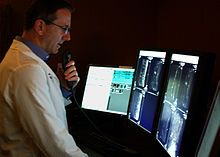
A radiologist interpreting magnetic resonance imaging.
Radiology is the medical specialty that uses medical imaging to diagnose and treat diseases within the bodies of both humans and animals.
A variety of imaging techniques such as X-ray radiography, ultrasound, computed tomography (CT), nuclear medicine including positron emission tomography (PET), and magnetic resonance imaging (MRI) are used to diagnose or treat diseases. Interventional radiology is the performance of usually minimally invasive medical procedures with the guidance of imaging technologies such as those mentioned above.
The modern practice of radiology involves several different
healthcare professions working as a team. The radiologist is a medical
doctor who has completed the appropriate post-graduate training and
interprets medical images, communicates these findings to other
physicians by means of a report or verbally, and uses imaging to perform
minimally invasive medical procedures. The nurse
is involved in the care of patients before and after imaging or
procedures, including administration of medications, monitoring of vital
signs and monitoring of sedated patients. The radiographer, also known as a "radiologic technologist" in some countries such as the United States,
is a specially trained healthcare professional that uses sophisticated
technology and positioning techniques to produce medical images for the
radiologist to interpret. Depending on the individual's training and
country of practice, the radiographer may specialize in one of the
above-mentioned imaging modalities or have expanded roles in image
reporting.
Diagnostic imaging modalities
Projection (plain) radiography
Radiography of the knee using a DR machine.
Projectional radiograph of the knee.
Radiographs (originally called roentgenographs, named after the discoverer of X-rays, Wilhelm Conrad Röntgen)
are produced by transmitting X-rays through a patient. The X-rays are
projected through the body onto a detector; an image is formed based on
which rays pass through (and are detected) versus those that are
absorbed or scattered in the patient (and thus are not detected).
Röntgen discovered X-rays on November 8, 1895 and received the first Nobel Prize in Physics for their discovery in 1901.
In film-screen radiography, an X-ray tube generates a beam of
X-rays, which is aimed at the patient. The X-rays that pass through the
patient are filtered through a device called an grid or X-ray filter,
to reduce scatter, and strike an undeveloped film, which is held
tightly to a screen of light-emitting phosphors in a light-tight
cassette. The film is then developed chemically and an image appears on
the film. Film-screen radiography is being replaced by phosphor plate radiography but more recently by digital radiography (DR) and the EOS imaging.
In the two latest systems, the X-rays strike sensors that converts the
signals generated into digital information, which is transmitted and
converted into an image displayed on a computer screen. In digital radiography
the sensors shape a plate, but in the EOS system, which is a
slot-scanning system, a linear sensor vertically scans the patient.
Plain radiography was the only imaging modality available during
the first 50 years of radiology. Due to its availability, speed, and
lower costs compared to other modalities, radiography is often the
first-line test of choice in radiologic diagnosis. Also despite the
large amount of data in CT scans, MR scans and other digital-based
imaging, there are many disease entities in which the classic diagnosis
is obtained by plain radiographs. Examples include various types of
arthritis and pneumonia, bone tumors (especially benign bone tumors),
fractures, congenital skeletal anomalies, etc.
Mammography and DXA are two applications of low energy projectional radiography, used for the evaluation for breast cancer and osteoporosis, respectively.
Fluoroscopy
Fluoroscopy and angiography are special applications of X-ray imaging, in which a fluorescent screen and image intensifier tube is connected to a closed-circuit television system. This allows real-time imaging of structures in motion or augmented with a radiocontrast
agent. Radiocontrast agents are usually administered by swallowing or
injecting into the body of the patient to delineate anatomy and
functioning of the blood vessels, the genitourinary system, or the gastrointestinal tract (GI tract). Two radiocontrast agents are presently in common use. Barium sulfate (BaSO4)
is given orally or rectally for evaluation of the GI tract. Iodine, in
multiple proprietary forms, is given by oral, rectal, vaginal,
intra-arterial or intravenous routes. These radiocontrast agents
strongly absorb or scatter X-rays, and in conjunction with the real-time
imaging, allow demonstration of dynamic processes, such as peristalsis
in the digestive tract or blood flow in arteries and veins. Iodine
contrast may also be concentrated in abnormal areas more or less than in
normal tissues and make abnormalities (tumors, cysts, inflammation)
more conspicuous. Additionally, in specific circumstances, air can be
used as a contrast agent for the gastrointestinal system and carbon
dioxide can be used as a contrast agent in the venous system; in these
cases, the contrast agent attenuates the X-ray radiation less than the
surrounding tissues.
