| Abortion | |
|---|---|
| Other names | Induced miscarriage, termination of pregnancy |
| Specialty | Obstetrics and gynecology |
| ICD-10-PCS | 10A0 |
| ICD-9-CM | 779.6 |
| MeSH | D000028 |
| MedlinePlus | 007382 |
Abortion is the termination of a pregnancy by removal or expulsion of an embryo or fetus. An abortion that occurs without intervention is known as a miscarriage or "spontaneous abortion"; these occur in approximately 30% to 40% of all pregnancies. When deliberate steps are taken to end a pregnancy, it is called an induced abortion, or less frequently "induced miscarriage". The unmodified word abortion generally refers to an induced abortion. The reasons why women have abortions are diverse and vary across the world. Reasons include maternal health, an inability to afford a child, domestic violence, lack of support, feeling they are too young, wishing to complete education or advance a career, and not being able or willing to raise a child conceived as a result of rape or incest.
When properly done, induced abortion is one of the safest procedures in medicine. In the United States, the risk of maternal mortality is 14 times lower after induced abortion than after childbirth. Unsafe abortions—those performed by people lacking the necessary skills, or in inadequately resourced settings—are responsible for between 5-13% of maternal deaths, especially in the developing world, though self-managed medication abortions are highly effective and safe. Public health data shows that making safe abortion legal and accessible reduces maternal deaths.
Modern methods use medication or surgery for abortions. The drug mifepristone in combination with prostaglandin appears to be as safe and effective as surgery during the first and second trimesters of pregnancy. The most common surgical technique involves dilating the cervix and using a suction device. Birth control, such as the pill or intrauterine devices, can be used immediately following abortion. When performed legally and safely on a woman who desires it, induced abortions do not increase the risk of long-term mental or physical problems. In contrast, unsafe abortions performed by unskilled individuals, with hazardous equipment, or in unsanitary facilities cause 47,000 deaths and 5 million hospital admissions each year. The World Health Organization states that "access to legal, safe and comprehensive abortion care, including post-abortion care, is essential for the attainment of the highest possible level of sexual and reproductive health". Historically, abortions have been attempted using herbal medicines, sharp tools, forceful massage, or other traditional methods.
Around 73 million abortions are performed each year in the world, with about 45% done unsafely. Abortion rates changed little between 2003 and 2008, before which they decreased for at least two decades as access to family planning and birth control increased. As of 2018, 37% of the world's women had access to legal abortions without limits as to reason. Countries that permit abortions have different limits on how late in pregnancy abortion is allowed. Abortion rates are similar between countries that restrict abortion and countries that broadly allow it, though this is partly because countries which restrict abortion tend to have higher unintended pregnancy rates.
There is debate over abortion with regard to moral, religious, ethical, and legal issues. Those who oppose abortion often argue that an embryo or fetus is a person with a right to life, and thus equate abortion with murder. Those who support the legality of abortion often argue that it is a woman's reproductive right. Others favor legal and accessible abortion as a public health measure.
Abortion laws and cultural or religious views of abortions are different around the world. In some areas, abortion is legal only in specific cases such as rape, fetal defects, poverty, risk to a woman's health, or incest.
Types
Induced
Approximately 205 million pregnancies occur each year worldwide. Over a third are unintended and about a fifth end in induced abortion. Most abortions result from unintended pregnancies. In the United Kingdom, 1 to 2% of abortions are done due to genetic problems in the fetus. A pregnancy can be intentionally aborted in several ways. The manner selected often depends upon the gestational age of the embryo or fetus, which increases in size as the pregnancy progresses.
Specific procedures may also be selected due to legality, regional availability, and doctor or a woman's personal preference. Reasons for procuring induced abortions are typically characterized as either therapeutic or elective. An abortion is medically referred to as a therapeutic abortion when it is performed to save the life of the pregnant woman; to prevent harm to the woman's physical or mental health; to terminate a pregnancy where indications are that the child will have a significantly increased chance of mortality or morbidity; or to selectively reduce the number of fetuses to lessen health risks associated with multiple pregnancy. An abortion is referred to as an elective or voluntary abortion when it is performed at the request of the woman for non-medical reasons. Confusion sometimes arises over the term elective because "elective surgery" generally refers to all scheduled surgery, whether medically necessary or not.
Spontaneous
Miscarriage, also known as spontaneous abortion, is the unintentional expulsion of an embryo or fetus before the 24th week of gestation. A pregnancy that ends before 37 weeks of gestation resulting in a live-born infant is a "premature birth" or a "preterm birth". When a fetus dies in utero after viability, or during delivery, it is usually termed "stillborn". Premature births and stillbirths are generally not considered to be miscarriages, although usage of these terms can sometimes overlap.
Studies of pregnant women in the US and China have shown that between 40% and 60% of embryos do not progress to birth. The vast majority of miscarriages occur before the woman is aware that she is pregnant, and many pregnancies spontaneously abort before medical practitioners can detect an embryo. Between 15% and 30% of known pregnancies end in clinically apparent miscarriage, depending upon the age and health of the pregnant woman. 80% of these spontaneous abortions happen in the first trimester.
