| Artificial insemination | |
|---|---|

Schematic illustration of artificial insemination
| |
| ICD-9-CM | 69.92 |
| MeSH | D007315 |
Artificial insemination (AI) is the deliberate introduction of sperm into a female's cervix or uterine cavity for the purpose of achieving a pregnancy through in vivo fertilization by means other than sexual intercourse. It is a fertility treatment for humans, and is common practice in animal breeding, including dairy cattle and pigs.
Artificial insemination may employ assisted reproductive technology, sperm donation and animal husbandry techniques. Artificial insemination techniques available include intracervical insemination and intrauterine insemination. The beneficiaries of artificial insemination are women who desire to give birth to their own child who may be single, women who are in a lesbian relationship or women who are in a heterosexual relationship but with a male partner who is infertile or who has a physical impairment which prevents full intercourse from taking place. Intracervical insemination (ICI) is the easiest and most common insemination technique and can be used in the home for self-insemination without medical practitioner assistance. Compared with natural insemination (i.e., insemination by sexual intercourse), artificial insemination can be more expensive and more invasive, and may require professional assistance.
Some countries have laws which restrict and regulate who can donate sperm and who is able to receive artificial insemination, and the consequences of such insemination. Some women who live in a jurisdiction which does not permit artificial insemination in the circumstance in which she finds herself may travel to another jurisdiction which permits it.
In humans
History
The first recorded case of artificial insemination was John Hunter in 1790, who helped impregnate a linen draper's wife. The first reported case of artificial insemination by donor occurred in 1884: Dr. William H. Pancoast, a professor in Philadelphia, took sperm from his "best looking" student to inseminate an anesthetized woman. The case was reported 25 years later in a medical journal. The sperm bank
was developed in Iowa starting in the 1920s in research conducted by
University of Iowa medical school researchers Jerome Sherman and Raymond
Bunge.
In the United Kingdom, the British obstetrician Mary Barton founded one of the first fertility clinics to offer donor insemination in the 1930s, with her husband Bertold Wiesner fathering up to 1000 offspring.
In the 1980s, direct intraperitoneal insemination (DIPI) was
occasionally used, where doctors injected sperm into the lower abdomen
through a surgical hole or incision, with the intention of letting them
find the oocyte at the ovary or after entering the genital tract through
the ostium of the fallopian tube.
General
The
sperm used in artificial insemination may be provided by either the
woman's husband or partner (partner sperm) or by a known or anonymous
sperm donor.
If the procedure is successful, the woman will conceive and carry
a baby to term in the normal manner. A pregnancy resulting from
artificial insemination is no different from a pregnancy achieved by
sexual intercourse. In all cases of artificial insemination, the
recipient woman will be the biological mother of any child produced, and
the male whose sperm is used will be the biological father.
There are multiple methods used to obtain the semen necessary for
artificial insemination. Some methods require only men, while others
require a combination of a male and female. Those that require only men
to obtain semen are masturbation or the aspiration of sperm by means of a
puncture of the testicle and epididymus. Methods of collecting semen
that involve a combination of a male and female include interrupted
intercourse, intercourse with a 'collection condom', or the post-coital
aspiration of the semen from the vagina.
There are a number of reasons why a woman with a male partner
would use artificial insemination to achieve pregnancy. For example, a
woman's immune system may be rejecting her partner's sperm as invading
molecules. Women who have issues with the cervix – such as cervical scarring, cervical blockage from endometriosis, or thick cervical mucus – may also benefit from artificial insemination, since the sperm must pass through the cervix to result in fertilization.
In the case of heterosexual couples who are finding it difficult
to conceive, before artificial insemination is turned to as the
solution, doctors will require an examination of both the male and
female involved in order to remove any and all physical hindrances that
are preventing them from naturally achieving a pregnancy. The couple is
also given a fertility test to determine the motility, number, and
viability of the male's sperm and the success of the female's ovulation.
From these tests, the doctor may or may not recommend a form of
artificial insemination.
Preparations
Timing
is critical, as the window and opportunity for fertilization is little
more than twelve hours from the release of the ovum. To increase the
chance of success, the woman's menstrual cycle is closely observed,
often using ovulation kits, ultrasounds or blood tests, such as basal body temperature
tests over, noting the color and texture of the vaginal mucus, and the
softness of the nose of her cervix. To improve the success rate of AI,
drugs to create a stimulated cycle may be used, but the use of such drugs also results in an increased chance of a multiple birth.
Sperm can be provided fresh or washed.
