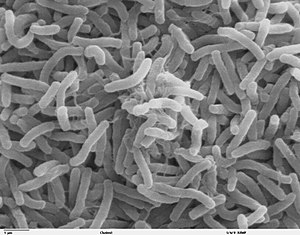
Scanning electron microscope image of Vibrio cholerae. This is the bacterium that causes cholera.
The germ theory of disease is the currently accepted scientific theory for many diseases. It states that microorganisms known as pathogens
or "germs" can lead to disease. These small organisms, too small to see
without magnification, invade humans, other animals, and other living
hosts. Their growth and reproduction within their hosts can cause
disease. "Germ" may refer to not just a bacterium but to any type of microorganism or even non-living pathogen that can cause disease, such as protists, fungi, viruses, prions, or viroids. Diseases caused by pathogens are called infectious diseases.
Even when a pathogen is the principal cause of a disease, environmental
and hereditary factors often influence the severity of the disease, and
whether a potential host individual becomes infected when exposed to
the pathogen.
The germ theory was proposed by Girolamo Fracastoro in 1546, and expanded upon by Marcus von Plenciz in 1762. Such views were held in disdain, however, and Galen's miasma theory
remained dominant among scientists and doctors. The nature of this
doctrine prevented them from understanding how diseases actually
progressed, with predictable consequences. By the early nineteenth
century, smallpox vaccination
was commonplace in Europe, though doctors were unaware of how it worked
or how to extend the principle to other diseases. Similar treatments
had been prevalent in India from just before AD 1000. A transitional period began in the late 1850s with the work of Louis Pasteur. This work was later extended by Robert Koch
in the 1880s. Viruses were discovered in the 1890s. By the end of the
1880s, the miasma theory was struggling to compete with the germ theory
of disease. Eventually, a "golden era" of bacteriology ensued, during which the theory quickly led to the identification of the actual organisms that cause many diseases.
Miasma theory
A representation by Robert Seymour of the cholera epidemic depicts the spread of the disease in the form of poisonous air.
The miasma theory was the predominant theory of disease transmission
before the germ theory took hold towards the end of the 19th century,
and it is no longer accepted as a scientific theory of disease. It held
that diseases such as cholera, chlamydia infection, or the Black Death were caused by a miasma (μίασμα, Ancient Greek: "pollution"), a noxious form of "bad air" emanating from rotting organic matter.
Miasma was considered to be a poisonous vapor or mist filled with
particles from decomposed matter (miasmata) that was identifiable by its
foul smell. The theory posited that diseases were the product of
environmental factors such as contaminated water, foul air, and poor
hygienic conditions. Such infections, according to the theory, were not
passed between individuals but would affect those within a locale that
gave rise to such vapors.
Development
Pre-19th century
In Antiquity, the Greek historian Thucydides (c. 460 – c. 400 BC) was the first person to state, in his account of the plague of Athens, that diseases could spread from an infected person to others.
One theory of the spread of contagious diseases that were not spread
by direct contact was that they were spread by "seeds" (Latin: semina) that were present in the air. In his poem, De rerum natura (On the Nature of Things, c. 56 BC), the Roman poet Lucretius
(c. 99 BC – c. 55 BC) stated that the world contained various "seeds",
some of which could sicken a person if they were inhaled or if they
contaminated his food. The Roman statesman Marcus Terentius Varro (116–27 BC) wrote, in his Rerum rusticarum libri III
(Three Books on Agriculture, 36 BC): "Precautions must also be taken in
the neighborhood of swamps […] because there are bred certain minute
creatures which cannot be seen by the eyes, which float in the air and
enter the body through the mouth and nose and there cause serious
diseases." The Greek physician Galen (AD 129 – c. 200/c. 216) speculated in his On Initial Causes (c. AD 175) that some patients might have "seeds of fever". In his On the Different Types of Fever (c. AD 175), Galen speculated that plagues were spread by "certain seeds of plague", which were present in the air. And in his Epidemics
(c. AD 176–178), Galen explained that patients might relapse during
recovery from a fever because some "seed of the disease" lurked in their
bodies, which would cause a recurrence of the disease if the patients
didn't follow a physician's therapeutic regimen.
