| Chemotherapy | |
|---|---|

A woman being treated with docetaxel chemotherapy for breast cancer. Cold mittens and wine coolers are placed on her hands and feet to reduce harm to her nails.
| |
| Synonyms | chemo |
Chemotherapy (often abbreviated to chemo and sometimes CTX or CTx) is a type of cancer treatment that uses one or more anti-cancer drugs (chemotherapeutic agents) as part of a standardized chemotherapy regimen. Chemotherapy may be given with a curative intent (which almost always involves combinations of drugs), or it may aim to prolong life or to reduce symptoms (palliative chemotherapy). Chemotherapy is one of the major categories of the medical discipline specifically devoted to pharmacotherapy for cancer, which is called medical oncology.
The term chemotherapy has come to connote non-specific usage of intracellular poisons to inhibit mitosis, cell division. The connotation excludes more selective agents that block extracellular signals (signal transduction). The development of therapies with specific molecular or genetic targets, which inhibit growth-promoting signals from classic endocrine hormones (primarily estrogens for breast cancer and androgens for prostate cancer) are now called hormonal therapies. By contrast, other inhibitions of growth-signals like those associated with receptor tyrosine kinases are referred to as targeted therapy.
Importantly, the use of drugs (whether chemotherapy, hormonal therapy or targeted therapy) constitutes systemic therapy for cancer in that they are introduced into the blood stream and are therefore in principle able to address cancer at any anatomic location in the body. Systemic therapy is often used in conjunction with other modalities that constitute local therapy (i.e. treatments whose efficacy is confined to the anatomic area where they are applied) for cancer such as radiation therapy, surgery or hyperthermia therapy.
Traditional chemotherapeutic agents are cytotoxic by means of interfering with cell division (mitosis) but cancer cells vary widely in their susceptibility to these agents. To a large extent, chemotherapy can be thought of as a way to damage or stress cells, which may then lead to cell death if apoptosis is initiated. Many of the side effects of chemotherapy can be traced to damage to normal cells that divide rapidly and are thus sensitive to anti-mitotic drugs: cells in the bone marrow, digestive tract and hair follicles. This results in the most common side-effects of chemotherapy: myelosuppression (decreased production of blood cells, hence also immunosuppression), mucositis (inflammation of the lining of the digestive tract), and alopecia (hair loss). Because of the effect on immune cells (especially lymphocytes), chemotherapy drugs often find use in a host of diseases that result from harmful overactivity of the immune system against self (so-called autoimmunity). These include rheumatoid arthritis, systemic lupus erythematosus, multiple sclerosis, vasculitis and many others.
Treatment strategies
| Cancer type | Drugs | Acronym |
|---|---|---|
| Breast cancer | Cyclophosphamide, methotrexate, 5-fluorouracil, vinorelbine | CMF |
| Doxorubicin, cyclophosphamide | AC | |
| Hodgkin's lymphoma | Docetaxel, doxorubicin, cyclophosphamide | TAC |
| Doxorubicin, bleomycin, vinblastine, dacarbazine | ABVD | |
| Mustine, vincristine, procarbazine, prednisolone | MOPP | |
| Non-Hodgkin's lymphoma | Cyclophosphamide, doxorubicin, vincristine, prednisolone | CHOP |
| Germ cell tumor | Bleomycin, etoposide, cisplatin | BEP |
| Stomach cancer | Epirubicin, cisplatin, 5-fluorouracil | ECF |
| Epirubicin, cisplatin, capecitabine | ECX | |
| Bladder cancer | Methotrexate, vincristine, doxorubicin, cisplatin | MVAC |
| Lung cancer | Cyclophosphamide, doxorubicin, vincristine, vinorelbine | CAV |
| Colorectal cancer | 5-fluorouracil, folinic acid, oxaliplatin | FOLFOX |
There are a number of strategies in the administration of chemotherapeutic drugs used today. Chemotherapy may be given with a curative intent or it may aim to prolong life or to palliate symptoms.
- Induction chemotherapy is the first line treatment of cancer with a chemotherapeutic drug. This type of chemotherapy is used for curative intent.
- Combined modality chemotherapy is the use of drugs with other cancer treatments, such as surgery, radiation therapy, or hyperthermia therapy.
- Consolidation chemotherapy is given after remission in order to prolong the overall disease-free time and improve overall survival. The drug that is administered is the same as the drug that achieved remission.
- Intensification chemotherapy is identical to consolidation chemotherapy but a different drug than the induction chemotherapy is used.
- Combination chemotherapy involves treating a person with a number of different drugs simultaneously. The drugs differ in their mechanism and side-effects. The biggest advantage is minimising the chances of resistance developing to any one agent. Also, the drugs can often be used at lower doses, reducing toxicity.
- Neoadjuvant chemotherapy is given prior to a local treatment such as surgery, and is designed to shrink the primary tumor. It is also given to cancers with a high risk of micrometastatic disease.
- Adjuvant chemotherapy is given after a local treatment (radiotherapy or surgery). It can be used when there is little evidence of cancer present, but there is risk of recurrence. It is also useful in killing any cancerous cells that have spread to other parts of the body. These micrometastases can be treated with adjuvant chemotherapy and can reduce relapse rates caused by these disseminated cells.
- Maintenance chemotherapy is a repeated low-dose treatment to prolong remission.
- Salvage chemotherapy or palliative chemotherapy is given without curative intent, but simply to decrease tumor load and increase life expectancy. For these regimens, in general, a better toxicity profile is expected.
All chemotherapy regimens require that the recipient be capable of undergoing the treatment. Performance status
is often used as a measure to determine whether a person can receive
chemotherapy, or whether dose reduction is required. Because only a
fraction of the cells in a tumor die with each treatment (fractional kill), repeated doses must be administered to continue to reduce the size of the tumor.
Current chemotherapy regimens apply drug treatment in cycles, with the
frequency and duration of treatments limited by toxicity.
Efficacy
The
efficacy of chemotherapy depends on the type of cancer and the stage.
The overall effectiveness ranges from being curative for some cancers,
such as some leukemias, to being ineffective, such as in some brain tumors, to being needless in others, like most non-melanoma skin cancers.
Dosage
Dose
response relationship of cell killing by chemotherapeutic drugs on
normal and cancer cells. At high doses the percentage of normal and
cancer cells killed is very similar. For this reason, doses are chosen
where anti-tumor activity exceeds normal cell death.
Dosage of chemotherapy can be difficult: If the dose is too low, it
will be ineffective against the tumor, whereas, at excessive doses, the
toxicity (side-effects) will be intolerable to the person receiving it. The standard method of determining chemotherapy dosage is based on calculated body surface area (BSA). The BSA is usually calculated with a mathematical formula or a nomogram,
using the recipient's weight and height, rather than by direct
measurement of body area. This formula was originally derived in a 1916
study and attempted to translate medicinal doses established with
laboratory animals to equivalent doses for humans. The study only included 9 human subjects.
When chemotherapy was introduced in the 1950s, the BSA formula was
adopted as the official standard for chemotherapy dosing for lack of a
better option.
Recently, the validity of this method in calculating uniform
doses has been questioned. The reason for this is that the formula only
takes into account the individual's weight and height. Drug absorption
and clearance are influenced by multiple factors, including age, gender,
metabolism, disease state, organ function, drug-to-drug interactions,
genetics, and obesity, which has a major impact on the actual
concentration of the drug in the person's bloodstream.
As a result, there is high variability in the systemic chemotherapy
drug concentration in people dosed by BSA, and this variability has been
demonstrated to be more than 10-fold for many drugs.
In other words, if two people receive the same dose of a given drug
based on BSA, the concentration of that drug in the bloodstream of one
person may be 10 times higher or lower compared to that of the other
person.