The washing of sperm increases the chances of fertilization. Pre- and
post-concentration of motile sperm is counted. Sperm from a sperm bank
will be frozen and quarantined for a period, and the donor will be
tested before and after production of the sample to ensure that he does
not carry a transmissible disease. For fresh shipping, a semen extender is used.
If sperm is provided by a private donor, either directly or
through a sperm agency, it is usually supplied fresh, not frozen, and it
will not be quarantined. Donor sperm provided in this way may be given
directly to the recipient woman or her partner, or it may be transported
in specially insulated containers. Some donors have their own freezing
apparatus to freeze and store their sperm.
Techniques
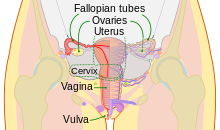
The human female reproductive system. The cervix is part of the uterus. The cervical canal connects the interiors of the uterus and vagina.
Semen used is used either fresh, raw, or frozen. Where donor sperm is
supplied by a sperm bank, it will always be quarantined and frozen, and
will need to be thawed before use. The sperm is ideally donated after
2-3 days of abstinence, without lubrication as the lubricant can inhibit
the sperm motility. When an ovum is released, semen is introduced into the woman's vagina, uterus or cervix, depending on the method being used.
Sperm is occasionally inserted twice within a 'treatment cycle'.
Intracervical insemination
Intracervical
insemination (ICI) simulates an ejaculation of semen by the penis into
the vagina during intercourse. It is painless and is the simplest,
easiest and most common method of artificial insemination. ICI involves
the introduction of unwashed or raw semen into the vagina at the
entrance to the cervix, usually by means of a needleless syringe.
ICI is commonly used in the home, by self-insemination and
practitioner insemination. Raw semen from a private donor may be used
for ICI. Semen supplied by a sperm bank prepared for ICI or IUI use is
suitable for ICI. It is a popular method amongst single and lesbian
women purchasing donor sperm on-line, and was previously used in many
fertility centers as a method of insemination, although its popularity
in this context has waned as other, more reliable methods of
insemination have become available.
During ICI, air is expelled from a needleless syringe which is
then filled with semen which has been allowed to liquify. A
specially-designed syringe, wider and with a more rounded end, may be
used for this purpose. Any further enclosed air is removed by gently
pressing the plunger forward. The woman lies on her back and the syringe
is inserted into the vagina. Care is optimal when inserting the
syringe, so that the tip is as close to the entrance to the cervix as
possible. A vaginal speculum may be used for this purpose. The plunger
is then slowly pushed forward and the semen in the syringe is gently
emptied deep into the vagina. It is important that the syringe is
emptied slowly for best results. The syringe may be left in place for
several minutes before removal. The woman can bring herself to orgasm so
that the cervix 'dips down' into the pool of semen, again replicating
closely vaginal intercourse, and this may improve the success rate. The
woman is advised to lie still for about half-an-hour to improve the
success rate.
One insemination during a cycle is usually sufficient. Additional inseminations may not improve the chances of a pregnancy.
Ordinary sexual lubricants should not be used in the process, but
special fertility or 'sperm-friendly' lubricants can be used for
increased ease and comfort.
When performed at home without the presence of a professional,
aiming the sperm in the vagina at the neck of the cervix may be more
difficult to achieve and the effect may be to 'flood' the vagina with
semen, rather than to target it specifically at the entrance to the
cervix. This procedure is therefore sometimes referred to as
intravaginal insemination (IVI).
Sperm supplied by a sperm bank will be frozen and must be allowed to
thaw before insemination. The sealed end of the straw itself must be cut
off and the open end of the straw is usually fixed straight on to the
tip of the syringe, allowing the contents to be drawn into the syringe.
Sperm from more than one straw can generally be used in the same
syringe. Where fresh semen is used, this must be allowed to liquefy
before inserting it into the syringe, or alternatively, the syringe may
be back-loaded.
A conception cap, which is a form of conception device,
may be inserted into the vagina following insemination and may be left
in place for several hours. Using this method, a woman may go about her
usual activities while the cervical cap holds the semen in the vagina
close to the entrance to the cervix. Advocates of this method claim that
it increases the chances of conception. One advantage with the
conception device is that fresh, non-liquefied semen may be used. The
male may ejaculate straight into the cap so that his fresh semen can be
inserted immediately into the vagina without waiting for it to liquefy,
although a collection cup may also be used. Other methods may be used to
insert semen into the vagina notably involving different uses of a
conception cap. This may, for example, be inserted filled with sperm
which does not have to be liquefied. Alternatively, a specially designed
conception cap with a tube attached may be inserted empty into the
vagina after which liquefied semen is poured into the tube. These
methods are designed to ensure that semen is inseminated as close as
possible to the cervix and that it is kept in place there to increase
the chances of conception.