During the Middle Ages, Isidore of Seville (c. 560–636) mentioned "plague-bearing seeds" (pestifera semina) in his On the Nature of Things (c. AD 613). Later in 1345, Tommaso del Garbo (c. 1305–1370) of Bologna, Italy mentioned Galen's "seeds of plague" in his work Commentaria non parum utilia in libros Galeni (Helpful commentaries on the books of Galen).
The Italian scholar and physician Girolamo Fracastoro proposed in 1546 in his book De Contagione et Contagiosis Morbis that epidemic diseases are caused by transferable seed-like entities (seminaria morbi)
that transmit infection by direct or indirect contact, or even without
contact over long distances. The diseases were categorised based on how
they were transmitted, and how long they could lie dormant.
Italian physician Francesco Redi provided early evidence against spontaneous generation. He devised an experiment in 1668 in which he used three jars. He placed a meatloaf
and egg in each of the three jars. He had one of the jars open, another
one tightly sealed, and the last one covered with gauze. After a few
days, he observed that the meatloaf in the open jar was covered by
maggots, and the jar covered with gauze had maggots on the surface of
the gauze. However, the tightly sealed jar had no maggots inside or
outside it. He also noticed that the maggots were found only on surfaces
that were accessible by flies. From this he concluded that spontaneous
generation is not a plausible theory.
Microorganisms are said to have been first directly observed in the 1670s by Anton van Leeuwenhoek, an early pioneer in microbiology. Yet Athanasius Kircher
may have done so prior. When Rome was struck by the bubonic plague in
1656, Kircher spent days on end caring for the sick. Searching for a
cure, Kircher observed microorganisms under the microscope and invented
the germ theory of disease, which he outlined in his Scrutinium pestis physico-medicum (Rome 1658).[16] Building on Leeuwenhoek's work, physician Nicolas Andry argued in 1700 that microorganisms he called "worms" were responsible for smallpox and other diseases.
In 1720, Richard Bradley
theorised that the plague and 'all pestilential distempers' were caused
by 'poisonous insects', living creatures viewable only with the help of
microscopes.
In 1762, the Austrian physician Marcus Antonius von Plenciz (1705–1786) published a book titled Opera medico-physica. It outlined a theory of contagion stating that specific animalcules
in the soil and the air were responsible for causing specific diseases.
Von Plenciz noted the distinction between diseases which are both
epidemic and contagious (like measles and dysentry), and diseases which
are contagious but not epidemic (like rabies and leprosy).
The book cites Anton van Leeuwenhoek to show how ubiquitous such
animalcules are, and was unique for describing the presence of germs in
ulcerating wounds. Ultimately, the theory espoused by von Plenciz was
not accepted by the scientific community.
Agostino Bassi
The Italian Agostino Bassi
was the first person to prove that a disease was caused by a
microorganism when he conducted a series of experiments between 1808 and
1813, demonstrating that a "vegetable parasite" caused a disease in
silkworms known as calcinaccio—this disease was devastating the
French silk industry at the time. The "vegetable parasite" is now known
to be a fungus pathogenic to insects called Beauveria bassiana (named after Bassi).
Ignaz Semmelweis
Ignaz Semmelweis, a Hungarian obstetrician working at the Vienna General Hospital (Allgemeines Krankenhaus) in 1847, noticed the dramatically high maternal mortality from puerperal fever following births assisted by doctors and medical students. However, those attended by midwives
were relatively safe. Investigating further, Semmelweis made the
connection between puerperal fever and examinations of delivering women
by doctors, and further realized that these physicians had usually come
directly from autopsies. Asserting that puerperal fever was a contagious
disease and that matter from autopsies were implicated in its
development, Semmelweis made doctors wash their hands with chlorinated
lime water before examining pregnant women. He then documented a sudden
reduction in the mortality rate from 18% to 2.2% over a period of a
year. Despite this evidence, he and his theories were rejected by most of the contemporary medical establishment.
