| Polycystic kidney disease | |
|---|---|
| Other names | Kidney - polycystic |
 | |
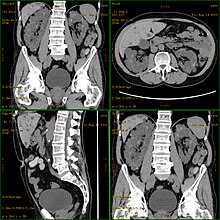
| Severely affected polycystic kidneys removed at time of transplantation | |
| Specialty | Nephrology |
| Symptoms | Abdominal pain |
| Types | ADPKD and ARPKD |
| Diagnostic method | MRI, CT scan, Ultrasound |
| Treatment | Antihypertensives, Life style management |
Polycystic kidney disease (PKD or PCKD, also known as polycystic kidney syndrome) is a genetic disorder in which the renal tubules become structurally abnormal, resulting in the development and growth of multiple cysts within the kidney. These cysts may begin to develop in utero, in infancy, in childhood, or in adulthood. Cysts are non-functioning tubules filled with fluid pumped into them, which range in size from microscopic to enormous, crushing adjacent normal tubules and eventually rendering them non-functional as well.
PKD is caused by abnormal genes which produce a specific abnormal protein; this protein has an adverse effect on tubule development. PKD is a general term for two types, each having their own pathology and genetic cause: autosomal dominant polycystic kidney disease (ADPKD) and autosomal recessive polycystic kidney disease (ARPKD). The abnormal gene exists in all cells in the body; as a result, cysts may occur in the liver, seminal vesicles, and pancreas. This genetic defect can also cause aortic root aneurysms, and aneurysms in the circle of Willis cerebral arteries, which if they rupture, can cause a subarachnoid hemorrhage.
Diagnosis may be suspected from one, some, or all of the following: new onset flank pain or red urine; a positive family history; palpation of enlarged kidneys on physical exam; an incidental finding on abdominal sonogram; or an incidental finding of abnormal kidney function on routine lab work (BUN, serum creatinine, or eGFR). Definitive diagnosis is made by abdominal CT exam.
Complications include hypertension due to the activation of the renin–angiotensin–aldosterone system (RAAS), frequent cyst infections, urinary bleeding, and declining renal function. Hypertension is treated with angiotensin converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs). Infections are treated with antibiotics. Declining renal function is treated with renal replacement therapy (RRT): dialysis and/or transplantation. Management from the time of the suspected or definitive diagnosis is by a board-certified nephrologist.
Signs and symptoms
Signs and symptoms include high blood pressure, headaches, abdominal pain, blood in the urine, and excessive urination. Other symptoms include pain in the back, and cyst formation (renal and other organs).
Cause
PKD is
caused by abnormal genes which produce a specific abnormal protein which
has an adverse effect on tubule development. PKD is a general term for
two types, each having their own pathology and genetic cause: autosomal dominant polycystic kidney disease (ADPKD) and autosomal recessive polycystic kidney disease (ARPKD).
Autosomal dominant
CT scan showing autosomal dominant polycystic kidney disease
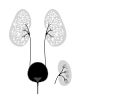
Cartoon of autosomal dominant polycystic kidney disease with normal kidney inset to right of diagram
Cartoon of autosomal recessive polycystic kidney disease with normal kidney inset to right of diagram
Autosomal dominant polycystic kidney disease (ADPKD) is the most common of all the inherited cystic kidney diseases with an incidence of 1:500 live births. Studies show that 10% of end-stage kidney disease (ESKD) patients being treated with dialysis in Europe and the U.S. were initially diagnosed and treated for ADPKD.
Genetic mutations in any of the three genes PKD1, PKD2, and PKD3 have similar phenotypical presentations.
- Gene PKD1 is located on chromosome 16 and codes for a protein involved in regulation of cell cycle and intracellular calcium transport in epithelial cells, and is responsible for 85% of the cases of ADPKD.
- A group of voltage-linked cation channels, with inward selectivity for K>Na>>Ca and outward selectivity for Ca2+ ≈ Ba2+ > Na+ ≈ K+, are coded for by PKD2 on chromosome 4
- PKD3 recently appeared in research papers as a postulated third gene. Fewer than 10% of cases of ADPKD appear in non-ADPKD families. Cyst formation begins in utero from any point along the nephron, although fewer than 5% of nephrons are thought to be involved. As the cysts accumulate fluid, they enlarge, separate entirely from the nephron, compress the neighboring kidney parenchyma, and progressively compromise kidney function.