Intrauterine insemination
Intrauterine insemination (IUI) involves injection of washed sperm into the uterus with a catheter. If unwashed semen is used, it may elicit uterine cramping, expelling the semen and causing pain, due to content of prostaglandins.
(Prostaglandins are also the compounds responsible for causing the
myometrium to contract and expel the menses from the uterus, during menstruation.) Resting on the table for fifteen minutes after an IUI is optimal for the woman to increase the pregnancy rate.
The indications to perform an intrauterine insemination are
usually a moderate male factor, the incapability to ejaculate in vagina
and an idiopathic infertility.
Unlike ICI, intrauterine insemination normally requires a medical
practitioner to perform the procedure. One of the requirements is to
have at least one permeable tube, proved by hysterosalpingography. The
infertility duration is also important. A female under 30 years of age
has optimal chances with IUI; for the man, a TMS of more than 5 million per ml is optimal. In practice, donor sperm will satisfy these criteria. A promising cycle is one that offers two follicles measuring more than 16 mm, and estrogen of more than 500 pg/mL on the day of hCG administration. A short period of ejaculatory abstinence before intrauterine insemination is associated with higher pregnancy rates. However, GnRH agonist
administration at the time of implantation does not improve pregnancy
outcome in intrauterine insemination cycles according to a randomized controlled trial.
IUI is a more efficient method of artificial insemination than
ICI and, because of its generally higher success rate, is usually the
insemination procedure of choice for single women and lesbians using
donor semen in a fertility centre and who are less likely to have
fertility issues of their own. Enabling the sperm to be inserted
directly into the womb will produce a better chance of conceiving.
It is also a method used by couples using donor sperm in a fertility centre.
The steps to follow in order to perform an intrauterine insemination are:
- Mild Controlled Ovarian Stimulation (COS): there is no control f how many oocytes are at the same time when stimulating ovulation. For that reason, it is necessary to check the amount being ovulated via ultrasound (checking the amount of follicles developing at the same time) and administering the desired amount of hormones.
- Ovulation Induction: using substances known as ovulation inductors.
- Semen capacitation: wash and centrifugation, swim-up, or gradient. The insemination shouldn't be performed later than an hour after capacitation.
- Luteal Phase support: progesterone lack of the endometrium could rick the pregnancy. To avoid that 200 mg/day of micronized progesterone are administered via vagina. If there is pregnancy, this hormone is kept administering until the tenth week of pregnancy.
IUI can be used in conjunction with controlled ovarian hyperstimulation (COH). Clomiphene Citrate is the first line, Letrozole is second line, in order to stimulate ovaries before moving on to IVF. Still, advanced maternal age
causes decreased success rates; women aged 38–39 years appear to have
reasonable success during the first two cycles of ovarian
hyperstimulation and IUI. However, for women aged over 40 years, there
appears to be no benefit after a single cycle of COH/IUI.[17] Medical experts therefore recommend considering in vitro fertilization after one failed COH/IUI cycle for women aged over 40 years.
A double intrauterine insemination theoretically increases pregnancy rates by decreasing the risk of missing the fertile window during ovulation. However, a randomized trial of insemination after ovarian hyperstimulation found no difference in live birth rate between single and double intrauterine insemination.
Due to the lack of reliable evidence from controlled clinical
trials, it is not certain which semen preparation techniques are more
effective (wash and centrifugation; swim-up; or gradient) in terms of
pregnancy and live birth rates.
Intrauterine tuboperitoneal insemination
Intrauterine tuboperitoneal insemination (IUTPI) involves injection of washed sperm into both the uterus and fallopian tubes.
The cervix is then clamped to prevent leakage to the vagina, best
achieved with a specially designed double nut bivalve (DNB) speculum.
The sperm is mixed to create a volume of 10 ml, sufficient to fill the uterine cavity, pass through the interstitial part of the tubes and the ampulla, finally reaching the peritoneal cavity and the Pouch of Douglas where it would be mixed with the peritoneal and follicular fluid. IUTPI can be useful in unexplained infertility, mild or moderate male infertility, and mild or moderate endometriosis. In non-tubal sub fertility, fallopian tube sperm perfusion may be the preferred technique over intrauterine insemination.