Gideon Mantell
Gideon Mantell, the Sussex doctor more famous for discovering dinosaur fossils, spent time with his microscope, and speculated in his Thoughts On Animalcules
(1850) that perhaps "many of the most serious maladies which afflict
humanity, are produced by peculiar states of invisible animalcular
life".
John Snow
Original map by John Snow showing the clusters of cholera cases in the London epidemic of 1854
John Snow was a skeptic of the then-dominant miasma theory.
Even though the germ theory of disease pioneered by Girolamo Fracastoro
had not yet achieved full development or widespread currency, Snow
demonstrated a clear understanding of germ theory in his writings. He
first published his theory in an 1849 essay On the Mode of Communication of Cholera, in which he correctly suggested that the fecal-oral route
was the mode of communication, and that the disease replicated itself
in the lower intestines. He even proposed in his 1855 edition of the
work, that the structure of cholera was that of a cell.
Having rejected effluvia and the poisoning of the blood in the first instance, and being led to the conclusion that the disease is something that acts directly on the alimentary canal, the excretions of the sick at once suggest themselves as containing some material which being accidentally swallowed might attach itself to the mucous membrane of the small intestines, and there multiply itself by appropriation of surrounding matter, in virtue of molecular changes going on within it, or capable of going on, as soon as it is placed in congenial circumstances.
— John Snow (1849)
For the morbid matter of cholera having the property of reproducing its own kind, must necessarily have some sort of structure, most likely that of a cell. It is no objection to this view that the structure of the cholera poison cannot be recognized by the microscope, for the matter of smallpox and of chancre can only be recognized by their effects, and not by their physical properties.
— John Snow (1855)
Snow's 1849 recommendation that water be "filtered and boiled before
it is used" is one of the first practical applications of germ theory in
the area of public health and is the antecedent to the modern boil-water advisory.
In 1855 he published a second edition of his article, documenting
his more elaborate investigation of the effect of the water supply in
the Soho, London epidemic of 1854.
By talking to local residents, he identified the source of the outbreak as the public water pump on Broad Street (now Broadwick Street). Although Snow's chemical and microscope examination of a water sample from the Broad Street pump
did not conclusively prove its danger, his studies of the pattern of
the disease were convincing enough to persuade the local council to
disable the well pump by removing its handle. This action has been
commonly credited as ending the outbreak, but Snow observed that the
epidemic may have already been in rapid decline.
Snow later used a dot map
to illustrate the cluster of cholera cases around the pump. He also
used statistics to illustrate the connection between the quality of the
water source and cholera cases. He showed that the Southwark and Vauxhall Waterworks Company was taking water from sewage-polluted sections of the Thames
and delivering the water to homes, leading to an increased incidence of
cholera. Snow's study was a major event in the history of public health
and geography. It is regarded as one of the founding events of the
science of epidemiology.
Later, researchers discovered that this public well had been dug only three feet from an old cesspit, which had begun to leak fecal bacteria.
The diapers of a baby, who had contracted cholera from another source,
had been washed into this cesspit. Its opening was originally under a
nearby house, which had been rebuilt farther away after a fire. The city
had widened the street and the cesspit was lost. It was common at the
time to have a cesspit under most homes. Most families tried to have
their raw sewage collected and dumped in the Thames to prevent their
cesspit from filling faster than the sewage could decompose into the
soil.
After the cholera epidemic had subsided, government officials
replaced the handle on the Broad Street pump. They had responded only to
the urgent threat posed to the population, and afterward they rejected
Snow's theory. To accept his proposal would have meant accepting the
fecal-oral method transmission of disease, which they dismissed.
Louis Pasteur
Louis
Pasteur’s pasteurization experiment illustrates the fact that the
spoilage of liquid was caused by particles in the air rather than the
air itself. These experiments were important pieces of evidence
supporting the idea of germ theory of disease.