This variability is typical with many chemotherapy drugs dosed by BSA,
and, as shown below, was demonstrated in a study of 14 common
chemotherapy drugs.
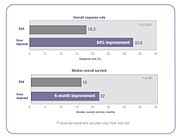
5-FU dose management results in significantly better response and survival rates versus BSA dosing.
The result of this pharmacokinetic variability among people, is that
many people do not receive the right dose to achieve optimal treatment
effectiveness with minimized toxic side effects. Some people are
overdosed while others are underdosed.
For example, in a randomized clinical trial, investigators found 85% of
metastatic colorectal cancer patients treated with 5-fluorouracil
(5-FU) did not receive the optimal therapeutic dose when dosed by the
BSA standard—68% were underdosed and 17% were overdosed.
There has been controversy over the use of BSA to calculate chemotherapy doses for people who are obese. Because of their higher BSA, clinicians often arbitrarily reduce the dose prescribed by the BSA formula for fear of overdosing. In many cases, this can result in sub-optimal treatment.
Several clinical studies have demonstrated that when chemotherapy
dosing is individualized to achieve optimal systemic drug exposure,
treatment outcomes are improved and toxic side effects are reduced.
In the 5-FU clinical study cited above, people whose dose was adjusted
to achieve a pre-determined target exposure realized an 84% improvement
in treatment response rate and a six-month improvement in overall
survival (OS) compared with those dosed by BSA.
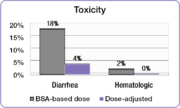
5-FU dose management avoids serious side effects experienced with BSA dosing
In the same study, investigators compared the incidence of common
5-FU-associated grade 3/4 toxicities between the dose-adjusted people
and people dosed per BSA.
The incidence of debilitating grades of diarrhea was reduced from 18%
in the BSA-dosed group to 4% in the dose-adjusted group and serious
hematologic side effects were eliminated. Because of the reduced toxicity, dose-adjusted patients were able to be treated for longer periods of time.
BSA-dosed people were treated for a total of 680 months while people in
the dose-adjusted group were treated for a total of 791 months.
Completing the course of treatment is an important factor in achieving better treatment outcomes.
Similar results were found in a study involving people with colorectal cancer who were treated with the popular FOLFOX regimen.
The incidence of serious diarrhea was reduced from 12% in the BSA-dosed
group of patients to 1.7% in the dose-adjusted group, and the incidence
of severe mucositis was reduced from 15% to 0.8%.
The FOLFOX study also demonstrated an improvement in treatment outcomes.
Positive response increased from 46% in the BSA-dosed group to 70% in
the dose-adjusted group. Median progression free survival (PFS) and
overall survival (OS) both improved by six months in the dose adjusted
group.
One approach that can help clinicians individualize chemotherapy
dosing is to measure the drug levels in blood plasma over time and
adjust dose according to a formula or algorithm to achieve optimal
exposure. With an established target exposure for optimized treatment
effectiveness with minimized toxicities, dosing can be personalized to
achieve target exposure and optimal results for each person. Such an
algorithm was used in the clinical trials cited above and resulted in
significantly improved treatment outcomes.
Oncologists are already individualizing dosing of some cancer drugs based on exposure. Carboplatin and busulfan
dosing rely upon results from blood tests to calculate the optimal dose
for each person. Simple blood tests are also available for dose
optimization of methotrexate, 5-FU, paclitaxel, and docetaxel.
The serum albumin level immediately prior to chemotherapy
administration is an independent prognostic predictor of survival in
various cancer types.
It has been proposed that a greater serum albumin level - such as that
achieved by albumin pre-administration prior to chemotherapy - adjusts
the albumin to drug molar ratio closer to 1.0. This has the effect of
sparing the drug from degradation or elimination by the hepatic monocyte
macrophages, resulting in a greater accumulation of the drug in the
tumor. This approach has the advantage that it is patient clinical status agnostic.
Types
Two
DNA bases that are cross-linked by a nitrogen mustard. Different
nitrogen mustards will have different chemical groups (R). The nitrogen
mustards most commonly alkylate the N7 nitrogen of guanine (as shown
here) but other atoms can be alkylated.
Alkylating agents
Alkylating agents are the oldest group of chemotherapeutics in use today. Originally derived from mustard gas used in World War I, there are now many types of alkylating agents in use. They are so named because of their ability to alkylate many molecules, including proteins, RNA and DNA. This ability to bind covalently to DNA via their alkyl group is the primary cause for their anti-cancer effects.
DNA is made of two strands and the molecules may either bind twice to
one strand of DNA (intrastrand crosslink) or may bind once to both
strands (interstrand crosslink). If the cell tries to replicate
crosslinked DNA during cell division, or tries to repair it, the DNA strands can break. This leads to a form of programmed cell death called apoptosis.
Alkylating agents will work at any point in the cell cycle and thus are
known as cell cycle-independent drugs. For this reason the effect on
the cell is dose dependent; the fraction of cells that die is directly
proportional to the dose of drug.
The subtypes of alkylating agents are the nitrogen mustards, nitrosoureas, tetrazines, aziridines, cisplatins and derivatives, and non-classical alkylating agents. Nitrogen mustards include mechlorethamine, cyclophosphamide, melphalan, chlorambucil, ifosfamide and busulfan. Nitrosoureas include N-Nitroso-N-methylurea (MNU), carmustine (BCNU), lomustine (CCNU) and semustine (MeCCNU), fotemustine and streptozotocin. Tetrazines include dacarbazine, mitozolomide and temozolomide. Aziridines include thiotepa, mytomycin and diaziquone (AZQ). Cisplatin and derivatives include cisplatin, carboplatin and oxaliplatin. They impair cell function by forming covalent bonds with the amino, carboxyl, sulfhydryl, and phosphate groups in biologically important molecules. Non-classical alkylating agents include procarbazine and hexamethylmelamine.
Antimetabolites
Deoxycytidine (left) and two anti-metabolite drugs (center and right); gemcitabine and decitabine. The drugs are very similar but they have subtle differences in their chemical structure.
Anti-metabolites
are a group of molecules that impede DNA and RNA synthesis. Many of
them have a similar structure to the building blocks of DNA and RNA. The
building blocks are nucleotides; a molecule comprising a nucleobase, a sugar and a phosphate group. The nucleobases are divided into purines (guanine and adenine) and pyrimidines (cytosine, thymine and uracil). Anti-metabolites resemble either nucleobases or nucleosides (a nucleotide without the phosphate group), but have altered chemical groups.
These drugs exert their effect by either blocking the enzymes required
for DNA synthesis or becoming incorporated into DNA or RNA. By
inhibiting the enzymes involved in DNA synthesis, they prevent mitosis
because the DNA cannot duplicate itself. Also, after misincorporation of
the molecules into DNA, DNA damage can occur and programmed cell death (apoptosis)
is induced. Unlike alkylating agents, anti-metabolites are cell cycle
dependent. This means that they only work during a specific part of the
cell cycle, in this case S-phase
(the DNA synthesis phase). For this reason, at a certain dose, the
effect plateaus and proportionally no more cell death occurs with
increased doses. Subtypes of the anti-metabolites are the anti-folates, fluoropyrimidines, deoxynucleoside analogues and thiopurines.
The anti-folates include methotrexate and pemetrexed. Methotrexate inhibits dihydrofolate reductase (DHFR), an enzyme that regenerates tetrahydrofolate from dihydrofolate. When the enzyme is inhibited by methotrexate, the cellular levels of folate coenzymes diminish. These are required for thymidylate and purine production, which are both essential for DNA synthesis and cell division.
Pemetrexed is another anti-metabolite that affects purine and
pyrimidine production, and therefore also inhibits DNA synthesis. It
primarily inhibits the enzyme thymidylate synthase, but also has effects on DHFR, aminoimidazole carboxamide ribonucleotide formyltransferase and glycinamide ribonucleotide formyltransferase. The fluoropyrimidines include fluorouracil and capecitabine.
