Passive immunity is the transfer of active humoral immunity of ready-made antibodies. Passive immunity can occur naturally, when maternal antibodies are transferred to the fetus through the placenta, and it can also be induced artificially, when high levels of antibodies specific to a pathogen or toxin (obtained from humans, horses, or other animals) are transferred to non-immune persons through blood products that contain antibodies, such as in immunoglobulin therapy or antiserum therapy. Passive immunization
is used when there is a high risk of infection and insufficient time
for the body to develop its own immune response, or to reduce the
symptoms of ongoing or immunosuppressive diseases.
Passive immunization can be provided when people cannot synthesize
antibodies, and when they have been exposed to a disease that they do
not have immunity against.
Naturally acquired
Maternal passive immunity is a type of naturally acquired passive immunity, and refers to antibody-mediated immunity conveyed to a fetus or infant by its mother. Naturally acquired passive immunity can be provided during pregnancy, and through breastfeeding. In humans, maternal antibodies (MatAb) are passed through the placenta to the fetus by an FcRn
receptor on placental cells. This occurs predominately during the third
trimester of pregnancy, and thus is often reduced in babies born
prematurely. Immunoglobulin G (IgG) is the only antibody isotype
that can pass through the human placenta, and is the most common
antibody of the five types of antibodies found in the body. IgG
antibodies protects against bacterial and viral infections in fetuses.
Immunization is often required shortly following birth to prevent
diseases in newborns such as tuberculosis, hepatitis B, polio, and pertussis,
however, maternal IgG can inhibit the induction of protective vaccine
responses throughout the first year of life. This effect is usually
overcome by secondary responses to booster immunization.
Maternal antibodies protect against some diseases, such as measles,
rubella, and tetanus, more effectively than against others, such as
polio and pertussis.
Maternal passive immunity offers immediate protection, though
protection mediated by maternal IgG typically only lasts up to a year.
Passive immunity is also provided through colostrum and breast milk, which contain IgA
antibodies that are transferred to the gut of the infant, providing
local protection against disease causing bacteria and viruses until the
newborn can synthesize its own antibodies.
Protection mediated by IgA is dependent on the length of time that an
infant is breastfed, which is one of the reasons the World Health
Organization recommends breastfeeding for at least the first two years
of life.
Other species besides humans transfer maternal antibodies before
birth, including primates and lagomorphs (which includes rabbits and
hares).
In some of these species IgM can be transferred across the placenta as
well as IgG. All other mammalian species predominantly or solely
transfer maternal antibodies after birth through milk. In these species,
the neonatal gut is able to absorb IgG for hours to days after birth.
However, after a period of time the neonate can no longer absorb
maternal IgG through their gut, an event that is referred to as "gut
closure". If a neonatal animal does not receive adequate amounts of
colostrum prior to gut closure, it does not have a sufficient amount of
maternal IgG in its blood to fight off common diseases. This condition
is referred to as failure of passive transfer. It can be diagnosed by
measuring the amount of IgG in a newborn's blood, and is treated with
intravenous administration of immunoglobulins. If not treated, it can be
fatal.
Artificially acquired
Artificially acquired passive immunity is a short-term immunization
achieved by the transfer of antibodies, which can be administered in
several forms; as human or animal blood plasma or serum, as pooled human immunoglobulin for intravenous (IVIG)
or intramuscular (IG) use, as high-titer human IVIG or IG from
immunized donors or from donors recovering from the disease, and as monoclonal antibodies (MAb). Passive transfer is used to prevent disease or used prophylactically in the case of immunodeficiency diseases, such as hypogammaglobulinemia. It is also used in the treatment of several types of acute infection, and to treat poisoning. Immunity derived from passive immunization lasts for a few weeks to three to four months. There is also a potential risk for hypersensitivity reactions, and serum sickness, especially from gamma globulin of non-human origin.
Passive immunity provides immediate protection, but the body does not
develop memory, therefore the patient is at risk of being infected by
the same pathogen later unless they acquire active immunity or
vaccination.
History and applications of artificial passive immunity
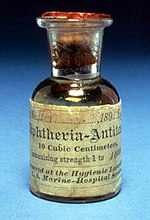
A vial of diphtheria antitoxin, dated 1895
In 1888 Emile Roux and Alexandre Yersin showed that the clinical effects of diphtheria were caused by diphtheria toxin and, following the 1890 discovery of an antitoxin-based immunity to diphtheria and tetanus by Emil Adolf von Behring and Kitasato Shibasaburō, antitoxin became the first major success of modern therapeutic immunology.
Shibasaburo and von Behring immunized guinea pigs with the blood
products from animals that had recovered from diphtheria and realized
that the same process of heat treating blood products of other animals
could treat humans with diphtheria.
By 1896, the introduction of diphtheria antitoxin was hailed as "the
most important advance of the [19th] Century in the medical treatment of
acute infective disease".
Prior to the advent of vaccines and antibiotics,
specific antitoxin was often the only treatment available for
infections such as diphtheria and tetanus. Immunoglobulin therapy
continued to be a first line therapy in the treatment of severe respiratory diseases until the 1930s, even after sulfonamides were introduced.
This
image is from the Historical Medical Library of The College of
Physicians of Philadelphia. This displays the administration of
diphtheria antitoxin from horse serum to young child, dated 1895.