Intratubal insemination
Intratubal insemination (ITI) involves injection of washed sperm into the fallopian tube, although this procedure is no longer generally regarded as having any beneficial effect compared with IUI. ITI however, should not be confused with gamete intrafallopian transfer,
where both eggs and sperm are mixed outside the woman's body and then
immediately inserted into the fallopian tube where fertilization takes
place.
Pregnancy rate
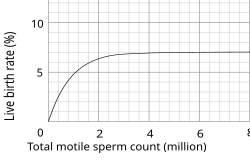
Approximate pregnancy rate as a function of total sperm count (may be twice as large as total motile sperm count). Values are for intrauterine insemination. (Old data, rates are likely higher today)
The rate of successful pregnancy for artificial insemination are 10-15% per menstrual cycle using ICI, and 15–20% per cycle for IUI. In IUI, about 60 to 70% have achieved pregnancy after 6 cycles.
However, these pregnancy rates may be very misleading, since many
factors have to be included to give a meaningful answer, e.g.
definition of success and calculation of the total population.
These rates can be influenced by age, overall reproductive health, and
if the patient had an orgasm during the insemination. The literature is
conflicting on immobilization after insemination has increasing the
chances of pregnancy.
Previous data suggests that it is statistically significant for the
patient to remain immobile for 15 minutes after insemination, while
other review article claims that it is not.
A point of consideration, is that it does cost the patient or
healthcare system to remain immobile for 15 minutes if it does increase
the chances. For couples with unexplained infertility, unstimulated IUI is no more effective than natural means of conception.
The pregnancy rate also depends on the total sperm count, or, more specifically, the total motile sperm count
(TMSC), used in a cycle. The success rate increases with increasing
TMSC, but only up to a certain count, when other factors become limiting
to success. The summed pregnancy rate of two cycles using a TMSC of 5
million (may be a TSC of ~10 million on graph) in each cycle is
substantially higher than one single cycle using a TMSC of 10 million.
However, although more cost-efficient, using a lower TMSC also increases
the average time taken to achieve pregnancy. Women whose age is
becoming a major factor in fertility may not want to spend that extra time.
Samples per child
The
number of samples (ejaculates) required to give rise to a child varies
substantially from person to person, as well as from clinic to clinic.
However, the following equations generalize the main factors involved:
For intracervical insemination:
- N is how many children a single sample can give rise to.
- Vs is the volume of a sample (ejaculate), usually between 1.0 mL and 6.5 mL
- c is the concentration of motile sperm in a sample after freezing and thawing, approximately 5–20 million per ml but varies substantially
- rs is the pregnancy rate per cycle, between 10% to 35%
- nr is the total motile sperm count recommended for vaginal insemination (VI) or intra-cervical insemination (ICI), approximately 20 million pr. ml.
The pregnancy rate increases with increasing number of motile sperm
used, but only up to a certain degree, when other factors become
limiting instead.
Derivation of the equation (click at right to view)
Approximate live birth rate (rs) among infertile couples as a function of total motile sperm count (nr). Values are for intrauterine insemination.
With these numbers, one sample would on average help giving rise to
0.1–0.6 children, that is, it actually takes on average 2–5 samples to
make a child.
For intrauterine insemination, a centrifugation fraction (fc) may be added to the equation:
- fc is the fraction of the volume that remains after centrifugation of the sample, which may be about half (0.5) to a third (0.33).
On the other hand, only 5 million motile sperm may be needed per cycle with IUI (nr=5 million).
Thus, only 1–3 samples may be needed for a child if used for IUI.
Social implications
One of the key issues arising from the rise of dependency on assisted reproductive technology
(ARTs) is the pressure placed on couples to conceive; 'where children
are highly desired, parenthood is culturally mandatory, and
childlessness socially unacceptable'.
The medicalization
of infertility creates a framework in which individuals are encouraged
to think of infertility quite negatively. In many cultures donor
insemination is religiously and culturally prohibited, often meaning
that less accessible "high tech" and expensive ARTs, like IVF, are the
only solution.
An over-reliance on reproductive technologies in dealing with infertility prevents many – especially, for example, in the "infertility belt"
of central and southern Africa – from dealing with many of the key
causes of infertility treatable by artificial insemination techniques;
namely preventable infections, dietary and lifestyle influences.
If good records are not kept, the offspring when grown up risk accidental incest.