Computed tomography
Image from a CT scan of the brain
CT imaging uses X-rays in conjunction with computing algorithms to image the body.
In CT, an X-ray tube opposite an X-ray detector (or detectors) in a
ring-shaped apparatus rotate around a patient, producing a
computer-generated cross-sectional image (tomogram). CT is acquired in
the axial
plane, with coronal and sagittal images produced by computer
reconstruction. Radiocontrast agents are often used with CT for enhanced
delineation of anatomy. Although radiographs provide higher spatial
resolution, CT can detect more subtle variations in attenuation of
X-rays (higher contrast resolution). CT exposes the patient to
significantly more ionizing radiation than a radiograph.
Spiral multidetector CT uses 16, 64, 254 or more detectors during
continuous motion of the patient through the radiation beam to obtain
fine detail images in a short exam time. With rapid administration of
intravenous contrast during the CT scan, these fine detail images can be
reconstructed into three-dimensional (3D) images of carotid, cerebral,
coronary or other arteries.
The introduction of computed tomography in the early 1970s
revolutionized diagnostic radiology by providing Clinicians with images
of real three-dimensional anatomic structures. CT scanning has become
the test of choice in diagnosing some urgent and emergent conditions,
such as cerebral hemorrhage, pulmonary embolism (clots in the arteries of the lungs), aortic dissection (tearing of the aortic wall), appendicitis, diverticulitis,
and obstructing kidney stones. Continuing improvements in CT
technology, including faster scanning times and improved resolution,
have dramatically increased the accuracy and usefulness of CT scanning,
which may partially account for increased use in medical diagnosis.
Ultrasound
Medical ultrasonography uses ultrasound (high-frequency sound waves)
to visualize soft tissue structures in the body in real time. No ionizing radiation
is involved, but the quality of the images obtained using ultrasound is
highly dependent on the skill of the person (ultrasonographer)
performing the exam and the patient's body size. Examinations of larger,
overweight patients may have a decrease in image quality as their subcutaneous fat
absorbs more of the sound waves. This results in fewer sound waves
penetrating to organs and reflecting back to the transducer, resulting
in loss of information and a poorer quality image. Ultrasound is also
limited by its inability to image through air pockets (lungs, bowel
loops) or bone. Its use in medical imaging has developed mostly within
the last 30 years. The first ultrasound images were static and
two-dimensional (2D), but with modern ultrasonography, 3D
reconstructions can be observed in real time, effectively becoming "4D".
Because ultrasound imaging techniques do not employ ionizing
radiation to generate images (unlike radiography, and CT scans), they
are generally considered safer and are therefore more common in obstetrical imaging.
The progression of pregnancies can be thoroughly evaluated with less
concern about damage from the techniques employed, allowing early
detection and diagnosis of many fetal anomalies. Growth can be assessed
over time, important in patients with chronic disease or
pregnancy-induced disease, and in multiple pregnancies (twins, triplets,
etc.). Color-flow Doppler ultrasound measures the severity of peripheral vascular disease and is used by cardiologists for dynamic evaluation of the heart, heart valves and major vessels. Stenosis, for example, of the carotid arteries may be a warning sign for an impending stroke. A clot,
embedded deep in one of the inner veins of the legs, can be found via
ultrasound before it dislodges and travels to the lungs, resulting in a
potentially fatal pulmonary embolism. Ultrasounds is useful as a guide to performing biopsies to minimise damage to surrounding tissues and in drainages such as thoracentesis. Small, portable ultrasound devices now replace peritoneal lavage in trauma wards by non-invasively assessing for the presence of internal bleeding and any internal organ damage. Extensive internal bleeding or injury to the major organs may require surgery and repair.
Magnetic resonance imaging
MRI of the knee.
MRI uses strong magnetic fields to align atomic nuclei (usually hydrogen protons) within body tissues, then uses a radio signal to disturb the axis of rotation of these nuclei and observes the radio frequency signal generated as the nuclei return to their baseline states.