Fluorouracil is a nucleobase analogue that is metabolised in cells to
form at least two active products; 5-fluourouridine monophosphate (FUMP)
and 5-fluoro-2'-deoxyuridine 5'-phosphate (fdUMP). FUMP becomes
incorporated into RNA and fdUMP inhibits the enzyme thymidylate
synthase; both of which lead to cell death. Capecitabine is a prodrug of 5-fluorouracil that is broken down in cells to produce the active drug. The deoxynucleoside analogues include cytarabine, gemcitabine, decitabine, azacitidine, fludarabine, nelarabine, cladribine, clofarabine, and pentostatin. The thiopurines include thioguanine and mercaptopurine.
Anti-microtubule agents
Vinca
alkaloids prevent the assembly of microtubules, whereas taxanes prevent
their disassembly. Both mechanisms cause defective mitosis.
Anti-microtubule agents are plant-derived chemicals that block cell division by preventing microtubule function. Microtubules are an important cellular structure composed of two proteins; α-tubulin and β-tubulin. They are hollow rod shaped structures that are required for cell division, among other cellular functions. Microtubules are dynamic structures, which means that they are permanently in a state of assembly and disassembly. Vinca alkaloids and taxanes
are the two main groups of anti-microtubule agents, and although both
of these groups of drugs cause microtubule dysfunction, their mechanisms
of action are completely opposite. The vinca alkaloids prevent the
formation of the microtubules, whereas the taxanes prevent the
microtubule disassembly. By doing so, they prevent the cancer cells from
completing mitosis. Following this, cell cycle arrest occurs, which
induces programmed cell death (apoptosis). Also, these drugs can affect blood vessel growth; an essential process that tumours utilise in order to grow and metastasise.
Vinca alkaloids are derived from the Madagascar periwinkle, Catharanthus roseus (formerly known as Vinca rosea). They bind to specific sites on tubulin, inhibiting the assembly of tubulin into microtubules. The original vinca alkaloids are natural products that include vincristine and vinblastine. Following the success of these drugs, semi-synthetic vinca alkaloids were produced: vinorelbine (used in the treatment of non-small-cell lung cancer), vindesine, and vinflunine. These drugs are cell cycle-specific. They bind to the tubulin molecules in S-phase and prevent proper microtubule formation required for M-phase.
Taxanes are natural and semi-synthetic drugs. The first drug of their class, paclitaxel, was originally extracted from the Pacific Yew tree, Taxus brevifolia. Now this drug and another in this class, docetaxel, are produced semi-synthetically from a chemical found in the bark of another Yew tree; Taxus baccata.
These drugs promote microtubule stability, preventing their
disassembly. Paclitaxel prevents the cell cycle at the boundary of G2-M,
whereas docetaxel exerts its effect during S-phase. Taxanes present difficulties in formulation as medicines because they are poorly soluble in water.
Podophyllotoxin is an antineoplastic lignan obtained primarily from the American Mayapple (Podophyllum peltatum) and Himalayan Mayapple (Podophyllum hexandrum or Podophyllum emodi). It has anti-microtubule activity, and its mechanism is similar to that of vinca
alkaloids in that they bind to tubulin, inhibiting microtubule
formation. Podophyllotoxin is used to produce two other drugs with
different mechanisms of action: etoposide and teniposide.
Topoisomerase inhibitors
Topoisomerase I and II Inhibitors
Topoisomerase inhibitors are drugs that affect the activity of two enzymes: topoisomerase I and topoisomerase II. When the DNA double-strand helix is unwound, during DNA replication or transcription,
for example, the adjacent unopened DNA winds tighter (supercoils), like
opening the middle of a twisted rope. The stress caused by this effect
is in part aided by the topoisomerase enzymes. They produce single- or
double-strand breaks into DNA, reducing the tension in the DNA strand.
This allows the normal unwinding of DNA to occur during replication or transcription. Inhibition of topoisomerase I or II interferes with both of these processes.
Two topoisomerase I inhibitors, irinotecan and topotecan, are semi-synthetically derived from camptothecin, which is obtained from the Chinese ornamental tree Camptotheca acuminata.
Drugs that target topoisomerase II can be divided into two groups. The
topoisomerase II poisons cause increased levels enzymes bound to DNA.
This prevents DNA replication and transcription, causes DNA strand breaks, and leads to programmed cell death (apoptosis). These agents include etoposide, doxorubicin, mitoxantrone and teniposide.
The second group, catalytic inhibitors, are drugs that block the
activity of topoisomerase II, and therefore prevent DNA synthesis and
translation because the DNA cannot unwind properly. This group includes novobiocin, merbarone, and aclarubicin, which also have other significant mechanisms of action.
Cytotoxic antibiotics
The cytotoxic antibiotics
are a varied group of drugs that have various mechanisms of action. The
common theme that they share in their chemotherapy indication is that
they interrupt cell division. The most important subgroup is the anthracyclines and the bleomycins; other prominent examples include mitomycin C, mitoxantrone, and actinomycin.
Among the anthracyclines, doxorubicin and daunorubicin were the first, and were obtained from the bacterium Streptomyces peucetius. Derivatives of these compounds include epirubicin and idarubicin. Other clinically used drugs in the anthracyline group are pirarubicin, aclarubicin, and mitoxantrone. The mechanisms of anthracyclines include DNA intercalation (molecules insert between the two strands of DNA), generation of highly reactive free radicals that damage intercellular molecules and topoisomerase inhibition.
Actinomycin is a complex molecule that intercalates DNA and prevents RNA synthesis.
Bleomycin, a glycopeptide isolated from Streptomyces verticillus, also intercalates DNA, but produces free radicals that damage DNA. This occurs when bleomycin binds to a metal ion, becomes chemically reduced and reacts with oxygen.
Mitomycin is a cytotoxic antibiotic with the ability to alkylate DNA.
Delivery
Two girls with acute lymphoblastic leukemia receiving chemotherapy. The girl at left has a central venous catheter inserted in her neck. The girl at right has a peripheral venous catheter. The arm board stabilizes the arm during needle insertion. Anti-cancer IV drip is seen at top right.
Most chemotherapy is delivered intravenously, although a number of agents can be administered orally (e.g., melphalan, busulfan, capecitabine).
There are many intravenous methods of drug delivery, known as vascular access devices. These include the winged infusion device, peripheral venous catheter, midline catheter, peripherally inserted central catheter (PICC), central venous catheter and implantable port.
The devices have different applications regarding duration of
chemotherapy treatment, method of delivery and types of chemotherapeutic
agent.
Depending on the person, the cancer, the stage of cancer, the
type of chemotherapy, and the dosage, intravenous chemotherapy may be
given on either an inpatient or an outpatient
basis. For continuous, frequent or prolonged intravenous chemotherapy
administration, various systems may be surgically inserted into the
vasculature to maintain access. Commonly used systems are the Hickman line, the Port-a-Cath, and the PICC line. These have a lower infection risk, are much less prone to phlebitis or extravasation, and eliminate the need for repeated insertion of peripheral cannulae.
Isolated limb perfusion (often used in melanoma), or isolated infusion of chemotherapy into the liver
or the lung have been used to treat some tumors. The main purpose of
these approaches is to deliver a very high dose of chemotherapy to tumor
sites without causing overwhelming systemic damage.
These approaches can help control solitary or limited metastases, but
they are by definition not systemic, and, therefore, do not treat
distributed metastases or micrometastases.
Topical chemotherapies, such as 5-fluorouracil, are used to treat some cases of non-melanoma skin cancer.
If the cancer has central nervous system involvement, or with meningeal disease, intrathecal chemotherapy may be administered.