Legal restrictions
Some
countries restrict artificial insemination in a variety of ways. For
example, some countries do not permit AI for single women, and some
Muslim countries do not permit the use of donor sperm. As of May 2013,
the following European countries permit medically assisted AI for single
women:
 Armenia
Armenia Belarus
Belarus Belgium
Belgium Bulgaria
Bulgaria Cyprus
Cyprus Denmark
Denmark Estonia
Estonia Finland
Finland Germany
Germany Greece
Greece Hungary
Hungary Iceland
Iceland Ireland
Ireland Latvia
Latvia Macedonia
Macedonia Moldova
Moldova Montenegro
Montenegro Netherlands
Netherlands Romania
Romania Russia
Russia Spain
Spain Ukraine
Ukraine United Kingdom
United Kingdom
In animals
A man performing artificial insemination of a cow.
A breeding mount with built-in artificial vagina used in semen collection from horses for use in artificial insemination
AI is used for pets, livestock, endangered species, and animals in zoos or marine parks difficult to transport.
Reasons and techniques
It may be used for many reasons, including to allow a male to
inseminate a much larger number of females, to allow use of genetic
material from males separated by distance or time, to overcome physical
breeding difficulties, to control the paternity of offspring, to
synchronise births, to avoid injury incurred during natural mating, and
to avoid the need to keep a male at all (such as for small numbers of
females or in species whose fertile males may be difficult to manage).
Semen is collected,
extended, then cooled or frozen. It can be used on site or shipped to
the female's location. If frozen, the small plastic tube holding the
semen is referred to as a straw. To allow the sperm to remain
viable during the time before and after it is frozen, the semen is mixed
with a solution containing glycerol or other cryoprotectants. An extender
is a solution that allows the semen from a donor to impregnate more
females by making insemination possible with fewer sperm. Antibiotics,
such as streptomycin, are sometimes added to the sperm to control some
bacterial venereal diseases. Before the actual insemination, estrus may be induced through the use of progestogen and another hormone (usually PMSG or Prostaglandin F2α).
History
IA tools brought from the USSR by Luis Thomasset in 1935 to work at Cambridge Laboratories and South America.
The first viviparous animal to be artificially fertilized was a dog. The experiment was conducted with success by the Italian Lazzaro Spallanzani in 1780. Another pioneer was the Russian Ilya Ivanov in 1899. In 1935, diluted semen from Suffolk sheep was flown from Cambridge in Britain to Kraków, Poland, as part of an international research project. The participants included Prawochenki (Poland), Milovanoff (USSR), Hammond and Walton (UK), and Thomasset (Uruguay).
Modern artificial insemination was pioneered by John O. Almquist of Pennsylvania State University. He improved breeding efficiency by the use of antibiotics (first proven with penicillin
in 1946) to control bacterial growth, decreasing embryonic mortality,
and increase fertility. This, and various new techniques for processing,
freezing, and thawing of frozen semen significantly enhanced the
practical utilization of AI in the livestock industry, and earned him
the 1981 Wolf Foundation Prize in Agriculture. Many techniques developed by him have since been applied to other species, including humans.
Species
Artificial insemination is used in many non-human animals, including sheep, horses, cattle, pigs, dogs, pedigree animals generally, zoo animals, turkeys and creatures as tiny as honeybees and as massive as orcas (killer whales).
Artificial insemination of farm animals is common in the
developed world, especially for breeding dairy cattle (75% of all
inseminations). Swine
are also bred using this method (up to 85% of all inseminations). It is
an economical means for a livestock breeder to improve their herds
utilizing males having desirable traits.
This procedure is condemned by animal rights campaigners such as People for the Ethical Treatment of Animals and Joey Carbstrong, who identify the practice as a form of rape due to its sexual, involuntary and perceived painful nature.
Although common with cattle and swine, AI is not as widely practised in the breeding of horses.
A small number of equine associations in North America accept only
horses that have been conceived by "natural cover" or "natural
service" – the actual physical mating of a mare to a stallion – the Jockey Club being the most notable of these, as no AI is allowed in Thoroughbred breeding. Other registries such as the AQHA and warmblood
registries allow registration of foals created through AI, and the
process is widely used allowing the breeding of mares to stallions not
resident at the same facility – or even in the same country – through
the use of transported frozen or cooled semen.
In modern species conservation, semen collection and artificial
insemination is used also in birds. In 2013 scientist of the
Justus-Liebig-University of Giessen, Germany, from the working group of
Michael Lierz, Clinic for birds, reptiles, amphibians and fish,
developed a novel technique for semen collection and artificial
insemination in parrots producing the world's first macaw by assisted
reproduction.
Scientists working with captive orcas
were able to pioneer the technique in the early 2000s, resulting in
"the first successful conceptions, resulting in live offspring, using
artificial insemination in any cetacean species". John Hargrove, a SeaWorld trainer, describes Kasatka as being the first orca to receive AI.