In 1890 antibody therapy was used to treat tetanus,
when serum from immunized horses was injected into patients with severe
tetanus in an attempt to neutralize the tetanus toxin, and prevent the
dissemination of the disease. Since the 1960s, human tetanus immune
globulin (TIG) has been used in the United States in unimmunized,
vaccine-naive or incompletely immunized patients who have sustained
wounds consistent with the development of tetanus. The administration of horse antitoxin remains the only specific pharmacologic treatment available for botulism.
Antitoxin also known as heterologous hyperimmune serum is often also
given prophylactically to individuals known to have ingested
contaminated food. IVIG treatment was also used successfully to treat several victims of toxic shock syndrome, during the 1970s tampon scare.
Antibody therapy is also used to treat viral infections. In 1945, hepatitis A infections, epidemic in summer camps, were successfully prevented by immunoglobulin treatment. Similarly, hepatitis B
immune globulin (HBIG) effectively prevents hepatitis B infection.
Antibody prophylaxis of both hepatitis A and B has largely been
supplanted by the introduction of vaccines; however, it is still
indicated following exposure and prior to travel to areas of endemic
infection.
In 1953, human vaccinia immunoglobulin (VIG) was used to prevent the spread of smallpox during an outbreak in Madras, India, and continues to be used to treat complications arising from smallpox vaccination. Although the prevention of measles is typically induced through vaccination, it is often treated immuno-prophylactically upon exposure. Prevention of rabies infection still requires the use of both vaccine and immunoglobulin treatments.
During a 1995 Ebola virus outbreak in the Democratic Republic of Congo,
whole blood from recovering patients, and containing anti-Ebola
antibodies, was used to treat eight patients, as there was no effective
means of prevention, though a treatment was discovered recently in the
2013 Ebola epidemic in Africa. Only one of the eight infected patients
died, compared to a typical 80% Ebola mortality, which suggested that
antibody treatment may contribute to survival. Immune globulin or immunoglobulin has been used to both prevent and treat reactivation of the herpes simplex virus (HSV), varicella zoster virus, Epstein-Barr virus (EBV), and cytomegalovirus (CMV).[12]
FDA licensed immunoglobulins
The following immunoglobulins are the immunoglubulins currently approved for use for infectious disease prophylaxis and immunotherapy, in the United States.
| Disease | Product | Source | Use |
|---|---|---|---|
| Botulism | Specific equine IgG | horse | Treatment of wound and food borne forms of botulism, infant botulism is treated with human botulism immune globulin (BabyBIG). |
| Cytomegalovirus (CMV) | hyper-immune IVIG | human | Prophylaxis, used most often in kidney transplant patients. |
| Diphtheria | Specific equine IgG | horse | Treatment of diphtheria infection. |
| Hepatitis A, measles | Pooled human Ig | human serum | Prevention of Hepatitis A and measles infection, treatment of congenital or acquired immunodeficiency. |
| Hepatitis B | Hepatitis B Ig | human | Post-exposure prophylaxis, prevention in high-risk infants (administered with Hepatitis B vaccine). |
| ITP, Kawasaki disease, IgG deficiency | Pooled human IgG | human serum | Treatment of ITP and Kawasaki disease, prevention/treatment of opportunistic infection with IgG deficiency. |
| Rabies | Rabies Ig | human | Post-exposure prophylaxis (administered with rabies vaccine). |
| Tetanus | Tetanus Ig | human | Treatment of tetanus infection. |
| Vaccinia | Vaccinia Ig | human | Treatment of progressive vaccinia infection including eczema and ocular forms (usually resulting from smallpox vaccination in immunocompromised individuals). |
| Varicella (chicken-pox) | Varicella-zoster Ig | human | Post-exposure prophylaxis in high risk individuals. |
Passive transfer of cell-mediated immunity
The one exception to passive humoral immunity is the passive transfer of cell-mediated immunity, also called adoptive immunization which involves the transfer of mature circulating lymphocytes. It is rarely used in humans, and requires histocompatible (matched) donors, which are often difficult to find, and carries severe risks of graft-versus-host disease. This technique has been used in humans to treat certain diseases including some types of cancer and immunodeficiency. However, this specialized form of passive immunity is most often used in a laboratory setting in the field of immunology, to transfer immunity between "congenic", or deliberately inbred mouse strains which are histocompatible.
Advantages and disadvantages
An
individual's immune response of passive immunity is "faster than a
vaccine" and can instill immunity in an individual that does not
"respond to immunization", often within hours or a few days. In addition
to conferring passive immunities, breastfeeding has other lasting
beneficial effects on the baby's health, such as decreased risk of
allergies and obesity.
A disadvantage to passive immunity is that producing antibodies
in a laboratory is expensive and difficult to do. In order to produce
antibodies for infectious diseases, there is a need for possibly
thousands of human donors to donate blood or immune animals' blood would
be obtained for the antibodies. Patients who are immunized with the
antibodies from animals may develop serum sickness due to the proteins
from the immune animal and develop serious allergic reactions.
Antibody treatments can be time consuming and are given through an
intravenous injection or IV, while a vaccine shot or jab is less time
consuming and has less risk of complication than an antibody treatment.
Passive immunity is effective, but only lasts a short amount of time.