Adverse effects
Chemotherapeutic
techniques have a range of side-effects that depend on the type of
medications used. The most common medications affect mainly the fast-dividing cells
of the body, such as blood cells and the cells lining the mouth,
stomach, and intestines. Chemotherapy-related toxicities can occur
acutely after administration, within hours or days, or chronically, from
weeks to years.
Immunosuppression and myelosuppression
Virtually all chemotherapeutic regimens can cause depression of the immune system, often by paralysing the bone marrow and leading to a decrease of white blood cells, red blood cells, and platelets.
Anemia and thrombocytopenia may require blood transfusion. Neutropenia (a decrease of the neutrophil granulocyte count below 0.5 x 109/litre) can be improved with synthetic G-CSF (granulocyte-colony-stimulating factor, e.g., filgrastim, lenograstim).
In very severe myelosuppression, which occurs in some regimens, almost all the bone marrow stem cells (cells that produce white and red blood cells) are destroyed, meaning allogenic or autologous bone marrow cell transplants
are necessary. (In autologous BMTs, cells are removed from the person
before the treatment, multiplied and then re-injected afterward; in allogenic BMTs, the source is a donor.) However, some people still develop diseases because of this interference with bone marrow.
Although people receiving chemotherapy are encouraged to wash
their hands, avoid sick people, and take other infection-reducing steps,
about 85% of infections are due to naturally occurring microorganisms
in the person's own gastrointestinal tract (including oral cavity) and skin. This may manifest as systemic infections, such as sepsis, or as localized outbreaks, such as Herpes simplex, shingles, or other members of the Herpesviridea. The risk of illness and death can be reduced by taking common antibiotics such as quinolones or trimethoprim/sulfamethoxazole before any fever or sign of infection appears. Quinolones show effective prophylaxis mainly with hematological cancer.
However, in general, for every five people who are immunosuppressed
following chemotherapy who take an antibiotic, one fever can be
prevented; for every 34 who take an antibiotic, one death can be
prevented. Sometimes, chemotherapy treatments are postponed because the immune system is suppressed to a critically low level.
In Japan, the government has approved the use of some medicinal mushrooms like Trametes versicolor, to counteract depression of the immune system in people undergoing chemotherapy.
Neutropenic enterocolitis
Due to immune system suppression, neutropenic enterocolitis (typhlitis) is a "life-threatening gastrointestinal complication of chemotherapy." Typhlitis is an intestinal infection which may manifest itself through symptoms including nausea, vomiting, diarrhea, a distended abdomen, fever, chills, or abdominal pain and tenderness.
Typhlitis is a medical emergency. It has a very poor prognosis and is often fatal unless promptly recognized and aggressively treated.
Successful treatment hinges on early diagnosis provided by a high index
of suspicion and the use of CT scanning, nonoperative treatment for
uncomplicated cases, and sometimes elective right hemicolectomy to prevent recurrence.
Gastrointestinal distress
Nausea, vomiting, anorexia, diarrhoea, abdominal cramps, and constipation are common side-effects of chemotherapeutic medications that kill fast-dividing cells. Malnutrition and dehydration
can result when the recipient does not eat or drink enough, or when the
person vomits frequently, because of gastrointestinal damage. This can
result in rapid weight loss, or occasionally in weight gain, if the
person eats too much in an effort to allay nausea or heartburn. Weight
gain can also be caused by some steroid medications. These side-effects
can frequently be reduced or eliminated with antiemetic drugs. Self-care measures, such as eating frequent small meals and drinking clear liquids or ginger
tea, are often recommended. In general, this is a temporary effect, and
frequently resolves within a week of finishing treatment. However, a
high index of suspicion is appropriate, since diarrhea and bloating are also symptoms of typhlitis, a very serious and potentially life-threatening medical emergency that requires immediate treatment.
Anemia
Anemia can be a combined outcome caused by myelosuppressive chemotherapy, and possible cancer-related causes such as bleeding, blood cell destruction (hemolysis), hereditary disease, kidney dysfunction, nutritional
deficiencies or anemia of chronic disease. Treatments to mitigate anemia include hormones to boost blood production (erythropoietin), iron supplements, and blood transfusions.
Myelosuppressive therapy can cause a tendency to bleed easily, leading
to anemia. Medications that kill rapidly dividing cells or blood cells
can reduce the number of platelets in the blood, which can result in bruises and bleeding. Extremely low platelet counts may be temporarily boosted through platelet transfusions and new drugs to increase platelet counts during chemotherapy are being developed. Sometimes, chemotherapy treatments are postponed to allow platelet counts to recover.
Fatigue
Fatigue
may be a consequence of the cancer or its treatment, and can last for
months to years after treatment. One physiological cause of fatigue is anemia, which can be caused by chemotherapy, surgery, radiotherapy, primary and metastatic disease or nutritional depletion. Anaerobic exercise has been found to be beneficial in reducing fatigue in people with solid tumors.
Nausea and vomiting
Nausea and vomiting
are two of the most feared cancer treatment-related side-effects for
people with cancer and their families. In 1983, Coates et al. found that
people receiving chemotherapy ranked nausea and vomiting as the first
and second most severe side-effects, respectively. Up to 20% of people
receiving highly emetogenic agents in this era postponed, or even
refused, potentially curative treatments.
Chemotherapy-induced nausea and vomiting (CINV) are common with many
treatments and some forms of cancer. Since the 1990s, several novel
classes of antiemetics
have been developed and commercialized, becoming a nearly universal
standard in chemotherapy regimens, and helping to successfully manage
these symptoms in many people. Effective mediation of these unpleasant
and sometimes-crippling symptoms results in increased quality of life
for the recipient and more efficient treatment cycles, due to less
stoppage of treatment due to better tolerance and better overall health.
Hair loss
Hair loss
(alopecia) can be caused by chemotherapy that kills rapidly dividing
cells; other medications may cause hair to thin. These are most often
temporary effects: hair usually starts to regrow a few weeks after the
last treatment, but sometimes with a change in colour, texture,
thickness or style. Sometimes hair has a tendency to curl after
regrowth, resulting in "chemo curls." Severe hair loss occurs most often
with drugs such as doxorubicin, daunorubicin, paclitaxel, docetaxel, cyclophosphamide, ifosfamide and etoposide. Permanent thinning or hair loss can result from some standard chemotherapy regimens.
Chemotherapy induced hair loss occurs by a non-androgenic mechanism, and can manifest as alopecia totalis, telogen effluvium, or less often alopecia areata.
It is usually associated with systemic treatment due to the high
mitotic rate of hair follicles, and more reversible than androgenic hair
loss, although permanent cases can occur. Chemotherapy induces hair loss in women more often than men.
Scalp cooling offers a means of preventing both permanent and temporary hair loss; however, concerns about this method have been raised.
Secondary neoplasm
Development of secondary neoplasia after successful chemotherapy or radiotherapy treatment can occur. The most common secondary neoplasm
is secondary acute myeloid leukemia, which develops primarily after
treatment with alkylating agents or topoisomerase inhibitors. Survivors of childhood cancer are more than 13 times as likely to get a secondary neoplasm during the 30 years after treatment than the general population. Not all of this increase can be attributed to chemotherapy.
Infertility
Some types of chemotherapy are gonadotoxic and may cause infertility.
Chemotherapies with high risk include procarbazine and other alkylating
drugs such as cyclophosphamide, ifosfamide, busulfan, melphalan,
chlorambucil, and chlormethine. Drugs with medium risk include doxorubicin and platinum analogs such as cisplatin and carboplatin. On the other hand, therapies with low risk of gonadotoxicity include plant derivatives such as vincristine and vinblastine, antibiotics such as bleomycin and dactinomycin, and antimetabolites such as methotrexate, mercaptopurine, and 5-fluorouracil.
Female infertility by chemotherapy appears to be secondary to premature ovarian failure by loss of primordial follicles.