Autosomal recessive
Autosomal recessive polycystic kidney disease
(ARPKD) (OMIM #263200) is the lesser common of the two types of PKD,
with an incidence of 1:20,000 live births and is typically identified in
the first few weeks after birth. Unfortunately, the kidneys are often underdeveloped resulting in a 30% death rate in newborns with ARPKD. PKHD1 is involved.
Mechanism
PKD1 and PKD2
Both autosomal dominant and autosomal recessive polycystic kidney disease cyst formation are tied to abnormal cilia-mediated signaling. The polycystin-1 and polycystin-2
proteins appear to be involved in both autosomal dominant and recessive
polycystic kidney disease due to defects in both proteins.
Both proteins have communication with calcium channel proteins, and
causes reduction in resting (intracellular) calcium and endoplasmic
reticulum storage of calcium.
The disease is characterized by a ‘second hit’ phenomenon, in
which a mutated dominant allele is inherited from a parent, with cyst
formation occurring only after the normal, wild-type gene sustains a
subsequent second genetic ‘hit’, resulting in renal tubular cyst
formation and disease progression.
PKD results from defects in the primary cilium,
an immotile, hair-like cellular organelle present on the surface of
most cells in the body, anchored in the cell body by the basal body.
In the kidney, primary cilia have been found to be present on most
cells of the nephron, projecting from the apical surface of the renal
epithelium into the tubule lumen. The cilia were believed to bend in the
urine flow, leading to changes in signalling, however this has since
been shown to be an experimental error (the bending of cilia was an
artifact of focal plane compensation, and also the actual effect on
micturition by severe hypertension and cardiac arrest) and that bending
of cilia does not contribute to alterations in Ca flux. While it is not
known how defects in the primary cilium lead to cyst development, it is
thought to possibly be related to disruption of one of the many
signaling pathways regulated by the primary cilium, including
intracellular calcium, Wnt/β-catenin, cyclic adenosine monophosphate
(cAMP), or planar cell polarity (PCP). Function of the primary cilium is
impaired, resulting in disruption of a number of intracellular
signaling cascades which produce differentiation of cystic epithelium,
increased cell division, increased apoptosis, and loss of resorptive
capacity.
Diagnosis
Polycystic kidney disease can be ascertained via a CT scan of abdomen, as well as, an MRI and ultrasound of the same area. A physical exam/test can reveal enlarged liver, heart murmurs and elevated blood pressure
Natural history
Most cases progress to bilateral disease in adulthood.
Treatment
Chr 11 FISH-mapped BACs from CGAP
There is no FDA-approved treatment. However, recent research
indicates that mild to moderate dietary restrictions slow the
progression of autosomal dominant polycystic kidney disease (ADPKD) in mice.
If and when the disease progresses enough in a given case, the nephrologist or other practitioner and the patient will have to decide what form of renal replacement therapy will be used to treat end-stage kidney disease (kidney failure, typically stage 4 or 5 of chronic kidney disease).
That will either be some form of dialysis,
which can be done at least two different ways at varying frequencies
and durations (whether it is done at home or in the clinic depends on
the method used and the patient's stability and training) and
eventually, if they are eligible because of the nature and severity of
their condition and if a suitable match can be found, unilateral or
bilateral kidney transplantation.
A Cochrane Review study of autosomal dominant polycystic kidney
disease made note of the fact that it is important at all times, while
avoiding antibiotic resistance,
to control infections of the cysts in the kidneys, and if affected, the
liver, when needed for a certain duration to combat infection, by
using, "bacteriostatic and bacteriocidal drugs".
Prognosis
ADPKD individuals might have a normal life; conversely, ARPKD can cause kidney dysfunction and can lead to kidney failure by the age of 40–60. ADPKD1 and ADPKD2 are very different, in that ADPKD2 is much milder.
Currently, there are no therapies proven effective to prevent the progression of ADPKD.