The radio signals are collected by small antennae, called coils,
placed near the area of interest. An advantage of MRI is its ability to
produce images in axial, coronal, sagittal
and multiple oblique planes with equal ease. MRI scans give the best
soft tissue contrast of all the imaging modalities. With advances in
scanning speed and spatial resolution, and improvements in computer 3D
algorithms and hardware, MRI has become an important tool in
musculoskeletal radiology and neuroradiology.
One disadvantage is the patient has to hold still for long
periods of time in a noisy, cramped space while the imaging is
performed. Claustrophobia (fear of closed spaces) severe enough to
terminate the MRI exam is reported in up to 5% of patients. Recent
improvements in magnet design including stronger magnetic fields (3 teslas),
shortening exam times, wider, shorter magnet bores and more open magnet
designs, have brought some relief for claustrophobic patients. However,
for magnets with equivalent field strengths, there is often a trade-off
between image quality and open design. MRI has great benefit in imaging
the brain, spine, and musculoskeletal system. The use of MRI is
currently contraindicated for patients with pacemakers, cochlear
implants, some indwelling medication pumps, certain types of cerebral
aneurysm clips, metal fragments in the eyes and some metallic hardware
due to the powerful magnetic fields and strong fluctuating radio signals
to which the body is exposed. Areas of potential advancement include
functional imaging, cardiovascular MRI, and MRI-guided therapy.
Nuclear medicine
Nuclear medicine imaging involves the administration into the patient
of radiopharmaceuticals consisting of substances with affinity for
certain body tissues labeled with radioactive tracer. The most commonly
used tracers are technetium-99m, iodine-123, iodine-131, gallium-67,
indium-111, thallium-201 and fludeoxyglucose (18F) (18F-FDG). The heart, lungs, thyroid, liver, brain, gallbladder, and bones are commonly evaluated for particular conditions using these techniques. While anatomical detail is limited in these studies, nuclear medicine is useful in displaying physiological
function. The excretory function of the kidneys, iodine-concentrating
ability of the thyroid, blood flow to heart muscle, etc. can be
measured. The principal imaging devices are the gamma camera
and the PET Scanner, which detect the radiation emitted by the tracer
in the body and display it as an image. With computer processing, the
information can be displayed as axial, coronal and sagittal images
(single-photon emission computed tomography - SPECT or Positron-emission
tomography - PET). In the most modern devices, nuclear medicine images
can be fused with a CT scan taken quasisimultaneously, so the physiological information can be overlaid or coregistered with the anatomical structures to improve diagnostic accuracy.
Positron emission tomography (PET) scanning deals with positrons instead of gamma rays detected by gamma cameras.
The positrons annihilate to produce two opposite traveling gamma rays
to be detected coincidentally, thus improving resolution. In PET
scanning, a radioactive, biologically active substance, most often
18F-FDG, is injected into a patient and the radiation emitted by the
patient is detected to produce multiplanar images of the body.
Metabolically more active tissues, such as cancer, concentrate the
active substance more than normal tissues. PET images can be combined
(or "fused") with anatomic (CT) imaging, to more accurately localize PET
findings and thereby improve diagnostic accuracy.
The fusion technology has gone further to combine PET and MRI similar to PET and CT. PET/MRI
fusion, largely practiced in academic and research settings, could
potentially play a crucial role in fine detail of brain imaging, breast
cancer screening, and small joint imaging of the foot. The technology
recently blossomed after passing the technical hurdle of altered
positron movement in strong magnetic field thus affecting the resolution
of PET images and attenuation correction.
Interventional radiology
Interventional radiology (IR or sometimes VIR for vascular and
interventional radiology) is a subspecialty of radiology in which
minimally invasive procedures are performed using image guidance. Some
of these procedures are done for purely diagnostic purposes (e.g., angiogram), while others are done for treatment purposes (e.g., angioplasty).
The basic concept behind interventional radiology is to diagnose or treat pathologies,
with the most minimally invasive technique possible. Minimally invasive
procedures are currently performed more than ever before. These
procedures are often performed with the patient fully awake, with little
or no sedation required. Interventional Radiologists and Interventional
Radiographers diagnose and treat several disorders, including peripheral vascular disease, renal artery stenosis, inferior vena cava filter placement, gastrostomy tube placements, biliary stents and hepatic interventions. Images are used for guidance, and the primary instruments used during the procedure are needles and catheters.