This loss is not necessarily a direct effect of the chemotherapeutic
agents, but could be due to an increased rate of growth initiation to
replace damaged developing follicles.
People may choose between several methods of fertility preservation prior to chemotherapy, including cryopreservation of semen, ovarian tissue, oocytes, or embryos.
As more than half of cancer patients are elderly, this adverse effect
is only relevant for a minority of patients. A study in France between
1999 and 2011 came to the result that embryo freezing before
administration of gonadotoxic agents to females caused a delay of
treatment in 34% of cases, and a live birth in 27% of surviving cases
who wanted to become pregnant, with the follow-up time varying between 1
and 13 years.
Potential protective or attenuating agents include GnRH analogs, where several studies have shown a protective effect in vivo in humans, but some studies show no such effect. Sphingosine-1-phosphate (S1P) has shown similar effect, but its mechanism of inhibiting the sphingomyelin apoptotic pathway may also interfere with the apoptosis action of chemotherapy drugs.
In chemotherapy as a conditioning regimen
in hematopoietic stem cell transplantation, a study of people
conditioned with cyclophosphamide alone for severe aplastic anemia came
to the result that ovarian recovery occurred in all women younger than
26 years at time of transplantation, but only in five of 16 women older
than 26 years.
Teratogenicity
Chemotherapy is teratogenic during pregnancy, especially during the first trimester, to the extent that abortion usually is recommended if pregnancy in this period is found during chemotherapy.
Second- and third-trimester exposure does not usually increase the
teratogenic risk and adverse effects on cognitive development, but it
may increase the risk of various complications of pregnancy and fetal myelosuppression.
In males previously having undergone chemotherapy or
radiotherapy, there appears to be no increase in genetic defects or
congenital malformations in their children conceived after therapy. The use of assisted reproductive technologies and micromanipulation techniques might increase this risk.
In females previously having undergone chemotherapy, miscarriage and
congenital malformations are not increased in subsequent conceptions. However, when in vitro fertilization and embryo cryopreservationis
practised between or shortly after treatment, possible genetic risks to
the growing oocytes exist, and hence it has been recommended that the
babies be screened.
Peripheral neuropathy
Between 30 and 40 percent of people undergoing chemotherapy experience chemotherapy-induced peripheral neuropathy
(CIPN), a progressive, enduring, and often irreversible condition,
causing pain, tingling, numbness and sensitivity to cold, beginning in
the hands and feet and sometimes progressing to the arms and legs. Chemotherapy drugs associated with CIPN include thalidomide, epothilones, vinca alkaloids, taxanes, proteasome inhibitors, and the platinum-based drugs.
Whether CIPN arises, and to what degree, is determined by the choice of
drug, duration of use, the total amount consumed and whether the person
already has peripheral neuropathy. Though the symptoms are mainly sensory, in some cases motor nerves and the autonomic nervous system are affected.
CIPN often follows the first chemotherapy dose and increases in
severity as treatment continues, but this progression usually levels off
at completion of treatment. The platinum-based drugs are the exception;
with these drugs, sensation may continue to deteriorate for several
months after the end of treatment. Some CIPN appears to be irreversible. Pain can often be managed with drug or other treatment but the numbness is usually resistant to treatment.
Cognitive impairment
Some
people receiving chemotherapy report fatigue or non-specific
neurocognitive problems, such as an inability to concentrate; this is
sometimes called post-chemotherapy cognitive impairment, referred to as "chemo brain" in popular and social media.
Tumor lysis syndrome
In particularly large tumors and cancers with high white cell counts, such as lymphomas, teratomas, and some leukemias, some people develop tumor lysis syndrome.
The rapid breakdown of cancer cells causes the release of chemicals
from the inside of the cells. Following this, high levels of uric acid, potassium and phosphate
are found in the blood. High levels of phosphate induce secondary
hypoparathyroidism, resulting in low levels of calcium in the blood.
This causes kidney damage and the high levels of potassium can cause cardiac arrhythmia.
Although prophylaxis is available and is often initiated in people with
large tumors, this is a dangerous side-effect that can lead to death if
left untreated.
Organ damage
Cardiotoxicity (heart damage) is especially prominent with the use of anthracycline drugs (doxorubicin, epirubicin, idarubicin, and liposomal doxorubicin). The cause of this is most likely due to the production of free radicals in the cell and subsequent DNA damage. Other chemotherapeutic agents that cause cardiotoxicity, but at a lower incidence, are cyclophosphamide, docetaxel and clofarabine.
Hepatotoxicity
(liver damage) can be caused by many cytotoxic drugs. The
susceptibility of an individual to liver damage can be altered by other
factors such as the cancer itself, viral hepatitis, immunosuppression and nutritional deficiency. The liver damage can consist of damage to liver cells, hepatic sinusoidal syndrome (obstruction of the veins in the liver), cholestasis (where bile does not flow from the liver to the intestine) and liver fibrosis.
Nephrotoxicity (kidney damage) can be caused by tumor lysis syndrome
and also due direct effects of drug clearance by the kidneys. Different
drugs will affect different parts of the kidney and the toxicity may be
asymptomatic (only seen on blood or urine tests) or may cause acute renal failure.
Ototoxicity (damage to the inner ear) is a common side effect of platinum based drugs that can produce symptoms such as dizziness and vertigo.
Other side-effects
Less common side-effects include red skin (erythema), dry skin, damaged fingernails, a dry mouth (xerostomia), water retention, and sexual impotence. Some medications can trigger allergic or pseudoallergic reactions.
Specific chemotherapeutic agents are associated with organ-specific toxicities, including cardiovascular disease (e.g., doxorubicin), interstitial lung disease (e.g., bleomycin) and occasionally secondary neoplasm (e.g., MOPP therapy for Hodgkin's disease).
Hand-foot syndrome is another side effect to cytotoxic chemotherapy.
Limitations
Chemotherapy
does not always work, and even when it is useful, it may not completely
destroy the cancer. People frequently fail to understand its
limitations. In one study of people who had been newly diagnosed with
incurable, stage 4 cancer,
more than two-thirds of people with lung cancer and more than
four-fifths of people with colorectal cancer still believed that
chemotherapy was likely to cure their cancer.
The blood–brain barrier poses an obstacle to delivery of chemotherapy to the brain.
This is because the brain has an extensive system in place to protect
it from harmful chemicals. Drug transporters can pump out drugs from the
brain and brain's blood vessel cells into the cerebrospinal fluid
and blood circulation. These transporters pump out most chemotherapy
drugs, which reduces their efficacy for treatment of brain tumors. Only
small lipophilic alkylating agents such as lomustine or temozolomide are able to cross this blood–brain barrier.
Blood vessels
in tumors are very different from those seen in normal tissues. As a
tumor grows, tumor cells furthest away from the blood vessels become low
in oxygen (hypoxic).
To counteract this they then signal for new blood vessels to grow. The
newly formed tumor vasculature is poorly formed and does not deliver an
adequate blood supply to all areas of the tumor. This leads to issues
with drug delivery because many drugs will be delivered to the tumor by
the circulatory system.
Resistance
Resistance
is a major cause of treatment failure in chemotherapeutic drugs. There
are a few possible causes of resistance in cancer, one of which is the
presence of small pumps on the surface of cancer cells that actively
move chemotherapy from inside the cell to the outside. Cancer cells
produce high amounts of these pumps, known as p-glycoprotein, in order to protect themselves from chemotherapeutics. Research on p-glycoprotein and other such chemotherapy efflux pumps is currently ongoing. Medications to inhibit the function of p-glycoprotein
are undergoing investigation, but due to toxicities and interactions
with anti-cancer drugs their development has been difficult. Another mechanism of resistance is gene amplification,
a process in which multiple copies of a gene are produced by cancer
cells. This overcomes the effect of drugs that reduce the expression of
genes involved in replication. With more copies of the gene, the drug
can not prevent all expression of the gene and therefore the cell can
restore its proliferative ability. Cancer cells can also cause defects
in the cellular pathways of apoptosis
(programmed cell death). As most chemotherapy drugs kill cancer cells
in this manner, defective apoptosis allows survival of these cells,
making them resistant. Many chemotherapy drugs also cause DNA damage,
which can be repaired by enzymes in the cell that carry out DNA repair.