The most common cause of spontaneous abortion during the first trimester is chromosomal abnormalities of the embryo or fetus, accounting for at least 50% of sampled early pregnancy losses. Other causes include vascular disease (such as lupus), diabetes, other hormonal problems, infection, and abnormalities of the uterus. Advancing maternal age and a woman's history of previous spontaneous abortions are the two leading factors associated with a greater risk of spontaneous abortion. A spontaneous abortion can also be caused by accidental trauma; intentional trauma or stress to cause miscarriage is considered induced abortion or feticide.
Methods
Medical
Medical abortions are those induced by abortifacient pharmaceuticals. Medical abortion became an alternative method of abortion with the availability of prostaglandin analogs in the 1970s and the antiprogestogen mifepristone (also known as RU-486) in the 1980s.
The most common early first trimester medical abortion regimens use mifepristone in combination with misoprostol (or sometimes another prostaglandin analog, gemeprost) up to 10 weeks (70 days) gestational age, methotrexate in combination with a prostaglandin analog up to 7 weeks gestation, or a prostaglandin analog alone. Mifepristone–misoprostol combination regimens work faster and are more effective at later gestational ages than methotrexate–misoprostol combination regimens, and combination regimens are more effective than misoprostol alone, particularly in the second trimester. Medical abortion regimens involving mifepristone followed by misoprostol in the cheek between 24 and 48 hours later are effective when performed before 70 days' gestation.
In very early abortions, up to 7 weeks gestation, medical abortion using a mifepristone–misoprostol combination regimen is considered to be more effective than surgical abortion (vacuum aspiration), especially when clinical practice does not include detailed inspection of aspirated tissue. Early medical abortion regimens using mifepristone, followed 24–48 hours later by buccal or vaginal misoprostol are 98% effective up to 9 weeks gestational age; from 9 to 10 weeks efficacy decreases modestly to 94%. If medical abortion fails, surgical abortion must be used to complete the procedure.
Early medical abortions account for the majority of abortions before 9 weeks gestation in Britain, France, Switzerland, United States, and the Nordic countries.
Medical abortion regimens using mifepristone in combination with a prostaglandin analog are the most common methods used for second trimester abortions in Canada, most of Europe, China and India, in contrast to the United States where 96% of second trimester abortions are performed surgically by dilation and evacuation.
A 2020 Cochrane Systematic Review concluded that providing women with medications to take home to complete the second stage of the procedure for an early medical abortion results in an effective abortion. Further research is required to determine if self-administered medical abortion is as safe as provider-administered medical abortion, where a health care professional is present to help manage the medical abortion. Safely permitting women to self-administer abortion medication has the potential to improve access to abortion. Other research gaps that were identified include how to best support women who choose to take the medication home for a self-administered abortion.
Surgical
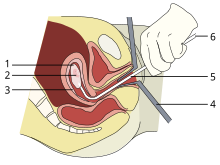
1: Amniotic sac
2: Embryo
3: Uterine lining
4: Speculum
5: Vacurette
6: Attached to a suction pump
Up to 15 weeks' gestation, suction-aspiration or vacuum aspiration are the most common surgical methods of induced abortion. Manual vacuum aspiration (MVA) consists of removing the fetus or embryo, placenta, and membranes by suction using a manual syringe, while electric vacuum aspiration (EVA) uses an electric pump. These techniques can both be used very early in pregnancy. MVA can be used up to 14 weeks but is more often used earlier in the U.S. EVA can be used later.
MVA, also known as "mini-suction" and "menstrual extraction", or EVA can be used in very early pregnancy when cervical dilation may not be required. Dilation and curettage (D&C) refers to opening the cervix (dilation) and removing tissue (curettage) via suction or sharp instruments. D&C is a standard gynecological procedure performed for a variety of reasons, including examination of the uterine lining for possible malignancy, investigation of abnormal bleeding, and abortion. The World Health Organization recommends sharp curettage only when suction aspiration is unavailable.
Dilation and evacuation (D&E), used after 12 to 16 weeks, consists of opening the cervix and emptying the uterus using surgical instruments and suction. D&E is performed vaginally and does not require an incision. Intact dilation and extraction (D&X) refers to a variant of D&E sometimes used after 18 to 20 weeks when removal of an intact fetus improves surgical safety or for other reasons.
Abortion may also be performed surgically by hysterotomy or gravid hysterectomy. Hysterotomy abortion is a procedure similar to a caesarean section and is performed under general anesthesia. It requires a smaller incision than a caesarean section and can be used during later stages of pregnancy. Gravid hysterectomy refers to removal of the whole uterus while still containing the pregnancy. Hysterotomy and hysterectomy are associated with much higher rates of maternal morbidity and mortality than D&E or induction abortion.
