus in peninsular Malaysia in 1999, when intensive pig farming began on the habitat of infected fruit bats. Unidentified infection of the pigs amplified the force of infection, eventually transmitting the virus to farmers and causing 105 human deaths.
Similarly, in recent times avian influenza and West Nile virus have spilled over into human populations probably due to interactions between the carrier host and domestic animals. Highly mobile animals such as bats and birds may present a greater risk of zoonotic transmission than other animals due to the ease with which they can move into areas of human habitation.
Because they depend on the human host for part of their life-cycle, diseases such as African schistosomiasis, river blindness, and elephantiasis are not defined as zoonotic, even though they may depend on transmission by insects or other vectors.