Upregulation of these genes can overcome the DNA damage and prevent the
induction of apoptosis. Mutations in genes that produce drug target
proteins, such as tubulin, can occur which prevent the drugs from binding to the protein, leading to resistance to these types of drugs.
Drugs used in chemotherapy can induce cell stress, which can kill a
cancer cell; however, under certain conditions, cells stress can induce
changes in gene expression that enables resistance to several types of
drugs.
Cytotoxics and targeted therapies
Targeted therapies
are a relatively new class of cancer drugs that can overcome many of
the issues seen with the use of cytotoxics. They are divided into two
groups: small molecule and antibodies. The massive toxicity seen with
the use of cytotoxics is due to the lack of cell specificity of the
drugs. They will kill any rapidly dividing cell, tumor or normal.
Targeted therapies are designed to affect cellular proteins or processes
that are utilised by the cancer cells. This allows a high dose to
cancer tissues with a relatively low dose to other tissues. Although the
side effects
are often less severe than that seen of cytotoxic chemotherapeutics,
life-threatening effects can occur. Initially, the targeted therapeutics
were supposed to be solely selective for one protein. Now it is clear
that there is often a range of protein targets that the drug can bind.
An example target for targeted therapy is the BCR-ABL1 protein produced
from the Philadelphia chromosome, a genetic lesion found commonly in chronic myelogenous leukemia and in some patients with acute lymphoblastic leukemia. This fusion protein has enzyme activity that can be inhibited by imatinib, a small molecule drug.
Mechanism of action
The
four phases of the cell cycle. G1 – the initial growth phase. S – the
phase in which DNA is synthesised. G2 – the second growth phase in
preparation for cell division. M – mitosis; where the cell divides to
produce two daughter cells that continue the cell cycle.
Cancer is the uncontrolled growth of cells coupled with malignant behaviour: invasion and metastasis (among other features). It is caused by the interaction between genetic susceptibility and environmental factors. These factors lead to accumulations of genetic mutations in oncogenes (genes that control the growth rate of cells) and tumor suppressor genes (genes that help to prevent cancer), which gives cancer cells their malignant characteristics, such as uncontrolled growth.
In the broad sense, most chemotherapeutic drugs work by impairing mitosis (cell division), effectively targeting fast-dividing cells. As these drugs cause damage to cells, they are termed cytotoxic.
They prevent mitosis by various mechanisms including damaging DNA and
inhibition of the cellular machinery involved in cell division. One theory as to why these drugs kill cancer cells is that they induce a programmed form of cell death known as apoptosis.
As chemotherapy affects cell division, tumors with high growth rates (such as acute myelogenous leukemia and the aggressive lymphomas, including Hodgkin's disease) are more sensitive to chemotherapy, as a larger proportion of the targeted cells are undergoing cell division at any time. Malignancies with slower growth rates, such as indolent lymphomas, tend to respond to chemotherapy much more modestly. Heterogeneic tumours may also display varying sensitivities to chemotherapy agents, depending on the subclonal populations within the tumor.
Cells from the immune system also make crucial contributions to the antitumor effects of chemotherapy. For example, the chemotherapeutic drugs oxaliplatin and cyclophosphamide can cause tumor cells to die in a way that is detectable by the immune system (called immunogenic cell death), which mobilizes immune cells with antitumor functions. Chemotherapeutic drugs that cause cancer immunogenic tumor cell death can make unresponsive tumors sensitive to immune checkpoint therapy.
Other uses
Some chemotherapy drugs are used in diseases other than cancer, such as in autoimmune disorders, and noncancerous plasma cell dyscrasia. In some cases they are often used at lower doses, which means that the side effects are minimized, while in other cases doses similar to ones used to treat cancer are used. Methotrexate is used in the treatment of rheumatoid arthritis (RA), psoriasis, ankylosing spondylitis and multiple sclerosis. The anti-inflammatory response seen in RA is thought to be due to increases in adenosine, which causes immunosuppression; effects on immuno-regulatory cyclooxygenase-2 enzyme pathways; reduction in pro-inflammatory cytokines; and anti-proliferative properties.
Although methotrexate is used to treat both multiple sclerosis and
ankylosing spondylitis, its efficacy in these diseases is still
uncertain. Cyclophosphamide is sometimes used to treat lupus nephritis, a common symptom of systemic lupus erythematosus. Dexamethasone along with either bortezomib or melphalan is commonly used as a treatment for AL amyloidosis. Recently, bortezomid in combination with cyclophosphamide and dexamethasone has also shown promise as a treatment for AL amyloidosis. Other drugs used to treat myeloma such as lenalidomide have shown promise in treating AL amyloidosis.
Chemotherapy drugs are also used in conditioning regimens prior to bone marow transplant (hematopoietic stem cell transplant).
Conditioning regimens are used to suppress the recipient's immune
system in order to allow a transplant to engraft. Cyclophosphamide is a
common cytotoxic drug used in this manner, and is often used in
conjunction with total body irradiation.
Chemotherapeutic drugs may be used at high doses to permanently remove
the recipient's bone marrow cells (myeloablative conditioning) or at
lower doses that will prevent permanent bone marrow loss
(non-myeloablative and reduced intensity conditioning).
When used in non-cancer setting, the treatment is still called
"chemotherapy", and is often done in the same treatment centers used for
people with cancer.
Occupational exposure and safe handling
In the 1970s, antineoplastic (chemotherapy) drugs were identified as hazardous, and the American Society of Health-System Pharmacists (ASHP) has since then introduced the concept of hazardous drugs
after publishing a recommendation in 1983 regarding handling hazardous
drugs. The adaptation of federal regulations came when the U.S. Occupational Safety and Health Administration (OSHA) first released its guidelines in 1986 and then updated them in 1996, 1999, and, most recently, 2006.
The National Institute for Occupational Safety and Health
(NIOSH) has been conducting an assessment in the workplace since then
regarding these drugs. Occupational exposure to antineoplastic drugs has
been linked to multiple health effects, including infertility and
possible carcinogenic effects. A few cases have been reported by the
NIOSH alert report, such as one in which a female pharmacist was
diagnosed with papillary transitional cell carcinoma. Twelve years
before the pharmacist was diagnosed with the condition, she had worked
for 20 months in a hospital where she was responsible for preparing
multiple antineoplastic drugs.
The pharmacist didn't have any other risk factor for cancer, and
therefore, her cancer was attributed to the exposure to the
antineoplastic drugs, although a cause-and-effect relationship has not
been established in the literature. Another case happened when a
malfunction in biosafety cabinetry is believed to have exposed nursing
personnel to antineoplastic drugs. Investigations revealed evidence of
genotoxic biomarkers two and nine months after that exposure.
Routes of exposure
Antineoplastic drugs are usually given through intravenous, intramuscular. intrathecal, or subcutaneous
administration. In most cases, before the medication is administered to
the patient, it needs to be prepared and handled by several workers.
Any worker who is involved in handling, preparing, or administering the
drugs, or with cleaning objects that have come into contact with
antineoplastic drugs, is potentially exposed to hazardous drugs. Health
care workers are exposed to drugs in different circumstances, such as
when pharmacists and pharmacy technicians prepare and handle
antineoplastic drugs and when nurses and physicians administer the drugs
to patients. Additionally, those who are responsible for disposing
antineoplastic drugs in health care facilities are also at risk of
exposure.