The more formal experiments on the relationship between germ and disease were conducted by Louis Pasteur between the year 1860 and 1864. He discovered the pathology of the puerperal fever and the pyogenic vibrio in the blood, and suggested using boric acid to kill these microorganisms before and after confinement.
Pasteur further demonstrated between 1860 and 1864 that fermentation and the growth of microorganisms in nutrient broths
did not proceed by spontaneous generation. He exposed freshly boiled
broth to air in vessels that contained a filter to stop all particles
passing through to the growth medium, and even with no filter at all,
with air being admitted via a long tortuous tube that would not pass
dust particles. Nothing grew in the broths: therefore the living
organisms that grew in such broths came from outside, as spores on dust,
rather than being generated within the broth.
Pasteur discovered that another serious disease of silkworms, pébrine, was caused by a small microscopic organism now known as Nosema bombycis
(1870). Pasteur saved France's silk industry by developing a method to
screen silkworms eggs for those that were not infected, a method that is
still used today to control this and other silkworm diseases.
Robert Koch
Robert Koch is known for developing four basic criteria (known as Koch's postulates)
for demonstrating, in a scientifically sound manner, that a disease is
caused by a particular organism. These postulates grew out of his
seminal work with anthrax using purified cultures of the pathogen that had been isolated from diseased animals.
Koch's postulates were developed in the 19th century as general
guidelines to identify pathogens that could be isolated with the
techniques of the day.
Even in Koch's time, it was recognized that some infectious agents were
clearly responsible for disease even though they did not fulfill all of
the postulates.
Attempts to rigidly apply Koch's postulates to the diagnosis of viral
diseases in the late 19th century, at a time when viruses could not be
seen or isolated in culture, may have impeded the early development of
the field of virology.
Currently, a number of infectious agents are accepted as the cause of
disease despite their not fulfilling all of Koch's postulates.
Therefore, while Koch's postulates retain historical importance and
continue to inform the approach to microbiologic diagnosis, fulfillment
of all four postulates is not required to demonstrate causality.
Koch's postulates have also influenced scientists who examine
microbial pathogenesis from a molecular point of view. In the 1980s, a molecular version of Koch's postulates was developed to guide the identification of microbial genes encoding virulence factors.
Koch's postulates:
- The microorganism must be found in abundance in all organisms suffering from the disease, but should not be found in healthy organisms.
- The microorganism must be isolated from a diseased organism and grown in pure culture.
- The cultured microorganism should cause disease when introduced into a healthy organism.
- The microorganism must be reisolated from the inoculated, diseased experimental host and identified as being identical to the original specific causative agent.
However, Koch abandoned the universalist requirement of the first
postulate altogether when he discovered asymptomatic carriers of cholera and, later, of typhoid fever. Asymptomatic or subclinical infection carriers are now known to be a common feature of many infectious diseases, especially viruses such as polio, herpes simplex, HIV, and hepatitis C. As a specific example, all doctors and virologists agree that poliovirus causes paralysis in just a few infected subjects, and the success of the polio vaccine in preventing disease supports the conviction that the poliovirus is the causative agent.
The third postulate specifies "should", not "must", because as Koch himself proved in regard to both tuberculosis and cholera,
not all organisms exposed to an infectious agent will acquire the
infection. Noninfection may be due to such factors as general health and
proper immune functioning; acquired immunity from previous exposure or
vaccination; or genetic immunity, as with the resistance to malaria
conferred by possessing at least one sickle cell allele.
The second postulate may also be suspended for certain
microorganisms or entities that cannot (at the present time) be grown in
pure culture, such as prions responsible for Creutzfeldt–Jakob disease.
In summary, a body of evidence that satisfies Koch's postulates is sufficient but not necessary to establish causation.
Sanitation
In the 1870s, Joseph Lister
was instrumental in developing practical applications of the germ
theory of disease with respect to sanitation in medical settings and
aseptic surgical techniques—partly through the use of carbolic acid (phenol) as an antiseptic.