The images provide maps that allow the clinician to guide these
instruments through the body to the areas containing disease. By
minimizing the physical trauma to the patient, peripheral interventions
can reduce infection rates and recovery times, as well as hospital
stays. To be a trained interventionalist in the United States, an
individual completes a five-year residency in radiology and a one- or
two-year fellowship in IR.
Analysis of images
A radiologist interprets medical images on a modern picture archiving and communication system (PACS) workstation. San Diego, CA, 2010.
Teleradiology
Teleradiology is the transmission of radiographic images from one
location to another for interpretation by an appropriately trained
professional, usually a Radiologist or Reporting Radiographer. It is
most often used to allow rapid interpretation of emergency room, ICU and
other emergent examinations after hours of usual operation, at night
and on weekends. In these cases, the images can be sent across time
zones (e.g. to Spain, Australia, India) with the receiving Clinician
working his normal daylight hours. However at present, large private
teleradiology companies in the U.S. currently provide most after-hours
coverage employing night working Radiologists in the U.S. Teleradiology
can also be used to obtain consultation with an expert or subspecialist
about a complicated or puzzling case. In the U.S., many hospitals
outsource their radiology departments to radiologists in India due to
the lowered cost and availability of high speed internet access.
Teleradiology requires a sending station, a high-speed internet
connection, and a high-quality receiving station. At the transmission
station, plain radiographs
are passed through a digitizing machine before transmission, while CT,
MRI, ultrasound and nuclear medicine scans can be sent directly, as they
are already digital data. The computer at the receiving end will need
to have a high-quality display screen that has been tested and cleared
for clinical purposes. Reports are then transmitted to the requesting
clinician.
The major advantage of teleradiology is the ability to use different
time zones to provide real-time emergency radiology services
around-the-clock. The disadvantages include higher costs, limited
contact between the referrer and the reporting Clinician, and the
inability to cover for procedures requiring an onsite reporting
Clinician. Laws and regulations concerning the use of teleradiology vary
among the states, with some requiring a license to practice medicine in
the state sending the radiologic exam. In the U.S., some states require
the teleradiology report to be preliminary with the official report
issued by a hospital staff Radiologist. Lastly, the major benefit of
teleradiology is that it can be automated with modern machine learning
techniques.
Professional training
United States
Radiology
is a field in medicine that has expanded rapidly after 2000 due to
advances in computer technology, which is closely linked to modern
imaging techniques. Applying for residency positions in radiology is
relatively competitive. Applicants are often near the top of their
medical school classes, with high USMLE (board) examination scores.
Diagnostic radiologists must complete prerequisite undergraduate
education, four years of medical school to earn a medical degree (D.O. or M.D.), one year of internship, and four years of residency training. After residency, radiologists may pursue one or two years of additional specialty fellowship training.
The American Board of Radiology
(ABR) administers professional certification in Diagnostic Radiology,
Radiation Oncology and Medical Physics as well as subspecialty
certification in neuroradiology, nuclear radiology, pediatric radiology
and vascular and interventional radiology. "Board Certification" in
diagnostic radiology requires successful completion of two examinations.
The Core Exam is given after 36 months of residency. This
computer-based examination is given twice a year in Chicago and Tucson.
It encompasses 18 categories. A pass of all 18 is a pass. A fail on 1 to
5 categories is a Conditioned exam and the resident will need to retake
and pass the failed categories. A fail on over 5 categories is a failed
exam. The Certification Exam, can be taken 15 months after completion
of the Radiology residency. This computer-based examination consists of 5
modules and graded pass-fail. It is given twice a year in Chicago and
Tucson. Recertification examinations are taken every 10 years, with
additional required continuing medical education as outlined in the
Maintenance of Certification document.
Certification may also be obtained from the American Osteopathic Board of Radiology (AOBR) and the American Board of Physician Specialties.
Following completion of residency training, Radiologists may
either begin practicing as a general Diagnostic Radiologist or enter
into subspecialty training programs known as fellowships. Examples of
subspeciality training in radiology include abdominal imaging, thoracic
imaging, cross-sectional/ultrasound, MRI, musculoskeletal imaging, interventional radiology, neuroradiology, interventional neuroradiology, paediatric radiology,
nuclear medicine, emergency radiology, breast imaging and women's
imaging. Fellowship training programs in radiology are usually one or
two years in length.