Dermal exposure is thought to be the main route of exposure due
to the fact that significant amounts of the antineoplastic agents have
been found in the gloves worn by healthcare workers who prepare, handle,
and administer the agents. Another noteworthy route of exposure is
inhalation of the drugs' vapors. Multiple studies have investigated
inhalation as a route of exposure, and although air sampling has not
shown any dangerous levels, it is still a potential route of exposure.
Ingestion by hand to mouth is a route of exposure that is less likely
compared to others because of the enforced hygienic standard in the
health institutions. However, it is still a potential route, especially
in the workplace, outside of a health institute. One can also be exposed
to these hazardous drugs through injection by needle sticks.
Research conducted in this area has established that occupational
exposure occurs by examining evidence in multiple urine samples from
health care workers.
Hazards
Hazardous
drugs expose health care workers to serious health risks. Many studies
show that antineoplastic drugs could have many side effects on the
reproductive system, such as fetal loss, congenital malformation, and
infertility. Health care workers who are exposed to antineoplastic drugs
on many occasions have adverse reproductive outcomes such as
spontaneous abortions, stillbirths, and congenital malformations.
Moreover, studies have shown that exposure to these drugs leads to
menstrual cycle irregularities. Antineoplastic drugs may also increase
the risk of learning disabilities among children of health care workers
who are exposed to these hazardous substances.
Moreover, these drugs have carcinogenic
effects. In the past five decades, multiple studies have shown the
carcinogenic effects of exposure to antineoplastic drugs. Similarly,
there have been research studies that linked alkylating agents with
humans developing leukemias. Studies have reported elevated risk of
breast cancer, nonmelanoma skin cancer, and cancer of the rectum among
nurses who are exposed to these drugs. Other investigations revealed
that there is a potential genotoxic effect from anti-neoplastic drugs to workers in health care settings.
Safe handling in health care settings
As of 2018, there were no occupational exposure limits set for antineoplastic drugs, i.e., OSHA or the American Conference of Governmental Industrial Hygienists (ACGIH) have not set workplace safety guidelines.
Preparation
NIOSH recommends using a ventilated cabinet
that is designed to decrease worker exposure. Additionally, it
recommends training of all staff, the use of cabinets, implementing an
initial evaluation of the technique of the safety program, and wearing
protective gloves and gowns when opening drug packaging, handling vials,
or labeling. When wearing personal protective equipment,
one should inspect gloves for physical defects before use and always
wear double gloves and protective gowns. Health care workers are also
required to wash their hands with water and soap before and after
working with antineoplastic drugs, change gloves every 30 minutes or
whenever punctured, and discard them immediately in a chemotherapy waste
container.
The gowns used should be disposable gowns made of
polyethylene-coated polypropylene. When wearing gowns, individuals
should make sure that the gowns are closed and have long sleeves. When
preparation is done, the final product should be completely sealed in a
plastic bag.
The health care worker should also wipe all waste containers
inside the ventilated cabinet before removing them from the cabinet.
Finally, workers should remove all protective wear and put them in a bag
for their disposal inside the ventilated cabinet.
Administration
Drugs
should only be administered using protective medical devices such as
needle lists and closed systems and techniques such as priming of IV
tubing by pharmacy personnel inside a ventilated cabinet. Workers should
always wear personal protective equipment such as double gloves,
goggles, and protective gowns when opening the outer bag and assembling
the delivery system to deliver the drug to the patient, and when
disposing of all material used in the administration of the drugs.
Hospital workers should never remove tubing from an IV bag that
contains an antineoplastic drug, and when disconnecting the tubing in
the system, they should make sure the tubing has been thoroughly
flushed. After removing the IV bag, the workers should place it together
with other disposable items directly in the yellow chemotherapy waste
container with the lid closed. Protective equipment should be removed
and put into a disposable chemotherapy waste container. After this has
been done, one should double bag the chemotherapy waste before or after
removing one's inner gloves. Moreover, one must always wash one's hands
with soap and water before leaving the drug administration site.
Employee training
All
employees whose jobs in health care facilities expose them to hazardous
drugs must receive training. Training should include shipping and
receiving personnel, housekeepers, pharmacists, assistants, and all
individuals involved in the transportation and storage of antineoplastic
drugs. These individuals should receive information and training to
inform them of the hazards of the drugs present in their areas of work.
They should be informed and trained on operations and procedures in
their work areas where they can encounter hazards, different methods
used to detect the presence of hazardous drugs and how the hazards are
released, and the physical and health hazards of the drugs, including
their reproductive and carcinogenic hazard potential. Additionally, they
should be informed and trained on the measures they should take to
avoid and protect themselves from these hazards. This information ought
to be provided when health care workers come into contact with the
drugs, that is, perform the initial assignment in a work area with
hazardous drugs. Moreover, training should also be provided when new
hazards emerge as well as when new drugs, procedures, or equipment are
introduced.
Housekeeping and waste disposal
When
performing cleaning and decontaminating the work area where
antineoplastic drugs are used, one should make sure that there is
sufficient ventilation to prevent the buildup of airborne drug
concentrations. When cleaning the work surface, hospital workers should
use deactivation and cleaning agents before and after each activity as
well as at the end of their shifts. Cleaning should always be done using
double protective gloves and disposable gowns. After employees finish
up cleaning, they should dispose of the items used in the activity in a
yellow chemotherapy waste container while still wearing protective
gloves. After removing the gloves, they should thoroughly wash their
hands with soap and water. Anything that comes into contact or has a
trace of the antineoplastic drugs, such as needles, empty vials,
syringes, gowns, and gloves, should be put in the chemotherapy waste
container.
Spill control
A
written policy needs to be in place in case of a spill of
antineoplastic products. The policy should address the possibility of
various sizes of spills as well as the procedure and personal protective
equipment required for each size. A trained worker should handle a
large spill and always dispose of all cleanup materials in the chemical
waste container according to EPA regulations, not in a yellow
chemotherapy waste container.
Occupational monitoring
A medical surveillance
program must be established. In case of exposure, occupational health
professionals need to ask for a detailed history and do a thorough
physical exam. They should test the urine of the potentially exposed
worker by doing a urine dipstick or microscopic examination, mainly looking for blood, as several antineoplastic drugs are known to cause bladder damage.
Urinary mutagenicity is a marker of exposure to antineoplastic
drugs that was first used by Falck and colleagues in 1979 and uses
bacterial mutagenicity assays. Apart from being nonspecific, the test
can be influenced by extraneous factors such as dietary intake and
smoking and is, therefore, used sparingly. However, the test played a
significant role in changing the use of horizontal flow cabinets to
vertical flow biological safety cabinets during the preparation of
antineoplastic drugs because the former exposed health care workers to
high levels of drugs. This changed the handling of drugs and effectively
reduced workers’ exposure to antineoplastic drugs.
Biomarkers of exposure to antineoplastic drugs commonly include urinary platinum, methotrexate, urinary cyclophosphamide and ifosfamide, and urinary metabolite of 5-fluorouracil.
In addition to this, there are other drugs used to measure the drugs
directly in the urine, although they are rarely used. A measurement of
these drugs directly in one's urine is a sign of high exposure levels
and that an uptake of the drugs is happening either through inhalation
or dermally.
Available agents
There is an extensive list of antineoplastic agents. Several classification schemes have been used to subdivide the medicines used for cancer into several different types.
History
Sidney Farber is regarded as the father of modern chemotherapy.