First trimester procedures can generally be performed using local anesthesia, while second trimester methods may require deep sedation or general anesthesia.
Labor induction abortion
In places lacking the necessary medical skill for dilation and extraction, or when preferred by practitioners, an abortion can be induced by first inducing labor and then inducing fetal demise if necessary. This is sometimes called "induced miscarriage". This procedure may be performed from 13 weeks gestation to the third trimester. Although it is very uncommon in the United States, more than 80% of induced abortions throughout the second trimester are labor-induced abortions in Sweden and other nearby countries.
Only limited data are available comparing labor-induced abortion with the dilation and extraction method. Unlike D&E, labor-induced abortions after 18 weeks may be complicated by the occurrence of brief fetal survival, which may be legally characterized as live birth. For this reason, labor-induced abortion is legally risky in the United States.
Other methods
Historically, a number of herbs reputed to possess abortifacient properties have been used in folk medicine. Among these are: tansy, pennyroyal, black cohosh, and the now-extinct silphium.
In 1978, one woman in Colorado died and another developed organ damage when they attempted to terminate their pregnancies by taking pennyroyal oil. Because the indiscriminant use of herbs as abortifacients can cause serious—even lethal—side effects, such as multiple organ failure, such use is not recommended by physicians.
Abortion is sometimes attempted by causing trauma to the abdomen. The degree of force, if severe, can cause serious internal injuries without necessarily succeeding in inducing miscarriage. In Southeast Asia, there is an ancient tradition of attempting abortion through forceful abdominal massage. One of the bas reliefs decorating the temple of Angkor Wat in Cambodia depicts a demon performing such an abortion upon a woman who has been sent to the underworld.
Reported methods of unsafe, self-induced abortion include misuse of misoprostol and insertion of non-surgical implements such as knitting needles and clothes hangers into the uterus. These and other methods to terminate pregnancy may be called "induced miscarriage". Such methods are rarely used in countries where surgical abortion is legal and available.
Safety
The health risks of abortion depend principally upon whether the procedure is performed safely or unsafely. The World Health Organization (WHO) defines unsafe abortions as those performed by unskilled individuals, with hazardous equipment, or in unsanitary facilities. Legal abortions performed in the developed world are among the safest procedures in medicine. In the United States as of 2012, abortion was estimated to be about 14 times safer for women than childbirth. CDC estimated in 2019 that US pregnancy-related mortality was 17.2 maternal deaths per 100,000 live births, while the US abortion mortality rate is 0.7 maternal deaths per 100,000 procedures. In the UK, guidelines of the Royal College of Obstetricians and Gynaecologists state that "Women should be advised that abortion is generally safer than continuing a pregnancy to term." Worldwide, on average, abortion is safer than carrying a pregnancy to term. A 2007 study reported that "26% of all pregnancies worldwide are terminated by induced abortion," whereas "deaths from improperly performed [abortion] procedures constitute 13% of maternal mortality globally." In Indonesia in 2000 it was estimated that 2 million pregnancies ended in abortion, 4.5 million pregnancies were carried to term, and 14-16 percent of maternal deaths resulted from abortion.
In the US from 2000 to 2009, abortion had a mortality rate lower than plastic surgery, lower or similar to running a marathon, and about equivalent to traveling 760 miles (1,220 km) in a passenger car. Five years after seeking abortion services, women who gave birth after being denied an abortion reported worse health than women who had either first or second trimester abortions. The risk of abortion-related mortality increases with gestational age, but remains lower than that of childbirth. Outpatient abortion is as safe from 64 to 70 days' gestation as it before 63 days.
There is little difference in terms of safety and efficacy between medical abortion using a combined regimen of mifepristone and misoprostol and surgical abortion (vacuum aspiration) in early first trimester abortions up to 10 weeks gestation. Medical abortion using the prostaglandin analog misoprostol alone is less effective and more painful than medical abortion using a combined regimen of mifepristone and misoprostol or surgical abortion.
Vacuum aspiration in the first trimester is the safest method of surgical abortion, and can be performed in a primary care office, abortion clinic, or hospital. Complications, which are rare, can include uterine perforation, pelvic infection, and retained products of conception requiring a second procedure to evacuate. Infections account for one-third of abortion-related deaths in the United States. The rate of complications of vacuum aspiration abortion in the first trimester is similar regardless of whether the procedure is performed in a hospital, surgical center, or office. Preventive antibiotics (such as doxycycline or metronidazole) are typically given before abortion procedures, as they are believed to substantially reduce the risk of postoperative uterine infection; however, antibiotics are not routinely given with abortion pills. The rate of failed procedures does not appear to vary significantly depending on whether the abortion is performed by a doctor or a mid-level practitioner.
Complications after second trimester abortion are similar to those after first trimester abortion, and depend somewhat on the method chosen. The risk of death from abortion approaches roughly half the risk of death from childbirth the farther along a woman is in pregnancy; from one in a million before 9 weeks gestation to nearly one in ten.