Some medical schools in the US have started to incorporate a
basic radiology introduction into their core MD training. New York
Medical College, the Wayne State University School of Medicine, Weill Cornell
Medicine, the Uniformed Services University, and the University of
South Carolina School of Medicine offer an introduction to radiology
during their respective MD programs.
Campbell University School of Osteopathic Medicine also integrates
imaging material into their curriculum early in the first year.
Radiographic exams are usually performed by Radiographers. Qualifications for Radiographers vary by country, but many Radiographers now are required to hold a degree.
Veterinary Radiologists are veterinarians who specialize in the
use of X-rays, ultrasound, MRI and nuclear medicine for diagnostic
imaging or treatment of disease in animals. They are certified in either
diagnostic radiology or radiation oncology by the American College of
Veterinary Radiology.
United Kingdom
Radiology
is an extremely competitive speciality in the UK, attracting applicants
from a broad range of backgrounds. Applicants are welcomed directly
from the foundation programme,
as well as those who have completed higher training. Recruitment and
selection into training post in clinical radiology posts in England,
Scotland and Wales is done by an annual nationally coordinated process
lasting from November to March. In this process, all applicants are
required to pass a Specialty Recruitment Assessment (SRA) test.
Those with a test score above a certain threshold are offered a single
interview at the London and the South East Recruitment Office. At a later stage, applicants declare what programs they prefer, but may in some cases be placed in a neighbouring region.
The training programme lasts for a total of five years. During
this time, doctors rotate into different subspecialities, such as
paediatrics, musculoskeletal or neuroradiology, and breast imaging.
During the first year of training, radiology trainees are expected to
pass the first part of the Fellowship of the Royal College of Radiologists
(FRCR) exam. This comprises a medical physics and anatomy examination.
Following completion of their part 1 exam, they are then required to
pass six written exams (part 2A), which cover all the subspecialities.
Successful completion of these allows them to complete the FRCR by
completing part 2B, which includes rapid reporting, and a long case
discussion.
After achieving a certificate of completion of training
(CCT), many fellowship posts exist in specialities such as
neurointervention and vascular intervention, which would allow the
Doctor to work as an Interventional Radiologist. In some cases, the CCT
date can be deferred by a year to include these fellowship programmes.
UK radiology registrars are represented by the Society of
Radiologists in Training (SRT), which was founded in 1993 under the
auspices of the Royal College of Radiologists.
The society is a nonprofit organisation, run by radiology registrars
specifically to promote radiology training and education in the UK.
Annual meetings are held by which trainees across the country are
encouraged to attend.
Currently, a shortage of radiologists in the UK has created
opportunities in all specialities, and with the increased reliance on
imaging, demand is expected to increase in the future. Radiographers, and less frequently Nurses,
are often trained to undertake many of these opportunities in order to
help meet demand. Radiographers often may control a "list" of a
particular set of procedures after being approved locally and signed off
by a Consultant Radiologist. Similarly, Radiographers may simply
operate a list for a Radiologist or other Physician on their behalf.
Most often if a Radiographer operates a list autonomously then they are
acting as the Operator and Practitioner under the Ionising Radiation
(Medical Exposures) Regulations 2000. Radiographers are represented by a
variety of bodies, most often this is the Society and College of Radiographers. Collaboration with Nurses is also common, where a list may be jointly organised between the Nurse and Radiographer.
Germany
After
obtaining medical licensure, German Radiologists complete a five-year
residency, culminating with a board examination (known as Facharztprüfung).
Italy
The
radiology training program in Italy increased from four to five years in
2008. Further training is required for specialization in radiotherapy
or nuclear medicine.
The Netherlands
Dutch radiologists complete a five-year residency program after completing the 6-year MD program.
India
The radiology training course is a post graduate 3-year program (MD/DNB Radiology) or a 2-year diploma (DMRD).
Singapore
Radiologists in Singapore complete a five-year undergraduate medicine degree followed by a one-year Internship (medical)
and then a five-year residency program. Some Radiologists may elect to
complete a one or two-year fellowship for further sub-specialization in
fields such as interventional radiology.