The first use of small-molecule drugs
to treat cancer was in the early 20th century, although the specific
chemicals first used were not originally intended for that purpose. Mustard gas was used as a chemical warfare agent during World War I and was discovered to be a potent suppressor of hematopoiesis (blood production). A similar family of compounds known as nitrogen mustards were studied further during World War II at the Yale School of Medicine. It was reasoned that an agent that damaged the rapidly growing white blood cells might have a similar effect on cancer. Therefore, in December 1942, several people with advanced lymphomas (cancers of the lymphatic system and lymph nodes) were given the drug by vein, rather than by breathing the irritating gas. Their improvement, although temporary, was remarkable. Concurrently, during a military operation in World War II, following a German air raid
on the Italian harbour of Bari, several hundred people were
accidentally exposed to mustard gas, which had been transported there by
the Allied forces
to prepare for possible retaliation in the event of German use of
chemical warfare. The survivors were later found to have very low white
blood cell counts.
After WWII was over and the reports declassified, the experiences
converged and led researchers to look for other substances that might
have similar effects against cancer. The first chemotherapy drug to be
developed from this line of research was mustine.
Since then, many other drugs have been developed to treat cancer, and
drug development has exploded into a multibillion-dollar industry,
although the principles and limitations of chemotherapy discovered by
the early researchers still apply.
The term chemotherapy
The word chemotherapy
without a modifier usually refers to cancer treatment, but its
historical meaning was broader. The term was coined in the early 1900s
by Paul Ehrlich as meaning any use of chemicals to treat any disease (chemo- + -therapy), such as the use of antibiotics (antibacterial chemotherapy). Ehrlich was not optimistic that effective chemotherapy drugs would be found for the treatment of cancer. The first modern chemotherapeutic agent was arsphenamine, an arsenic compound discovered in 1907 and used to treat syphilis. This was later followed by sulfonamides (sulfa drugs) and penicillin. In today's usage, the sense "any treatment of disease with drugs" is often expressed with the word pharmacotherapy.
Sales
The top 10 best-selling (in terms of revenue) cancer drugs of 2013:
| No. | 2013 Global Sales | INN | Trade names | Marketing authorization holder | Indications |
|---|---|---|---|---|---|
| 1 | $7.78 billion | Rituximab | Rituxan, MabThera | Roche, Pharmstandard | non-Hodgkin's lymphoma, CLL |
| 2 | $6.75 billion | Bevacizumab | Avastin | Roche | Colorectal, lung, ovarian and brain cancer |
| 3 | $6.56 billion | Trastuzumab | Herceptin | Roche | Breast, esophagus and stomach cancer |
| 4 | $4.69 billion | Imatinib | Gleevec | Novartis | Leukemia, GI cancer |
| 5 | $1.09 billion | Lenalidomide | Revlimid | Celgene, Pharmstandard | Multiple myeloma, mantle cell lymphoma |
| 6 | $2.7 billion | Pemetrexed | Alimta | Eli Lilly | Lung cancer |
| 7 | $2.6 billion | Bortezomib | Velcade | Johnson & Johnson, Takeda, Pharmstandard | Multiple myeloma |
| 8 | $1.87 billion | Cetuximab | Erbitux | Merck KGaA, Bristol-Myers Squibb | Colon and head and neck cancer |
| 9 | $1.73 billion | Leuprorelin | Lupron, Eligard | AbbVie and Takeda; Sanofi and Astellas Pharma | Prostate and ovarian cancer |
| 10 | $1.7 billion | Abiraterone | Zytiga | Johnson & Johnson | Prostate cancer |
Research
Scanning electron micrograph of mesoporous silica; a type of nanoparticle used in the delivery of chemotherapeutic drugs.
Targeted therapies
Specially
targeted delivery vehicles aim to increase effective levels of
chemotherapy for tumor cells while reducing effective levels for other
cells. This should result in an increased tumor kill or reduced toxicity
or both.
Antibody-drug conjugates
Antibody-drug conjugates (ADCs) comprise an antibody,
drug and a linker between them. The antibody will be targeted at a
preferentially expressed protein in the tumour cells (known as a tumor antigen) or on cells that the tumor can utilise, such as blood vessel endothelial cells.
They bind to the tumor antigen and are internalised, where the linker
releases the drug into the cell. These specially targeted delivery
vehicles vary in their stability, selectivity, and choice of target,
but, in essence, they all aim to increase the maximum effective dose
that can be delivered to the tumor cells.
Reduced systemic toxicity means that they can also be used in people
who are sicker, and that they can carry new chemotherapeutic agents that
would have been far too toxic to deliver via traditional systemic
approaches.
The first approved drug of this type was gemtuzumab ozogamicin (Mylotarg), released by Wyeth (now Pfizer). The drug was approved to treat acute myeloid leukemia, but has now been withdrawn from the market because the drug did not meet efficacy targets in further clinical trials. Two other drugs, trastuzumab emtansine and brentuximab vedotin, are both in late clinical trials, and the latter has been granted accelerated approval for the treatment of refractory Hodgkin's lymphoma and systemic anaplastic large cell lymphoma.
Nanoparticles
Nanoparticles are 1–1000 nanometer (nm) sized particles that can promote tumor selectivity and aid in delivering low-solubility
drugs. Nanoparticles can be targeted passively or actively. Passive
targeting exploits the difference between tumor blood vessels and normal
blood vessels. Blood vessels in tumors are "leaky" because they have
gaps from 200–2000 nm, which allow nanoparticles to escape into the
tumor. Active targeting uses biological molecules (antibodies, proteins, DNA and receptor ligands) to preferentially target the nanoparticles to the tumor cells. There are many types of nanoparticle delivery systems, such as silica, polymers, liposomes and magnetic particles.
Nanoparticles made of magnetic material can also be used to concentrate
agents at tumor sites using an externally applied magnetic field. They have emerged as a useful vehicle in magnetic drug delivery for poorly soluble agents such as paclitaxel.
Electrochemotherapy
Electrochemotherapy is the combined treatment in which injection of a
chemotherapeutic drug is followed by application of high-voltage
electric pulses locally to the tumor. The treatment enables the
chemotherapeutic drugs, which otherwise cannot or hardly go through the
membrane of cells (such as bleomycin and cisplatin), to enter the cancer
cells. Hence, greater effectiveness of antitumor treatment is achieved.
Clinical electrochemotherapy has been successfully used for
treatment of cutaneous and subcutaneous tumors irrespective of their
histological origin.
The method has been reported as safe, simple and highly effective in
all reports on clinical use of electrochemotherapy. According to the
ESOPE project (European Standard Operating Procedures of
Electrochemotherapy), the Standard Operating Procedures (SOP) for
electrochemotherapy were prepared, based on the experience of the
leading European cancer centres on electrochemotherapy.
Recently, new electrochemotherapy modalities have been developed for
treatment of internal tumors using surgical procedures, endoscopic
routes or percutaneous approaches to gain access to the treatment area.
Hyperthermia therapy
Hyperthermia therapy
is heat treatment for cancer that can be a powerful tool when used in
combination with chemotherapy (thermochemotherapy) or radiation for the
control of a variety of cancers. The heat can be applied locally to the
tumor site, which will dilate blood vessels to the tumor, allowing more
chemotherapeutic medication to enter the tumor. Additionally, the
tumor cell membrane will become more porous, further allowing more of
the chemotherapeutic medicine to enter the tumor cell.
Hyperthermia has also been shown to help prevent or reverse
"chemo-resistance." Chemotherapy resistance sometimes develops over
time as the tumors adapt and can overcome the toxicity of the chemo
medication. "Overcoming chemoresistance has been extensively studied
within the past, especially using CDDP-resistant cells. In regard to the
potential benefit that drug-resistant cells can be recruited for
effective therapy by combining chemotherapy with hyperthermia, it was
important to show that chemoresistance against several anticancer drugs
(e.g. mitomycin C, anthracyclines, BCNU, melphalan) including CDDP could
be reversed at least partially by the addition of heat.
Other animals
Chemotherapy is used in veterinary medicine similar to how it is used in human medicine.